Abstract
Background
Despite the fact that there is a large amount of research on childhood attention deficit hyperactivity disorder (ADHD) treatment and an increasing amount of research on adult ADHD, little is known about the prevalence and influence of parental ADHD. Therefore, this study examined the frequency of parental ADHD in a clinical sample of German children suffering from ADHD. We also tried to find different levels of symptom severity for prognostic relevance. Furthermore, the association between subtypes of ADHD in children and their parents was investigated.
Method
In this study, parents of 79 ADHD children were screened for ADHD according to the Diagnostic and Statistical Manual of Mental Disorders, 5th edition and International Classification of Diseases, 10th edition. The Wender Utah Rating Scale and the ADHS-Self-Report were given to 75 mothers and 49 fathers for retrospective and current symptoms. Frequency of ADHD symptoms and severity groups was calculated and relationship between parental and children’s ADHD was tested.
Results
ADHD occurrence for mothers of children with ADHD was 41.3%, for fathers 51.0%. About 16.0% of the mothers had a mixed type, 9.3% had a hyperactive-impulsive subtype, and 16.0% had an inattentive subtype. Of the fathers, 18.4% had a mixed type, 10.2% had a hyperactive-impulsive subtype, and 22.4% had an inattentive subtype; 61% of the mothers and 46.9% of the fathers had low symptom severity. Medium symptom severity was reported by 37.7% mothers and 46.9% fathers, while 1.3% of the mothers and 6.2% of the fathers showed severe symptoms. No significant correlation between parental and child diagnoses was observed.
Conclusion
As nearly half of the parents suffered from ADHD, these results are a matter of concern in families with ADHD children. Besides parent–child interactions, parental ADHD symptoms might influence parental education style and also effects parent training as well as the child’s therapy outcome. In the future, parents should be screened for ADHD symptoms if they or their child receive treatment and to adjust processes and design of treatment to the symptoms.
Keywords: attention deficit hyperactivity disorder, adult, parents, frequency, DSM-5, ICD-10
Introduction
Attention deficit hyperactivity disorder (ADHD) is a high prevalence psychiatric disorder, with a worldwide prevalence of 5.29% for children and adolescents and 4.4% in adulthood.1,2 Individuals with ADHD are at high risk for developing other psychiatric comorbidities in childhood, adolescence, and adulthood.3–5 Boys are twice as likely to be affected with ADHD than girls.6,7
In general, the pathogenesis of ADHD is assumed to be multifactorial influenced by genetic and environmental factors.8,9 Previous studies failed to show substantial and significant correlations between ADHD subtypes in families.10–12 They, therefore, suggest a unique genetic cause for ADHD and nonfamilial, environmental causes for different symptoms focus and subtype. Relevant environmental factors are psychosocial factors such as lower socioeconomic status, maternal psychiatric disorder, and family dysfunction.13–16 Notably, these factors tend to serve as universal predictors for children’s mental health rather than being specific to ADHD.8,17 Furthermore, coercive child–parent interactions take place more in families with ADHD children: parents give more verbal directions and repeated commands, communicate negatively more frequently, and are less responsive than parents of children without ADHD.18–22 Biological factors like maternal smoking, drug and alcohol exposure during pregnancy, and low birth weight also contribute to ADHD.23–26
ADHD symptoms tend to change over time with waning hyperactivity and impulsivity, but rather persisting inattention.27 During childhood, more motor activity, shorter duration of play, higher frequency of activity shifts, more oppositional behavior, and less social skills are reported.20,28–30 In addition, these children suffer from distractibility, school problems, low achievement motivation, rejection from peers, and low self-esteem.31–33 In adolescence, they reveal less hyperactivity but internal fidgetiness, persisting inattention, emotional problems, aggressive, dissocial, and alcohol/drug problems.31,34 Adults with ADHD show a higher divorce rate, have more interpersonal conflicts, suffer from emotional dysregulation, and report more problems in organizing and planning activities, more car accidents, and more drug and alcohol problems than healthy adults.35–37
In 41%–55% of the families with at least one child with ADHD, at least one parent is also affected.12,38 Based on high heritability and chronification, the disorder frequently affects both children and their parents. Parental ADHD influences family functioning, parenting, and the quality of life of their children.39–43 Inattention and impulsivity are especially suggested to impair parenting by leading to impaired organizational skills.44 Families with parents suffering from ADHD show less structure in everyday life. This mediated a positive association between parental ADHD symptoms and inconsequent discipline, involvement, and unsupportive responses to expressed negative emotions of the child.45
Therapy of children and adolescents suffering from ADHD includes psychoeducation, parent training, school intervention, psychopharmacological or behavior therapy.46,47 According to the National Institute for Health and Clinical Excellence, parent training is the first-line treatment for preschool children, school-age children, and adolescents with mild-to-moderate ADHD.48
Parental ADHD might not only affect family functioning, but also treatment utilization and outcome of child therapy or parent training.42 Several studies imply that parent training for ADHD children is less effective for parents suffering from ADHD.18,49,50 Parent training was effective in changing behavior in ADHD children for mothers with low and medium ADHD symptoms, but not for mothers suffering from high ADHD symptoms.49 Mothers with higher levels of ADHD perceived less change in their ADHD children’s disruptive behavior after brief parent training.50
To date, lots of treatment studies have focused either on parents of children with ADHD51–54 or adults with ADHD themselves.55–57 Comparatively, few have examined samples of affected parents,58–63 even though about half of the ADHD children have at least one ADHD parent.12,38 Effects of pharmacotherapy on parenting vary across different trials and measures, for example, ADHD mothers reported medium to large effects on inconsistent discipline and involvement with methylphenidate,59 which could not be observed by clinicians.60 There were no interaction effects of behavioral parent training and pharmacotherapy.58 Furthermore, prevalence of children with ADHD receiving a treatment and having parents with ADHD is lacking. Therefore, the aim of this study was to evaluate the magnitude and severity of parental ADHD in a German clinical sample of children with ADHD. For this clinical sample, we first hypothesized parental ADHD in most of the households with affected children.12 Second, based on previous findings, we expected to find equally sized groups of parents with low, medium, and high levels of ADHD symptoms according to the distribution found by Sonuga-Barke et al.49 Third, we expected no significant relationship between the ADHD subtypes of the children and their parents.12
Method
Study sample
The sample consisted of 79 children and adolescents suffering from ADHD and their mothers and fathers from Germany who started outpatient treatment in a social pediatrics center. Only children and adolescents diagnosed with ADHD based on International Classification of Diseases, 10th edition (ICD-10) criteria,64 by attending professional psychotherapist, were included in the present study, either as having a mixed subtype (F90.0: “Disturbance of activity and attention,” F90.1: “Hyperkinetic conduct disorder”) or a predominantly inattentive subtype (F98.8: “Other specified behavioral and emotional disorders with onset usually occurring in childhood and adolescence”). Children with physical illness or comorbid psychiatric disorders were excluded. The subjects’ sex, age, medication, and distribution of diagnoses are shown in Table 1.
