To the Editor,
Pre-exposure prophylaxis—commonly referred to as PrEP—is a new HIV prevention method that significantly reduces an individual's risk of acquiring HIV if taken regularly.1–3 With the introduction of a new HIV prevention method—especially a highly effective one—counseling guidance is needed to help potential users determine if the new method is the right approach for them. Guidance is also necessary for helping individuals consider how the new method fits, or does not fit, with their current risk-reduction behaviors, if any.
For the best protection against HIV, individuals would use PrEP together with other prevention measures, such as using condoms consistently and correctly, to reduce their risk of HIV. However, some individuals may have limited or no control over condom use with some or all of their partners, or may wish not to use condoms. HIV prevention counseling must therefore address the possibility that some individuals who use PrEP may choose to discontinue condom use or to use condoms less consistently, even if they are encouraged to continue condom use while using PrEP.
We have developed counseling guidance that promotes informed decision making on sexual health for women in Kenya and South Africa who have expressed interest in using PrEP as part of their HIV risk-reduction strategy, particularly with respect to (1) decisions concerning PrEP and condom use, and (2) the prevention of pregnancy and other sexually transmitted infections when PrEP is used alone. Findings from our research on PrEP suggested such guidance would be needed.
We conducted a survey among 799 women in Bondo, Kenya, and Pretoria, South Africa, to find out if and how their sexual behaviors (e.g., condom use, having sex with a new partner) might change or stay the same if they were to start taking PrEP. Among these women, 27–40% indicated that they would be inclined to reduce their use of other HIV-risk reduction measures, depending on the context of the risk situation, if they took PrEP.4
Follow-up qualitative interviews were then conducted with 60 purposively-selected participants (30 in Bondo and 30 in Pretoria) whose survey responses suggested that they would be more likely to reduce condom use or have sex with a new partner if they took PrEP. Three interrelated themes were identified from these interviews that described women's motivations for reducing use of other HIV risk-reduction measures if using PrEP: (1) “PrEP protects”—PrEP was perceived as an effective HIV prevention method that replaced the need for condoms, (2) condoms were a source of conflict in relationships and PrEP would provide an opportunity to resolve or avoid this conflict, and (3) having sex without a condom or having sex with a new partner was necessary for receiving material goods and financial assistance—PrEP would provide reassurance in these situations. Many also believed that PrEP alone would be a sufficient HIV risk-reduction strategy.5
These results highlighted the necessity of having guidance that encourages informed decision-making by providing essential HIV prevention information within the context of PrEP while helping women to reflect upon the information within their own values and risk situations and apply the information to their individual needs and circumstances.
“Guidance for Providing Informed-Choice Counseling on Sexual Health for Women Interested in Pre-Exposure Prophylaxis (PrEP)” is based on the informed-choice counseling approach traditionally used in family planning and supported by research on informed decision making.6–9 To develop the guidance, we explored women's and counselors' perceptions of the concept of an informed-choice approach for PrEP-specific risk-reduction counseling.
We conducted eight focus group discussions (four in Bondo and four in Pretoria) with women at higher risk of HIV to gauge the acceptability of the informed-choice approach. Women in the discussions spoke about supporting an informed-choice framework for PrEP-specific counseling, liking that a client could choose the risk-reduction strategy best suited for her, and believing that counselors would be able to provide clients with sufficient information, allowing a woman to make a good decision about her own health.10
We also conducted in-depth interviews with six risk-reduction counselors (three in Bondo and three in Pretoria) to gather information, such as what the counselors thought women would want to know about PrEP in order to make informed decisions about its use, to help shape the guidance. Lastly, we incorporated aspects of the counseling materials and messages that were developed for a PrEP demonstration project for women called Strategies to Combine PrEP with Prevention Efforts (SCOPE); development of the SCOPE protocol and materials was sponsored by FHI 360 with funding from the US Agency for International Development (USAID).11
In March 2015, we facilitated six workshops in Bondo and Kisumu, Kenya, and in Pretoria, South Africa, to review and discuss the proposed guidance. Workshop participants included key stakeholders such as officials from the Ministry of Health, members of community advisory boards, and HIV risk-reduction counselors. The guidance was finalized after comments from the workshops were incorporated, and workshop participants were provided an opportunity to give feedback on the final draft of the guidance.
The guidance has two guiding principles:
Principle 1: Enabling women to make an informed and voluntary choice of HIV prevention options is the foundation of effective counseling. An informed and voluntary choice means individuals are entitled to attain high standards of sexual and reproductive health, receive relevant information and means to act on this information, and make their own decisions without discrimination, coercion, or violence.
