OVERVIEW
Corneal ectasia is one of the rare yet potentially devastating complications encountered after refractive surgery including laser in situ keratomileusis (LASIK) and photorefractive keratectomy (PRK). This complication affects the primary desired outcome of LASIK, excellent uncorrected distance visual acuity (UDVA). Ectasia after refractive surgery is a progressive increase in myopia, with or without increasing astigmatism, with keratometric steepening of the cornea and topographic asymmetric inferior corneal steepening. Over time there can be associated thinning of the central and paracentral ectatic cornea. It comes to clinical attention when there is associated loss of UDVA, which is usually accompanied with loss of best corrected distance visual acuity (CDVA).(1, 2)
The first few recognized reports were published by Seiler et al. in 1998.(3, 4) They described case reports of patients after LASIK with progression of myopia and rapid progression of central steepening, which they classified as keratectasia. Since these initial reports, there have been hundreds of reported cases in the literature.(2-19) These reports include cases of ectasia that occur as early as a few days to a week after LASIK, and cases that occur as late as several years later.(4, 6, 7) However, only a minority of cases are found at either of these extremes; 50% of cases present within the first year and up to 80% present within 2 years.(8)
In the early years of LASIK, ectasia was under recognized.(2-4) Detection tools were not as precise as what is now available. The main goal in recognizing ectasia was to prevent misclassification as myopic regression and thus prevent re-treatment, which would worsen visual outcomes by hastening the progression of ectasia. Treatment strategies, once limited, have now increased in scope and have improved outcomes for patients.
Epidemiology and Demographics
The majority of ectasia cases after refractive surgery occur after LASIK and not PRK. One large series found that 96% of cases occurred after cases and only 4% occurred after PRK. As a result, most of the discussion in this paper refers to ectasia after LASIK.(8)
The actual incidence of ectasia after LASIK is undetermined. Reported incidence estimates from various populations of cases range from 0.04-0.6%.(2, 8-11) There are a wide range of preoperative characteristics in those patients who develop ectasia. Prior studies show that as a whole, there are more males than females, they tend to be younger, more myopic, and have thinner corneas at baseline.(8, 12-15, 20)
Biomechanical and Histopathologic Properties of the Cornea
LASIK is associated with changes in histopathology and biomechanics of the cornea that put patients at risk for developing ectasia after LASIK. LASIK results in a weakening of the biomechanical strength of the cornea as the effective thickness of the cornea is reduced. The LASIK flap itself is functionally decoupled from the cornea thus providing minimal tensile strength.(21) In the majority of patients, this is of no clinical consequence.(16) However, in a small subset of patients, this results in significant loss of biomechanical integrity. Most of these patients have predisposing pre-operative factors making them more likely to develop ectasia; a small percentage have had either corneas that are overly thinned or a low residual stromal bed (RSB) thickness from a deep ablation or a thicker flap, resulting in a loss of ability to maintain the integrity of the cornea.(22) Thicker flaps and deeper ablations, leaving thinner RSBs, have a greater effect in reducing biomechanical integrity. In the native cornea, the anterior 40% of the cornea has a higher cohesive tensile strength than the posterior 60% perhaps due to the higher keratocyte density in the anterior 10% of the stroma.(16, 21, 22) Roberts and Dupps suggest that biomechanical modification after LASIK is focal in nature.(23) Work by Scarcelli et. al evaluating biomechanical strength of keratoconus corneas with Brillouin microscopy also found that mechanical loss was focal, primarily concentrated within the area of the cone.(24) This focal reduction in elastic modulus results in biomechanical decompensation initiating a cycle of increased strain, stress redistribution, and subsequent focal steepening and thinning; in short, ectasia.(16, 21-25)
One histopathologic study looked at 12 ectatic corneas after LASIK that underwent corneal transplantation.(26) The specimens were examined under light microscopy and transmission electron microscopy (TEM). The former showed epithelial hypoplasia and hyperplasia, bowman’s layer breaks, hypocellular stromal scarring, thinned RSBs, and artifactually larger interlamellar clefts within the ectatic region. There was thinning and loss of rigidity in the stress-bearing regions of the stroma. TEM showed thinning of the collagen lamellae and loss of the total number of lamellae within the RSB. They concluded that there was both interlamellar and subsequent interfibrillar slippage contributing to the chronic biomechanical failure in ectasia after LASIK. A nearly identical biomechanical failure is seen in keratoconus.(26) Thus LASIK may reduce corneal biomechanical integrity by reducing load-bearing tissue, and decreasing the tensile strength of the remaining issue both due to decoupling of the LASIK flap and the decrease of keratocyte density thus leading to instability and contributing to the development of ectasia after LASIK.
