Abstract
Background
Research has demonstrated that increases in palliative homecare nursing are associated with a reduction in the rate of subsequent hospitalizations. However, little evidence is available about the cost-savings potential of palliative nursing when accounting for both increased nursing costs and potentially reduced hospital costs.
Methods
Our retrospective cohort study included cancer decedents from British Columbia, Ontario, and Nova Scotia who received any palliative nursing in the last 6 months of life. A Poisson regression analysis was used to determine the association of increased nursing costs (in 2-week blocks) on the relative average hospital costs in the subsequent 2-week block and on the overall total cost (hospital costs plus nursing costs in the preceding 2-week block).
Results
The cohort included 58,022 cancer decedents. Results of the analysis for the last month of life showed an association between increased nursing costs and decreased relative hospital costs in comparisons with a reference group (>0 to 1 hour nursing in the block): the maximum decrease was 55% for Ontario, 31% for British Columbia, and 38% for Nova Scotia. Also, increased nursing costs in the last month were almost always associated with lower total costs in comparison with the reference. For example, cost savings per person-block ranged from $376 (>10 nursing hours) to $1,124 (>4 to 6 nursing hours) in British Columbia.
Conclusions
In the last month of life, increased palliative nursing costs (compared with costs for >0 to 1 hour of nursing in the block) were associated with lower relative hospital costs and a lower total cost in a subsequent block. Our research suggests a cost-savings potential associated with increased community-based palliative nursing.
Keywords: Palliative care, homecare, nursing, hospitalization, costing, end of life, Canadian data
INTRODUCTION
Policymakers across Canada and internationally are increasingly recognizing end-of-life care as a priority because of its economic and care quality implications. Overall, 55% of Canadians die in hospital1, but research shows that most Canadians prefer to be cared for and to die at home2. Research has shown that, of provincial health care budgets, 10% is spent on patients in the last year of life3, with most of those costs being driven by hospital care4. Policymakers are investing in homecare nursing—and particularly palliative homecare nursing—because of its alignment with the preference of patients to be cared for and to die at home and its potential for cost savings by avoiding expensive acute hospitalizations.
The major gap in homecare research is a lack of multi-jurisdictional comparisons and costing analyses. Ontario research has demonstrated an association between increased hours of palliative nursing and a decreased likelihood that patients will be hospitalized or die in hospital in the last 2 weeks of life5. A U.K. study showed that patients receiving specialist end-of-life care nursing, via Marie Curie nurses specifically, were less likely to use late-life hospital care6. However, those studies were limited in that they did not examine cost savings and focused only on one health system, which brings into question their generalizability to other jurisdictions.
Comparing multiple jurisdictions across Canada is critical because, although each province has publicly-funded homecare systems, and most provinces have generalist homecare nurses who provide palliative care, those systems are organized differently, providing end-of-life nursing care in various ways7. For instance, in Ontario (ON), public employees provide single-entry coordinating services, but all nursing services are contracted to the private sector. In British Columbia (BC), all homecare nursing services and management are delivered by public employees. In Nova Scotia (NS), homecare management is conducted by public employees, and both public and private employees provide homecare nursing services. A multi-provincial cancer cohort study using data from those three provinces was therefore created to compare multiple jurisdictions using standardized definitions. Research findings from that study confirmed that increased palliative nursing hours are associated with decreased subsequent hospitalizations at end of life—and especially in the last month of life8.
The fact that the findings were consistent across the three provinces strongly supported the efficacy of palliative homecare nursing in diverse jurisdictions. However, that study did not examine costs. Indeed, little empirical evidence has described the cost effects of community-based palliative nursing care. Understanding those costs is especially important because, in some cases, substantial nursing time, which has its own associated costs, is required to support patients at home. A key gap in this knowledge is therefore an examination of the total costs of care that accounts for potentially reduced hospital costs and that includes the increased palliative nursing costs.
Building on the existing multi-provincial cancer cohort, we sought, in the present study, to examine the temporal associations of palliative nursing costs with subsequent hospitalization costs and with total costs in the last 6 months of life. The hypothesis was that, even when the hourly costs of palliative nursing were included, the total costs for patients receiving more nursing would be lower because of avoided or lowered (shorter length of stay) hospitalization costs. Such an investigation of the cost-savings potential of palliative homecare nursing is important in making a determination about whether supporting end-of-life patients at home is an efficient service that avoids unnecessary and expensive hospitalizations.
METHODS
Study Cohort
Our retrospective cohort study of end-of-life home care considered cancer decedents in the Canadian provinces of ON, NS, and BC during 5 fiscal years from 1 April 2004 to 31 March 2009. To be included, decedents had to be 19 years of age or older with a prior cancer diagnosis, a confirmed cancer cause of death in the provincial cancer registry9, and at least 1 record of homecare nursing with palliative intent (hereinafter called “palliative nursing”) after their cancer diagnosis and within 6 months of their date of death. “Palliative nursing” was defined as all visit-hours after the first identification of end-of-life care status based on provincial homecare database codes within the last 6 months of life. Homecare end-of-life status is given to those with a prognosis of “expected death within 6 months,” who are “not responsive to curative treatment and are dying,” and who have service goals “to alleviate distressing symptoms to achieve the best quality of life by providing complex support in the last stages of their illness”10. When a patient was diagnosed less than 6 months from death, only the time from diagnosis to death was examined.
Data Sources
Each province was responsible for accessing, linking, and analyzing its own provincial data. A national study protocol designed through group consensus was implemented by each province. Within each province, unique encrypted patient identifiers were derived from cancer registry data, which provided data for primary cancer type and date of cancer death11. The provincial cancer registry data were then linked with the other provincial administrative datasets. The Discharge Abstract Database maintained by the Canadian Institute for Health Information provided data concerning hospital admissions and comorbidity12; provincial homecare databases provided data on use of palliative nursing; and provincial health insurance databases provided information about the demographics of age at death, sex, and postal code (for income quintile, community size, and region)13,14.