Table 1.
Sex, age, and medication for the participating children and adolescents according to ICD-10
| Group | Sum | Sex | Age, years | Medication | |
|---|---|---|---|---|---|
|
|
|
|
|||
| N (%) | Male (%) | Female (%) | M (SD) | N (%) | |
| Mixed subtype | 58 (73.4) | 49 (62.0) | 9 (11.4) | 11.05 (2.57) | 22 (37.9) |
| Inattentive subtype | 21 (26.6) | 14 (18.0) | 7 (8.6) | 11.31 (2.69) | 7 (33.33) |
| Total | 79 (100.0) | 63 (80.0) | 16 (20.0) | 11.12 (2.59) | 29 (36.7) |
Abbreviations: ICD-10, International Classification of Diseases, 10th edition; M, mean; N, total number; SD, standard deviation.
Most of the participating children lived with both of their parents (63.3%), 33.8% lived with one parent after a divorce. The remaining children lived with their grandparents (2.9%).
Participation in this study included the completion of these psychological questionnaires by parents and participation was absolutely voluntary. Furthermore, parents were prior adequately informed of the aims, methods, any possible conflicts of interest, institutional affiliations of the psychologists, the anticipated benefits and potential risks of the study and the discomfort it may entail, post-study provisions, and any other relevant aspects of the study. They were informed that participation in this project was independent to treatment and that they had the right to refuse to participate in the study or to withdraw consent to participate at any time without reprisal. Psychologists ensured that the parents had understood the information, afterwards, the psychologist sought the potential subject’s freely-given written informed consent. In addition, all parents were informed about the opportunity of getting information about the general outcome and results of the study.
The psychologist was not involved in any therapy or otherwise dependent relationship with the parents. Only subjects who were capable of giving informed consent were included. The psychologists had fully informed the parents concerning the questionnaires and that this project was not a part of any treatment. In addition, the parents were informed that the refusal to participate or their decision to withdraw from the study had no effect on any other aspects as treatment or patient-physician relationship. The study was conducted according to standard ethical guidelines as defined by the Declaration of Helsinki. The Institutional Review Board did not require additional ethical approval because the data were selected from a standardized diagnostic procedure. A total of 180 questionnaires were handed out, of these 79 families with at least questionnaires of one parent were given back. The response rate was 43.89%. Cases with completed forms from at least one parent were admitted to the study. In the rare case of forgotten items, we utilized mean value replacement to build proper sum scores.
Diagnostic measures
Wender Utah Rating Scale
The WURS-K65 is the German short version of the Wender Utah Rating Scale.66 The scale is a self-assessment tool for the retrospective assessment of the presence and severity of ADHD in childhood (age 8–10 years). It comprises 25 items, of which 21 refer to ADHD (inattention, hyperactivity, impulsivity, emotional dysregulation, temper, affective lability, emotional overreactivity, and disorganization) and four serve as control items. Adults rated themselves on a 5-point Likert scale ranging from 0 (not at all or very slightly) to 4 (very much). At a cutoff score of 30 or higher, sensitivity was 85% and specificity was 76%. The scale manifested excellent internal consistence (α=0.91) and a split-half correlation of r12 =0.85.67
ADHS-Selbstbeurteilungsskala
The ADHS-Self-Report (ADHS-SB)68 is a self-report tool based on the 18 ICD-1064 research and the Diagnostic and Statistical Manual of Mental Disorders, 4th edition criteria.69 Eighteen items cover inattention, impulsivity, and hyperactivity and four additional items cover age of onset, generalization, and subjective affliction on a 4-point Likert scale. According to the authors, a cutoff score of 15 provides a sensitivity of 77% and a specificity of 75%. Retest-reliability (r=0.80) and internal consistence (α=0.90) are good.68 In this study, we used the ADHS-SB to evaluate ADHD symptoms according to Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5).70 We used DSM-5 criteria as they better determine adults with ADHD even if they no longer show all of their childhood symptoms due to developmental maturing or compensation. The 18 requested core symptoms remained the same from Diagnostic and Statistical Manual of Mental Disorders, 4th edition to DSM-5. However, in the new version, five instead of six symptoms in one domain are requested for diagnosis.
Statistical analyses
For all analyses, SPSS version 21.0 (IBM Corporation, Armonk, NY, USA) was used. We tested for Gaussian distribution of all relevant variables using the Kolmogorov–Smirnov test. The level of significance was set at α≤0.05. All variables were normally distributed. Chi-square test was used for the categorical variables and unpaired sample t-test for numeric variables.
Results
To examine the frequency of parental ADHD symptomatology in our study sample, we first analyzed the sum scores of the WURS-K according to sex in mothers and fathers. For mothers (n=75), a mean of M=22.42 (standard deviation [SD] =10.99) was found for the sum score of the WURS-K, while fathers (n=49) showed a mean of M=25.83 (SD =13.92). An unpaired t-test revealed no significant differences between mothers and fathers (P=0.253; dCohen=0.279). The separate analysis of the WURS-K for mothers and fathers revealed that 49.1% of the fathers scored above the cut-off (≥30) for ADHD symptomatology in childhood, while 27.3% of the mothers scored above the cut-off (Figure 1). This difference was significant (χ2 (1)=6.600; P=0.017).
