Abstract
Background
Endometriosis has been associated with a lean body habitus. However, we do not understand whether endometriosis is also associated with other characteristics of adiposity, including adipose tissue distribution and amount of visceral adipose tissue (VAT; adipose tissue lining inner organs). Having these understandings may provide insights on how endometriosis develops—some of the physiologic actions of adipose tissue differ depending on tissue amount and location, and are related to proposed mechanisms of endometriosis development.
Objectives
To review the literature regarding overall adiposity, adipose tissue distribution and/or VAT, and endometriosis.
Methods
We reviewed and synthesized studies indexed in PubMed and/or Web of Science. We included studies that had one or more measures of overall adiposity, adipose tissue distribution, and/or VAT, and women with and without endometriosis for comparison. We summarized the findings and commented on the methods used and potential sources of bias.
Results
Out of 366 identified publications, 19 (5.2%) were eligible. Two additional publications were identified from reference lists. Current research included measures of overall adiposity (e.g., body figure drawings) or adipose tissue distribution (e.g., waist-to-hip ratio), but not VAT. The weight of evidence indicated that endometriosis was associated with low overall adiposity and with a preponderance of adipose tissue distributed below the waist (peripheral).
Discussion
Endometriosis may be associated with being lean or having peripherally distributed adipose tissue. Well-designed studies with various sampling frameworks and precise measures of adiposity and endometriosis are needed to confirm associations between adiposity measures and endometriosis, and delineate potential etiologic mechanisms underlying endometriosis.
Keywords: adiposity, body size, endometriosis, systematic review
Endometriosis is a chronic women’s health problem that affects at least 10%-11% of reproductive age women (Buck Louis et al., 2011; Olive & Schwartz, 1993). It is defined by the presence of uterine endometrial glands and stroma located outside of the uterine cavity (Burney & Giudice, 2012; Rogers et al., 2013). Endometriosis is diagnosed via surgical visualization (Scholefield, Sajjad, & Morgan, 2002) with or without histologic confirmation. Severity of disease is described as stages I (minimal), II (mild), III (moderate), and IV (severe) depending on the location, size, and depth of endometrial implants and related operative findings such as adhesions (Canis et al., 1997; Practice Committee of the American Society for Reproductive Medicine [ASRM], 2012). Compared to women without endometriosis, women with the disease experience a 20% reduction in quality-adjusted life years (Simoens et al., 2012) and have greater risk for certain cancers (Melin, Sparén, Persson, & Bergqvist, 2006; Pearce et al., 2012). The societal and economic costs of endometriosis are estimated to be about $70 billion annually for both in- and out-patient medical costs and indirect costs associated with reduced productivity.
The natural history of endometriosis remains unknown despite this being an active area of research. Historically, endometriosis was thought to arise after the onset of menses from retrograde menstruation. This is the theory that endometrial tissue spreads outside the uterus when menstrual fluid flows back through the fallopian tubes during menstruation (Sampson, 1927). There are no definitive data that retrograde menstruation occurs more in women with than without endometriosis (D’Hooghe & Debrock, 2002; Halme, Hammod, Hulka, Raj, & Talbert, 1984). Recently, researchers have posited that endometriosis may have fetal origins (Signorile et al., 2010), further complicating our understanding of the natural history of the disease. To better understand the etiology and risk factors for endometriosis, researchers are searching for endometriosis biomarkers —”objective, quantifiable characteristics of biological processes” (Strimbu & Tavel, 2010, p. 2). While this is an active area of research, investigators have yet to definitively identify endometriosis biomarkers (Borrelli, Abrão, & Mechsner, 2014; Fassbender et al., 2013; Fassbender, Burney, Dorien, D’Hooghe, & Giudice, 2015; May et al., 2010; May, Villar, Kirtley, Kennedy, & Becker, 2011).
Complicating understanding of endometriosis is its symptomatology. Key endometriosis symptoms include menstrual irregularities, chronic pelvic pain, dyspareunia, or dysmenorrhea difficulty conceiving (Burney & Giudice, 2012; Murphy, 2002; Practice Committee of the ASRM, 2012). However, many of these endometriosis symptoms are associated with other gynecologic disorders. Moreover, not all women with endometriosis are symptomatic. Although health practitioners often initiate diagnostic workups based on symptoms (Ballard, Lowton, & Wright, 2006), evidence does not support this practice (Eskenazi & Warner, 1997; Vercellini et al., 2007).
Some research findings suggest that endometriosis is associated with lean body habitus as measured by body mass index (BMI) (Viganò et al., 2012). However, BMI is a proxy of adiposity, reflecting overall body mass rather than adipose tissue mass. In addition, BMI does not reflect the distribution of body fat (Deurenberg, Yap, & van Staveren, 1998; Shah & Braverman, 2012). Better understanding of which aspects of adiposity may be associated with endometriosis are needed in order to identify etiologic or mediating pathways associated with adiposity and endometriosis. For instance, some research findings suggest that adipose tissue has immunologic properties (Rasouli & Kern, 2008; Schäffler, Schölmerich, & Salzberger, 2007; Waki & Tontonoz, 2007). The immunologic properties of adipose tissue are known to differ depending on tissue type and location (Ibrahim, 2010; Vatier et al., 2012). It is possible that the immunologic properties of adipose tissue may be involved in or impacted by the development of endometriosis. Endometriosis may arise due to altered immunologic functioning (Committee on Practice Bulletins—Gynecology, 2010; Practice Committee of the ASRM, 2012; Rocha, Reis, & Taylor, 2013). This altered functioning may include the promotion or inhibition of inflammation (Kobashi et al., 2005; Mandal, Pratt, Barnes, McMullen, & Nagy, 2011; Ouchi et al., 2000) and stimulation of angiogenesis (Adya, Tan, Chen, & Randeva, 2012; Cao, Brakenhielm, Wahlestedt, Thyberg, & Cao, 2001). One potential link among immunity, endometriosis, and adiposity is M2 phenotype macrophages. These macrophages, which are anti-inflammatory and promote tissue regeneration at injury sites (Murray & Wynn, 2011), have been implicated in the development of endometriosis (Smith, Pearson, Hachey, Xia, & Wachtman, 2012; Wang et al., 2014; Wang et al., 2015). These macrophages are also associated with leanness in mice (Lumeng, Bodzin, & Saltiel, 2007). If links exist among adiposity-related immunity, quantity and location of adipose tissue, and endometriosis, it could be possible to identify diagnostic markers of endometriosis that combine adiposity measures with biomarkers.
Purpose
The purpose of our systematic review is to summarize the literature describing observational studies in which researchers included women with—or at risk for—endometriosis and measures of endometriosis and adiposity inclusive of overall adiposity, adipose tissue distribution, and visceral adipose tissue (VAT). We defined overall adiposity as the total adipose tissue on people’s bodies, adipose tissue distribution as the location of adipose tissue across the body, and VAT as the amount of adipose tissue that lines the inner organs.
Methods
Study Selection
We deemed publications eligible for review if they had been published before January 22, 2014 and met our inclusion criteria: (a) reported findings from observational studies; (b) included one or more measures of adiposity; and (c) included both women with and without endometriosis. Endometriosis could have been diagnosed by physicians during the studies or reported by participants as being diagnosed with endometriosis by a physician. We retained studies in which (a) researchers recruited small samples of women, (b) adiposity measures were self-reported, and (c) women were assessed for endometriosis using methods other than the clinical gold standard of visualized disease (Practice Committee of the ASRM, 2012). We did this to minimize selection bias and provide a comprehensive summary of the current literature available to researchers and health practitioners.
We excluded experimental research studies because many participants would have been taking medications which may alter the amount and distribution of adipose tissue (Bruce et al., 1991). Publications in which authors only reported BMI without also reporting weights and heights were excluded because we did not have original data to review. In addition, we excluded studies in which researchers only assessed BMI as an adiposity measure; Viganò et al. (2012) recently completed a review on associations between BMI and endometriosis; to complement their work, we chose to review studies based on measures of adiposity other than BMI.
Search Strategy
We conducted searches in PubMed and Web of Science using a predetermined list of search terms (see Table, Supplemental Digital Content 1). We uploaded citations into Reference Manager (v. 11). After full-text review, we verified that the studies we planned to include did meet our eligibility criteria. We also checked reference lists to identify additional publications.
Reporting Procedure
We used the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement (prisma-statement.org) to guide our reporting. We abstracted the following data from each publication: design; sample; description of comparison group, criteria for assessing adiposity and diagnosing endometriosis; methods that researchers used to improve internal validity in their designs; and results. We identified limitations and (dis)similarities across studies we reviewed. We reported: (a) differences either in means for continuous variables or in proportions for ordinal variables from bivariate analyses; (b) odds ratios (ORs) and 95% confidence intervals (CIs) for findings from cross-sectional case control studies; and (c) rate ratios (RR) and 95% CIs for findings from prospective cohort studies. Because none of the studies that we identified included findings on VAT, we report findings based on measures of overall adiposity and/or adipose tissue.
Results
Eligible Studies
The complete process of identifying eligible publications is shown in a figure (see Supplemental Digital Content 2). After removing duplicates, we vetted 366 unique publications. We excluded 347 (94.8%) publications because they failed to meet inclusion criteria; 19 publications (5.2%) met these criteria. With two additional publications we found from reference lists, a total of 21 publications were available for this review. Of the 21 publications, 18 (85.7%) were described as case control studies. Three of the 21 were based on data from a single, prospective cohort study which was the Nurses’ Health Study II (NHSII) (see Tables 1 and 2 for references).
TABLE 1.