Organization of Data
We aimed to examine the temporal association of the main exposure (palliative nursing costs) with the outcomes of interest (hospital costs and total costs) in a subsequent period. The data were therefore organized into 2-week blocks of time before death, resulting in a patient having a maximum of 13 blocks of data before death: block 13 being 6 months from death (weeks 26 and 25 from death), and block 1 being the block closest to death (weeks 2 and 1 from death)8,15. We chose the 2-week blocks based on an analysis of the average length of stay per hospitalization, which was approximately 8 days in the last month and 14 days in the other five months.
Outcomes of Interest
The first outcome of interest was the average hospitalization costs in a 2-week block of time. Hospital costs were determined using the resource intensity weight of each patient’s hospital stay, which indicates the case-mix severity and is calculated in the Discharge Abstract Database using the “case mix groups plus” methodology16–18. All provinces then multiplied the resource intensity weights by $5,269 (the Ontario cost per weighted case for 2008)18. The Ontario cost per weighted case data were used as the standard for all provinces to ensure comparability and consistency in the analysis. In NS, access to the 2008 resource intensity weights and the 2008 case mix groups plus standard was available for decedents only in fiscal year 2008–2009; thus, NS decedents from that year only were included in the analysis. Costs for an entire hospital stay were divided by the length of stay to determine the average daily cost of the hospitalization, allowing for the costs to be appropriately allocated to the corresponding 2-week blocks.
The second outcome of interest was the total cost, which is the total of the eligible observed hospital costs for patients in each 2-week block, plus the corresponding average palliative nursing costs in the preceding 2-week block. We categorized the actual total cost based on categories for the average cost of nursing time in a block [for example, >$87 to $174 (>1 to 2 hours of nursing)], and we present the data as the difference compared with the total cost for a reference group [that is, >$0 to $87 (>0 to 1 hours of palliative nursing in the block)]. The net difference in total cost compared with the reference is presented separately for the last 6 months of life and for the last month of life.
Main Exposure
The main exposure of interest was palliative nursing costs in a 2-week block of time, as already described. Those costs were calculated using the hourly ON visiting nursing costs of $86.47 in 2008–200916, which includes administrative overhead and travel. The ON values were used to ensure consistency and comparability across provinces. Palliative-intent nursing visits were measured in ON as time (hours/day), and in BC as a nursing visit received or in NS as a nursing visit authorized per defined period (typically, 28 days, although frequently re-evaluated during that period). To determine the nursing costs in each block in ON, hours per block were multiplied by the Ontario hourly cost. In BC and NS, the average number of daily visits within an authorized period was determined and allocated into 2-week blocks (that is, prorated). Visits were assumed to be 1 hour in duration, and the visit hours were then multiplied by the Ontario hourly cost.
Other Covariates
Other covariates included patient age, sex, primary cancer site (diagnosis closest to death), neighborhood income quintile, community size, and time closer to death (in 2-week blocks). We controlled for any Charlson comorbidity beyond cancer within a look-back period of 6 months for those with a diagnosis longer than 6 months (months 12–6 from death) or shorter than 6 months (6 months preceding the diagnosis)12.
Data Analyses
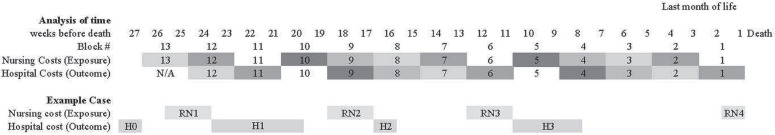
Applying a longitudinal costing method developed for mental health19 to palliative homecare, we examined the temporal association of palliative nursing costs in a 2-week block with the average hospitalization costs in the subsequent 2-week block. Thus, data were structured at the block level for each individual. For example, the analysis explored the relationship between the average palliative nursing costs in block 13 and the average hospitalization costs in block 12; the nursing costs in block 12 and the hospitalization costs in block 11; and so on until death occurred at the end of block 1. Hospitalization costs occurring before block 12 were outside the study window, and nursing costs in block 1 had no subsequent block for which to observe the outcome (hospitalization costs), and thus those nursing costs were not considered in the analysis. Moreover, whenever a hospitalization crossed more than 2 blocks (the patient was in the hospital for at least 1 entire block), it meant that the patient was not eligible for homecare nursing during that time (no exposure time). Blocks with no homecare exposure time were not eligible for analysis, and thus true hospital costs in blocks occurring after any non-eligible exposure blocks were not counted in the analysis. In other words, the maximum length of stay for which the study measured hospital costs was 27 days. Thus, our cost methods underestimate the true hospital costs. See Figure 1 for a sample case.
FIGURE 1.
Schematic of the approach used to analyze the temporal association between exposure (nursing costs in a 2-week block) and study outcome (hospital costs in a subsequent block) over time. All nursing costs in block 13 are associated with all hospital costs in block 12, all nursing costs in block 12 are associated with hospital costs in block 11, and so on, until death occurs at the end of block 1. The analysis of the last month of life includes the exposures in blocks 3 and 2 and the outcomes in blocks 2 and 1. The sample case shows a patient with 4 blocks of nursing visits and 3 hospitalizations. Note that H0 happened before the study window and is therefore not considered in the analysis. Each nursing visit is indicated by an RN number, and each hospitalization, by a sequential H number. For instance, in block 13 only half of RN1 is calculated, which is associated with the hospital costs in block 12 (in which only part of H1 is calculated); the remainder of RN1 is calculated in block 12, which is associated with the portion of the H1 hospital costs calculated in block 11. Because of being in hospital for the entire period represented by block 11, the patient was not eligible for nursing hours in the community, and that exposure block is thus ineligible; the part of H1 that falls in block 10 is therefore also excluded from the analysis. Later on, in block 9, the RN2 nursing costs are calculated and associated with any hospital costs in block 8 (H2). Farther on, in block 6, the costs of RN3 nursing are associated with hospital costs in the subsequent block (block 5), which occur as only partial H3 costs (that is, the first 2 weeks of the 3-week hospital stay are calculated in block 5). Again, the remainder of the H3 event costs occurring in block 4 are not counted because the patient was not eligible for nursing at any time in block 5. The RN4 event occurring in block 1 is not counted in our analysis, because there is no subsequent outcome block.
