The Evaluation Study of Congestive Heart Failure and Pulmonary Artery Catheterization Effectiveness (ESCAPE) trial in 20051 demonstrated that the addition of pulmonary artery (PA) catheterization to standard management in heart failure (HF) did not improve patient outcomes but was associated with an unanticipated increase in adverse events. Consequently, current HF guidelines recommend limiting the use of PA catheters to patients with cardiogenic shock or mechanical ventilation (American College of Cardiology–American Heart Association [ACC-AHA] class I, level of evidence C) and discourage PA catheter use in routine management of HF (ACC-AHA class III, level of evidence B).2 Given these recommendations, we examined contemporary trends in the use of PA catheterization in patients hospitalized with HF.
Methods
Using survey analysis in the National Inpatient Sample,3 we identified 2 492 284 adult patients (aged >18 years) from January 1, 2001, to December 31, 2012, with a primary diagnosis of HF using previously validated codes 428.x, 402.x1, 404.x1, and 404.x3 from the International Classification of Diseases, Ninth Revision, which translate to an estimated 11 888 525 hospitalizations for HF nationally during this period.4 Among these codes, we identified the use of PA catheters with procedure codes 89.63, 89.64, 89.66, 89.67, and 89.685 while excluding hospitalizations in which PA catheterization may have been used for monitoring in a surgical procedure, mechanical circulatory support was used, and right-sided heart catheterization was performed without PA catheter use. The study was approved by the institutional review board of the University of Iowa, which waived the requirement for informed consent because the study used deidentified data.
We analyzed the data from January 1, 2011, through December 31, 2012. We examined calendar-year changes in the use of PA catheters among patients with a primary diagnosis of HF, focusing on the period before (2001–2006) and after (2006–2012) the ESCAPE trial.1 We also examined trends in hierarchical subgroups consisting of cardiogenic shock, requirement of mechanical ventilation without cardiogenic shock, and HF without cardiogenic shock or respiratory failure.
Results
During the study period, we identified 15 786 patients translating to 75 209 HF hospitalizations with PA catheter use nationally (0.6% of all HF hospitalizations). Baseline characteristics of patients undergoing PA catheter placement changed over time, with a decrease in the mean age, incidence of acute myocardial infarction and cardiac arrest, and use of mechanical ventilation (Table).
Table.
Trends in Characteristics for Patients With Use of PA Catheters Among Patients Hospitalized for HF
| Characteristic | Study Yeara |
P Value for Trendb |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | ||
| No. of PA catheters, mean (SD) | 8482 (842) | 7953 (712) | 7302 (573) | 6446 (557) | 5777 (577) | 5278 (507) | 4682 (517) | 4883 (499) | 5739 (848) | 5494 (638) | 6136 (757) | 7035 (486) | |
| No. of catheters per 1000 hospitalizations for HF, mean (SD) | 7.9 (0.8) | 7.6 (0.7) | 6.7 (0.5) | 6.1 (0.5) | 5.7 (0.6) | 5.3 (0.5) | 4.9 (0.5) | 5.2 (0.5) | 5.9 0.(9) | 5.9 (0.7) | 6.5 (0.8) | 7.9 (0.5) | <.001 |
| Patient characteristics | |||||||||||||