Case-Control Studies: Study Characteristics
| Setting | n | Age | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Studya | Year | Location | Clinic type | Case | Control | Group | Inclusionb | M | (SD) | Parityc |
| Ayas | 2012 | Turkey | Hospital OB-GYN | 36 | 37 | Case | Laparotomy/laparoscopy | 32.4 | (5.7) | 1.0 (1.3) |
| Control | Same as cases | 30.5 | (5.8) | 0.9 (1.1) | ||||||
| Bedaiwy | 2006 | USA | Tertiary hospital | 60 | 48 | Case | Laparoscopyd | 33.0 | (5.5) | 0.6 (0.9) |
| Control-1 | Laparoscopyd,e | 31.3 | (3.6) | 0.3 (0.6) | ||||||
| Control-2 | Laparoscopyd,f | 33.6 | (5.9) | 1.6 (1.1) | ||||||
| Cramer | 1986 | USA, Canada |
Infertility centers | 268 | 3794 | Case | Infertility evaluation | --m | --m | 9.2 |
| Control | Delivery of live-born child, no infertility history |
--m | --m | 100.0 | ||||||
| Darrow | 1994 | USA | Endometriosis center |
104 | 198 | Case | New endometriosis diagnosis, age 19–45 years, New York state residents, English speaking |
--n | --n | -- |
| Control-1 | Friend of case | --n | --n | -- | ||||||
| Control-2 | Clinic patientg | --n | --n | -- | ||||||
| Ferrero | 2005 | Italy | Hospital OB-GYN | 366 | 248 | Case | Laparoscopyh | 33.3 | (4.6) | 24.9 |
| Control | 34.7 | |||||||||
| Hediger | 2005 | USA | Hospitals | 32 | 52 | Case | Laparoscopyi, age 18–40 years |
32.7 | (4.4) | 15.6 |
| Control | 31.6 | (5.0) | 50.0 | |||||||
| Kvaskoff | 2009 | France | n/a | 4241 | 92,974 | Case | Age 40–65 years, insured by national health plan |
-- | -- | -- |
| Control | -- | -- | -- | |||||||
| Pillet | 2012 | France | Hospital OB-GYN | 238 | 238 | Case | Laparotomy/laparoscopyh age <42 years |
31.5 | (5.3) | 0.2 (0.6) |
| Control | 31.4 | (5.2) | 0.5 (1.0) | |||||||
| Matalliotakis | 2008 | USA | Hospital OB-GYN | 535 | 200 | Case | Laparotomy/laparoscopyk,l | 34.3 | (6.5) | 35.3 |
| Control | Infertility, surgical evaluation |
34.4 | (4.4) | 33.5 | ||||||
| McCann | 1993 | USA | Endometriosis center |
88 | 88 | Case | Age 19–45 years, laparoscopy-diagnosed endometriosis within 1 year of interview, White, English speaking |
29.4 | (4.7) | -- |
| Control | Friends of cases, not biologically related, no endometriosis, within 2 years of case friend not patients at the center |
29.4 | (4.6) | -- | ||||||
| Nagle | 2009 | Australia | n/aj | 268 | 244 | Case | Enrolled in Endogene Study, no family history of endometriosis, diagnosed with stage III/IV endometriosis |
36.4 | (7.1) | -- |
| Control | Enrolled on Australian Twin Registry |
36.3 | (7.6) | -- | ||||||
| Pandey | 2010 | India | Hospital OB-GYN | 15 | 35 | Case | Laparoscopyl, age 18–45 years, infertility |
29.3 | (5.2) | -- |
| Control | 30.1 | (3.1) | -- | |||||||
| Rico | 1993 | No description | 28 | 33 | Case | Laparoscopyl | 31.9 | (1.6) | -- | |
| Control | 32.7 | (6.0) | -- | |||||||
| Sahmani | 2013 | Iran | Surgical hospital | 97 | 107 | Case | Laparoscopyk,l, age 18–42 years, chronic pelvic pain or infertility |
29.5 | (5.5) | -- |
| Control | Laparoscopyk,l | 29.8 | (4.5) | -- | ||||||
| Savaris | 2011 | Brazil | Endometriosis clinic |
25 | 20 | Case |
Laparoscopy |
27.1 | (4.6) | -- |
| Control | 28.9 | (4.5) | -- | |||||||
| Signorello | 1997 | USA | Surgical hospital | 50 | 136 | Case | Pelviscopy/laparoscopy, English speaking, age 23- 44 years, infertility or history of miscarriages |
--o | --o | -- |
| Control-1 | --o | --o | -- | |||||||
| Control-2 | Laparoscopic tubal ligation | --m | --m | -- | ||||||
| Vercellini | 2013 | Italy | Hospital OB-GYN | 200 | 100 | Case-1 | Laparotomy/laparoscopyh | 32.1 | (4.0) | -- |
| Case-2 | 32.1 | (3.8) | -- | |||||||
| Control | 32.1 | (3.8) | -- | |||||||
| Yi | 2010 | Hospital OB-GYN | 48 | 36 | Case | Pelvic surgical procedureh,k, l | 36.5 | (1.0) | -- | |
| Control | 37.8 | (1.0) | -- | |||||||
Note. hx = history; OB-GYN = obstetrics-gynecology; SD = standard deviation; US = United States.
First author last name only.
Inclusion criteria as described in the publications.
Mean (SD) or percent parous.
For chronic pelvic pain, infertility, tubal ligation, or sterilization reversal.
10 controls with idiopathic infertility.
38 controls undergoing tubal ligation or reanastomosis.
Condition other than endometriosis.
For benign gynecological conditions.
For diagnosis or tubal sterilization.
Most participants were recruited from the general population and a smaller number were referred from endometriosis associations and collaborating gynecologists (Treloar et al., 2002).
For pelvic pain.
For infertility.
Majority of cases and controls age 30–34 years.
Majority of cases, friend controls, and medical controls age <30 years.
Majority of cases and infertile controls age 30–34 years and fertile controls age 35–39 years.
TABLE 2.
Nurses’ Health Study II Publications: Study Characteristicsa
| Sample | ||||
|---|---|---|---|---|
| Studyb | Year | Incident cases | N | Characteristics |
| Missmer | 2004 | 1,721c | 90,065 | • None provided |
| Shah | 2013 | 5,504d | 101,074 | • Majority White (>91%) |
| • Age: mean in the 30s | ||||
| Vitonis | 2010 | 1,817c | 87,603 | • Majority parous |
| • Age: mean early–mid 30s | ||||
| •Parity: mean about 2 | ||||
NoteResearchers used data from the Nurses’ Health Study II, a prospective cohort study (www.channing.harvard.edu/nhs/).
First author last name shown.
No infertility history or evaluated for infertility at time of laparoscopy.
Fertile or infertile.
Study Characteristics
Participants in case control studies were recruited predominantly from clinical sites. Participants in the NHSII study were recruited from the general population across 14 states and included nurses 25–42 years of age. Information about case control and prospective cohort study participants is provided in Tables 1 and 2, respectively.
Researchers used a variety of measures to assess overall adiposity and/or adipose tissue distribution (Tables 3 and 4). In 16 of 21 publications (76.2%), researchers included studies that included overall adiposity measures such as: weight; percentage body fat; body silhouettes, which included eight visual representations of overall adiposity from lowest amount (score = 1) to greatest amount (score = 9) across the life course; and Stunkard body figures (Stunkard, Sørenson, & Schulsinger, 1983), which are nine graded visual representations of overall adiposity from underweight to obese. In eight of the 21 publications (38.1%), researchers described studies that included measures of adipose tissue distribution. These measures included skinfold thicknesses, body circumferences, or circumference-based ratios (e.g., waist-to-hip).
TABLE 3.
Case-Control Studies: Measurement of Adiposity and Endometriosis
| Adiposity |
Endometriosis |
|||||
|---|---|---|---|---|---|---|
| Studya | Year | Type | Measures | Procedure | Cases | Controls |
| Ayas | 2012 | Overall | Weight Percentage body fat |
TANITA analyzerb | Laparotomy/laparoscopy | Same as cases |
| Bedaiwy | 2006 | Overall | Weight | No description | Laparotomy | Same as cases |
| Cramer | 1986 | Overall | Weight | No description | Laparotomy/laparoscopy | Unclear |
| Darrow | 1994 | Overall | Weight: usual adult Weight: maximum ever |
Self-report | Laparoscopy | Unclear |
| Distribution | Waistc Hipc Thighc |
No description | ||||
| Ferrero | 2005 | Overall | Weight | Chart extractiond | Laparoscopye | Same as cases |
| Hediger | 2005 | Overall | Weight Adult weight (minimum) Adult weight (maximum) SBFS |
Self-report | Laparoscopy | Same as cases |
| Kvaskoff | 2009 | Overall | Body silhouettef | Self-reportg | Self-reporth | Same as cases |
| Pillet | 2012 | Overall | Weight | Self-reporti | Laparotomy/laparoscopyj | Same as cases |
| Matalliotakis | 2008 | Overall | Weight | Chart extractiond | Laparoscopye | Same as cases |
| McCann | 1993 | Overall | Weight | Self-report | Laparoscopy | Unclear |
| Distribution | Waist circumference Hip circumference Left thigh circumference Waist-to-hip ratio Waist-to-thigh ratio |
Investigator-using calibrated tape measure |
||||
| Nagle | 2009 | Overall | Relative weightk | Self-report | Surgically confirmedl | Unclear |
| Pandey | 2010 | Overall | Weight | No description | Laparoscopyj | Same as cases |
| Rico | 1993 | Overall | Weight | No description | Clinical data Laparoscopic data |
Unclear |
| Sahmani | 2013 | Distribution | Waist circumference | No description | Laparoscopy/laparotomy | Same as cases |
| Savaris | 2011 | Overall | Body densitym Fat percentageo |
No description | Videolaparoscopyj,n | Unclear |
| Distribution | Skinfoldsp | Harpenden adipometer | ||||
| Signorello | 1997 | Overall | Weight | Self-reportd | Surgical confirmationl | Same as cases |
| Vercellini | 2013 | Distribution | Waist-to-hip ratio Breast-to-underbreast ratio |
Trained physician- measured before surgery |
Pelvic visualization at surgery |
Pelvic visualization at surgery/histology |
| Yi | 2010 | Overall | Weight | No description | Laparoscopy or histology | Same as cases |
| Distribution | Waist circumference Hip circumference Waist-to-hip ratio |
Waist: at minimal girth Hip: at maximum of buttocks |
||||
Note. SBFS = Stunkard Body Figure Scale (9 figures).