PREOPERATIVE RISK FACTORS
As the early case reports of ectasia after LASIK were published, there was an attempt to determine pre-operative risk factors for ectasia to improve patient screening. Residual stromal bed thickness, corneal thickness, and abnormal topography (ie. forme fruste keratoconus) were recognized early on as potential markers.(17-19) Multiple enhancements have also been correlated with ectasia.(8) Barraquer was the first to estimate that the minimal thickness need to avoid iatrogenic keratoconus, as it was called at the time, was 250-300 um.(4, 18, 19, 27) Seiler suggested that using a percentage of the corneal thickness as a minimal residual stromal thickness rather than an absolute number would be safer, however the limitation at the time was lack of sufficient aggregate data to calculate this.(19)
As more cases of ectasia occurred, physicians began looking at larger case series and other risk factors were identified including high myopia, abnormal topography (ie. forme fruste keratoconus), and low RSB. In one large series, all patients who developed ectasia after LASIK had one or more of these recognizable pre-operative risk factors.(2)
Randleman et al. did a large retrospective study in which they looked at 171 cases of ectasia after refractive surgery (164 were after LASIK) with age-matched controls with uneventful LASIK with no postoperative complications. They looked at preoperative and postoperative characteristics of the cases and controls. Some of the pertinent characteristics looked at included age, gender, refraction, spherical equivalent, refraction, preoperative pachymetry, preoperative topography, estimated flap thickness (predicted or measured), intraoperative pachymetry measurements (if obtained), calculated central ablation depth, RSB thickness (measured intra op or calculated based on preoperative pachymetry), and time to onset of ectasia. Ectasia cases were on average younger, more myopic, were more likely to have abnormal topography, had thinner corneas before surgery, and had less RSB thickness. The most significant factor that distinguished cases from controls was abnormal topography. These findings were consistent with what prior papers had noted.(2, 4, 17-19, 27, 28) In an attempt to develop a quantitative method by which to identify eyes at risk for developing ectasia after LASIK, they used this data to create a risk factor stratification scale which they named the Ectasia Risk Score System (ERSS). Topography pattern, RSB thickness, Age, preoperative corneal thickness, and preoperative spherical equivalent manifest refraction were included. The scoring system assigned different points, from 0-4, based on the findings. The higher points were assigned to factors found to be more correlated with ectatic cases as compared to controls (the highest points were assigned to those most correlated). In their series, the risk calculator was 96% sensitive and 91% specific.(8) Randleman et al. also performed a separate validation of the ERSS with an independent series of fifty eyes that developed ectasia after LASIK, compared to fifty matched controls.(12)
The ERSS was based on placido disk-based topography, which measures anterior surface curvature. Other imaging modalities, including Scheimpflug and high resolution anterior segment ocular coherence tomography (AS-OCT) can determine regional and relational corneal thickness and epithelial thickness profiles. They can also show posterior corneal curvature. Changes in epithelial thickness may be related to early keratoconus (forme fruste and otherwise). Authors have suggested that the use of epithelial thickness profiles may serve as an early indicator of ectatic changes.(20, 29-31) Ocular response analyzers (ORA) measure corneal hysteresis; however studies have shown that it is not a useful discriminator for keratoconus or ectasia.(32)
CLINICAL AND TOPOGRAPHIC SIGNS OF ECTASIA
Clinical Signs
Early clinical detection of ectasia after LASIK requires high clinical suspicion. The first signs are often progression of myopia and astigmatism, with a resulting decrease in UCVA. This can sometimes be confused with treatment regression. More advanced and concerning signs are an increase in irregular astigmatism and an accompanying decrease in BCVA. This can be accompanied by corneal thinning, usually inferiorly.(20)
Topographic Signs
Topographic changes are initially subtle. There can be a mild increase in irregular astigmatism. This may be accompanied by focal steepening, often inferiorly. These changes progress and become more well-defined over time. In advanced cases, the changes can be indistinguishable from KCN or PMD. (Fig. 1-4)
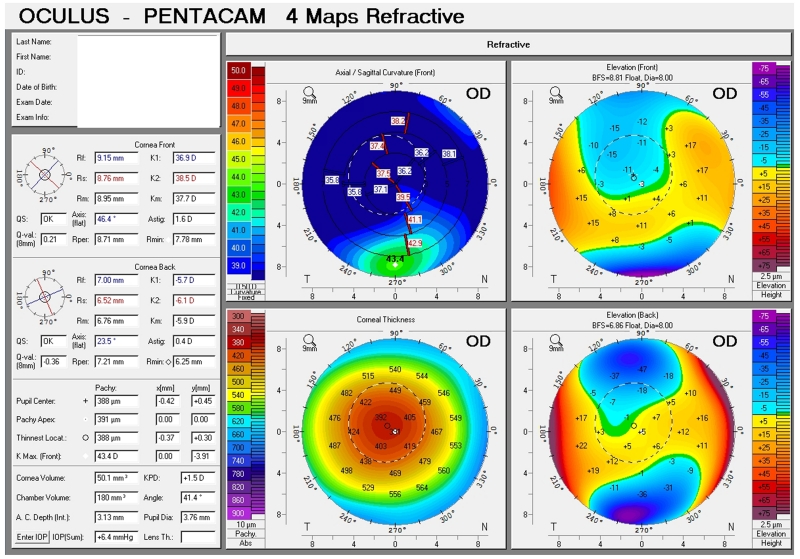
Figure 1. Early ectasia.
Initial topographic changes in corneal ectasia. There is mild inferior corneal steepening.