Figure 1.
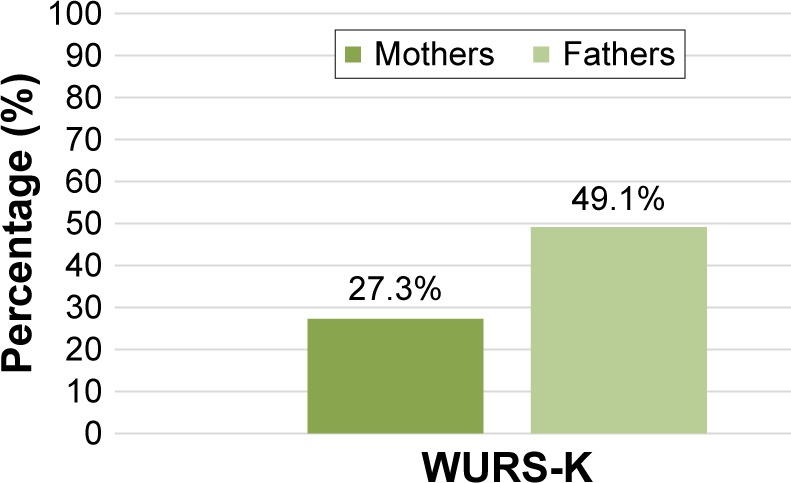
Prevalence of parents above the cut-off for retrospective ADHD symptoms (WURS-K).
Abbreviations: ADHD, attention deficit hyperactivity disorder; WURS-K, Wender Utah Rating Scale.
For current ADHD symptomatology (ADHS-SB), mothers reported a mean of M=12.17 (SD =10.54) and fathers a mean of M=14.56 (SD =12.67). This result was not significantly different between mothers and fathers (P=0.125; dCohen=0.209). However, about 43.1% of fathers and 33.8% of mothers scored above the cut-off (≥15; Figure 2). The difference between mothers and fathers concerning their current ADHD symptomatology was not significant (χ2 (1)=1.150; P=0.352). Results are displayed in Table 2.
Figure 2.
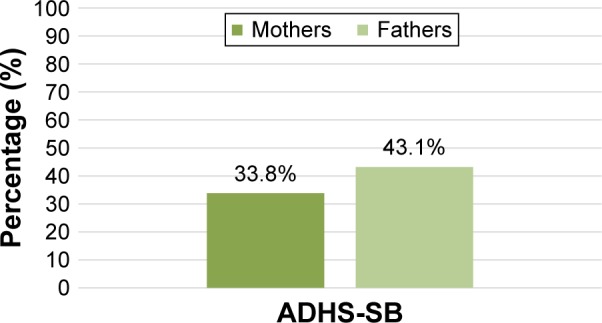
Prevalence of parents above the cut-off current ADHD symptoms (ADHS-SB).
Abbreviations: ADHD, attention deficit hyperactivity disorder; ADHS-SB, ADHS-Selbstbeurteilungsskala.
Table 2.
ADHD symptomatology in mothers and fathers
| Mothers
|
Fathers
|
|||||
|---|---|---|---|---|---|---|
| M (SD) | ≥Cut-off (%) | M (SD) | ≥Cut-off (%) | P for mean | P for cut-off | |
| WURS-K | 22.42 (10.99) | 27.3 | 25.83 (13.92) | 49.1 | 0.253 | 0.017 |
| ADHS-SB | 12.17 (10.54) | 33.8 | 14.54 (12.67) | 43.1 | 0.125 | 0.352 |
Abbreviations: ADHD, attention deficit hyperactivity disorder; ADHS-SB, ADHS-Self-Report; M, mean; SD, standard deviation; WURS-K, Wender Utah Rating Scale.
Regarding the aggregated frequency of ADHD symptomatology for parents above the cut-off criteria of the ADHS-SB and WURS-K, we revealed a high incidence for ADHD symptoms in childhood (36.4%; WURS-K) as well as current ADHD symptomatology (37.5%; ADHS-SB).
To distinguish between parents with low, medium, and high symptomatology, we split the total score of the ADHS-SB into three groups according to Sonuga-Barke et al49: low symptomatology (0–7 symptoms present), medium symptomatology (8–15 symptoms present), and high symptomatology (≥16 symptoms present). About half of the parents had low symptom severity. The results are represented in Table 3.
Table 3.
Distribution of symptom severity in mothers and fathers
| Mothers | Fathers | |
|---|---|---|
|
| ||
| N (%) | N (%) | |
| Low symptom severity (0–7) | 46 (61.0) | 23 (46.9) |
| Medium symptom severity (8–15) | 28 (37.7) | 23 (46.9) |
| High symptom severity (=16) | 1 (1.3) | 3 (6.2) |
| Total | 75 (100.0) | 49 (100.0) |
Abbreviation: N, total number.
Based on the diagnostic guidelines of the ADHS-SB, we identified different subtypes: ADHD mixed subtype (DSM-5), ADHD primarily hyperactive-impulsive subtype (DSM-5), ADHD primarily inattentive subtype (DSM-5), and ADHD according to ICD-10 (F90.0). For this purpose, we only examined if a symptom was present or absent, regardless of its value on ADHS-SB. Table 4 shows the various diagnoses for both parents. According to this procedure, 41.3% of the mothers and 51.0% of the fathers fulfilled criteria of an ADHD diagnosis. The difference between mothers and fathers concerning their ADHD diagnosis was not significant (χ2 (1)=2.431; P=0.092). In addition, 44.3% (N=35) of the children had at least one parent who currently met the ADHD criteria, whereas no significant relation between parental diagnosis and ADHD diagnosis of their child was observed (χ2 (4)=5.767; P=0.217 [mothers]; χ2 (4)=3.060; P=0.383 [fathers]). According to our results, the subtype distribution of child ADHD symptomatology therefore does not correspond to subtype symptomatology in affected parents.