| Age, mean (SE), y | 67.2 (0.8) | 67.1 (0.8) | 66.6 (0.6) | 66.6 (0.7) | 66.2 (0.8) | 65.0 (0.8) | 64.0 (0.9) | 62.5 (0.7) | 62.9 (0.7) | 61.1 (0.7) | 63.2 (0.8) | 62.9 (0.5) | <.001 |
| Aged ≥65 y | 62.1 (2.4) | 61.4 (2.4) | 60.0 (2.0) | 58.7 (2.3) | 57.6 (2.4) | 54.6 (2.2) | 49.9 (2.7) | 49.0 (2.4) | 47.3 (2.1) | 43.7 (2.1) | 47.7 (2.3) | 49.0 (1.8) | <.001c |
| Female | 43.2 (1.7) | 43.4 (1.6) | 44.0 (1.6) | 42.3 (1.7) | 42.2 (1.8) | 41.5 (1.7) | 41.2 (2.1) | 37.4 (1.8) | 38.2 (1.5) | 35.0 (1.8) | 37.1 (1.7) | 41.0 (1.6) | <.001c |
| Race | |||||||||||||
| White | 55.1 (3.4) | 47.6 (3.7) | 50.0 (3.6) | 54.5 (3.3) | 47.0 (4.9) | 51.6 (3.4) | 47.4 (3.8) | 48.2 (4.0) | 44.2 (6.4) | 51.4 (3.5) | 57.8 (3.8) | 59.0 (2.2) | <.001d |
| Black | 11.8 (1.7) | 12.0 (1.6) | 10.7 (1.4) | 13.6 (2.2) | 7.5 (1.3) | 15.6 (2.2) | 15.3 (2.7) | 17.6 (2.7) | 15.4 (3.1) | 24.7 (3.3) | 21.4 (2.6) | 25.3 (1.9) | |
| Other | 8.2 (1.3) | 8.4 (1.5) | 9.5 (1.3) | 7.0 (1.2) | 7.2 (1.2) | 9.2 (1.5) | 10.2 (1.5) | 12.6 (1.7) | 10.9 (2.2) | 11.8 (1.7) | 9.6 (1.8) | 11.4 (0.9) | |
| Missing | 24.8 (4.2) | 32.0 (5.1) | 29.7 (4.3) | 25.0 (3.7) | 38.2 (6.0) | 23.6 (3.9) | 27.1 (4.9) | 21.6 (5.6) | 29.4 (9.9) | 12.1 (4.2) | 11.2 (4.9) | 4.3 (1.2) | |
| Secondary cardiovascular discharge diagnoses | |||||||||||||
| Cardiogenic shock | 8.2 (1.0) | 7.6 (0.9) | 8.1 (0.8) | 7.5 (0.7) | 6.9 (1.0) | 7.6 (1.0) | 6.3 (0.9) | 8.7 (0.9) | 11.4 (2.3) | 12.4 (1.4) | 12.4 (1.2) | 14.2 (1.1) | <.001 |
| AMI | 7.6 (0.9) | 7.3 (0.7) | 7.8 (0.8) | 6.9 (0.8) | 5.9 (0.7) | 4.7 (0.7) | 4.2 (0.6) | 4.1 (0.6) | 3.9 (0.5) | 4.5 (0.7) | 4.6 (0.6) | 3.8 (0.7) | <.001c |
| CAD | 48.4 (1.4) | 46.7 (1.3) | 48.8 (1.4) | 45.5 (1.7) | 45.7 (1.9) | 45.6 (1.7) | 46.6 (3.5) | 46.9 (1.9) | 52.2 (1.7) | 47.4 (1.7) | 54.8 (1.7) | 53.7 (1.4) | <.001 |
| Cardiac arrest | 5.5 (0.6) | 3.6 (0.5) | 4.0 (0.6) | 3.8 (0.5) | 3.1 (0.5) | 2.3 (0.5) | 1.9 (0.4) | 2.8 (0.6) | 2.5 (0.4) | 2.6 (0.5) | 2.4 (0.4) | 2.7 (0.4) | <.001c |
| Comorbid conditions | |||||||||||||
| Hypertension | 48.3 (1.7) | 49.6 (2.3) | 50.2 (1.7) | 50.8 (1.9) | 52.8 (2.2) | 54.4 (2.1) | 53.7 (2.6) | 55.7 (2.1) | 64.2 (1.8) | 64.1 (2.4) | 67.3 (2.4) | 70.2 (1.5) | <.001 |
| Diabetes mellitus | 34.2 (1.4) | 34.1 (1.4) | 33.0 (1.6) | 34.0 (1.4) | 35.6 (1.5) | 34.2 (1.9) | 36.1 (1.8) | 36.2 (2.0) | 43.2 (1.4) | 39.0 (2.1) | 41.3 (1.5) | 45.9 (1.4) | <.001 |
| CKD | 6.0 (0.6) | 5.4 (0.6) | 5.9 (0.7) | 4.4 (0.6) | 9.3 (0.9) | 23.2 (1.4) | 37.0 (2.5) | 33.9 (2.2) | 39.9 (1.6) | 42.6 (2.0) | 43.8 (2.0) | 42.2 (1.4) | <.001 |
| Tobacco abuse | 4.1 (0.5) | 4.6 (0.6) | 5.2 (0.7) | 5.0 (0.7) | 5.0 (0.7) | 7.3 (0.9) | 7.5 (1.1) | 9.8 (1.2) | 13.3 (1.5) | 13.4 (1.7) | 17.4 (1.6) | 18.3 (1.4) | <.001 |
| CCI | 1.3 (0.0) | 1.3 (0.0) | 1.3 (0.0) | 1.3 (0.0) | 1.4 (0.0) | 1.4 (0.0) | 1.3 (0.0) | 1.3 (0.0) | 1.3 (0.0) | 1.4 (0.0) | 1.5 (0.0) | 1.5 (0.0) | <.001 |
| History | |||||||||||||
| MI | 10.6 (1.0) | 9.0 (0.8) | 9.6 (0.8) | 9.7 (1.0) | 8.3 (0.9) | 9.9 (1.0) | 10.6 (1.0) | 11.2 (1.0) | 13.4 (1.5) | 12.4 (1.3) | 14.4 (1.2) | 14.4 (1.1) | <.001 |
| CABG | 10.9 (0.8) | 11.7 (0.8) | 11.8 (1.1) | 9.6 (0.9) | 10.1 (1.0) | 11.2 (1.1) | 8.1 (0.9) | 10.5 (1.0) | 13.0 (1.4) | 11.9 (1.2) | 13.4 (1.1) | 14.1 (1.0) | <.001 |
Abbreviations: AMI, acutemyocardial infarction (MI); CABG, coronary artery bypasses graft; CAD, coronary artery disease; CCI, chronic coronary insufficiency; CKD, chronic kidney disease; HF, heart failure; PA, pulmonary artery.