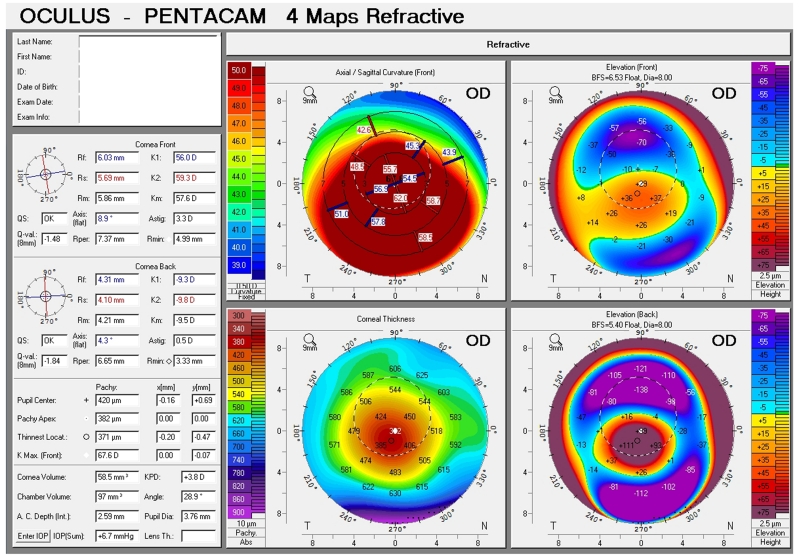
Figure 4. KCN.
Keratoconus can be confused for corneal ectasia when looking at topography alone. Here there is moderate inferior steepening in more of an asymmetric bow tie manner.
Exacerbation with repeat surgery
Patients as above, with characteristics suspicious for possible ectasia, should not undergo any enhancement surgery. Early ectasia can present with just subtle refractive changes and multiple repeat enhancements would worsen the condition.(2, 11) This may be due to less RSB after each enhancement. Utilizing intraoperative pachymetry measurements or confocal microscopy prior to repeat enhancement can provide accurate RSB thickness measurements without disruption of the flap itself. (33, 34)
MANAGEMENT OF ECTASIA
Eyes with postoperative ectasia develop increased myopia and astigmatism with decreased UCVA and subsequently BCVA. Woodward et al. describe the characteristics of ectatic eyes in a cohort of 74 eyes. The mean UCVA (20/400) and mean BCVA (20/108) were both significantly decreased, as compared to the preoperative mean BCVA (20/21).(35)
Once patients have developed symptomatic ectasia, the next step is to provide visual rehabilitation. There are many treatments currently available, both non-invasive and invasive; some have been available for many decades, and some are newer treatment modalities still under investigation.
Conservative Management
Glasses
Mild cases of ectasia have been treated with spectacles and/or soft contact lenses. However, this is usually insufficient for the majority of cases given the high incidence of irregular astigmatism.(8, 35)
Rigid Gas Permeable Lenses
The majority of decreased vision results from irregular astigmatism. Rigid gas permeable lenses (RGP) are the main treatment option for irregular astigmatism and work well for the majority of ectasia after LASIK cases. One large study showed that 80% of ectatic eyes were successfully treated with RGPs. The mean BCVA could be improved to 20/35 with RGP (from baseline BCVA of 20/108). Most of the RGP failures occurred in the first 2 years of RGP wear.(20, 35) Reasons for failure were similar to those experienced by keratoconus patients: discomfort and intolerance, inability to fit the ectatic cornea, or poor resultant visual acuity.(36, 37) Fitting can be complex and, unsurprisingly, is akin to fitting for keratoconus. Many different lens types have been shown to provide appropriate fit and comfort.(38) When a patient is unable to tolerate traditional RGP, hybrid contact lenses have been reported to improve tolerance.(39)
Scleral Lenses
In patients who lack subjective and/or physiologic tolerance of RGP or hybrid lenses, large diameter scleral lenses can have therapeutic value. Scleral lenses are an older style of lens with renewed interest in this, and other, specific patient populations. These lenses fit over a larger surface and provide a larger pocket of tears neutralizing optical irregularities and are more comfortable. Contact lens fitting for ectatic eyes is complex. Optometrists need to account for reverse geometry of eyes that have undergone myopic ablation, excessive steepening, etc.(40-43) Scleral lenses essentially make the fitting independent of corneal contour, allowing for a more accurate fit.(42, 43)
Minimally Invasive Management
Intracorneal ring segments
Intracorneal ring segments (ICRS) are extra material implanted in the deep stroma at the corneal mid-periphery changing the corneal curvature and corneal shape. This displaces the local anterior surface creating a steepening of the peripheral cornea and flattening of the central anterior cornea. ICRS can effectively improve visual acuity by reducing refractive error and in improving keratometry. However, it has been unclear how long these effects last and whether patients with ICRS are less likely to go on to keratoplasty.(44-47)
Pinero et al. found that ICRS resulted in an improvement in BCVA (39% at 6 months and 60% at 24 months) as well as a significant decrease in manifest cylinder. There was also a reduction in corneal aberrations (specifically, coma-like aberrations). The cornea was found to be flatter on average at 6 months. However, these effects did not last at 12 months. There are also risks with ICRS implantation. In 6/34 (18%) eyes the rings were explanted; in 3 eyes this was due to visual problems namely loss of BCVA or visual quality and resulting patient dissatisfaction, in the remaining 3 eyes the ring segments either migrated or extruded. In 2/34 (6%) eyes the rings had to be re-positioned to achieve a greater effect.(48) Although early studies have been promising, the above study raises important questions; namely if the regression seen holds in other populations, if so if the regression plateaus or if it progresses until the effect of the procedure is negated. More studies including longitudinal follow up of ICRS will be needed to assess the long-term utility of this procedure