Nursing costs were categorized for analysis after a preliminary examination of the nursing cost distribution. The categories used were $0 (0 hours), more than $0 to $87 (>0 to 1 hours, which was the reference group), more than $87 to $174 (>1 to 2 hours), more than $174 to $348 (>2 to 4 hours), more than $348 to $522 (>4 to 6 hours), and more than $522 (>6 hours) for the last 6 months of life. In the last month of life, nursing costs were further stratified to include groups of more than $522 to $697 (>6 to 8 hours), more than $697 to $870 (>8 to 10 hours), and more than $870 (>10 hours).
Because hospital cost (to the nearest dollar) can be viewed as a count, we found that its histogram followed a Poisson distribution, especially because of the sizable proportion of blocks with zero hospitalizations20. We therefore applied a Poisson regression analysis in which the outcome was the hospital costs and the primary covariate was the palliative nursing costs (as a categorical variable). In addition, to account for block-to-block repeated measures from the same patient, we used a generalized estimating equations approach with an exchangeable correlation structure21. We also controlled for other covariates, as listed earlier. Two separate regressions were run: for the last 6 months of life and for the last month of life. The latter regression included exposure blocks 3 and 2, run on outcome blocks 2 and 1. The output from the regression analyses provided the observed average hospital cost per block for the various categories of nursing costs. We used the actual provincial average nursing costs per block within a category when calculating total cost. The study was approved by research ethics boards at McMaster University (ON), Capital Health (NS), and the BC Cancer Agency (BC).
RESULTS
The study included 58,022 cancer decedents from BC (n = 17,368), ON (n = 39,542), and NS (n = 1,112) who collectively received 1,573,453 palliative nursing hours (Table i). The cohort collectively used $757 million in true hospital costs during the last 6 months of life, of which $333 million (44%) was not included (that is, it came from blocks with no eligible nursing exposure time in preceding 2-week block). For this cohort, the age and sex distributions were similar across all three provinces: approximately half were women, and most were more than 70 years of age. Lung cancer was the most prevalent diagnosis in all three provinces, followed by colorectal cancer. Approximately 16% of the cohort had a Deyo-modified Charlson comorbidity score of 1 or more. Community sizes differed across the provinces: the NS population resided in smaller communities (<500,000 residents); ON was the only province with decedents from all five community sizes.
TABLE I.
Demographics of the study cohort
| Variable | British Columbia | Ontario | Nova Scotia | Overall | ||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||
| (n) | (%) | (n) | (%) | (n) | (%) | (n) | (%) | |
| Patients (n) | 17,368 | — | 39,542 | — | 1,112 | — | 58,022 | — |
| Age group | ||||||||
| 19–29 Years | 60 | 0.3 | 173 | 0.4 | 4 | 0.4 | 237 | 0.4 |
| 30–39 Years | 193 | 1 | 550 | 1 | 8 | 1 | 751 | 1 |
| 40–49 Years | 892 | 5 | 2,281 | 6 | 44 | 4 | 3,217 | 6 |
| 50–59 Years | 2,594 | 15 | 6,092 | 15 | 136 | 12 | 8,822 | 15 |
| 60–69 Years | 4,133 | 24 | 9,394 | 24 | 288 | 26 | 13,815 | 24 |
| 70–79 Years | 5,284 | 30 | 12,153 | 31 | 328 | 29 | 17,765 | 31 |
| 80–89 Years | 3,677 | 21 | 7,948 | 20 | 245 | 22 | 11,870 | 20 |
| ≥90 Years | 535 | 3 | 951 | 2 | 59 | 5 | 1,545 | 3 |
| Sex | ||||||||
| Female | 8,273 | 48 | 19,071 | 48 | 529 | 48 | 27,873 | 48 |
| Male | 9,095 | 52 | 20,471 | 52 | 583 | 52 | 30,149 | 52 |
| Cancer type | ||||||||
| Brain | 459 | 3 | 1,076 | 3 | 39 | 4 | 1,574 | 3 |
| Breast | 1,346 | 8 | 3,553 | 9 | 80 | 7 | 4,979 | 9 |
| Colorectal | 2,146 | 12 | 5,582 | 14 | 173 | 16 | 7,901 | 14 |
| Gynecologic | 766 | 4 | 2,030 | 5 | 43 | 4 | 2,839 | 5 |
| Head and neck | 452 | 3 | 1,075 | 3 | 24 | 2 | 1,551 | 3 |
| Hematologic | 1,159 | 7 | 2,360 | 6 | 62 | 6 | 3,581 | 6 |
| Lung | 4,806 | 28 | 10,496 | 27 | 303 | 27 | 15,605 | 27 |
| Other | 2,373 | 14 | 4,569 | 12 | 142 | 13 | 7,084 | 12 |
| Other gastrointestinal | 2,033 | 12 | 4,532 | 11 | 116 | 10 | 6,681 | 12 |
| Other genitourinary | 782 | 5 | 2,024 | 5 | 58 | 5 | 2,864 | 5 |
| Prostate | 1,046 | 6 | 2,245 | 6 | 72 | 6 | 3,363 | 6 |
| Income quintile | ||||||||
| 1 (lowest) | 3,684 | 21 | 7,740 | 20 | 227 | 20 | 11,651 | 20 |
| 2 | 3,590 | 21 | 8,537 | 22 | 248 | 22 | 12,375 | 21 |
| 3 | 3,337 | 19 | 7,677 | 19 | 224 | 20 | 11,238 | 19 |
| 4 | 3,354 | 19 | 7,710 | 19 | 198 | 18 | 11,262 | 19 |
| 5 (highest) | 3,403 | 20 | 7,878 | 20 | 215 | 19 | 11,496 | 20 |
| Charlson–Deyo modified comorbidity score | ||||||||
| 0 | 6,996 | 40 | 17,066 | 43 | 486 | 44 | 24,548 | 42 |
| ≥1 | 2,399 | 14 | 6,960 | 18 | 209 | 19 | 9,568 | 16 |
| Missinga | 7,973 | 46 | 15,516 | 39 | 417 | 38 | 23,906 | 41 |
| Fiscal year of death | ||||||||
| 2004–2005 | 4,273 | 25 | NA | NA | NA | NA | 4,273 | 7 |
| 2005–2006 | 3,437 | 20 | 9,139 | 23 | NA | NA | 12,576 | 22 |
| 2006–2007 | 3,515 | 20 | 10,078 | 25 | NA | NA | 13,593 | 23 |
| 2007–2008 | 3,674 | 21 | 10,093 | 26 | NA | NA | 13,767 | 24 |
| 2008–2009 | 2,469 | 14 | 10,232 | 26 | 1,112 | 100 | 13,813 | 24 |
| Community size | ||||||||
| <10,000 | 1,689 | 10 | 5,483 | 14 | 422 | 38 | 7,172 | 12 |
| 10,000–99,999 | 3,945 | 23 | 4,364 | 11 | 150 | 13 | 8,731 | 15 |
| 100,000–499,999 | 3,426 | 20 | 10,592 | 27 | 540 | 49 | 14,168 | 24 |
| 500,000–1,499,999 | NA | NA | 6,419 | 16 | NA | NA | 6,959 | 12 |
| ≥1,500,000 | 8,308 | 48 | 12,684 | 32 | NA | NA | 20,992 | 36 |
Cases in which patients had no hospitalizations from which to derive a Charlson score; in contrast, 0 indicates hospitalization billing codes that do not indicate a chronic disease.