First author last name.
Measurements taken around surgery, between day 4 and 10 of women’s menstrual cycle; women assessed with empty bladders after 8 hours fasting; foot-to-foot TANITA body composition analyzer BC-420MA (Japan) was used.
What the measures were e.g., circumference) was not described.
No information about how or when weight and height were gathered.
Chart extraction of findings.
At puberty, ages 20–25 and 35–40 years.
Questionnaire included body figure drawings from 1 = leanest to 8 = largest.
Self-report of treatment for or diagnosis of endometriosis.
Weight obtained via interview conducted by surgeon one month before surgery.
Histologically confirmed.
Under-weight, average weight, or over-weight at age 10 and 16 years.
Detail not provided.
Petroski equation for women 18–51 years.
Visualization of implants.
Siri formula.
Tricipital, subscapular, suprailiac, and calf.
TABLE 4.
Nurses’ Health Study II Publications: Measures of Adiposity and Endometriosisa
| Studyb | Year | Adiposity | Endometriosis |
|---|---|---|---|
| Missmer | 2004 | Distribution Waist circumferencec Hip circumferencec |
Laparoscopically- confirmed |
| Shah | 2013 | Distribution Waist circumferencec Hip circumferencec |
Physician- diagnosed |
| Vitonis | 2010 | Overall Body sized |
Laparoscopically- confirmed |
NoteResearchers used data from the Nurses’ Health Study II, a prospective cohort study (www.channing.harvard.edu/nhs/).
First author last name shown.
Self-measurements obtained using an investigator-provided tape measure and instructions.
Questionnaire with Stunkard figures for ages 5, 10, and 20 years.
Study Findings
In 13 of the 21 publications, researchers reported bivariate analyses between one or more measures of overall adiposity and endometriosis. In five of the 13 publications (38.5%), researchers found inverse associations between overall adiposity and endometriosis. In nine of the 13 publications (69.2%), researchers did not observe any such association (Table 5). In five of the 21 publications, researchers reported bivariate analyses between one or more measures of peripheral adipose tissue distribution and endometriosis. In two of the five publications (40.0%), researchers found a positive association between peripheral adiposity measures and endometriosis. In all five publications, researchers found no such association. In five publications of the 21 publications, researchers controlled for potentially confounding variables when assessing associations between endometriosis and overall adiposity. (See Table 6 for findings from case control studies. See Table 7 for findings from NHSII publications.) In three of these five publications (60.0%), researchers reported inverse relationships between endometriosis and at least one overall adiposity measure. In one of the five publications (20.0%), researchers reported a positive relationship, while in two publications (40.0%) researchers reported no relationship. In three of the 21 publications, researchers controlled for potential confounders when assessing associations between endometriosis and one or more measures of peripheral adipose tissue distribution (e.g., low waist-to-hip ratio). In two of the three publications (66.7%), researchers found association between endometriosis and adipose tissue distribution. In all three publications, researchers reported no association between other adipose distribution measures. Among Nurses’ Health Study II participants, there was an inverse relationship between adjusted risk of endometriosis and body size perception at age 20 (but not ages 5 or 10) among nulliparous women, who had a greater risk compared to parous women (Vitonis, Baer, Hankinson, Laufer, & Missmer, 2010).
TABLE 5.
Case-Control Studies: Association of Adiposity with Endometriosis from Bivariate Analyses
| Studya | Year | Adiposity measure (units) | Cases | Controls | p< .05b |
|---|---|---|---|---|---|
| Ayas | 2012 | Weight (kg), M (SD) | 29.95 (8.02) | 26.87 (7.55) | No |
| Percent body fat (%),M (SD) | 20.78 (9.19) | 17.35 (7.1) | No | ||
| Bedaiwy | 2006 | Weight (kg), M (SD) | 65.2 (12.6) | G1: 83.9 (40.2) G2: 72.1 (14.7) |
No No |
| Ferrero | 2005 | Weight (kg), M (SD) | 57.2 (8.0) | 58.8 (10.0) | Yes |
| Hediger | 2005 | Weight (lb), M (SD) | |||
| At time of study | 143.4 (28.8) | 158.9 (38.6) | Yes | ||
| Minimum adult weight | 119.9 (17.8) | 125.3 (26.3) | No | ||
| Maximum adult weight | 157.8 (36.8) | 167.3 (41.4) | No | ||
| Kvaskoff | 2009 | Body silhouette, n (%) | |||
| At puberty | |||||
| 1 | 991 (23.4) | 19 715 (21.2) | Yes | ||
| 2 | 1511 (35.6) | 33 084 (35.6) | No | ||
| 3 | 937 (22.1) | 21 261 (22.9) | No | ||
| 4 | 594 (14.0) | 13 920 (15.0) | No | ||
| ≥5 | 208 (4.9) | 4994 (5.3) | No | ||
| At 20–25 years old | |||||
| 1 | 477 (11.3) | 9225 (9.9) | Yes | ||
| 2 | 1906 (44.9) | 40 756 (43.8) | No | ||
| 3 | 1357 (32.0) | 30 184 (32.5) | No | ||
| 4 | 391 (9.2) | 9958 (10.7) | No | ||
| ≥5 | 110 (2.6) | 2851 (3.1) | No | ||
| At 35–40 years old | |||||
| 1 | 149 (3.5) | 3428 (3.7) | No | ||
| 2 | 1203 (28.4) | 25 112 (27) | No | ||
| 3 | 1889 (44.5) | 41 265 (44.4) | No | ||
| 4 | 740 (17.5) | 17 112 (18.4) | No | ||
| ≥5 | 260 (6.1) | 6057 (6.5) | No | ||
| Pillet | 2012 | Weight (kg), M (SD) | 59.1 (9.8) | 63.6 (11.3) | Yes |
| Matalliotakis | 2008 | Weight (kg), M (SD) | 66.5 (14.0) | 70.9 (17.9) | Yes |
| McCann | 1993 | Weight (kg), M (SD) | |||
| All participants | 58.9 (8.3) | 59.1 (9.0) | No | ||
| < 30 years old | 57.5 (7.8) | 59.0 (10.7) | No | ||
| ≥ 30 years old | 60.4 (9.6) | 59.2 (6.8) | No | ||
| Waist circumference (cm), M (SD) | |||||
| All participants | 72.2 (8.0) | 73.4 (9.1) | No | ||
| < 30 years old | 70.5 (7.8) | 74.0 (10.3) | No | ||
| ≥ 30 years old | 74.0 (7.8) | 72.8 (7.7) | No | ||
| Hip circumference (cm), M (SD) | |||||
| All participants | 100.3 (8.4) | 98.6 (10.7) | No | ||
| < 30 years old | 98.5 (7.3) | 98.3 (12.1) | No | ||
| ≥ 30 years old | 102.3 (9.1) | 98.9 (9.0) | No | ||
| Thigh circumference (cm), M (SD) | |||||
| All participants | 57.2 (5.2) | 57.2 (6.2) | No | ||
| 30 years old | 55.9 (4.0) | 57.1 (7.0) | No | ||
| ≥ 30 years old | 58.5 (6.1) | 57.4 (5.3) | No | ||
| Waist/hip ratio, M (SD) | |||||
| All participants | 0.72 (0.04) | 0.75 (0.06) | Yes | ||
| < 30 years old | 0.72 (0.04) | 0.76 (0.06) | Yes | ||
| ≥ 30 years old | 0.72 (0.04) | 0.74 (0.06) | No | ||
| Waist/thigh ratio, M (SD) | |||||
| All participants | 1.26 (0.09) | 1.29 (0.12) | No | ||
| < 30 years old | 1.26 (0.10) | 1.30 (0.11) | No | ||
| ≥ 30 years old | 1.27 (0.07) | 1.27 (0.13) | No | ||
| Pandey | 2010 | Weight (kg), M (SD) | 55.3 (4.4) | 57.6 (7.6) | No |
| Rico | 1993 | Weight (kg), M (SD) | 57.8 (7.1) | 58.3 (7.5) | No |
| Sahmani | 2013 | Waist circumference (cm), M (SD) | 81.2 (9.7) | 80.6 (9.1) | No |
| Savaris | 2011 | Body fat percent > 23% (%) | (84) | (65) | No |
| Vercellini | 2013 | Waist/hip ratio (tertiles), n (%) | |||
| <0.7 | RV: 19 (19) P/O: 16 (16) |
12 (12) | No No |
||
| 0.7–0.8 | RV: 53 (53) P/O: 56 (56) |
51 (51) | No No |
||
| >0.8 | RV: 28 (28) P/O: 28 (28) |
37 (37) | No No |
||
| Breast/underbreast ratio (tertiles), n(%) | |||||
| < 1.1 | RV: 16 (16) P/O: 24 (24) |
21 (21) | Yes | ||
| 1.1–1.2 | RV: 60 (60) P/O: 66 (66) |
71 (71) | No No |
||
| > 1.2 | RV: 24 (24) P/O: 10 (10) |
8 (8) | No No |
||
| Yi | 2010 | Weight (kg), M (SD) | 55.3 (1.0) | 59.6 (1.4) | Yes |
| Waist circumference (cm), M (SD) | 75.5 (1.0) | 79.1 (1.2) | Yes | ||
| Hip circumference (cm), M (SD) | 90.9 (0.8) | 93.0 (0.9) | No | ||
| Waist/hip ratio, M (SD) | 0.83 (0.007) | 0.85 (0.01) | Yes |
Note. CI = confidence interval; P/O = peritoneal or ovarian endometriosis; RV = rectovaginal endometriosis; SD = standard deviation.
First author last name.
Or indicated as significant by authors.
TABLE 6.