Corneal Cross-Linking (CXL)
Corneal cross-linking (CXL) is a minimally invasive therapeutic modality to halt ectasia progression. CXL has been approved and is being used routinely in Europe and other areas internationally, for both keratoconus and ectasia after LASIK. CXL is still not clinically available in the US, however, as it is still undergoing review by the FDA after recent completion of clinical trials. CXL increases corneal rigidity in biomechanical studies.(49-51)
CXL can halt and possibility reverse ectasia. Various studies have reported on CXL decreasing maximum keratometry readings, stabilizing or reducing refractive error and thus improving both corrected and uncorrected visual acuity; they have also shown initial reduction in mean corneal curvature and flattening of the steepest simulated keratometry readings.(52, 53) Possible complications include keratitis, corneal haze, endothelial cell loss, and failure of treatment. CXL has been shown to have long-term stability with minimal side effects if safety parameters are followed.(15, 49) Some patients with ectasia resulting in severe thinning do not meet current safety guidelines for CXL of a minimum corneal thickness of 400 microns for endothelial safety.(51)
Management strategies can be combined. Yildirim et al. performed a study for 16 eyes combining ICRS and CXL for ectasia after LASIK eyes on the same day. UDVA improved significantly as did CDVA for distance with decreased mean spherical and cylindrical refraction at the last visit (mean 43 months, range 36 to 62 months). Maximum keratometry values also decreased by 6 D on average. There were no serious complications.(54) More studies are necessary to repeat these findings and show longer term results.
CXL can also be combined with photorefractive keratectomy (PRK), topography guided. Studies have shown significant improvement in spherical equivalent, defocus, UCDVA and CDVA, as well as topography for both keratoconic and ectasia after LASIK eyes. The method of choice has been simultaneous PRK followed by CXL, as this has resulted in better outcomes. A variation of PRK has been described in the Cretan protocol. The epithelium is used as a masking agent and removed using transepithelial PTK instead of mechanically, this is followed by CXL. Studies have shown better visual and refractive outcomes with the Cretan protocol. Additional studies are needed to directly compare these two protocols, to repeat these findings described, and to show longer term results.(55)
Invasive Management
Penetrating Keratoplasty (PKP) / Deep Anterior Lamellar Keratoplasty (DALK)
Corneal transplantation is the option of last resort when all aforementioned therapeutic options fail. Luckily, less than 8% of cases fall into this category.(35) PKP for ectasia has excellent outcomes similar to results for keratoconus patients.(56) DALK has replaced PKP as the procedure of choice for keratoconus (and by extrapolation, ectasia) because of excellent visual outcomes with lower risk of transplant rejection.(57)
Melles’ group looked at DALK specifically in ectasia after LASIK patients. They found improved BCVA, decreased keratometry and mean apical keratometry values, and decreased mean keratometric astigmatism. The endothelial cell profile also remained unchanged and there were no major complications. However, 12/20 (60%) eyes required refractive procedures to correct residual ametropia.(58) More studies evaluate the long term consequences of refractive procedures in post-keratoplasty eyes.
CONCLUSION
Ectasia remains a rare yet feared complication of refractive surgery. The presence of a validated risk scoring system and new diagnostic modalities to aide in risk detection will hopefully decrease incidence of ectasia after LASIK.
Many visual rehabilitation options exist. Rigid gas permeable contact lenses and scleral lenses are effective for the majority of cases. Intracorneal ring segments and collagen cross-linking are options in more advanced cases of ectasia and early outcomes are encouraging. The goal of treatments is to minimize invasiveness, halt progression of ectasia, and optimize visual outcomes.
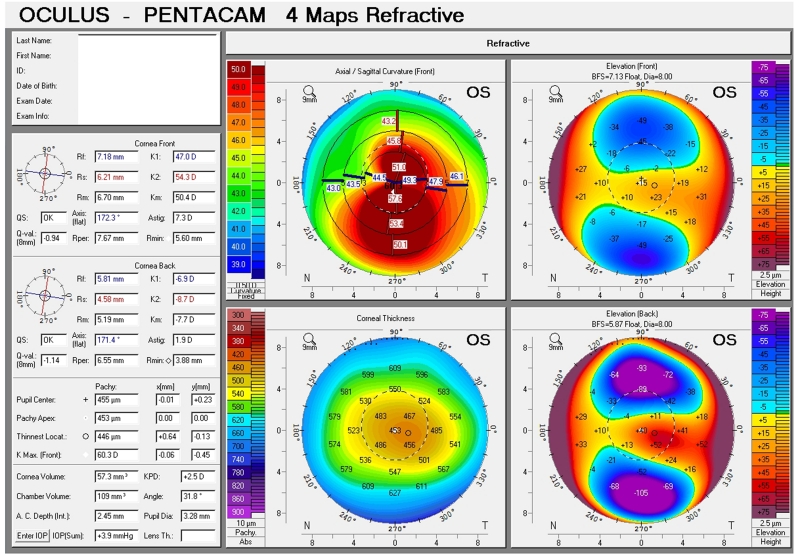
Figure 2. Intermediate ectasia.