NA = not applicable.
Relative Hospital Costs
Regression analysis in each province showed a statistically significant decrease in average relative hospital costs as nursing costs increased compared with the reference (equivalent cost of >0 to 1 hour nursing in a block) during the last 6 months of life (Table ii). The effect size varied by province: the range for the relative hospital cost decrease in BC was 24% (>1 to 2 hours) to 28% (>2 to 4 hours); the range in ON was 18% (>2 to 4 hours) to 27% (>1 to 2 hours); and NS showed significant decrease of 33% (>4 to 6 hours and >6 hours only). Moreover, blocks in which patients received no nursing were associated with a significant decrease in relative hospital costs of 69% in BC and 24% in ON. As patients approached closer to death, average relative hospital costs increased by approximately 20%.
TABLE II.
Factors associated with average hospital costs per blocka in the last 6 months of life
| Factor | British Columbia | Ontario | Nova Scotia | |||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| RR | CL | RR | CL | RR | CL | |
| Each block closer to death | 1.21 | 1.20, 1.22 | 1.18 | 1.18, 1.17 | 1.21 | 1.17, 1.25 |
| Nursing cost per block | ||||||
| $0 (0 hours) | 0.31 | 0.25, 0.37 | 0.76 | 0.72, 0.81 | 1.14 | 0.58, 2.22 |
| >$0–$87 (>0 to 1 hours) | Reference | Reference | Reference | |||
| >$87–$174 (>1 to 2 hours) | 0.76 | 0.71, 0.81 | 0.73 | 0.70, 0.76 | 0.78 | 0.58, 1.04 |
| >$174–$348 (>2 to 4 hours) | 0.72 | 0.67, 0.76 | 0.82 | 0.78, 0.86 | 1.02 | 0.77, 1.37 |
| >$348–$522 (>4 to 6 hours) | 0.75 | 0.69, 0.81 | 0.80 | 0.76, 0.85 | 0.67 | 0.50, 0.90 |
| >$522 (>6 hours) | 0.74 | 0.68, 0.80 | 0.77 | 0.73, 0.80 | 0.67 | 0.51, 0.88 |
| Age group | ||||||
| <30 Years | 1.99 | 1.34, 2.94 | 2.03 | 1.65, 2.49 | 7.52 | 4.26, 13.28 |
| 30–39 Years | 1.48 | 1.22, 1.78 | 1.66 | 1.46, 1.90 | 0.99 | 0.47, 2.10 |
| 40–49 Years | 1.45 | 1.30, 1.61 | 1.40 | 1.30, 1.49 | 1.11 | 0.71, 1.75 |
| 50–59 Years | 1.16 | 1.08, 1.25 | 1.21 | 1.15, 1.28 | 1.32 | 1.44, 1.94 |
| 60–69 Years | 1.10 | 1.03, 1.17 | 1.12 | 1.08, 1.17 | 1.32 | 1.32, 1.68 |
| 70–79 Years | Reference | Reference | Reference | |||
| 80–89 Years | 0.89 | 0.83, 0.95 | 0.84 | 0.80, 0.88 | 0.95 | 0.95, 1.26 |
| ≥90 Years | 0.71 | 0.61, 0.83 | 0.66 | 0.58, 0.75 | 0.63 | 0.63, 1.04 |
| Sex | ||||||
| Women | 1.08 | 1.02, 1.14 | 1.03 | 0.99, 1.07 | 0.92 | 0.74, 1.15 |
| Men | Reference | Reference | Reference | |||
| Comorbidity score | ||||||
| 0 | Reference | Reference | Reference | |||
| ≥1 | 1.11 | 1.04, 1.19 | 1.05 | 1.00, 1.10 | 1.02 | 0.88, 1.40 |
| Missing | 0.86 | 0.81, 0.90 | 0.79 | 0.77, 0.82 | 0.88 | 0.70, 1.10 |
| Community size | ||||||
| <10,0000 | Reference | Reference | Reference | |||
| 10,000–99,999 | 0.98 | 0.89, 1.07 | 0.98 | 0.93, 1.04 | 1.05 | 0.78, 1.41 |
| 100,000–499,999 | 0.78 | 0.71, 0.86 | 0.81 | 0.77, 0.85 | 0.90 | 0.73, 1.12 |
| 500,000–1,499,999 | NA | 0.76 | 0.72, 0.81 | NA | ||
| >1,500,000 | 1.04 | 0.96, 1.13 | 0.83 | 0.79, 0.87 | NA | |
Boldface type indicate statistical significance (<0.05). Also controlled for income quintile and cancer type (data not shown).
RR = relative rate of average hospital cost; CL = confidence limits; NA = not applicable.