Case Control Studies: Adiposity and Endometriosis Diagnosis Using Logistic Regression
| Studya | Year | Adiposity measure | OR | 95% CI | Trend | AOR | 95% CI | Trend |
|---|---|---|---|---|---|---|---|---|
| Cramerb | 1986 | Weight (kg) | ||||||
| ≤56 | 1 | referent | 1 | referent | ||||
| 56–63 | 1.4 | NR | 1.2 | [0.8–1.6] | ||||
| ≥64 | 1.1 | NR | 0.8 | [0.5, 1.1] | ||||
| Hedigerc | 2005 | Perceived figure BMI | 0.9 | [0.8, 1.0] | 0.9 | [0.75, 0.99] |
||
| McCannd | 1993 | Waist/hip ratio | ||||||
| < 30 years old | .001 | .006 | ||||||
| 0.61–0.72 | 6.2 | [2.0, 19.0] | 6.2 | [1.4, 26.7] | ||||
| 0.72–0.76 | 1.4 | [0.4, 4.4] | 3.2 | [0.6, 16.0] | ||||
| 0.76–1.01 | 1 | referent | 1 | referent | ||||
| ≥ 30 years old | .20 | .11 | ||||||
| 0.61–0.72 | 1.3 | [0.4, 4.3] | 1.6 | [0.4, 6.7] | ||||
| 0.72–0.76 | 1.1 | [0.3–3.8] | 1.4 | [0.3, 6.7] | ||||
| 0.76–1.01 | 1 | referent | 1 | referent | ||||
| Waist/thigh ratio | ||||||||
| < 30 years old | .08 | .19 | ||||||
| 1.03–1.22 | 3.6 | [1.2, 10.8] | 2.4 | [0.6, 9.3] | ||||
| 1.22–1.31 | 1.7 | [0.6, 4.7] | 2.7 | [0.7, 9.9] | ||||
| 1.31–1.75 | 1 | referent | 1 | referent | ||||
| ≥ 30 years old | .79 | .76 | ||||||
| 1.03–1.22 | 0.6 | [0.2, 1.9] | 0.6 | [0.1, 2.2] | ||||
| 1.22–1.31 | 1.2 | [0.4, 3.7] | 1.3 | [0.4, 4.7] | ||||
| 1.31–1.75 | 1 | referent | 1 | referent | ||||
| Naglee | 2009 | RW (age 10) | ||||||
| Self-report | ||||||||
| Underweight | NR | NR | 0.9 | [0.5, 1.7] | ||||
| Average | NR | NR | 1.0 | referent | ||||
| Overweight | NR | NR | 2.8 | [1.1, 7.5] | ||||
| Mothers’ report | ||||||||
| Underweight | NR | NR | 1.2 | [0.5, 2.9] | ||||
| Average | NR | NR | 1.0 | referent | ||||
| Overweight | NR | NR | 2.1 | [0.4, 11.0] | ||||
| RW (age 16) | ||||||||
| Self-report | ||||||||
| Underweight | NR | NR | 1.4 | [0.7, 2.7] | ||||
| Average | NR | NR | 1 | referent | ||||
| Overweight | NR | NR | 0.5 | [0.3, 1.0] | ||||
| Mothers’ report | ||||||||
| Underweight | NR | NR | 5.9 | [1.6, 20.9] | ||||
| Average | NR | NR | 1 | referent | ||||
| Overweight | NR | NR | 1.0 | [0.3, 3.6] | ||||
| Signorellof | 1997 | Weight/10 kg; FCs | 0.9 | NR | 0.7 | |||
| Weight/10 kg; IFCs | 0.9 | NR | 0.8 | [0.6, 1.2] |
Note. Values were rounded to the nearest tenth. Trend lists the p-value for the trend in ORs or AORs. AOR = adjusted odds ratio; CI = confidence interval; FC = fertile control; IFC = infertile control; NR = not reported; OR = odds ratio; RW = relative weight.
First author last name.
Adjusted for: Center, age at interview, difference between age at menarche and index date, education, religion, menstrual pain, and cycle length.
Adjusted for: Age, being ≥ 68 inches tall, parity.
Adjusted for: Age, BMI, whether ever pregnant, age at menarche, intensity of menstrual flow, any change in symptoms over time.
Analyses for weight at age 10 adjusted for: Age at menarche; state of residence, relative weight at age 16 years. Analyses for weight at age 16 were adjusted for: Age at menarche; state of residence, relative weight at age 10 years.
Adjusted for: Age, highest educational level attained, regularity of menstrual cycle, exercise, height.
TABLE 7.
Nurses’ Health Study II Publications: Rate Ratios With Multivariate Adjustment, Stratified by Fertility Status
| All |
No infertility |
Infertility history |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Studya | Year | Adiposity | RR | 95% CI | RR | 95% CI | RR | 95% CI | pb |
| Missmer | 2004c | Waist/hip ratio | .36 | ||||||
| < 0.70 | 0.9 | [0.6, 1.4] | 0.8 | [0.5, 1.3] | 1.5 | [0.7, 3.1] | |||
| 0.70–0.79 | 1.0 | referent | 1.0 | referent | 1.0 | referent | |||
| 0.80–0.89 | 1.0 | [0.8, 1.2] | 0.9 | [0.7, 1.2] | 1.2 | [0.7, 2.2] | |||
| > 0.89 | 1.0 | [0.6, 1.5] | 0.9 | [0.5, 1.4] | 1.6 | [0.6, 4.2] | |||
| ptrend | .87 | .82 | .79 | ||||||
| Shah | 2013d | Waist (cm) | <.001 | ||||||
| 22.0–29.9 | 1.1 | [1.0, 1.2] | 1.1 | [0.8, 1.3] | 1.1 | [0.9, 1.2] | |||
| 30.0–32.9 | 1.0 | referent | 1.0 | referent | 1.0 | referent | |||
| 33.0–37.9 | 1.0 | [0.9, 1.1] | 0.9 | [0.6, 1.2] | 1.1 | [0.9, 1.2] | |||
| 38.0–65.0 | 1.0 | [0.8, 1.1] | 0.6 | [0.4, 0.8] | 1.1 | [0.9, 1.3] | |||
| ptrend | .19 | .0003 | .60 | ||||||
| Waist/hip ratio | .16 | ||||||||
| < 0.60 | 2.8 | [1.4, 5.6] | 2.9 | [1.4, 6.2] | 4.0 | [0.5, 33.0] | |||
| 0.60–0.69 | 1.0 | [0.9, 1.2] | 0.9 | [0.8, 1.1] | 1.2 | [0.9, 1.71] | |||
| 0.70–0.79 | 1.0 | referent | 1.0 | referent | 1.0 | referent | |||
| 0.80–0.89 | 1.0 | [0.9, 1.0] | 0.9 | [0.8, 1.0] | 1.1 | [0.9, 1.3] | |||
| ≥ 0.90 | 1.0 | [0.9, 1.2] | 1.1 | [0.9, 1.3] | 0.7 | [0.5, 1.1] | |||
| ptrend | .41 | .76 | .13 | ||||||
| Vitonis | 2010e | Figure (age 5) | .84 | ||||||
| 1 | 1.2 | [1.1, 1.4] | 1.3 | [1.1, 1.5] | 1.1 | [0.8, 1.5] | |||
| 2 | 1.0 | [0.9, 1.1] | 1.0 | [0.9, 1.2] | 0.9 | [0.7, 1.2] | |||
| 3 | 1.0 | referent | 1.0 | referent | 1.0 | referent | |||
| 4 | 0.9 | [0.7, 1.0] | 0.9 | [0.7, 1.1] | 0.8 | [0.5, 1.2]) | |||
| ≥ 5 | 0.9 | [0.7, 1.1] | 0.9 | [0.7, 1.1] | 0.9 | [0.6, 1.4] | |||
| ptrend | < .001 | < .001 | .24 | ||||||
| Figure (age 10) | .77 | ||||||||
| 1 | 1.1 | [1.0, 1.3] | 1.2 | [1.0, 1.4] | 1.1 | [0.8, 1.5] | |||
| 2 | 1.0 | [0.9, 1.2] | 1.0 | [0.9, 1.2] | 1.0 | [0.8, 1.4] | |||
| 3 | 1.0 | referent | 1.0 | referent | 1.0 | referent | |||
| 4 | 0.9 | [0.7, 1.0] | 0.9 | [0.7, 1.0] | 0.8 | [0.6, 1.2] | |||
| ≥ 5 | 0.9 | [0.7, 1.0] | 0.8 | [0.7, 1.0] | 1.0 | [0.7, 1.5] | |||
| ptrend | <.001 | .001 | .30 | ||||||
| Figure (age 20) | |||||||||
| 1 | 1.3 | [1.1, 1.7] | 1.3 | [1.0, 1.7] | 1.6 | [0.9, 2.6] | .36 | ||
| 2 | 1.0 | [0.9, 1.2] | 1.0 | [0.9, 1.1] | 1.2 | [0.9, 1.2] | |||
| 3 | 1.0 | referent | 1.0 | referent | 1.0 | referent | |||
| 4 | 1.1 | [0.9, 1.2] | 1.0 | [0.9, 1.2] | 1.3 | [1.0, 1.7] | |||
| ≥ 5 | 0.9 | [0.7, 1.0] | 0.9 | [0.8, 1.1] | 0.9 | [0.6, 1.3] | |||
| ptrend | .04 | .21 | .20 | ||||||
Note. Values for RRs and CI upper and lower limits were rounded to the nearest tenth. CI = confidence interval; RR = rate ratio.
First author last name.
p-value for test for heterogeneity comparing effects among women having no past or current infertility with those having concurrent infertility.
Adjusted for: Age, race, calendar time, parity, BMI at 18 years old.
Adjusted for: Age, calendar time, infertility status, parity.
Adjusted for: Age, birth weight, calendar time, age at menarche, parity, oral contraceptive use, adult BMI.
Adjusted for: Adjusted for age, calendar time, birth weight, age at menarche, parity, oral contraceptive use, adult BMI.
Methodological Quality
The methodological quality of the studies was varied. Quality varied with regard to small sample sizes, recruitment of women from clinical sites, and inclusion of few measures of adiposity or its distribution. These issues could have increased the likelihood of measurement error and bias that impact generalizability of findings. Many limitations stemmed from the use of observational cross-sectional designs. The use of such designs to assess associations between endometriosis and adiposity is understandable because screening tools for endometriosis are lacking, the symptomatology of the disease is complicated, and the disease is difficult to diagnose.