There is moderate inferior steepening with a larger area of involvement.
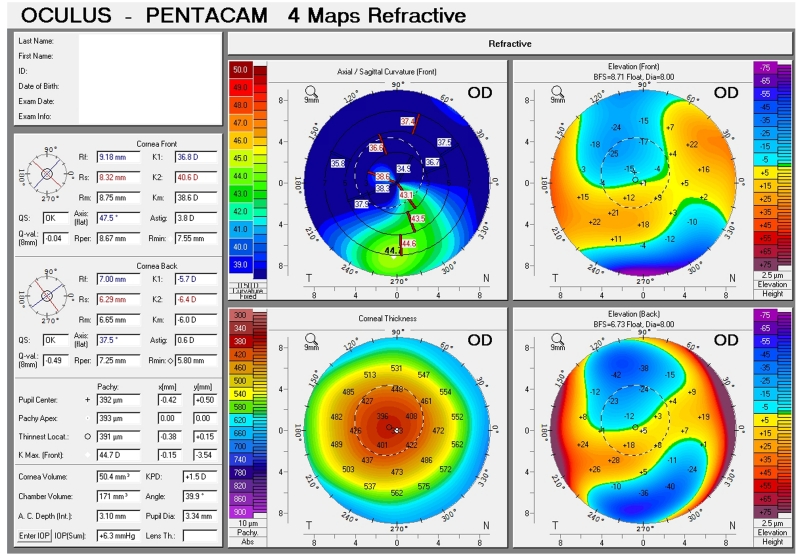
Figure 3. Topography of advanced ectasia.
Marked inferior steepening is noted with the entire inferior cornea and some portions of the superior cornea involved.
Acknowledgments
Financial Support:
JBR: Supported in part by an unrestricted departmental grant to Emory University Department of Ophthalmology from Research to Prevent Blindness, Inc.
MAW: Receives funding from National Eye Institute - Clinician Scientist award - NEI-K23EY023596
Footnotes
Financial Disclosures: None (JBR), None (MAW), None (MAW)
References
- 1.Krachmer JHMM, Holland EJ. Cornea. Elsiever; Mosby: 2010. [Google Scholar]
- 2.Randleman JB, Russell B, Ward MA, Thompson KP, Stulting RD. Risk factors and prognosis for corneal ectasia after LASIK. Ophthalmology. 2003;110(2):267–75. doi: 10.1016/S0161-6420(02)01727-X. [DOI] [PubMed] [Google Scholar]
- 3.Rao SN, Epstein RJ. Early onset ectasia following laser in situ keratomileusus: case report and literature review. Journal of refractive surgery (Thorofare, NJ : 1995) 2002;18(2):177–84. doi: 10.3928/1081-597X-20020301-13. [DOI] [PubMed] [Google Scholar]
- 4.Seiler T, Koufala K, Richter G. Iatrogenic keratectasia after laser in situ keratomileusis. Journal of refractive surgery (Thorofare, NJ : 1995) 1998;14(3):312–7. doi: 10.3928/1081-597X-19980501-15. [DOI] [PubMed] [Google Scholar]
- 5.Seiler T, Quurke AW. Iatrogenic keratectasia after LASIK in a case of forme fruste keratoconus. Journal of cataract and refractive surgery. 1998;24(7):1007–9. doi: 10.1016/s0886-3350(98)80057-6. [DOI] [PubMed] [Google Scholar]
- 6.Geggel HS, Talley AR. Delayed onset keratectasia following laser in situ keratomileusis. Journal of cataract and refractive surgery. 1999;25(4):582–6. doi: 10.1016/s0886-3350(99)80060-1. [DOI] [PubMed] [Google Scholar]
- 7.Lifshitz T, Levy J, Klemperer I, Levinger S. Late bilateral keratectasia after LASIK in a low myopic patient. Journal of refractive surgery (Thorofare, NJ : 1995) 2005;21(5):494–6. doi: 10.3928/1081-597X-20050901-12. [DOI] [PubMed] [Google Scholar]
- 8.Randleman JB, Woodward M, Lynn MJ, Stulting RD. Risk assessment for ectasia after corneal refractive surgery. Ophthalmology. 2008;115(1):37–50. doi: 10.1016/j.ophtha.2007.03.073. [DOI] [PubMed] [Google Scholar]
- 9.Rad AS, Jabbarvand M, Saifi N. Progressive keratectasia after laser in situ keratomileusis. Journal of refractive surgery (Thorofare, NJ : 1995) 2004;20(5 Suppl):S718–22. doi: 10.3928/1081-597X-20040903-18. [DOI] [PubMed] [Google Scholar]
- 10.Pallikaris IG, Kymionis GD, Astyrakakis NI. Corneal ectasia induced by laser in situ keratomileusis. Journal of cataract and refractive surgery. 2001;27(11):1796–802. doi: 10.1016/s0886-3350(01)01090-2. [DOI] [PubMed] [Google Scholar]
- 11.Binder PS, Trattler WB. Evaluation of a risk factor scoring system for corneal ectasia after LASIK in eyes with normal topography. Journal of refractive surgery (Thorofare, NJ : 1995) 2010;26(4):241–50. doi: 10.3928/1081597X-20100212-02. [DOI] [PubMed] [Google Scholar]
- 12.Randleman JB, Trattler WB, Stulting RD. Validation of the Ectasia Risk Score System for preoperative laser in situ keratomileusis screening. American journal of ophthalmology. 2008;145(5):813–8. doi: 10.1016/j.ajo.2007.12.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Klein SR, Epstein RJ, Randleman JB, Stulting RD. Corneal ectasia after laser in situ keratomileusis in patients without apparent preoperative risk factors. Cornea. 2006;25(4):388–403. doi: 10.1097/01.ico.0000222479.68242.77. [DOI] [PubMed] [Google Scholar]
- 14.Ambrosio R, Jr., Dawson DG, Salomao M, Guerra FP, Caiado AL, Belin MW. Corneal ectasia after LASIK despite low preoperative risk: tomographic and biomechanical findings in the unoperated, stable, fellow eye. Journal of refractive surgery (Thorofare, NJ : 1995) 2010;26(11):906–11. doi: 10.3928/1081597X-20100428-02. [DOI] [PubMed] [Google Scholar]