In the last month of life generally, we observed an association between increasing nursing costs (compared with the reference group: >0 to 1 hours) and decreasing relative hospital costs, and a dose–response trend was evident (Table iii). For instance, as the nursing categories in ON increased compared with the reference (>1 to 2 hours, >2 to 4 hours, >4 to 6 hours, >6 to 8 hours, >8 to 10 hours, and >10 hours), the average relative hospital costs in the subsequent block decreased by 22%, 29%, 40%, 31%, 30%, and 55% respectively. Similar statistically significant and dose–response trends were observed across all nursing categories in BC. In NS, it was only in one nursing category (>10 hours) that we observed an association with relative hospital costs: a significant decrease of 38%. Moreover, when a given block had no associated nursing costs, we observed a statistically significant decrease in relative hospital costs in the subsequent 2-week block in BC and ON (67% and 47% respectively) and a statistically nonsignificant decrease in NS (13%).
TABLE III.
Factors associated with average hospital costs per blocka in the last month of life
| Factor | British Columbia | Ontario | Nova Scotia | |||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| RR | CL | RR | CL | RR | CL | |
| Each block closer to death | 1.92 | 1.85, 1.99 | 1.68 | 1.63, 1.73 | 2.10 | 1.84, 2.41 |
| Nursing cost per block | ||||||
| $0 (0 hours) | 0.33 | 0.28, 0.39 | 0.53 | 0.49, 0.56 | 0.87 | 0.50, 1.51 |
| >$0–$87 (>0 to 1 hours) | Reference | Reference | Reference | |||
| >$87–$174 (>1 to 2 hours) | 0.89 | 0.83, 0.95 | 0.78 | 0.74, 0.83 | 0.91 | 0.68, 1.23 |
| >$174–$348 (>2 to 4 hours) | 0.79 | 0.74, 0.84 | 0.71 | 0.67, 0.75 | 1.10 | 0.80, 1.52 |
| >$348–$522 (>4 to 6 hours) | 0.74 | 0.68, 0.80 | 0.60 | 0.56, 0.63 | 0.86 | 0.63, 1.19 |
| >$522–$697 (>6 to 8 hours) | 0.69 | 0.63, 0.76 | 0.69 | 0.64, 0.74 | 0.80 | 0.51, 1.26 |
| >$697–$870 (>8 to 10 hours) | 0.71 | 0.62, 0.81 | 0.71 | 0.65, 0.76 | 0.59 | 0.34, 1.02 |
| >$870 (>10 hours) | 0.71 | 0.63, 0.81 | 0.45 | 0.42, 0.48 | 0.62 | 0.45, 0.84 |
| Age group | ||||||
| <30 Years | 0.81 | 0.58, 1.14 | 1.86 | 1.46, 2.36 | 10.82 | 6.61, 17.72 |
| 30–39 Years | 1.33 | 1.11, 1.59 | 1.66 | 1.43, 1.92 | 1.49 | 0.72, 3.05 |
| 40–49 Years | 1.38 | 1.23, 1.55 | 1.47 | 1.36, 1.58 | 1.42 | 0.26, 2.18 |
| 50–59 Years | 1.13 | 1.04, 1.22 | 1.24 | 1.17, 1.31 | 1.28 | 0.96, 1.71 |
| 60–69 Years | 1.12 | 1.05, 1.20 | 1.12 | 1.07, 1.18 | 0.91 | 0.70, 1.17 |
| 70–79 Years | Reference | Reference | Reference | |||
| 80–89 Years | 0.90 | 0.84, 0.97 | 0.82 | 0.78, 0.87 | 0.63 | 0.47, 0.84 |
| ≥90 Years | 0.80 | 0.68, 0.94 | 0.71 | 0.62, 0.81 | 0.63 | 0.40, 1.00 |
| Sex | ||||||
| Women | 0.95 | 0.90, 1.01 | 0.98 | 0.94, 1.02 | 0.83 | 0.67, 1.03 |
| Men | Reference | Reference | Reference | |||
| Comorbidity score | ||||||
| 0 | Reference | Reference | Reference | |||
| ≥1 | 1.09 | 1.02, 1.17 | Reference | 0.95, 1.05 | 1.15 | 0.90, 1.47 |
| Missing | 0.92 | 0.87, 0.97 | 0.89 | 0.85, 0.93 | 0.89 | 0.71, 1.11 |
| Community size | ||||||
| <10,000 | Reference | Reference | Reference | |||
| 10,000–99,999 | 0.97 | 0.88, 1.06 | 1.05 | 0.99, 1.11 | 1.06 | 0.82, 1.38 |
| 100,000–499,999 | 0.81 | 0.73, 0.89 | 0.80 | 0.76, 0.85 | 0.91 | 0.74, 1.13 |
| 500,000–1,499,999 | NA | 0.64 | 0.60, 0.68 | NA | ||
| >1,500,000 | 1.06 | 0.97, 1.16 | 0.80 | 0.76, 0.84 | NA | |
Boldface type indicates statistical significance (<0.05). Also controlled for income quintile and cancer type (data not shown).
RR = relative rate of average hospital cost; CL = confidence limits; NA = not applicable.
When we examined other covariates in the last 6 months and last month of life, the covariates generally associated with relatively higher average relative hospital costs were age (<70 years) and a higher comorbidity score. Compared with lung cancer, sites associated with higher relative hospital costs were gynecologic, hematologic, other gastrointestinal, and other genitourinary cancers. Sex was not significantly associated with relative hospital costs. Income was not significantly associated with relative hospital costs, except in Ontario in the last month of life (with relative hospital costs increasing as income quintile decreased). Compared with communities of fewer than 10,000 people, larger community sizes (at and above the 100,000–499,999 population range) were generally associated with significantly lower average relative hospital costs.
Difference in Total Costs Compared with Reference
We examined the observed total cost (adding the hospital costs in a block to the homecare nursing costs in the preceding block) for all 13 blocks in the last 6 months of life and for the last month of life separately, stratified by nursing cost categories per block (Table iv). Of person–blocks that had hospital costs, the average hospital cost per block was $5,089 (interquartile range: $2,711–$8,848) in BC, $6,150 (interquartile range: $2,805–$8,630) in ON, and $5,576 (interquartile range: $2,699–$9,333) in NS.
TABLE IV.