Principle 2: Women are capable of making informed decisions about their overall sexual health. When provided with relevant information and guidance, women can make the decisions that are best for them—including decisions on the use of other risk-reduction measures, particularly condoms, when they are using PrEP. Telling women to “always use condoms” in addition to PrEP disregards the fact that consistent condom use may not be realistic for many women. It may also lead to the perception that PrEP is not effective on its own, which can discourage some women from using PrEP at all, leaving them without protection in situations in which consistent condom use is not achievable.
Instead, women who are unable to use condoms consistently or who do not want to use condoms when taking PrEP need guidance to (1) make informed decisions about contraception and about regular screening and treatment for sexually transmitted infections, and (2) understand the importance of PrEP adherence, especially if PrEP will be used as the primary HIV prevention strategy.
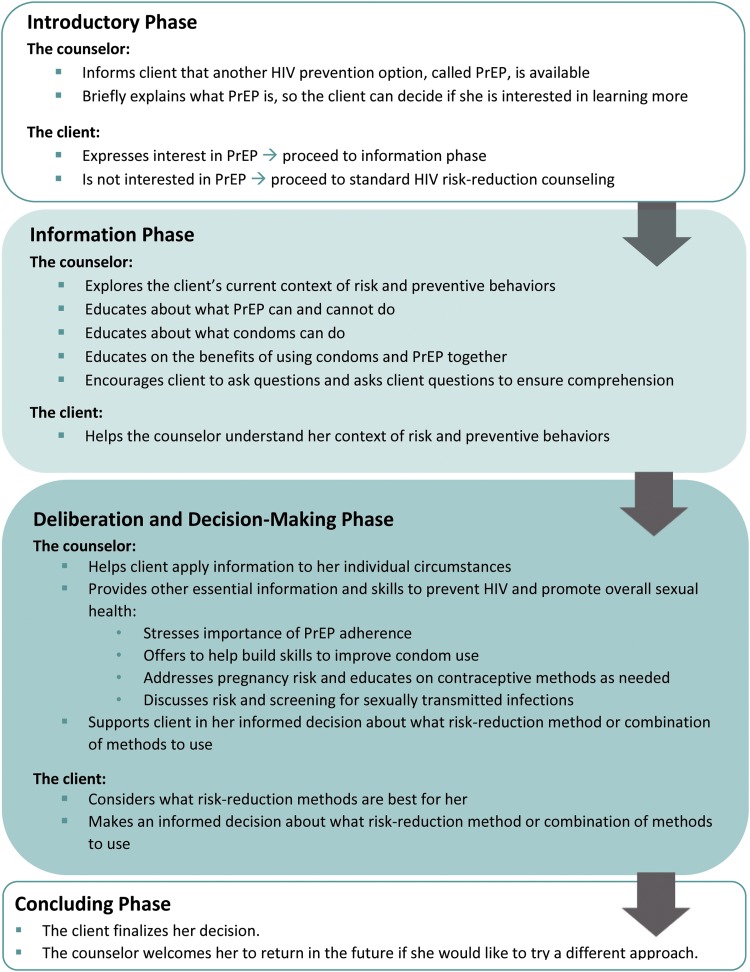
“Guidance for Providing Informed-Choice Counseling on Sexual Health for Women Interested in Pre-Exposure Prophylaxis (PrEP)” is written for counselors who provide HIV risk-reduction counseling at facilities that offer PrEP to clients. It is intended to be incorporated into and delivered as part of standard risk-reduction counseling and evidence-based PrEP adherence counseling. The guidance is divided into four sequential phases (Fig. 1):
1. The Introductory Phase: a client expresses interest in learning more about PrEP.
2. The Information Phase: the counselor provides accurate information about PrEP and condoms.
3. The Deliberation and Decision-Making Phase: the counselor helps the client apply this information to her individual circumstances and to consider what the best option is for her overall sexual health.
4. The Concluding Phase: the client finalizes her plan to reduce her risk of HIV and to maintain her overall sexual health. The counselor summarizes the client's plan and welcomes her to return if she would like to try another approach in the future.
FIG. 1.
Phases of informed-choice pre-exposure prophylaxis (PrEP) counseling.
The guidance document outlines the steps for all four phases and describes how to carry out each step. Comprehensive information and essential questions are included to help guide a woman through a decision-making process and choose the HIV risk-reduction strategy that is best for her. To explain in brief, the introductory phase is likely the first time a counselor and a client have talked about PrEP, and it can be initiated either by the client or by a provider. We recommend three steps during this phase:
Step 1. Set the agenda for the counseling session
Step 2. Inform the client that PrEP is available
Step 3. Briefly explain what PrEP is
If the client is interested in learning more about PrEP, the counselor proceeds to the next phase.