- 15.Amoils SP, Deist MB, Gous P, Amoils PM. Iatrogenic keratectasia after laser in situ keratomileusis for less than −4.0 to −7.0 diopters of myopia. Journal of cataract and refractive surgery. 2000;26(7):967–77. doi: 10.1016/s0886-3350(00)00434-x. [DOI] [PubMed] [Google Scholar]
- 16.Bromley JG, Randleman JB. Treatment strategies for corneal ectasia. Current opinion in ophthalmology. 2010;21(4):255–8. doi: 10.1097/ICU.0b013e32833a8bfe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Holland SP, Srivannaboon S, Reinstein DZ. Avoiding serious corneal complications of laser assisted in situ keratomileusis and photorefractive keratectomy. Ophthalmology. 2000;107(4):640–52. doi: 10.1016/s0161-6420(99)00131-1. [DOI] [PubMed] [Google Scholar]
- 18.Koch DD. The riddle of iatrogenic keratectasia. Journal of cataract and refractive surgery. 1999;25(4):453–4. doi: 10.1016/s0886-3350(99)80027-3. [DOI] [PubMed] [Google Scholar]
- 19.Seiler T. Iatrogenic keratectasia: academic anxiety or serious risk? Journal of cataract and refractive surgery. 1999;25(10):1307–8. doi: 10.1016/s0886-3350(99)00250-3. [DOI] [PubMed] [Google Scholar]
- 20.Randleman JB, Woodward MA. Chapter 4: Evaluation and Diagnosis of Ectasia. In: Hafezi F, Randleman JB, editors. Corneal Collagen Cross-Linking. Slack Incorporated; New Jersey: 2013. pp. 31–8. [Google Scholar]
- 21.Schmack I, Dawson DG, McCarey BE, Waring GO, 3rd, Grossniklaus HE, Edelhauser HF. Cohesive tensile strength of human LASIK wounds with histologic, ultrastructural, and clinical correlations. Journal of refractive surgery (Thorofare, NJ : 1995) 2005;21(5):433–45. doi: 10.3928/1081-597X-20050901-04. [DOI] [PubMed] [Google Scholar]
- 22.Randleman JB, Dawson DG, Grossniklaus HE, McCarey BE, Edelhauser HF. Depth-dependent cohesive tensile strength in human donor corneas: implications for refractive surgery. Journal of refractive surgery (Thorofare, NJ : 1995) 2008;24(1):S85–9. doi: 10.3928/1081597X-20080101-15. [DOI] [PubMed] [Google Scholar]
- 23.Roberts CJ, Dupps WJ., Jr. Biomechanics of corneal ectasia and biomechanical treatments. Journal of cataract and refractive surgery. 2014;40(6):991–8. doi: 10.1016/j.jcrs.2014.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Scarcelli G, Besner S, Pineda R, Yun SH. Biomechanical characterization of keratoconus corneas ex vivo with Brillouin microscopy. Investigative ophthalmology & visual science. 2014;55(7):4490–5. doi: 10.1167/iovs.14-14450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dupps WJ, Jr., Wilson SE. Biomechanics and wound healing in the cornea. Experimental eye research. 2006;83(4):709–20. doi: 10.1016/j.exer.2006.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dawson DG, Randleman JB, Grossniklaus HE, O’Brien TP, Dubovy SR, Schmack I, et al. Corneal ectasia after excimer laser keratorefractive surgery: histopathology, ultrastructure, and pathophysiology. Ophthalmology. 2008;115(12):2181–91.e1. doi: 10.1016/j.ophtha.2008.06.008. [DOI] [PubMed] [Google Scholar]
- 27.Belin MW, Ambrosio R., Jr. Corneal ectasia risk score: statistical validity and clinical relevance. Journal of refractive surgery (Thorofare, NJ : 1995) 2010;26(4):238–40. doi: 10.3928/1081597X-20100318-01. [DOI] [PubMed] [Google Scholar]
- 28.Belin MW, Khachikian SS. New devices and clinical implications for measuring corneal thickness. Clinical & experimental ophthalmology. 2006;34(8):729–31. doi: 10.1111/j.1442-9071.2006.01395.x. [DOI] [PubMed] [Google Scholar]
- 29.Temstet C, Sandali O, Bouheraoua N, Hamiche T, Galan A, El Sanharawi M, et al. Corneal epithelial thickness mapping using Fourier-domain optical coherence tomography for detection of form fruste keratoconus. Journal of cataract and refractive surgery. 2015;41(4):812–20. doi: 10.1016/j.jcrs.2014.06.043. [DOI] [PubMed] [Google Scholar]