Unless otherwise specified, data are expressed as percentage (SE) of patients.
Calculated for positive trends, unless otherwise stated.
Calculated for negative trend.
Calculated for trends between white vs nonwhite races.
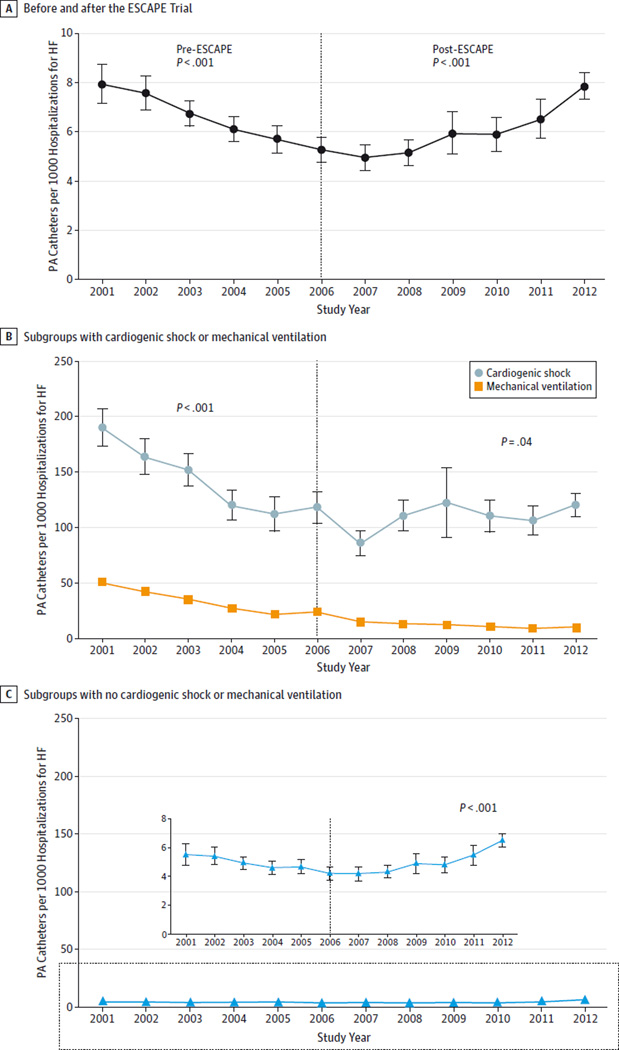
From 2001 to 2007, use of PA catheters initially decreased from 7.9 to 4.9 per 1000 HF hospitalization in 2007, but increased thereafter to 7.9 per 1000 HF hospitalizations in 2012 (Figure). In the subgroup with cardiogenic shock, use of PA catheters dropped from 190 per 1000 in 2001 to 86 per 1000 HF hospitalizations in 2007 (P < .001 for trend) and increased modestly to 121 per 1000 HF hospitalizations in 2012 (P = .04 for trend). Among patients with respiratory failure, use of PA catheters decreased consistently from 50 per 1000 in 2001 to 10 per 1000 HF hospitalizations in 2012. In contrast, among patients without cardiogenic shock or mechanical ventilation requirements, which constituted 74% of all use of PA catheters, their use initially decreased from 5.6 per 1000 admissions in 2001 to 4.2 per 1000 in 2007, followed by a steady increase to 6.5 per 1000 admissions in 2012 (P < .001 for trend).