Sample size was small (< 50 women with and without endometriosis) in seven of the total 21 publications (33.3%). The limited sample sizes can impact statistical power and Type II error rates. Power calculations were provided in only two of the 21 (9.5%) publications. In most publications (n = 13; 61.9%), women were recruited from clinical sites where women were undergoing gynecologic surgery (Table 1). The findings from these studies should be interpreted carefully because of the potential for centripetal (filter) bias, which can occur when women with endometriosis are overrepresented at clinics that provide gynecologic surgery relative to women in the general population. This bias may be compounded by referral bias, in which participants with endometriosis may be referred from primary care to specialty care sites and, therefore, overrepresented at these specialty sites relative to the general population. In addition, findings may be complicated by lead time bias that arises from a shorter time between the emergence of a disease to diagnosis among women with access to and receiving health care relative to women without access or not engaging in healthcare (Szklo & Nieto, 2004). In studies based on NHSII data, only registered nurses were included as participants, limiting the generalizability of the findings.
Choices of comparison groups are a key consideration when synthesizing research findings. Current endometriosis research has included different types of control groups, such as friends of case participants and women undergoing surgical evaluation for gynecologic pathologies (Table 1). Because women within a social network may have similar adiposity (Christakis & Fowler, 2007), it may be more to difficult to find differences in adiposity measures between women with and without endometriosis.
Adiposity has been measured in a limited number of ways. In most publications (n = 11; 52.4%) researchers reported use of a single measure of adiposity (Table 1). In nine publications (42.9%), women self-reported adiposity on questionnaires, but self-reported adiposity may not be accurate (Nyholm et al., 2007). To minimize such error, the NHSII protocol asked participants to read standardized instructions for measuring body circumferences, but participant measurements may not be as precise as those obtained by trained individuals (Rimm et al., 1990).
The operational definition of endometriosis is another consideration: in most studies, endometriosis was assessed via laparoscopy and/or laparotomy (Tables 1 and 2). This was consistent with the clinical gold standard in the United States which requires visualized disease, at a minimum (Practice Committee of the ASRM, 2012). In two of the 21 publications (9.5%), diagnoses were extracted from medical charts, but information about how clinicians had made the original diagnoses was not provided. The three NHSII-based publications relied on participant self-reports of endometriosis diagnosis or treatment. Validation studies showed that not all women who reported being diagnosed with endometriosis had had a diagnosis in their medical records (Kvaskoff et al., 2009; Missmer et al., 2004). They did not validate women’s self-reports of never having been diagnosed with endometriosis against women’s medical records.
Discussion
Our systematic review revealed that research on the relationships between measures of adiposity and endometriosis is limited. Among the publications we reviewed, most included only measures of overall adiposity (e.g., body silhouette figures). Few publications described studies in which researchers measured adipose tissue distribution (e.g., waist and hip circumferences). VAT was not measured in any of the studies. Therefore, the types of adiposity measures that researchers used were limited.
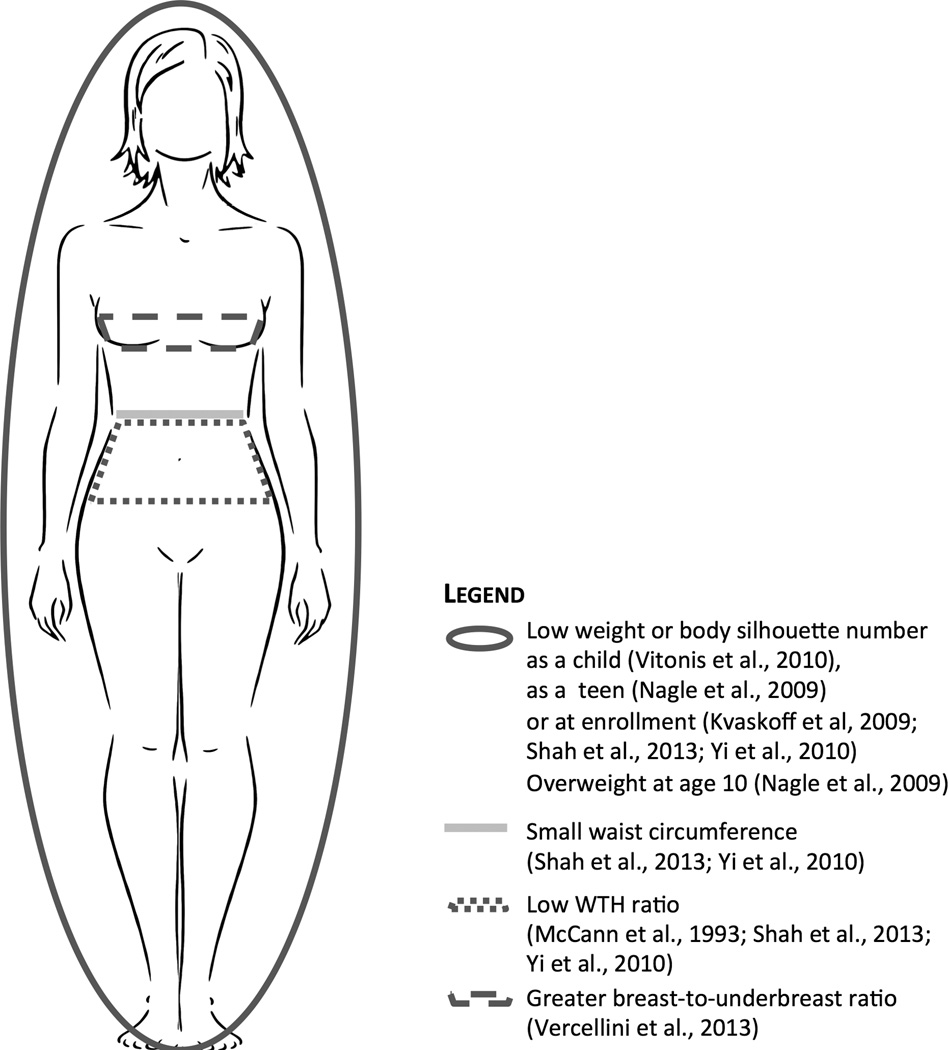
Overall findings suggested that lean body habitus, particularly low amounts of adipose tissue and adipose tissue below the waist, may be associated with endometriosis (Figure 1). The inverse relationship between overall adiposity and endometriosis is congruent with hypotheses and data about how adipose tissue may be involved in the development of endometriosis through immunological pathways. For example, being lean is associated with a predominance of the M2 macrophages, whereas being larger is associated with a predominance of M1 macrophages (Lumeng et al., 2007). (In general, M1 macrophages promote inflammation and inhibit angiogenesis and tissue remodeling; in contrast M2 macrophages are anti-inflammatory and promote angiogenesis and tissue remodeling; Brown et al., 2012; Jetten et al., 2014; Ruffell et al., 2009).
FIGURE 1.
Visual summary of findings from the systematic review. WTH = waist-to-hip.
Researchers have found some evidence that M2 macrophages may be involved in the development of endometriosis potentially through the actions of M2 including angiogenesis and tissue remodeling (Smith et al., 2012; Wang et al., 2014; Wang et al., 2015). Findings that adipose tissue below the waist is associated with endometriosis are generally consistent with the current hypotheses that estrogen influences the amount and distribution of adipose tissue (Jasieńska, Ziomkiewicz, Ellison, Lipson, & Thune, 2004; Ley, Lees, & Stevenson, 1992) and endometriosis is an estrogen-dependent disease (Kitawaki et al., 2002). Thus, when researchers observed that being lean and having adipose tissue predominantly below the waist were associated with endometriosis, their findings were consistent some proposed biological mechanisms of endometriosis.
We also found no publications that reported associations between VAT and endometriosis. Because we know that VAT is biologically active relative to subcutaneous fat (Ibrahim, 2010), researchers can design future studies to investigate relationships between VAT and endometriosis that may help identify possible etiologic mechanisms of the disease. These researchers could sample sufficient numbers of participants to power their planned analyses, recruit from community-dwelling female populations to reduce centripetal bias, and operationalize endometriosis with physicians’ reports of visualized disease.
Weighing the findings we reviewed, we note important methodological considerations from observational studies on endometriosis risk factors. First, these studies may contain threats to internal validity. These threats stem from recruiting small numbers of participants (e.g., < 50 participants) and including only women who sought care from specialty clinical sites. Small samples and samples consisting only of patients from specialty clinical sites limit researchers’ abilities to detect differences between women with and without endometriosis in the general population. Findings from such studies limit scientists in generalizing findings to women who either have no signs or symptoms of the disease or women who do not seek care (e.g., lack access to healthcare). Researchers might be able to detect differences between women with and without endometriosis if they were to recruit larger numbers of women and recruit women from varying sites and the general population.
Second, many studies were limited in how researchers assessed adiposity. In several publications, researchers did not include a variety of measures to capture various characteristics of adiposity, including adipose tissue distribution and visceral adiposity. Without adequate measures, researchers could miss detecting more nuanced relationships between adiposity characteristics (e.g., amount, location) and endometriosis that could identify potential disease mechanisms. Researchers can include varied measures of adiposity into their future studies.
Third, many studies were limited in the timing of the measures of adiposity. Most researchers assessed participants’ adiposity at the time of their endometriosis diagnosis. This practice may result in an incomplete picture of adiposity characteristics and the onset and progression of the disease. Endometriosis has been found among adolescents and young adults (Dun et al., 2015), yet many women who may have had endometriosis when they were younger are not diagnosed until they are later in adulthood. Researchers would likely gain rich information about the natural history and biological mechanisms of endometriosis by assessing adiposity and endometriosis from childhood through women’s’ reproductive years. This research may provide insights regarding the natural history and biological mechanisms of the disease.