- 30.Li Y, Tan O, Brass R, Weiss JL, Huang D. Corneal epithelial thickness mapping by Fourier-domain optical coherence tomography in normal and keratoconic eyes. Ophthalmology. 2012;119(12):2425–33. doi: 10.1016/j.ophtha.2012.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rocha KM, Perez-Straziota CE, Stulting RD, Randleman JB. SD-OCT analysis of regional epithelial thickness profiles in keratoconus, postoperative corneal ectasia, and normal eyes. Journal of refractive surgery (Thorofare, NJ : 1995) 2013;29(3):173–9. doi: 10.3928/1081597X-20130129-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fontes BM, Ambrosio R, Jr., Jardim D, Velarde GC, Nose W. Corneal biomechanical metrics and anterior segment parameters in mild keratoconus. Ophthalmology. 2010;117(4):673–9. doi: 10.1016/j.ophtha.2009.09.023. [DOI] [PubMed] [Google Scholar]
- 33.Randleman JB, Hewitt SM, Lynn MJ, Stulting RD. A comparison of 2 methods for estimating residual stromal bed thickness before repeat LASIK. Ophthalmology. 2005;112(1):98–103. doi: 10.1016/j.ophtha.2004.07.013. [DOI] [PubMed] [Google Scholar]
- 34.Randleman JB. Post-laser in-situ keratomileusis ectasia: current understanding and future directions. Current opinion in ophthalmology. 2006;17(4):406–12. doi: 10.1097/01.icu.0000233963.26628.f0. [DOI] [PubMed] [Google Scholar]
- 35.Woodward MA, Randleman JB, Russell B, Lynn MJ, Ward MA, Stulting RD. Visual rehabilitation and outcomes for ectasia after corneal refractive surgery. Journal of cataract and refractive surgery. 2008;34(3):383–8. doi: 10.1016/j.jcrs.2007.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lim N, Vogt U. Characteristics and functional outcomes of 130 patients with keratoconus attending a specialist contact lens clinic. Eye (London, England) 2002;16(1):54–9. doi: 10.1038/sj.eye.6700061. [DOI] [PubMed] [Google Scholar]
- 37.Dana MR, Putz JL, Viana MA, Sugar J, McMahon TT. Contact lens failure in keratoconus management. Ophthalmology. 1992;99(8):1187–92. doi: 10.1016/s0161-6420(92)31825-1. [DOI] [PubMed] [Google Scholar]
- 38.Ward MA. Contact lens management following corneal refractive surgery. Ophthalmology clinics of North America. 2003;16(3):395–403. doi: 10.1016/s0896-1549(03)00059-2. [DOI] [PubMed] [Google Scholar]
- 39.Nau AC. A comparison of synergeyes versus traditional rigid gas permeable lens designs for patients with irregular corneas. Eye & contact lens. 2008;34(4):198–200. doi: 10.1097/ICL.0b013e31815c859b. [DOI] [PubMed] [Google Scholar]
- 40.Alio JL, Belda JI, Artola A, Garcia-Lledo M, Osman A. Contact lens fitting to correct irregular astigmatism after corneal refractive surgery. Journal of cataract and refractive surgery. 2002;28(10):1750–7. doi: 10.1016/s0886-3350(02)01489-x. [DOI] [PubMed] [Google Scholar]
- 41.Martin R, Rodriguez G. Reverse geometry contact lens fitting after corneal refractive surgery. Journal of refractive surgery (Thorofare, NJ : 1995) 2005;21(6):753–6. doi: 10.3928/1081-597X-20051101-16. [DOI] [PubMed] [Google Scholar]
- 42.Schornack MM, Patel SV. Relationship between corneal topographic indices and scleral lens base curve. Eye & contact lens. 2010;36(6):330–3. doi: 10.1097/ICL.0b013e3181eb8418. [DOI] [PubMed] [Google Scholar]
- 43.Stason WB, Razavi M, Jacobs DS, Shepard DS, Suaya JA, Johns L, et al. Clinical benefits of the Boston Ocular Surface Prosthesis. American journal of ophthalmology. 2010;149(1):54–61. doi: 10.1016/j.ajo.2009.07.037. [DOI] [PubMed] [Google Scholar]
- 44.Uceda-Montanes A, Tomas JD, Alio JL. Correction of severe ectasia after LASIK with intracorneal ring segments. Journal of refractive surgery (Thorofare, NJ : 1995) 2008;24(4):408–11. doi: 10.3928/1081597X-20080401-15. [DOI] [PubMed] [Google Scholar]