Observed differences in total costs (hospital plus nursing costs) per blocka
| Resource use | British Columbia | Ontario | Nova Scotia | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||||||||
| Blocks (n) | Average nursing cost per block | Observed average hospital cost per block | Standard deviation of average hospital cost per block | Difference in total cost per block compared with reference | Blocks (n) | Average nursing cost per block | Observed average hospital cost per block | Standard deviation of average hospital cost per block | Difference in total cost per block compared with reference | Blocks (n) | Average nursing cost per block | Observed average hospital cost per block | Standard deviation of average hospital cost per block | Difference in total cost per block compared with reference | |
| Last 6 months of life | |||||||||||||||
| $0 (0 hours) | 3,644 | $0 | $783 | $2,618 | −$884 | 32,155 | $0 | $1,185 | $3,381 | −$295 | 95 | $0 | $2,551 | $4,741 | $1,048 |
| >$0 to $87 (>0 to 1 hours) | 18,264 | $49 | $1,618 | $3,649 | Reference | 48534 | $86 | $1,393 | $3,635 | Reference | 935 | $58 | $1,445 | $3,409 | $0 |
| >$87 to $174 (>1 to 2 hours) | 24,448 | $131 | $1,186 | $3,063 | −$349 | 49406 | $173 | $1,024 | $2,937 | −$282 | 1,339 | $157 | $1,268 | $2,977 | −$77 |
| >$174 to $348 (>2 to 4 hours) | 31,143 | $247 | $1,152 | $2,946 | −$267 | 27983 | $310 | $1,184 | $3,243 | $14 | 602 | $249 | $193 | $3,636 | −$1,060 |
| >$348 to $522 (>4 to 6 hours) | 11,682 | $423 | $1,307 | $3,045 | $63 | 57501 | $478 | $1,202 | $3,099 | $200 | 1,092 | $419 | $1,077 | $267 | −$6 |
| >$522 (>6 hours) | 8,823 | $791 | $1,499 | $3,335 | $624 | 32155 | $1,300 | $1,223 | $3,189 | $1,043 | 1,305 | $1,153 | $1,392 | $2,984 | $1,042 |
| Last month of life | |||||||||||||||
| $0 (0 hours) | 1,621 | $0 | $1,058 | $3,033 | −$2,750 | 6,020 | $0 | $1,851 | $4,214 | −$1,637 | 40 | $0 | $3,321 | $4,032 | −$356 |
| >$0 to $87 (>0 to 1 hours) | 4,391 | $49 | $3,759 | $5,100 | Reference | 8810 | $86 | $3,402 | $5,388 | Reference | 189 | $53 | $3,624 | $5,216 | $0 |
| >$87 to $174 (>1 to 2 hours) | 5,297 | $132 | $2,986 | $4,463 | −$689 | 11924 | $173 | $2,669 | $4,491 | −$646 | 306 | $153 | $3,064 | $4,103 | −$460 |
| >$174 to $348 (>2 to 4 hours) | 7,907 | $251 | $2,478 | $4,052 | −$1,079 | 8037 | $308 | $2,460 | $4,498 | −$720 | 204 | $248 | $3,534 | $4,540 | $105 |
| >$348 to $522 (>4 to 6 hours) | 3,753 | $426 | $2,258 | $3,793 | −$1,124 | 4135 | $478 | $2,134 | $3,908 | −$877 | 279 | $425 | $2,422 | $3,654 | −$830 |
| >$522 to $697 (>6 to 8 hours) | 1,791 | $598 | $2,089 | $3,634 | −$1,121 | 2892 | $644 | $2,439 | $4,271 | −$406 | 93 | $607 | $2,514 | $3,778 | −$556 |
| >$697 to $870 (>8 to 10 hours) | 917 | $773 | $2,201 | $3,918 | −$833 | 13013 | $821 | $2,550 | $4,388 | −$118 | 63 | $787 | $1,870 | $3,126 | −$1,020 |
| >$870 (>10 hours) | 983 | $1,244 | $2,188 | $4,174 | −$376 | 6020 | $1,802 | $1,612 | $3,592 | −$75 | 341 | $1,426 | $2,142 | $3,532 | −$109 |
Boldface type reflects a lower total cost per patient in a 2-week block compared with the reference cost (patients receiving 1 hour of nursing in a 2-week block).
Compared with the reference (equivalent cost of >0 to 1 nursing hours), total cost in the last 6 months of life was consistently lower only for blocks having more than 1 to 2 nursing hours [range: decreased by $77 (NS) to $349 (BC)]. For blocks with more than 6 nursing hours, total cost was, compared with the reference, consistently higher in all three provinces, ranging from $624 (BC) to $1,043 (ON) more.
However, in the last month of life in all three provinces, the total cost was consistently lower than the reference in blocks with more nursing hours, although no dose–response trend was observed. For ON, the range was a total cost that was decreased by $75 (>10 hours) to $877 (>4 to 6 hours). For BC, the range was a total cost that was decreased by $376 (>10 hours) to $1,124 (>4 to 6 hours). For NS, the range was a total cost that was decreased by $109 (>10 hours) to $1,020 (>8 to 10 hours). An exception occurred in NS, where more than 2 to 4 hours of nursing was associated with a total cost that was higher by $105 compared with the reference. In all three provinces, blocks with no nursing costs consistently resulted in a lower total cost than occurred for the reference, ranging from a total cost that was decreased by $356 (NS) to $2,750 (BC).
We also used a Poisson model to predict the average hospital costs of a patient in each nursing category; the resulting costs were very similar to the observed costs (data not shown).
DISCUSSION
This multi-provincial observational cohort study of cancer decedents shows a temporal association between increased palliative homecare nursing costs in a 2-week block compared with a reference group (>0 to 1 hours of palliative nursing) and decreased relative hospital costs in a subsequent 2-week block, sometimes in the last 6 months of life and almost always in the last month of life. Those results confirmed our hypothesis: in all three provinces, an increase palliative homecare nursing was associated with an overall lower total cost, but only in the last month of life. To our knowledge, the present cohort study is the largest to examine the relationship between palliative nursing costs and subsequent hospital costs across multiple health systems.