Finally, several studies were limited in how endometriosis was assessed. In these studies, researchers did not apply the gold standard criteria for diagnosing endometriosis, which is a surgically visualized disease. Instead, these researchers included women’s reports of having received an endometriosis diagnoses from a physician. Because endometriosis may exist in women who have no symptoms, such women with endometriosis may have been excluded from case groups. While some researchers assessed the validity of women’s self-reported diagnosis of endometriosis, they did not assess the validity of women’s self-reported lack of having received endometriosis diagnoses. Researchers could benefit from assessing endometriosis with the clinical gold standard in clinical samples. For studies in which participants are recruited from the general population, researchers could use emerging radiologic imaging that can indicate endometriosis (e.g., transvaginal ultrasound or magnetic resonance imaging) (Exacoustos et al., 2014; Guerriero et al., 2015; Noventa et al., 2015; Thomeer et al., 2014). When researchers decide to assess endometriosis with women’s reports of having an endometriosis diagnosis, researchers could evaluate the validity of their measures. Researchers could compare women’s self-reports of never being diagnosed to corresponding medical records.
Implications
Findings in our review suggest that there may be an association between endometriosis and either overall adiposity or adipose tissue distribution. However, we found gaps in the literature. Many studies included (a) small numbers of participants recruited from specialty clinics; (b) one or a few number of adiposity measures; and (c) adiposity assessments at the time when endometriosis was diagnosed. Several studies included women’s reports of being diagnosed with endometriosis. To address these gaps, researchers can design longitudinal studies to investigate associations between adiposity and endometriosis by including (a) adequately sized samples of women randomly selected from a variety of sites, including the general population, in order to capture women who are asymptomatic and/or do not access healthcare; (b) rigorously measured adiposity, including measures of overall adiposity, distribution, and VAT; (c) measurements of adiposity at various points throughout the lifespan; and (d) physician-visualized endometriosis via surgery among women undergoing the procedure or via imaging technologies among women who do not have indications for surgery.
Researchers could investigate potential biological mechanisms involved in the development of endometriosis that are proposed to be related to overall adiposity, adipose tissue distribution, and/or VAT. Researchers can test current hypotheses about how adiposity may be linked to endometriosis as mediated by the immune system, including the activation and actions of M2 macrophages. To understand these links, researchers could continue to investigate peripheral biomarkers of endometriosis that are products of adipose tissue, such as leptin and adiponectin (Pandey, Kriplani, Yadav, Lyngdoh, & Mahapatra, 2010). Researchers could also investigate peripheral adipokines implicated in other gynecologic diseases but not yet studied with relation to endometriosis, such as visfatin (Tian et al., 2013). To provide insights regarding underlying pathways that contribute to the development of the disease, such as immune-related pathways, researchers can collect adipose tissue and endometriotic lesion biospecimens to quantify adipocytes or other adiposity- and endometriosis-related biomarkers.
Limitations
Despite a systematic search and consultation with a librarian, we may not have included all relevant articles. We decided a priori to exclude publications in which the only adiposity measure was BMI. We were not able to conduct a meta-analysis because the number of empirically-based studies with comparable adiposity measures was limited (Egger, Smith, & Phillips, 1997).
Conclusions
In this systematic review, 21 publications in which associations between endometriosis and either overall adiposity or adipose tissue distribution were assessed. The studies varied by design (case control, prospective cohort), sampling frameworks (recruited women undergoing surgery, recruited nurses across 14 states), adiposity measures (e.g., self-reported weight, researcher-measured waist circumference), and endometriosis assessments (surgically visualized disease, self-reported physician-diagnosed disease). Collectively, these data suggest that lower overall adiposity and adipose tissues concentrated below—rather than above—the waist are each associated with endometriosis. To identify disease mechanisms, studies can be designed that recruit both women seeking care from clinical sites and women randomly sampled from the general population. Relationships can be assessed between different characteristics of adiposity over time relative to the natural history of endometriosis and its clinical stages. To assess mechanisms and pathways of the disease, peripheral adiposity biomarkers associated with endometriosis can be assessed, as can presence of adipokines or endometriosis-related biomarkers in endometriotic lesions. Findings from future research could fill critical gaps regarding whether and how adiposity may be associated with endometriosis.
Supplementary Material
Supplemental Digital Content 1. Table that includes searches in PubMed and Web of Science using a predetermined list of search terms. .Doc
Supplemental Digital Content 2. Figure illustrating the complete process of identifying eligible publications. .TIFF
Acknowledgments
The authors would like to thank the University of Wisconsin-Madison School of Nursing faculty, staff, and students, the ENDO Study Group, the NICHD Division of Intramural Population Health Research, the National Institute of Nursing Research (NINR) Division of Intramural Research, and the National Institutes of Health (NIH) Office of Intramural Training and Education for their support.
Dr. Backonja was funded through the NINR/National Institutes of Health Graduate Partnership Program during the literature review and initial writing of the manuscript. She is currently funded by the NIH, National Library of Medicine (NLM) Biomedical and Health Informatics Training Program at the University of Washington (Grant Nr. T15LM007442).
Contributor Information
Uba Backonja, National Library of Medicine Biomedical Informatics Postdoctoral Fellow, Division of Biomedical and Health Informatics, University of Washington School of Medicine, Seattle, WA.
Germaine M. Buck Louis, Director and Senior Investigator, Office of the Director Division of Intramural Population Health Research, Eunice Kennedy Shriver National Institute of Child Health and Human Development, Rockville, MD.
Diane R. Lauver, Professor, School of Nursing, University of Wisconsin-Madison, Madison, WI.
References
- Adya R, Tan BK, Chen J, Randeva HS. Protective actions of globular and full-length adiponectin on human endothelial cells: Novel insights into adiponectin-induced angiogenesis. Journal of Vascular Research. 2012;49:534–543. doi: 10.1159/000338279. [DOI] [PubMed] [Google Scholar]
- Committee on Practice Bulletins—Gynecology. American College of Obstetricians and Gynecologists. Management of endometriosis [Practice Bulletin] Obstetrics & Gynecology. 2010;116:223–236. [Google Scholar]
- Ayas S, Bayraktar M, Gürbüz A, Alkan A, Eren S. Uterine junctional zone thickness, cervical length and bioelectrical impedance analysis of body composition in women with endometriosis. Balkan Medical Journal. 2012;29:410–413. doi: 10.5152/balkanmedj.2012.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ballard K, Lowton K, Wright J. What’s the delay? A qualitative study of women’s experiences of reaching a diagnosis of endometriosis. Fertility and Sterility. 2006;86:1296–1301. doi: 10.1016/j.fertnstert.2006.04.054. [DOI] [PubMed] [Google Scholar]
- Bedaiwy MA, Falcone T, Goldberg JM, Sharma RK, Nelson DR, Agarwal A. Peritoneal fluid leptin is associated with chronic pelvic pain but not infertility in endometriosis patients. Human Reproduction. 2006;21:788–791. doi: 10.1093/humrep/dei376. [DOI] [PubMed] [Google Scholar]
- Borrelli GM, Abrão MS, Mechsner S. Can chemokines be used as biomarkers for endometriosis? A systematic review. Human Reproduction. 2014;29:253–266. doi: 10.1093/humrep/det401. [DOI] [PubMed] [Google Scholar]
- Brown BN, Londono R, Tottey S, Zhang L, Kukla KA, Wolf MT, Badylak SF. Acta Biomaterialia. 2012;8:978–987. doi: 10.1016/j.actbio.2011.11.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruce R, Lees B, Whitcroft SI, McSweeney G, Shaw RW, Stevenson JC. Changes in body composition with danazol therapy. Fertility and Sterility. 1991;56:574–576. [PubMed] [Google Scholar]
- Buck Louis GMB, Hediger ML, Peterson CM, Croughan M, Sundaram R, Stanford J ENDO Study Working Group. Incidence of endometriosis by study population and diagnostic method: The ENDO study. Fertility and Sterility. 2011;96:360–365. doi: 10.1016/j.fertnstert.2011.05.087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burney RO, Giudice LC. Pathogenesis and pathophysiology of endometriosis. Fertility and Sterility. 2012;98:511–519. doi: 10.1016/j.fertnstert.2012.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canis M, Donnez JG, Guzick DS, Halme JK, Rock JA, Schenken RS, Vernon MW. Revised American society for reproductive medicine classification of endometriosis: 1996. Fertility and Sterility. 1997;67:817–821. doi: 10.1016/s0015-0282(97)81391-x. [DOI] [PubMed] [Google Scholar]