Table 4.
Distribution of diagnoses for mothers and fathers
| Mothers | Fathers | |
|---|---|---|
|
| ||
| N (%) | N (%) | |
| Mixed subtype (DSM-5) | 11 (14.7) | 9 (18.4) |
| Hyperactive-impulsive subtype (DSM-5) | 7 (9.3) | 5 (10.2) |
| Inattentive subtype (DSM-5) | 12 (16.0) | 11 (22.4) |
| Disturbance of activity and attention (ICD-10) | 1 (1.3) | 0 (0.0) |
| No ADHD diagnosis | 44 (58.7) | 24 (49.0) |
| Total | 75 (100.0) | 49 (100.0) |
Abbreviations: ADHD, attention deficit hyperactivity disorder; DSM-5, Diagnostic and Statistical Manual of Mental Disorders, 5th edition; ICD-10, International Classification of Diseases, 10th edition; N, total number.
Discussion
Our study showed that about 44% of ADHD children in a clinical sample have at least one parent with symptoms that fulfill criteria for adult ADHD diagnosis. About half of all parents showed more than seven symptoms. Parental and child ADHD diagnosis were not related.
Regarding our first hypothesis, we found the percentage of children having at least one parent fulfilling clinical ADHD criteria to be 44%. This rate is lower than 55% found by Smalley et al,12 but corresponds to 41% by Takeda et al.38 Smalley et al12 analyzed ADHD-affected sibling pairs, which might reflect families with higher genetic load and thus higher rates of parental ADHD. In addition, they reported significantly more affected parents in families with at least one affected girl in their population of 70% boys and 30% girls with ADHD. Our sample consisted of only 20% girls who could account for the even smaller prevalence like Takeda et al38 with 24% affected girls. Another evidence for the pertinence of the ADHD child’s sex for parental ADHD prevalence could be the higher symptom number of siblings of females with ADHD than siblings of ADHD males.71 Additionally, Goos et al72 found higher ADHD severity among children with maternal ADHD history than paternal ADHD, whereas Takeda et al38 found paternal ADHD to influence severity and maternal not at all. As our major interest was the potential effect of parental ADHD symptoms on family functioning and child therapy outcome, we focused mainly on current symptomatology for identifying ADHD types and neglected childhood symptoms for frequency calculation. Following this, we cannot rule out a possible overestimation of clinical diagnoses.
The responding rate of 43.89% for the parents’ questionnaires could have induced an underestimation of parental ADHD frequency and severity in terms of parents with higher levels of ADHD might struggle with sending back the documents due to problems in organizing and sticking to a task based on their inattention problems. It is also conceivable that parents with low socioeconomic status or parents who are unsatisfied with the treatment had lower motivation for being compliant and this decreased the responding rate. We will therefore address this potential bias in another ongoing study by comparing possible influencing factors (sociodemographic factors, child therapy outcome, and parental symptom severity) of compliant and noncompliant parents.
We found no significant correlation of ADHD type for child and parents, concordant to Smalley et al.12 The vast majority of children in our sample had a mixed subtype, whereas the majority of affected parents had an inattentive or in similar quantity a mixed subtype, according to DSM-5 criteria. As the children were diagnosed according to the ICD-10 classification system, this could possibly be associated with a lower presence of subtype relation. Supplementary, criteria for mixed subtype differed between ICD-10 and DSM-5 not for the amount of required symptoms, but for the core symptoms. ADHD subtypes in the context of family structures is still a matter of debate. Results of Faraone et al10,11 and Smalley et al12 militate in favor of a shared genetic contribution to inattention and hyperactivity-impulsivity. Though Faraone et al10 showed that inattentive and combined ADHD types did not repeat in relatives, but the hyperactive-impulsive did. Yet this effect was limited by a small sample size. Furthermore, Todd et al73 also revealed that the primarily inattentive and combined subtypes coclustered within families and the hyperactive-impulsive type was specific. They suggested different subtyping not through DSM criteria but by differentiating between the severity of symptoms (“latent class”).
Furthermore, contrary to our hypothesis, we could not find a similar distribution of parental symptom severity in mothers (and fathers) like Sonuga-Barke et al49 did. Most of the ADHD mothers in our sample (61%) reported low ADHD symptoms (0–7), a considerable amount (38%) displayed medium symptoms (8–15), and only one reported high symptoms (16 and over). According to Sonuga-Barke et al,49 this would militate in favor of their accessibility for substantial parent training effects. The fathers reported a slightly different arrangement with almost half of them (47%) having each low and medium symptoms, whereas 6% of them showed high symptoms. Further investigation is needed to identify potential distributions in symptom severity that could count for missing parent training effects or child’s therapy outcome. In addition, separating into only low versus high symptom levels might be more useful, like Banks et al39 did.