Related studies examining home-based palliative care programs delivered within the U.S. Medicare hospice benefit also demonstrated cost savings22–24. Those studies used propensity score matching to identify appropriate control groups; however, they did not differentiate the particular effect of palliative home nursing services, and results were specific to the United States, which requires a beneficiary to forego acute-care services before accessing the hospice benefit25. One international meta-analysis review that focused on specialist palliative care home nursing services found, because of heterogeneity in study quality and cost definitions, inconclusive evidence of cost savings26.
Our study adds to the literature by being multi-jurisdictional, with consistent definitions, and using a temporal association and dose–response design to add credibility with respect to the direct effect of home nursing on subsequent hospitalizations. Unlike the U.S. studies, which found cost savings for long enrolment periods of 105 days22,23, the cost savings in our study were observed mostly during the last month of life. Our findings might be more generalizable to countries with a similar single-payer health care system, such as the European Union, the United Kingdom, or Australia.
That we observed a consistently lower total cost in three provinces is noteworthy. Our data show that the reference group (>0 to 1 hours of nursing in a 2-week block) generally had the highest hospital costs in the subsequent 2-week block. That observation supports the notion that too few nursing services, when required, lead to a more costly hospitalization. Moreover, in the last month of life, a lower total cost was evident even when the most palliative nursing hours were delivered (equivalent to 14 hours per block in BC, 21 hours per block in ON, and 16 hours per block in NS), although the cost savings were smallest compared with other categories.
Although we detected moderate-to-large relative reductions in average hospital costs as nursing costs increased, the difference translated into only several hundreds to a thousand dollars of total-cost difference. On the one hand, our study underestimates the true hospital costs. Specifically, only 56% ($424 million) of true hospital costs were included; the costs excluded came from lengthy hospital stays resulting in 2-week blocks with no nursing time exposure. On the other hand, that observation partly suggests that the hospital costs at end of life might not be as expensive as previously thought—mainly because patients do not spend most of that time in hospital. Hospital costs were $0 in 80% of blocks in the last 6 months of life and in 63% of blocks in the last month of life, thus greatly decreasing the overall average cost. Also in our data, terminal hospitalizations lasted only an average of 1 week, shorter than length of hospital stays observed in earlier months. An alternative explanation might be that these patients occupy a valuable hospital bed at end of life, but do not undergo expensive procedures. Instead, greater end-of-life costs might be incurred earlier in the disease trajectory, in the form of heroic treatments such as expensive surgeries or chemotherapy drugs.
Consistent with other research5,8, our study shows that, compared with the reference group, a lack of nursing in a given block was also associated with lower relative hospital costs in the subsequent block and a lower total cost. This group of patients is distinct, given that they received no palliative nursing services that might prevent subsequent hospitalizations. We hypothesize that patients receiving no nursing were less medically complex or had sufficient caregiver support, both factors being associated with less hospitalization27. They could also have been in a quiescent period in the progression of their illness or in a residential hospice (although, because of a shortage of facilities, only 2% of all deaths in Ontario occur in a hospice). Such factors might produce sporadic users—that is, patients who use a nursing service and then do not use such services in subsequent weeks.
Our study had several limitations. Our cohort was cancer-focused; results might not be generalizable to non-cancer diagnoses. There is a potential for underreporting or delayed initiation of homecare nursing with palliative intent, which would lead to a selection bias in patients. To have a standard comparison, we used ON cost estimates in the analyses for all three provinces, but ON costs might not be representative of the true costs in BC or NS. Our analysis does not include the costs of services that might be required to support care at home, such as physician services, drugs, nursing supplies, generalist homecare nursing without palliative intent, or privately-funded homecare services; such costs would have to be calculated to comprehensively estimate the true cost savings potential. However, within our study parameters, our cost-savings estimates are conservative, because they exclude hospital costs in blocks with no nursing time exposure in the preceding block, and because the ON nursing cost standard is the most expensive in the country. We were not able to include important covariates such as quality of care or patient preferences or caregiver availability. The sample size in NS might not have been sufficient to detect the same significant trends observed for BC or ON for several outcomes. Finally, our study examined a temporal association over a very large cohort, but that association is not causal. Additional sensitivity analyses using different time intervals are required to confirm our results and to validate hours authorized in BC and NS with respect to hours actually delivered. Future research is required to examine what constitutes the right level of care and to identify the contextual factors that influence both patterns of home nursing hours and overall hospitalization costs.
CONCLUSIONS
Our multi-provincial cancer decedent cohort shows that, compared with the receipt of more than 0 to 1 hours of palliative nursing in a 2-week block, receipt of more palliative nursing hours is associated with lower relative hospital costs in the subsequent 2-week block, and a lower total cost over the entire 4-week period. This research is important to support the cost-savings potential of increased community-based palliative care. The results indicate that investing more financial resources into palliative homecare nursing services could potentially lead to cost savings from either shorter or avoided hospitalizations, even when accounting for the additional costs of increased nursing.
ACKNOWLEDGMENTS
The authors thank Ying Liu for analysis, and Drs. Melissa Brouwers and Jonathan Sussman for support in the overall study. This study was funded by a grant from the Canadian Cancer Society Research Institute (no. 700689) and was also supported by the Canadian Centre for Applied Research in Cancer Control (Canadian Cancer Society Research Institute grant no. 019789). The study used databases maintained by the Institute for Clinical Evaluative Sciences, which receives funding from the Ontario Ministry of Health and Long-Term Care. The BC Cancer Agency and the British Columbia Ministry of Health approved access to and use of the data held by Population Data BC for this study. Portions of the data used in this report were made available by the Nova Scotia Department of Health and Wellness and the Population Health Research Unit (now known as Health Data Nova Scotia) of Dalhousie University. The opinions, results, and conclusions reported in this paper are those of the authors and are independent from the funding and data-provision sources.
CONFLICT OF INTEREST DISCLOSURES
We have read and understood Current Oncology’s policy on disclosing conflicts of interest, and we declare that we have none.