- Cao R, Brakenhielm E, Wahlestedt C, Thyberg J, Cao Y. Leptin induces vascular permeability and synergistically stimulates angiogenesis with FGF-2 and VEGF. Proceedings of the National Academy of Sciences of the United States of America. 2001;98:6390–6395. doi: 10.1073/pnas.101564798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. New England Journal of Medicine. 2007;357:370–379. doi: 10.1056/NEJMsa066082. [DOI] [PubMed] [Google Scholar]
- Cramer DW, Wilson E, Stillman RJ, Berger MJ, Belisle S, Schiff I, Schoenbaum SC. The relation of endometriosis to menstrual characteristics, smoking, and exercise. JAMA. 1986;255:1904–1908. [PubMed] [Google Scholar]
- Darrow SL, Selman S, Batt RE, Zielezny MA, Vena JE. Sexual activity, contraception, and reproductive factors in predicting endometriosis. American Journal of Epidemiology. 1994;140:500–509. doi: 10.1093/oxfordjournals.aje.a117276. [DOI] [PubMed] [Google Scholar]
- Deurenberg P, Yap M, van Staveren WA. Body mass index and percent body fat: A meta analysis among different ethnic groups. International Journal of Obesity. 1998;22:1164–1171. doi: 10.1038/sj.ijo.0800741. [DOI] [PubMed] [Google Scholar]
- D’Hooghe TM, Debrock S. Endometriosis, retrograde menstruation and peritoneal inflammation in women and in baboons. Human Reproduction Update. 2002;8:84–88. doi: 10.1093/humupd/8.1.84. [DOI] [PubMed] [Google Scholar]
- Dun EC, Kho KA, Morozov VV, Kearney S, Zurawin JL, Nezhat CH. Endometriosis in adolescents. Journal of the Society of Laparoendoscopic Surgeons. 2015;19:e2015.00019. doi: 10.4293/JSLS.2015.00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egger M, Smith GD, Phillips AN. Meta-analysis: Principles and procedures. British Medical Journal. 1997;315:1533–1537. doi: 10.1136/bmj.315.7121.1533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eskenazi B, Warner ML. Epidemiology of endometriosis. Obstetrics and Gynecological Clinics of North America. 1997;24:235–258. doi: 10.1016/s0889-8545(05)70302-8. [DOI] [PubMed] [Google Scholar]
- Exacoustos C, Malzoni M, Di Giovanni A, Lazzeri L, Tosti C, Petraglia F, Zupi E. Ultrasound mapping system for the surgical management of deep infiltrating endometriosis. Fertility and Sterility. 2014;102:143–150. doi: 10.1016/j.fertnstert.2014.03.043. [DOI] [PubMed] [Google Scholar]
- Fassbender A, Burney RO, O DF, D’Hooghe T, Giudice L. Update on biomarkers for the detection of endometriosis. BioMed Research International, Article. 2015:130854. doi: 10.1155/2015/130854. Retrieved from http://www.hindawi.com/journals/bmri/2015/130854/ [DOI] [PMC free article] [PubMed]
- Fassbender A, Vodolazkaia A, Saunders P, Lebovic D, Waelkens E, De Moor B, D’Hooghe T. Biomarkers of endometriosis. Fertility and Sterility. 2013;99:1135–1145. doi: 10.1016/j.fertnstert.2013.01.097. [DOI] [PubMed] [Google Scholar]
- Ferrero S, Anserini P, Remorgida V, Ragni N. Body mass index in endometriosis. European Journal of Obstetrics & Gynecology and Reproductive Biology. 2005;121:94–98. doi: 10.1016/j.ejogrb.2004.11.019. [DOI] [PubMed] [Google Scholar]
- Guerriero S, Ajossa S, Minguez JA, Jurado M, Mais V, Melis GB, Alcazar JL. Diagnostic accuracy of transvaginal ultrasound for diagnosis of deep endometriosis regarding locations other than recto-sigmoid: Systematic review and meta-analysis. Ultrasound in Obstetrics & Gynecology. 2015 doi: 10.1002/uog.15667. [DOI] [PubMed] [Google Scholar]
- Halme J, Hammond MG, Hulka JF, Raj SG, Talbert LM. Retrograde menstruation in healthy women and in patients with endometriosis. Obstetrics and Gynecology. 1984;64:151–154. [PubMed] [Google Scholar]
- Hediger ML, Hartnett HJ, Louis GMB. Association of endometriosis with body size and figure. Fertility and Sterility. 2005;84:1366–1374. doi: 10.1016/j.fertnstert.2005.05.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ibrahim MM. Subcutaneous and visceral adipose tissue: Structural and functional differences. Obesity Reviews. 2010;11:11–18. doi: 10.1111/j.1467-789X.2009.00623.x. [DOI] [PubMed] [Google Scholar]
- Jasieńska G, Ziomkiewicz A, Ellison PT, Lipson SF, Thune I. Large breasts and narrow waists indicate high reproductive potential in women. Proceedings of the Royal Society of London-Series B: Biological Sciences. 2004;271:1213–1217. doi: 10.1098/rspb.2004.2712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jetten N, Verbruggen S, Gijbels MJ, Post MJ, De Winther MP, Donners MM. Anti-inflammatory M2, but not pro-inflammatory M1 macrophages promote angiogenesis in vivo. Angiogenesis. 2014;17:109–118. doi: 10.1007/s10456-013-9381-6. [DOI] [PubMed] [Google Scholar]
- Kitawaki J, Kado N, Ishihara H, Koshiba H, Kitaoka Y, Honjo H. Endometriosis: The pathophysiology as an estrogen-dependent disease. Journal of Steroid Biochemistry and Molecular Biology. 2002;83:149–155. doi: 10.1016/s0960-0760(02)00260-1. [DOI] [PubMed] [Google Scholar]
- Kobashi C, Urakaze M, Kishida M, Kibayashi E, Kobayashi H, Kihara S, Kobayashi M. Adiponectin inhibits endothelial synthesis of interleukin-8. Circulation Research. 2005;97:1245–1252. doi: 10.1161/01.RES.0000194328.57164.36. [DOI] [PubMed] [Google Scholar]
- Kvaskoff M, Mesrine S, Clavel-Chapelon F, Boutron-Ruault M-C. Endometriosis risk in relation to naevi, freckles and skin sensitivity to sun exposure: The French E3N cohort. International Journal of Epidemiology. 2009;38:1143–1153. doi: 10.1093/ije/dyp175. [DOI] [PubMed] [Google Scholar]
- Ley CJ, Lees B, Stevenson JC. Sex- and menopause-associated changes in body-fat distribution. American Journal of Clinical Nutrition. 1992;55:950–954. doi: 10.1093/ajcn/55.5.950. [DOI] [PubMed] [Google Scholar]
- Lumeng CN, Bodzin JL, Saltiel AR. Obesity induces a phenotypic switch in adipose tissue macrophage polarization. Journal of Clinical Investigation. 2007;117:175–184. doi: 10.1172/JCI29881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mandal P, Pratt BT, Barnes M, McMullen MR, Nagy LE. Molecular mechanism for adiponectin-dependent M2 macrophage polarization: Link between the metabolic and innate immune activity of full-length adiponectin. Journal of Biological Chemistry. 2011;286:13460–13469. doi: 10.1074/jbc.M110.204644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matalliotakis IM, Cakmak H, Fragouli YG, Goumenou AG, Mahutte NG, Arici A. Epidemiological characteristics in women with and without endometriosis in the Yale series. Archives of Gynecology and Obstetrics. 2008;277:389–393. doi: 10.1007/s00404-007-0479-1. [DOI] [PubMed] [Google Scholar]
- May KE, Conduit-Hulbert SA, Villar J, Kirtley S, Kennedy SH, Becker CM. Peripheral biomarkers of endometriosis: A systematic review. Human Reproduction Update. 2010;16:651–674. doi: 10.1093/humupd/dmq009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May KE, Villar J, Kirtley S, Kennedy SH, Becker CM. Endometrial alterations in endometriosis: A systematic review of putative biomarkers. Human Reproduction Update. 2011;17:637–653. doi: 10.1093/humupd/dmr013. [DOI] [PubMed] [Google Scholar]
- McCann SE, Freudenheim JL, Darrow SL, Batt RE, Zielezny MA. Endometriosis and body fat distribution. Obstetrics & Gynecology. 1993;82:545–549. [PubMed] [Google Scholar]
- Melin A, Sparén P, Persson I, Bergqvist A. Endometriosis and the risk of cancer with special emphasis on ovarian cancer. Human Reproduction. 2006;21:1237–1242. doi: 10.1093/humrep/dei462. [DOI] [PubMed] [Google Scholar]
- Missmer SA, Hankinson SE, Spiegelman D, Barbieri RL, Marshall LM, Hunter DJ. Incidence of laparoscopically confirmed endometriosis by demographic, anthropometric, and lifestyle factors. American Journal of Epidemiology. 2004;160:784–796. doi: 10.1093/aje/kwh275. [DOI] [PubMed] [Google Scholar]
- Murphy AA. Clinical aspects of endometriosis. Annals of the New York Academy of Sciences. 2002;955:1–10. doi: 10.1111/j.1749-6632.2002.tb02760.x. [DOI] [PubMed] [Google Scholar]
- Murray PJ, Wynn TA. Protective and pathogenic functions of macrophage subsets. Nature Reviews Immunology. 2011;11:723–737. doi: 10.1038/nri3073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagle CM, Bell TA, Purdie DM, Treloar SA, Olsen CM, Grover S, Green AC. Relative weight at ages 10 and 16 years and risk of endometriosis: A case-control analysis. Human Reproduction. 2009;24:1501–1506. doi: 10.1093/humrep/dep048. [DOI] [PubMed] [Google Scholar]
- Noventa M, Saccardi C, Litta P, Vitagliano A, D’Antona D, Abdulrahim B, Gizzo S. Ultrasound techniques in the diagnosis of deep pelvic endometriosis: Algorithm based on a systematic review and meta-analysis. Fertility and Sterility. 2015;104:366–383. doi: 10.1016/j.fertnstert.2015.05.002. [DOI] [PubMed] [Google Scholar]
- Nyholm M, Gullberg B, Merlo J, Lundqvist-Persson C, Råstam L, Lindblad U. The validity of obesity based on self-reported weight and height: Implications for population studies. Obesity. 2007;15:197–208. doi: 10.1038/oby.2007.536. [DOI] [PubMed] [Google Scholar]
- Olive DL, Schwartz LB. Endometriosis. New England Journal of Medicine. 1993;328:1759–1769. doi: 10.1056/NEJM199306173282407. [DOI] [PubMed] [Google Scholar]
- Ouchi N, Kihara S, Arita Y, Okamoto Y, Maeda K, Kuriyama H, Matsuzawa Y. Adiponectin, an adipocyte-derived plasma protein, inhibits endothelial NF-kappaB signaling through a cAMP-dependent pathway. Circulation. 2000;102:1296–1301. doi: 10.1161/01.cir.102.11.1296. [DOI] [PubMed] [Google Scholar]