To sum up, the main clinical outcome of our study is that parental ADHD is highly prevalent in families with ADHD children and adolescents even though family members do not show similar patterns of subtypes. If parents suffer from ADHD, this is not only a matter for adult psychiatrists or psychotherapists, but also for treatment of children and adolescents addressing parenting behavior. As ADHD in childhood is often associated with adverse family interactions that maintain or aggravate the syndrome,74 parent training is substantial and recommended by several guidelines.48 Yet those effects have not been documented and studies often show low methodological quality.54 Besides the problem of generalization, this might be concerned with parental ADHD: in addition to the child ADHD severity, evidence that parental ADHD is a major predictor in the outcome of ADHD interventions is given: the higher the maternal ADHD, the lower the effect of parent training on the ADHD child.49,50 Furthermore, mothers with high levels of ADHD symptoms seem to have lower parenting self-esteem, a more external locus of control and less effective disciplinary styles.39 Johnston et al43 have outlined three types of cognitive dysfunction in adult ADHD that could lead to impairments in parenting competences: cognitive processes, self-regulatory deficits, and motivational or arousal difficulties. Parental ADHD characteristics as difficulty in keeping appointments, being restless during visits, being unable to remember instructions, having difficulties in sticking to behavior modifications or monopolizing the clinician’s attention42 must also be kept in mind as they could directly affect the child’s therapy process. If necessary, the child’s therapy setting must be adjusted for these parents43 and parents with medium or severe ADHD symptoms should be motivated for separate therapy. In addition, those parents might need more structure, a higher level of instructions, more repetitions of important contents, more booster sessions, as well as more support for transfer into everyday life. Thus, screening parents of children with ADHD for adult ADHD is beneficial for the therapy outcome of their children. Screening the literature for a combined treatment of parental and child ADHD symptomatology, we could only find one randomized controlled trial reported by Jans et al.75 They found maternal ADHD treatment and parent training to reduce children’s externalizing behavior but to the same extent that a control group which received counseling did. Yet there was no placebo group, low treatment compliance, and no special treatment arrangements were made to counterbalance the maternal ADHD disadvantage as mentioned above. Altogether, it seems as if there is a lack of research focusing on the important relationship of concurrent ADHD symptomatology in children and their parents. Further studies are needed to examine the role of parental ADHD in therapeutic process.
Conclusion
Parental ADHD seems to be an important factor in the therapy process of ADHD children. About 40% of ADHD children have at least one parent with clinical ADHD symptoms. Therefore, screening for parental ADHD might be useful to increase the child’s therapy outcome.
Acknowledgments
The authors acknowledge support for the Article Processing Charge by the Deutsche Forschungsgemeinschaft and the Open Access Publication Fund of Bielefeld University.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Polanczyk G, Rohde LA. Epidemiology of attention-deficit/hyperactivity disorder across the lifespan. Curr Opin Psychiatry. 2007;20:386–392. doi: 10.1097/YCO.0b013e3281568d7a. [DOI] [PubMed] [Google Scholar]
- 2.Polanczyk G, de Lima MS, Horta BL, Biederman J, Rohde LA. The worldwide prevalence of ADHS: a systematic review and metaregression analysis. Am J Psychiatry. 2007;164:942–948. doi: 10.1176/ajp.2007.164.6.942. [DOI] [PubMed] [Google Scholar]
- 3.Biederman J, Newcorn J, Sprich S. Comorbidity of attention deficit hyperactivity disorder with conduct, depressive, anxiety, and other disorders. Am J Psychiatry. 1991;148:564–577. doi: 10.1176/ajp.148.5.564. [DOI] [PubMed] [Google Scholar]
- 4.Kessler RC, Adler L, Barkley R, et al. The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. Am J Psychiatry. 2006;163(4):716–723. doi: 10.1176/appi.ajp.163.4.716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wilens TE, Biederman J, Brown S, et al. Psychiatric comorbidity and functioning in clinically referred preschool children and school-age youths with ADHD. J Am Acad Child Adolesc Psychiatry. 2002;41(3):262–268. doi: 10.1097/00004583-200203000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Döpfner M, Breuer D, Wille N, Erhart M, Ravens-Sieberer U; for Bella Study Group How often do children meet ICD-10/DSM-IV criteria of attention deficit-/hyperactivity disorder and hyperkinetic disorder? Parent based prevalence rates in a national sample – results of the BELLA study. Eur Child Adoles Psy. 2008;17:59–70. doi: 10.1007/s00787-008-1007-y. [DOI] [PubMed] [Google Scholar]
- 7.Neuman RJ, Sitdhiraksa N, Reich W, et al. Estimation of prevalence of DSM-IV and latent class-defined ADHD subtypes in a population-based sample of child and adolescent twins. Twin Res Hum Genet. 2005;8(4):392–401. doi: 10.1375/1832427054936646. [DOI] [PubMed] [Google Scholar]
- 8.Biederman J. Attention-deficit/hyperactivity disorder: a selective overview. Biol Psychiatry. 2005;57:1215–1220. doi: 10.1016/j.biopsych.2004.10.020. [DOI] [PubMed] [Google Scholar]