REFERENCES
- 1.Canadian Institute for Health Information (cihi) End-of-Life Hospital Care for Cancer Patients. Ottawa, ON: CIHI; 2013. [Google Scholar]
- 2.Brazil K, Howell D, Bedard M, Krueger P, Heidebrecht C. Preferences for place of care and place of death among informal caregivers of the terminally ill. Palliat Med. 2005;19:492–9. doi: 10.1191/0269216305pm1050oa. [DOI] [PubMed] [Google Scholar]
- 3.Tanuseputro P, Wodchis WP, Fowler R, et al. The health care cost of dying: a population-based retrospective cohort study of the last year of life in Ontario, Canada. PLoS One. 2015;10:e0121759. doi: 10.1371/journal.pone.0121759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cheung MC, Earle CC, Rangrej J, et al. Impact of aggressive management and palliative care on cancer costs in the final month of life. Cancer. 2015;121:3307–15. doi: 10.1002/cncr.29485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Seow H, Barbera L, Howell D, Dy SM. Using more end-of-life homecare services is associated with using fewer acute care services: a population-based cohort study. Med Care. 2010;48:118–24. doi: 10.1097/MLR.0b013e3181c162ef. [DOI] [PubMed] [Google Scholar]
- 6.Chitnis XA, Georghiou T, Steventon A, Bardsley MJ. Effect of a home-based end-of-life nursing service on hospital use at the end of life and place of death: a study using administrative data and matched controls. BMJ Support Palliat Care. 2013;3:422–30. doi: 10.1136/bmjspcare-2012-000424. [DOI] [PubMed] [Google Scholar]
- 7.Canadian Healthcare Association . Home Care in Canada: From the Margins to the Mainstream. Ottawa, ON: Canadian Healthcare Association; 2009. [Google Scholar]
- 8.Seow H, Sutradhar R, McGrail K, et al. End-of-life cancer care: temporal association between homecare nursing and hospitalizations. J Palliat Med. 2015. [Epub ahead of print]. [DOI] [PubMed]
- 9.Clarke EA, Marrett LD, Kreiger N. Cancer registration in Ontario: a computer approach. IARC Sci Publ. 1991:246–57. [PubMed] [Google Scholar]
- 10.Canadian Institute for Health Information (cihi) Development of National Indicators and Reports for Home Care: Phase 2 Indicator Descriptions. Ottawa, ON: CIHI; 2002. [Google Scholar]
- 11.Canadian Institute for Health Information (cihi) Data Quality of the Discharge Abstract Database Following the First-Year Implementation of ICD-10-CA/CCI. Ottawa, ON: CIHI; 2004. [Google Scholar]
- 12.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with icd-9-cm administrative databases. J Clin Epidemiol. 1992;45:613–19. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 13.Statistics Canada . Annual Demographic Estimates: Subprovincial Areas, 2007 to 2012. Ottawa, ON: Statistics Canada; 2010. [Google Scholar]
- 14.Wilkins R. PCCF+ Version 3G User’s Guide. Ottawa, ON: Statistics Canada; 2001. [Google Scholar]
- 15.Seow H, Barbera L, Pataky R, et al. J Pain Symptom Manage. 2015. Does increasing home care nursing reduce emergency department visits at the end of life? A population-based cohort study of cancer decedents. pii:S0885–3924(15)00572–2. [DOI] [PubMed] [Google Scholar]
- 16.Wodchis W, Bushmeneva K, Nikitovic M, McKillop I. Guidelines on Person-Level Costing Using Administrative Databases in Ontario. Toronto, ON: Health System Performance Research Network; 2012. [Google Scholar]
- 17.Canadian Institute for Health Information (cihi) The Cost of Hospital Stays: Why Costs Vary. Ottawa, ON: CIHI; 2008. [Google Scholar]
- 18.Canadian Institute for Health Information (cihi) Canadian MIS Database: Hospital Financial Performance Indicators, 2208–2009 to 2012–2013. Ottawa, ON: CIHI; 2015. [Google Scholar]
- 19.Cui Z, Faries DE, Shen W, Able SL, Novick D. Longitudinal analysis of healthcare costs: a case study of patients with major depressive disorder treated with duloxetine. J Med Econ. 2013;16:623–32. doi: 10.3111/13696998.2013.778267. [DOI] [PubMed] [Google Scholar]
- 20.Barber J, Thompson S. Multiple regression of cost data: use of generalised linear models. J Health Serv Res Policy. 2004;9:197–204. doi: 10.1258/1355819042250249. [DOI] [PubMed] [Google Scholar]
- 21.Liang KY, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22. doi: 10.1093/biomet/73.1.13. [DOI] [Google Scholar]
- 22.Kelley AS, Deb P, Du Q, Aldridge Carlson MD, Morrison RS. Hospice enrollment saves money for Medicare and improves care quality across a number of different lengths-of-stay. Health Aff (Millwood) 2013;32:552–61. doi: 10.1377/hlthaff.2012.0851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Taylor DH, Jr, Ostermann J, Van Houtven CH, Tulsky JA, Steinhauser K. What length of hospice use maximizes reduction in medical expenditures near death in the US Medicare program? Soc Sci Med. 2007;65:1466–78. doi: 10.1016/j.socscimed.2007.05.028. [DOI] [PubMed] [Google Scholar]
- 24.Kerr CW, Donohue KA, Tangeman JC, et al. Cost savings and enhanced hospice enrollment with a home-based palliative care program implemented as a hospice–private payer partnership. J Palliat Med. 2014;17:1328–35. doi: 10.1089/jpm.2014.0184. [DOI] [PubMed] [Google Scholar]
- 25.United States Department of Health and Human Services . Code of Federal Regulations. Washington, DC: Government Publishing Office; 2000. Hospice care. Title 42. Sec. 418.1. [Google Scholar]
- 26.Luckett T, Davidson PM, Lam L, Phillips J, Currow DC, Agar M. Do community specialist palliative care services that provide home nursing increase rates of home death for people with life-limiting illnesses? A systematic review and meta-analysis of comparative studies. J Pain Symptom Manage. 2013;45:279–97. doi: 10.1016/j.jpainsymman.2012.02.017. [DOI] [PubMed] [Google Scholar]
- 27.Higginson IJ, Sarmento VP, Calanzani N, Benalia H, Gomes B. Dying at home—is it better: a narrative appraisal of the state of the science. Palliat Med. 2013;27:918–94. doi: 10.1177/0269216313487940. [DOI] [PubMed] [Google Scholar]