- Pandey N, Kriplani A, Yadav RK, Lyngdoh BT, Mahapatra SC. Peritoneal fluid leptin levels are increased but adiponectin levels are not changed in infertile patients with pelvic endometriosis. Gynecological Endocrinology. 2010;26:843–849. doi: 10.3109/09513590.2010.487585. [DOI] [PubMed] [Google Scholar]
- Pearce CL, Templeman C, Rossing MA, Lee A, Near AM, Webb PM Ovarian Association Consortium. Association between endometriosis and risk of histological subtypes of ovarian cancer: A pooled analysis of case-control studies. Lancet Oncology. 2012;13:385–394. doi: 10.1016/S1470-2045(11)70404-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Practice Committee of the American Society for Reproductive Medicine. Endometriosis and infertility: A committee opinion. Fertility and Sterility. 2012;98:591–598. doi: 10.1016/j.fertnstert.2012.05.031. [DOI] [PubMed] [Google Scholar]
- Rasouli N, Kern PA. Adipocytokines and the metabolic complications of obesity. Journal of Clinical Endocrinology & Metabolism. 2008;93:s64–s73. doi: 10.1210/jc.2008-1613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rico H, Revilla M, Arnanz F, Villa LF, Perera S, Arribas I. Total and regional bone mass values and biochemical markers of bone remodeling in endometriosis. Obstetrics & Gynecology. 1993;81:272–274. [PubMed] [Google Scholar]
- Rimm EB, Stampfer MJ, Colditz GA, Chute CG, Litin LB, Willett WC. Validity of self-reported waist and hip circumferences in men and women. Epidemiology. 1990;1:466–473. doi: 10.1097/00001648-199011000-00009. [DOI] [PubMed] [Google Scholar]
- Rocha ALL, Reis FM, Taylor RN. Angiogenesis and endometriosis. Obstetrics and Gynecology International. 2013;2013:859619. doi: 10.1155/2013/859619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers PAW, D’Hooghe TM, Fazleabas A, Giudice LC, Montgomery GW, Petraglia F, Taylor RN. Defining Future Directions for Endometriosis Research Workshop Report from the 2011 World Congress of Endometriosis in Montpellier, France. Reproductive Sciences. 2013;20:483–499. doi: 10.1177/1933719113477495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruffell D, Mourkioti F, Gambardella A, Kirstetter P, Lopez RG, Rosenthal N, Nerlov C. A CREB-C/EBPbeta cascade induces M2 macrophage-specific gene expression and promotes muscle injury repair. Proceedings of the National Academy of Sciences of the United States of America. 2009;106:17475–17480. doi: 10.1073/pnas.0908641106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahmani M, Ghaleh TD, Darabi M, Darabi M, Rashvand Z, Najafipour R. I405V polymorphism of CETP gene and lipid profile in women with endometriosis. Gynecological Endocrinology. 2013;29:712–715. doi: 10.3109/09513590.2013.797396. [DOI] [PubMed] [Google Scholar]
- Sampson JA. Peritoneal endometriosis due to menstrual dissemination of endometrial tissue into the pelvic cavity. American Journal of Obstetrics and Gynecology. 1927;14:422–469. [Google Scholar]
- Savaris AL, do Amaral VF. Nutrient intake, anthropometric data and correlations with the systemic antioxidant capacity of women with pelvic endometriosis. European Journal of Obstetrics & Gynecology and Reproductive Biology. 2011;158:314–318. doi: 10.1016/j.ejogrb.2011.05.014. [DOI] [PubMed] [Google Scholar]
- Schäffler A, Schölmerich J, Salzberger B. Adipose tissue as an immunological organ: Toll-like receptors, C1q/TNFs and CTRPs. Trends in Immunology. 2007;28:393–399. doi: 10.1016/j.it.2007.07.003. [DOI] [PubMed] [Google Scholar]
- Scholefield HJ, Sajjad Y, Morgan PR. Cutaneous endometriosis and its association with caesarean section and gynaecological procedures. Journal of the Institute of Obstetrics and Gynaecology. 2002;22:553–554. doi: 10.1080/0144361021000003762. [DOI] [PubMed] [Google Scholar]
- Shah NR, Braverman ER. Measuring adiposity in patients: The utility of body mass index (BMI), percent body fat, and leptin. PLOS ONE. 2012;7:e33308. doi: 10.1371/journal.pone.0033308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah DK, Correia KF, Vitonis AF, Missmer SA. Body size and endometriosis: Results from 20 years of follow-up within the Nurses’ Health Study II prospective cohort. Human Reproduction. 2013;28:1783–1792. doi: 10.1093/humrep/det120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Signorello LB, Harlow BL, Cramer DW, Spiegelman D, Hill JA. Epidemiologic determinants of endometriosis: A hospital-based case-control study. Annals of Epidemiology. 1997;7:267–274. doi: 10.1016/s1047-2797(97)00017-3. [DOI] [PubMed] [Google Scholar]
- Signorile PG, Baldi F, Bussani R, D’Armiento M, De Falco M, Boccellino M, Baldi A. New evidence of the presence of endometriosis in the human fetus. Reproductive BioMedicine Online. 2010;2:142–147. doi: 10.1016/j.rbmo.2010.04.002. [DOI] [PubMed] [Google Scholar]
- Simoens S, Dunselman G, Dirksen C, Hummelshoj L, Bokor A, Brandes I, D’Hooghe T. The burden of endometriosis: Costs and quality of life of women with endometriosis and treated in referral centres. Human Reproduction. 2012;27:1292–1299. doi: 10.1093/humrep/des073. [DOI] [PubMed] [Google Scholar]
- Smith KA, Pearson CB, Hachey AM, Xia D-L, Wachtman LM. Alternative activation of macrophages in rhesus macaques (Macaca mulatta) with endometriosis. Comparative Medicine. 2012;62:303–310. [PMC free article] [PubMed] [Google Scholar]
- Strimbu K, Tavel JA. What are biomarkers? Current Opinion in HIV and AIDS. 2010;5:463–466. doi: 10.1097/COH.0b013e32833ed177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stunkard AJ, Sørenson T, Schulsinger F. Use of the Danish Adoption Register for the study of obesity and thinness. In: Kety SS, Rowland LP, Sidman RL, Matthysse SW, editors. The genetics of neurological and psychiatric disorders. New York, NY: Raven Press; 1983. pp. 115–120. [PubMed] [Google Scholar]
- Szklo M, Nieto FJ. Epidemiology: Beyond the basics. Sudbury, MA: Jones & Bartlett; 2004. [Google Scholar]
- Thomeer MG, Steensma AB, van Santbrink EJ, Willemssen FE, Wielopolski PA, Hunink MG, Krestin GP. Can magnetic resonance imaging at 3.0-Tesla reliably detect patients with endometriosis? Initial results. Journal of Obstetrics and Gynaecology Research. 2014;40:1051–1058. doi: 10.1111/jog.12290. [DOI] [PubMed] [Google Scholar]
- Tian W, Zhu Y, Wang Y, Teng F, Zhang H, Liu G, Xue F. Visfatin, a potential biomarker and prognostic factor for endometrial cancer. Gynecologic Oncology. 2013;129:505–512. doi: 10.1016/j.ygyno.2013.02.022. [DOI] [PubMed] [Google Scholar]
- Treloar S, Hadfield R, Montgomery G, Lambert A, Wicks J, Barlow DH International Endogene Study Group. The International Endogene Study: A collection of families for genetic research in endometriosis. Fertility and Sterility. 2002;78:679–685. doi: 10.1016/s0015-0282(02)03341-1. [DOI] [PubMed] [Google Scholar]
- Vatier C, Kadiri S, Muscat A, Chapron C, Capeau J, Antoine B. Visceral and subcutaneous adipose tissue from lean women respond differently to lipopolysaccharide-induced alteration of inflammation and glyceroneogenesis. Nutrition & Diabetes. 2012;2:e51. doi: 10.1038/nutd.2012.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vercellini P, Buggio L, Somigliana E, Barbara G, Viganò P, Fedele L. Attractiveness of women with rectovaginal endometriosis: A case-control study. Fertility and Sterility. 2013;99:212–218. doi: 10.1016/j.fertnstert.2012.08.039. [DOI] [PubMed] [Google Scholar]
- Vercellini P, Fedele L, Aimi G, Pietropaolo G, Consonni D, Crosignani PG. Association between endometriosis stage, lesion type, patient characteristics and severity of pelvic pain symptoms: A multivariate analysis of over 1000 patients. Human Reproduction. 2007;22:266–271. doi: 10.1093/humrep/del339. [DOI] [PubMed] [Google Scholar]
- Viganò P, Somigliana E, Panina P, Rabellotti E, Vercellini P, Candiani M. Principles of phenomics in endometriosis. Human Reproduction Update. 2012;18:248–259. doi: 10.1093/humupd/dms001. [DOI] [PubMed] [Google Scholar]
- Vitonis AF, Baer HJ, Hankinson SE, Laufer MR, Missmer SA. A prospective study of body size during childhood and early adulthood and the incidence of endometriosis. Human Reproduction. 2010;25:1325–1334. doi: 10.1093/humrep/deq039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waki H, Tontonoz P. Endocrine functions of adipose tissue. Annual Review of Pathology: Mechanisms of Disease. 2007;2:31–56. doi: 10.1146/annurev.pathol.2.010506.091859. [DOI] [PubMed] [Google Scholar]
- Wang Y, Chen H, Wang N, Guo H, Fu Y, Xue S, Kuang Y. Combined 17β-estradiol with TCDD promotes M2 polarization of macrophages in the endometriotic milieu with aid of the interaction between endometrial stromal cells and macrophages. PloS One. 2015;10:e0125559. doi: 10.1371/journal.pone.0125559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y, Fu Y, Xue S, Ai A, Chen H, Lyu Q, Kuang Y. The M2 polarization of macrophage induced by fractalkine in the endometriotic milieu enhances invasiveness of endometrial stromal cells. International Journal of Clinical and Experimental Pathology. 2014;7:194–203. [PMC free article] [PubMed] [Google Scholar]
- Yi KW, Shin J-H, Park HT, Kim T, Kim SH, Hur J-Y. Resistin concentration is increased in the peritoneal fluid of women with endometriosis. American Journal of Reproductive Immunology. 2010;64:318–323. doi: 10.1111/j.1600-0897.2010.00840.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Digital Content 1. Table that includes searches in PubMed and Web of Science using a predetermined list of search terms. .Doc
Supplemental Digital Content 2. Figure illustrating the complete process of identifying eligible publications. .TIFF