- 9.Faraone SV, Doyle AE. The nature and heritability of attention-deficit/hyperactivity disorder. Child Adolesc Psychiatr Clin N Am. 2001;10(2):299–316. [PubMed] [Google Scholar]
- 10.Faraone SV, Biederman J, Friedman D. Validity of DSM-IV subtypes of attention deficit/hyperactivity disorder: a family perspective. J Am Acad Child Adolesc Psychiatry. 2000a;39:300–307. doi: 10.1097/00004583-200003000-00011. [DOI] [PubMed] [Google Scholar]
- 11.Faraone SV, Biederman J, Mick E, et al. Family study of girls with attention deficit hyperactivity disorder. Am J Psychiatry. 2000b;157:1077–1083. doi: 10.1176/appi.ajp.157.7.1077. [DOI] [PubMed] [Google Scholar]
- 12.Smalley SL, McGough JJ, Del’Homme M, et al. Familial clustering of symptoms and disruptive behaviors in multiplex families with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2000;39(9):1135–1143. doi: 10.1097/00004583-200009000-00013. [DOI] [PubMed] [Google Scholar]
- 13.Barkley RA, Fischer M, Edelbrock C, Smallish L. The adolescent outcome of hyperactive children diagnosed by research criteria – III. Mother-child interactions, family conflicts and maternal psychopathology. J Child Psychol Psychiatry. 1991;32(2):233–255. doi: 10.1111/j.1469-7610.1991.tb00304.x. [DOI] [PubMed] [Google Scholar]
- 14.Biederman J, Milberger S, Faraone SV, et al. Family-environment risk factors for attention deficit hyperactivity disorder: a test of Rutter’s indicators of adversity. Arch Gen Psychiatry. 1995;52:464–470. doi: 10.1001/archpsyc.1995.03950180050007. [DOI] [PubMed] [Google Scholar]
- 15.Biederman J, Faraone SV, Monuteaux MC. Differential effect of environmental adversity by gender: Rutter’s index of adversity in a group of boys and girls with and without ADHD. Am J Psychiatry. 2002;159:1556–1562. doi: 10.1176/appi.ajp.159.9.1556. [DOI] [PubMed] [Google Scholar]
- 16.Scahill L, Schwab-Stone M, Merikangas KR, Leckman JF, Zhang H, Kasl S. Psychosocial and clinical correlates of ADHD in a community sample of school-age children. J Am Acad Child Adolesc Psychiatry. 1999;38(8):976–984. doi: 10.1097/00004583-199908000-00013. [DOI] [PubMed] [Google Scholar]
- 17.Humphreys KL, Mehta N, Lee SS. Association of parental ADHD and depression with externalizing and internalizing dimensions of child psychopathology. J Atten Disord. 2012;16(4):267–275. doi: 10.1177/1087054710387264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Modesto-Lowe V, Danforth JS, Brooks D. ADHD: Does parenting style matter? Clin Pediatrics. 2008;47(9):865–872. doi: 10.1177/0009922808319963. [DOI] [PubMed] [Google Scholar]
- 19.Danforth JS, Barkley RA, Stokes TF. Observations of parent-child interactions with hyperactive children. Research and clinical implications. Clin Psychol Rev. 1991;11:703–727. [Google Scholar]
- 20.DuPaul GJ, McGoey KE, Eckert TL, Vanbrakle J. Preschool children with attention-deficit/hyperactivity disorder: impairments in behavioral, social, and school functioning. J Am Acad Child Adolesc Psychiatry. 2001;40(5):508–515. doi: 10.1097/00004583-200105000-00009. [DOI] [PubMed] [Google Scholar]
- 21.Johnston C. Parent characteristics and parent-child interactions in families of nonproblem children and ADHD children with higher and lower levels of oppositional-defiant behavior. J Abnorm Child Psychol. 1996;24(1):85–104. doi: 10.1007/BF01448375. [DOI] [PubMed] [Google Scholar]
- 22.Keown LK, Woodward LJ. Early parent–child relations and family functioning of preschool boys with pervasive hyperactivity. J Abnorm Child Psychol. 2002;30(6):541–553. doi: 10.1023/a:1020803412247. [DOI] [PubMed] [Google Scholar]
- 23.Mick E, Biederman J, Prince J, Fischer MJ, Faraone SV. Impact of low birth weight on attention-deficit/hyperactivity disorder. J Dev Behav Pediatr. 2002;23:16–22. doi: 10.1097/00004703-200202000-00004. [DOI] [PubMed] [Google Scholar]
- 24.Mick E, Biederman J, Faraone SV, Sayer J, Kleinman S. Case-control study of attention-deficit hyperactivity disorder and maternal smoking, alcohol use, and drug use during pregnancy. J Am Acad Child Adolesc Psychiatry. 2002;41(4):378–385. doi: 10.1097/00004583-200204000-00009. [DOI] [PubMed] [Google Scholar]
- 25.Milberger S, Biederman J, Faraone SV, Chen L, Jones J. Is maternal smoking during pregnancy a risk factor for attention deficit hyperactivity disorder in children? Am J Psychiatry. 1996;153(9):1138–1142. doi: 10.1176/ajp.153.9.1138. [DOI] [PubMed] [Google Scholar]
- 26.Thapar A, Fowler T, Rice F, et al. Maternal smoking during pregnancy and attention deficit hyperactivity disorder symptoms in offspring. Am J Psychiatry. 2003;160(11):1985–1989. doi: 10.1176/appi.ajp.160.11.1985. [DOI] [PubMed] [Google Scholar]
- 27.Biederman J, Mick E, Faraone SV. Age-dependent decline of symptoms of attention deficit hyperactivity disorder: impact of remission definition and symptom type. Am J Psychiatry. 2000;157:816–818. doi: 10.1176/appi.ajp.157.5.816. [DOI] [PubMed] [Google Scholar]
- 28.Alessandri SM. Attention, play, and social behavior in ADHD preschoolers. J Abnorm Child Psychol. 1992;20:289–302. doi: 10.1007/BF00916693. [DOI] [PubMed] [Google Scholar]
- 29.Greenhill LL, Posner K, Vaughan BS, Kratochvil CJ. Attention deficit hyperactivity disorder in preschool children. Child Adolesc Psychiatr Clin N Am. 2008;17(2):347–366. doi: 10.1016/j.chc.2007.11.004. [DOI] [PubMed] [Google Scholar]
- 30.Kadesjö C, Kadesjö B, Hägglöff B, Gillberg C. ADHD in Swedish 3- to 7-year-old children. J Am Acad Child Adolesc Psychiatry. 2001;40:1021–1028. doi: 10.1097/00004583-200109000-00010. [DOI] [PubMed] [Google Scholar]