- 45.Kymionis GD, Tsiklis NS, Pallikaris AI, Kounis G, Diakonis VF, Astyrakakis N, et al. Long-term follow-up of Intacs for post-LASIK corneal ectasia. Ophthalmology. 2006;113(11):1909–17. doi: 10.1016/j.ophtha.2006.05.043. [DOI] [PubMed] [Google Scholar]
- 46.Pokroy R, Levinger S, Hirsh A. Single Intacs segment for post-laser in situ keratomileusis keratectasia. Journal of cataract and refractive surgery. 2004;30(8):1685–95. doi: 10.1016/j.jcrs.2004.02.050. [DOI] [PubMed] [Google Scholar]
- 47.Guell JL, Velasco F, Sanchez SI, Gris O, Garcia-Rojas M. Intracorneal ring segments after laser in situ keratomileusis. Journal of refractive surgery (Thorofare, NJ : 1995) 2004;20(4):349–55. doi: 10.3928/1081-597X-20040701-08. [DOI] [PubMed] [Google Scholar]
- 48.Pinero DP, Alio JL, Uceda-Montanes A, El Kady B, Pascual I. Intracorneal ring segment implantation in corneas with post-laser in situ keratomileusis keratectasia. Ophthalmology. 2009;116(9):1665–74. doi: 10.1016/j.ophtha.2009.05.030. [DOI] [PubMed] [Google Scholar]
- 49.Yildirim A, Cakir H, Kara N, Uslu H, Gurler B, Ozgurhan EB, et al. Corneal collagen crosslinking for ectasia after laser in situ keratomileusis: long-term results. Journal of cataract and refractive surgery. 2014;40(10):1591–6. doi: 10.1016/j.jcrs.2014.01.042. [DOI] [PubMed] [Google Scholar]
- 50.Hafezi F, Kanellopoulos J, Wiltfang R, Seiler T. Corneal collagen crosslinking with riboflavin and ultraviolet A to treat induced keratectasia after laser in situ keratomileusis. Journal of cataract and refractive surgery. 2007;33(12):2035–40. doi: 10.1016/j.jcrs.2007.07.028. [DOI] [PubMed] [Google Scholar]
- 51.Spoerl E, Mrochen M, Sliney D, Trokel S, Seiler T. Safety of UVA-riboflavin cross-linking of the cornea. Cornea. 2007;26(4):385–9. doi: 10.1097/ICO.0b013e3180334f78. [DOI] [PubMed] [Google Scholar]
- 52.Wollensak G, Spoerl E, Seiler T. Riboflavin/ultraviolet-a-induced collagen crosslinking for the treatment of keratoconus. American journal of ophthalmology. 2003;135(5):620–7. doi: 10.1016/s0002-9394(02)02220-1. [DOI] [PubMed] [Google Scholar]
- 53.Wittig-Silva C, Whiting M, Lamoureux E, Lindsay RG, Sullivan LJ, Snibson GR. A randomized controlled trial of corneal collagen cross-linking in progressive keratoconus: preliminary results. Journal of refractive surgery (Thorofare, NJ : 1995) 2008;24(7):S720–5. doi: 10.3928/1081597X-20080901-15. [DOI] [PubMed] [Google Scholar]
- 54.Yildirim A, Uslu H, Kara N, Cakir H, Gurler B, Colak HN, et al. Same-day intrastromal corneal ring segment and collagen cross-linking for ectasia after laser in situ keratomileusis: long-term results. American journal of ophthalmology. 2014;157(5):1070–6. doi: 10.1016/j.ajo.2014.02.011. [DOI] [PubMed] [Google Scholar]
- 55.Kymionis GD, Grentzelos MA, Portaliou DM, Kankariya VP, Randleman JB. Corneal collagen cross-linking (CXL) combined with refractive procedures for the treatment of corneal ectatic disorders: CXL plus. Journal of refractive surgery (Thorofare, NJ : 1995) 2014;30(8):566–76. doi: 10.3928/1081597X-20140711-10. [DOI] [PubMed] [Google Scholar]
- 56.Pramanik S, Musch DC, Sutphin JE, Farjo AA. Extended long-term outcomes of penetrating keratoplasty for keratoconus. Ophthalmology. 2006;113(9):1633–8. doi: 10.1016/j.ophtha.2006.02.058. [DOI] [PubMed] [Google Scholar]
- 57.Fogla R, Padmanabhan P. Results of deep lamellar keratoplasty using the big-bubble technique in patients with keratoconus. American journal of ophthalmology. 2006;141(2):254–9. doi: 10.1016/j.ajo.2005.08.064. [DOI] [PubMed] [Google Scholar]
- 58.Salouti R, Nowroozzadeh MH, Makateb P, Zamani M, Ghoreyshi M, Melles GR. Deep anterior lamellar keratoplasty for keratectasia after laser in situ keratomileusis. Journal of cataract and refractive surgery. 2014;40(12):2011–8. doi: 10.1016/j.jcrs.2014.04.029. [DOI] [PubMed] [Google Scholar]