Figure. Temporal Trends in the Use of Pulmonary Artery (PA) Catheters in Hospitalization for Heart Failure (HF).
A decline in the use of PA catheters is seen in the era before the Evaluation Study of Congestive Heart Failure and Pulmonary Artery Catheterization Effectiveness (ESCAPE) trial (2001–2006) and an increased use of PA catheters in the post-ESCAPE era (2007–2012). Similar use of PA catheters is observed in hierarchical subgroups of patients with HF and cardiogenic shock or with no mechanical ventilation or cardiogenic shock, but not in those with mechanical ventilation without cardiogenic shock, in whom use has continued to decline (P < .001). Dotted vertical line represents publication of ESCAPE trial; error bars, SEs for national estimates. P values are calculated for trend. Inset graph in part C shows the trend plot with a smaller scale.
Discussion
In a national sample of hospitalizations for HF, we found a significant decline in the use of PA catheters from 2001 through 2007, consistent with findings previously reported by Wiener and Welch5 and in agreement with other studies questioning the usefulness of PA catheterization.6 In contrast, despite evidence against routine use in HF in the ESCAPE trial, we observed a significant increase in the use of PA catheters in HF management in recent years. Moreover, the largest increase is seen in patients without a definite indication. This finding highlights the discordance between guideline recommendations and current clinical practice regarding management of acute HF.
Several factors may explain the observed increase in the use of PA catheters in recent years. These factors include increasing use of advanced HF therapies and the preparatory hemodynamic evaluations and increasing prevalence of co-morbidities such as pulmonary hypertension and chronic kidney disease that may prompt invasive assessment of volume status.7 Future studies are needed to determine whether a proportion of the increase in the use of PA catheters among patients with HF is attributable to inappropriate overuse.
Acknowledgments
Dr Fonarow reports receiving research support from the Agency for Healthcare Research and Quality and the National Institutes of Health and serving as a consultant for Amgen, Bayer, Gambro, Novartis, and Medtronic.
Footnotes
Author Contributions: Drs Pandey and Khera had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Pandey, Khera, Golwala, Fonarow.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Pandey, Khera.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Pandey, Khera, Kumar.
Administrative, technical, or material support: Fonarow.
Study supervision: Fonarow.
Conflict of Interest Disclosures: No other disclosures were reported.
References
- 1.Binanay C, Califf RM, Hasselblad V, et al. ESCAPE Investigators and ESCAPE Study Coordinators. Evaluation Study of Congestive Heart Failure and Pulmonary Artery Catheterization Effectiveness: the ESCAPE trial. JAMA. 2005;294(13):1625–1633. doi: 10.1001/jama.294.13.1625. [DOI] [PubMed] [Google Scholar]
- 2.Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013;128(16):1810–1852. doi: 10.1161/CIR.0b013e31829e8807. [DOI] [PubMed] [Google Scholar]
- 3.Khera R, Cram P, Lu X, et al. Trends in the use of percutaneous ventricular assist devices: analysis of National Inpatient Sample data, 2007 through 2012. JAMA Intern Med. 2015;175(6):941–950. doi: 10.1001/jamainternmed.2014.7856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.American Heart Association. American Stroke Association. GetWith the Guidelines–Heart Failure fact sheet. [Accessed June 6, 2015]; http://www.heart.org/idc/groups/heart-public/@private/@wcm/@hcm/@gwtg/documents/downloadable/ucm_310967.pdf. Published October 2013. [Google Scholar]
- 5.Wiener RS, Welch HG. Trends in the use of the pulmonary artery catheter in the United States, 1993–2004. JAMA. 2007;298(4):423–429. doi: 10.1001/jama.298.4.423. [DOI] [PubMed] [Google Scholar]
- 6.Reade MC, Angus DC. PAC-Man: game over for the pulmonary artery catheter? Crit Care. 2006;10(1):303. doi: 10.1186/cc3977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Loh JC, Creaser J, Rourke DA, et al. Temporal trends in treatment and outcomes for advanced heart failure with reduced ejection fraction from 1993–2010: findings from a university referral center. Circ Heart Fail. 2013;6(3):411–419. doi: 10.1161/CIRCHEARTFAILURE.112.000178. [DOI] [PMC free article] [PubMed] [Google Scholar]