- 31.Harpin VA. The effect of ADHD on the life of an individual, their family, and community from preschool to adult life. Arch Dis Child. 2005;90(Suppl 1):i2–i7. doi: 10.1136/adc.2004.059006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hoza B. Peer functioning in children with ADHD. Ambul Pediatr. 2007;7(1 Suppl):101–106. doi: 10.1016/j.ambp.2006.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Loe IM, Feldman HM. Academic and educational outcomes of children with ADHD. Ambul Pediatr. 2007;7:82–90. doi: 10.1016/j.ambp.2006.05.005. [DOI] [PubMed] [Google Scholar]
- 34.Barkley RA, Anastopoulos AD, Guevremont DC, Fletcher KE. Adolescents with ADHD: patterns of behavioral adjustment, academic functioning and treatment utilization. J Am Acad Child Adolesc Psychiatry. 1991;30:752–761. doi: 10.1016/s0890-8567(10)80010-3. [DOI] [PubMed] [Google Scholar]
- 35.Barkley RA, Fischer M, Smallish L, Fletcher K. Young adult outcome of hyperactive children: adaptive functioning in major life activities. J Am Acad Child Adolesc Psychiatry. 2006;45:192–202. doi: 10.1097/01.chi.0000189134.97436.e2. [DOI] [PubMed] [Google Scholar]
- 36.Davidson MA. ADHD in adults: a review of the literature. J Atten Disord. 2008;11(6):628–641. doi: 10.1177/1087054707310878. [DOI] [PubMed] [Google Scholar]
- 37.Fischer M, Barkley RA, Smallish L, Fletcher K. Hyperactive children as young adults: driving abilities, safe driving behavior, and adverse driving outcomes. Accid Anal Prev. 2007;39:94–105. doi: 10.1016/j.aap.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 38.Takeda T, Stotesbery K, Power T, et al. Parental ADHD status and its association with proband ADHD subtype and severity. J Pediatr. 2010;157:995–1000. doi: 10.1016/j.jpeds.2010.05.053. [DOI] [PubMed] [Google Scholar]
- 39.Banks T, Ninowski JE, Mash EJ, Semple DL. Parenting behavior and cognitions in a community sample of mothers with and without symptoms of attention-deficit/hyperactivity disorder. J Child Fam Stud. 2008;17(1):28–43. [Google Scholar]
- 40.Harvey E, Danforth JS, McKee TE, Ulaszek WR, Friedman JL. Parenting of children with attention-deficit/hyperactivity disorder (ADHD): the role of parental ADHD symptomatology. J Atten Disord. 2003;7(1):31–42. doi: 10.1177/108705470300700104. [DOI] [PubMed] [Google Scholar]
- 41.Murray C, Johnston CJ. Parenting in mothers with and without attention-deficit/hyperactivity disorder. J Abnorm Psychol. 2006;115(1):52–61. doi: 10.1037/0021-843X.115.1.52. [DOI] [PubMed] [Google Scholar]
- 42.Weiss M, Hechtman L, Weiss G. ADHD in parents. J Am Acad Child Adolesc Psychiatry. 2000;39(8):1059–1061. doi: 10.1097/00004583-200008000-00023. [DOI] [PubMed] [Google Scholar]
- 43.Johnston C, Mash EJ, Miller N, Ninowski JE. Parenting in adults with attention-deficit/hyperactivity disorder (ADHD) Clin Psychol Rev. 2012;32(4):215–228. doi: 10.1016/j.cpr.2012.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kendziora KT, O’Leary SG. Dysfunctional parenting as a focus for prevention and treatment of child behavior problems. Adv Clin Child Psych. 1993;15:175–206. [Google Scholar]
- 45.Mokrova I, O’Brien M, Calkins S, Keane S. Parental ADHD symptomatology and ineffective parenting: the connecting link of home chaos. Parent Sci Pract. 2010;10:119–135. doi: 10.1080/15295190903212844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pliszka S, AACAP Work Group on Quality Issues Practice parameter for the assessment and treatment of children and adolescents with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2007;46:894–921. doi: 10.1097/chi.0b013e318054e724. [DOI] [PubMed] [Google Scholar]
- 47.Deutsche Gesellschaft für Kinder- und Jugendpsychiatrie und Psychotherapie [German Foundation for Children and Adolescent Psychiatry and Psychotherapy] Köln: Deutscher Ärzte-Verlag. 2007:239–254. German. [Google Scholar]
- 48.National Collaborating Centre for Mental Health . Clinical Guideline 27. London: National Institute for Health and Clinical Excellence; 2008. Attention deficit hyperactivity disorder: diagnosis and management of ADHD in children, young people and adults. [Google Scholar]
- 49.Sonuga-Barke EJS, Daley D, Thompson M. Does maternal ADHD reduce the effectiveness of parent training for preschool children’s ADHD? J Am Acad Child Adolesc Psychiatry. 2002;41(6):696–702. doi: 10.1097/00004583-200206000-00009. [DOI] [PubMed] [Google Scholar]
- 50.Chronis-Tuscano A, O’Brien KA, Johnston C, et al. The relation between maternal ADHD symptoms and improvement in child behavior following brief behavioral parent training is mediated by change in negative parenting. J Abnorm Child Psychol. 2011;39:1047–1057. doi: 10.1007/s10802-011-9518-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Danforth JS, Harvey E, Ulaszek WR, McKee TE. The outcome of group parent training for families of children with attention-deficit hyperactivity disorder and defiant/aggressive behavior. J Behav Ther Exp Psychiatry. 2006;37(3):188–205. doi: 10.1016/j.jbtep.2005.05.009. [DOI] [PubMed] [Google Scholar]
- 52.Kohut CS, Andrews J. The efficacy of parent training programs for ADHD children: a fifteen-year review. Dev Disabil Bull. 2004;32(2):155–172. [Google Scholar]
- 53.Loren RA, Vaughn AJ, Langberg JM, et al. Effects of an 8-session behavioral parent training group for parents of children with ADHD on child impairment and parenting confidence. J Atten Disord. 2015;19(2):158–166. doi: 10.1177/1087054713484175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zwi M, Jones H, Thorgaard C, York A, Dennis JA. Parent training interventions for attention deficit hyperactivity disorder (ADHD) in children aged 5 to 18 years. Cochrane Database Syst Rev. 2011:12. doi: 10.1002/14651858.CD003018.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Chandler ML. Psychotherapy for adult attention deficit/hyperactivity disorder: a comparison with cognitive behaviour therapy. J Psychiatr Ment Health Nurs. 2013;20(9):814–820. doi: 10.1111/jpm.12023. [DOI] [PubMed] [Google Scholar]
- 56.Pallanti S, Salerno L. Pharmacological treatment and management of attention deficit hyperactivity disorder (ADHD) in adults. Minerva Psichiatr. 2013;54(4):297–315. [Google Scholar]
- 57.Retz W, Retz-Junginger P. Prediction of methylphenidate treatment outcome in adults with attention-deficit/hyperactivity disorder (ADHD) Eur Arch Psychiatry Clin Neurosci. 2014;264(Suppl 1):35–43. doi: 10.1007/s00406-014-0542-4. [DOI] [PubMed] [Google Scholar]
- 58.Babinski DE, Waxmonsky JG, Pelham WE. Treating parents with attention-deficit/hyperactivity disorder: the effects of behavioral parent training and acute stimulant medication treatment on parent–child interactions. J Abnorm Child Psychol. 2014;42:1129–1140. doi: 10.1007/s10802-014-9864-y. [DOI] [PubMed] [Google Scholar]
- 59.Chronis-Tuscano A, Seymour KE, Stein MA, et al. Efficacy of osmotic-release oral system (OROS) methylphenidate for mothers with attention-deficit/hyperactivity disorder (ADHD) J Clin Psychiatry. 2008;69:1938–1947. doi: 10.4088/jcp.v69n1213. [DOI] [PubMed] [Google Scholar]
- 60.Chronis-Tuscano A, Rooney M, Seymour K, et al. Effects of maternal stimulant medication on observed parenting in mother-child dyads with attention-deficit/hyperactivity disorder. J Clin Child Adolesc Psychol. 2010;39:581–587. doi: 10.1080/15374416.2010.486326. [DOI] [PubMed] [Google Scholar]
- 61.Evans SW, Vallano G, Pelham W. Treatment of parenting behavior with a psychostimulant: a case study of an adult with attention-deficit hyperactivity disorder. J Child Adolesc Psychopharmacol. 1994;4:63–69. [Google Scholar]
- 62.Waxmonsky JG, Waschbusch DA, Babinski DE, et al. Does pharmacological treatment of ADHD in adults enhance parenting performance? Results of a double-blind randomized trial. CNS Drugs. 2014;28:665–677. doi: 10.1007/s40263-014-0165-3. [DOI] [PubMed] [Google Scholar]
- 63.Wietecha L, Young J, Ruff D, Dunn D, Findling RL, Saylor K. Atomoxetine once daily for 24 weeks in adults with attention-deficit/hyperactivity disorder (ADHD): impact of treatment on family functioning. Clin Neuropharmacol. 2012;35:125–133. doi: 10.1097/WNF.0b013e3182560315. [DOI] [PubMed] [Google Scholar]
- 64.Dilling H, Mombour W, Schmidt MH. Internationale Klassifikation psychischer Störungen: ICD-10 Kapitel V (F) [International classification of mental disorders: ICD-10 Chapter V (F)] 6th ed. Bern: Huber; 2008. German. [Google Scholar]
- 65.Retz-Junginger P, Retz W, Blocher D, et al. Wender Utah Rating Scale (WURS-K): Die deutsche Kurzform zur retrospektiven Erfassung des hyperkinetischen Syndroms bei Erwachsenen [German short-version of the Wender Utah Rating Scale] Nervenarzt. 2002;74(11):987–993. doi: 10.1007/s00115-001-1215-x. [DOI] [PubMed] [Google Scholar]
- 66.Ward MF, Wender PH, Reimherr FH. The Wender Utah Rating Scale: an aid in the retrospective diagnosis of childhood attention deficit hyperactivity disorder. Am J Psychiatry. 1993;150:885–890. doi: 10.1176/ajp.150.6.885. [DOI] [PubMed] [Google Scholar]
- 67.Retz-Junginger P, Retz W, Blocher D, et al. Reliabilität und Validität der Wender-Utah-Rating-Scale-Kurzform. Retrospektive Erfassung von Symptomen aus dem Spektrum der Aufmerksamkeitsdefizit/Hyperaktivitätsstörung. [Reliability and validity of the Wender-Utha-Rating-Scale short version] Nervenarzt. 2003;73(9):830–838. doi: 10.1007/s00115-002-1447-4. German. [DOI] [PubMed] [Google Scholar]
- 68.Rösler M, Retz W, Retz-Junginger P, et al. Instrumente zur Diagnostik der Aufmerksamkeitsdefizit-/Hyperaktivitätsstörung (AHDS) im Erwachsenenalter. [Instruments to diagnose ADHD in adulthood] Nervenarzt. 2004;75(9):888–895. doi: 10.1007/s00115-003-1622-2. German. [DOI] [PubMed] [Google Scholar]
- 69.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders, DSM-IV. Washington DC: American Psychiatric Association; 1994. [Google Scholar]
- 70.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders, DSM-V. Washington DC: American Psychiatric Association; 2013. [Google Scholar]
- 71.Rhee SH, Waldman ID. Etiology of sex differences in the prevalence of ADHD: an examination of inattention and hyperactivity-impulsivity. Am J Med Genet B Neuropsychiatr Genet. 2004;127B:60–64. doi: 10.1002/ajmg.b.20131. [DOI] [PubMed] [Google Scholar]
- 72.Goos LM, Ezzatian P, Schachar R. Parent-of-origin effects in attention-deficit hyperactivity disorder. Psychiatry Res. 2007;149:1–9. doi: 10.1016/j.psychres.2006.08.006. [DOI] [PubMed] [Google Scholar]
- 73.Todd RD, Rasmussen ER, Neuman RJ, et al. Familiarity and heritability of subtypes of attention deficit hyperactivity disorder in a population sample of adolescent female twins. Am J Psychiatry. 2001;158:1891–1898. doi: 10.1176/appi.ajp.158.11.1891. [DOI] [PubMed] [Google Scholar]
- 74.Daley D, Sonuga-Barke EJS, Thompson M. Assessing expressed emotion in mothers of preschool ADHD children: psychometric properties of a modified speech sample. Br J Clin Psychol. 2003;42:53–67. doi: 10.1348/014466503762842011. [DOI] [PubMed] [Google Scholar]
- 75.Jans T, Jacob C, Warnke A, et al. Does intensive multimodal treatment for maternal ADHD improve the efficacy of parent training for children with ADHD? A randomized controlled multicenter trial. J Child Psychol Psychiatry. doi: 10.1111/jcpp.12443. Epub 2015 Jun 30. [DOI] [PubMed] [Google Scholar]