During the information phase, the counselor learns about the client's current context of risk and preventive behaviors and provides essential information on PrEP and other preventive options, encouraging the client to ask questions throughout. We recommend four steps in this phase:
Step 1. Explore the client's current context of risk and preventive behaviors
Step 2. Educate about what PrEP can and cannot do
Step 3. Educate about what condoms can do
Step 4. Educate on the benefits of using PrEP and condoms together
During the deliberation and decision-making phase, the counselor helps the client to think about her overall sexual health while applying what she has learned about HIV prevention during the information phase to her individual circumstances. The counselor and client will also discuss, and the client will likely choose among, multiple HIV risk-reduction approaches in which she may rely on PrEP alone or PrEP in combination with other HIV prevention approaches. Special emphasis is given for clients who are unable to use condoms consistently or are planning to use PrEP without condoms or other HIV risk-reduction methods. To be effective, counselors should be prepared to consider and accommodate all women's individual situations and preferences. We recommend two steps in this phase:
Step 1. Help the client apply the information to her individual circumstances
Step 2. Provide other essential information and skills to prevent HIV and promote overall sexual health
During the concluding phase, the counselor provides a brief summary of the client's plan for HIV risk reduction, PrEP adherence, and overall sexual health and ensures that the client is comfortable with this plan. The counselor also acknowledges to the client that her HIV risk-reduction needs will likely change over time and reminds the client that counselors are available to discuss different HIV risk-reduction options if her current situation changes or if she would like to try a different approach.
To conclude, emtricitabine/tenofovir disoproxil fumarate has recently been approved for use as PrEP in both South Africa and Kenya.12,13 The scale-up of PrEP will now be possible in these countries, and planners must consider numerous pragmatic factors to ensure access to those who want and need PrEP.14 Informed-choice counseling is one of those factors. Women need accurate information and supportive guidance so they can make informed and voluntary decisions on the HIV prevention methods that best fit their needs. “Guidance for Providing Informed-Choice Counseling on Sexual Health for Women Interested in Pre-Exposure Prophylaxis (PrEP)” can contribute to filling this need.
To download the guidance document, go to http://www.fhi360.org/projects/prep-and-risk-compensation-assessing-effect-and-preparing-rollout.
Acknowledgments
We are appreciative of the individuals who provided valuable comments on the guidance during workshops held in Kenya and South Africa. We are also grateful to the individuals who participated in the research that served as the foundation for these guidelines and to the larger research team at IRDO, SRC, and FHI 360 who contributed to the implementation of the research.
The development of this guidance and the research that informed it were funded by the National Institute of Mental Health, National Institutes of Health, under award number R01MH095531. The contents of the guidance are solely the responsibility of the writers and do not necessarily represent the official views of the National Institutes of Health.
Author Disclosure Statement
No conflicting financial interests exist.
References
- 1.Grant RM, Lama JR, Anderson PL, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. New Engl J Med 2010;363:2587–2599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baeten JM, Donnell D, Ndase P, et al. Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. New Engl J Med 2012;367:399–410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thigpen MC, Kebaabetswe PM, Paxton LA, et al. Antiretroviral preexposure prophylaxis for heterosexual HIV transmission in Botswana. New Engl J Med 2012;367:423–434 [DOI] [PubMed] [Google Scholar]
- 4.Corneli A, Field S, Namey E, Agot K, et al. Preparing for the rollout of pre-exposure prophylaxis (PrEP): A vignette survey to identify intended sexual behaviors among women in Kenya and South Africa if using PrEP. PLoS One 2015;10:e0129177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Corneli A,14Namey E, Ahmed K, et al. Motivations for reducing other risk-reduction practices if taking pre-exposure prophylaxis: Findings from a qualitative study among women in Kenya and South Africa. AIDS Patient Care STDS 2015;29:503–509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Upadhyay U. Informed choice in family planning: Helping people decide. Population Rep 2001; Series J, No. 50 [PubMed]
- 7.Bruce J. Fundamental elements of the quality of care: A simple framework. Stud Fam Plan 1990;21:61–91 [PubMed] [Google Scholar]
- 8.Vanstone M, Kinsella EA, Nisker J. Information-sharing to promote informed choice in prenatal screening in the spirit of the SOGC clinical practice guideline: A proposal for an alternative model. J Obstet Gynaecol Can 2012;34:269–275 [DOI] [PubMed] [Google Scholar]
- 9.Kim YM, Kols A, Mucheke S. Informed choice and decision-making in family planning counseling in Kenya. Int Fam Plann Persp 1998;24:4–11 [PubMed] [Google Scholar]
- 10.Corneli A, Namey E, Ahmed K, et al. Preparing for risk-reduction counseling on pre-exposure prophylaxis for women in Kenya and South Africa. The HIV Research for Prevention Conference, Cape Town, South Africa, October28–31, 2014 [P46.01] [Google Scholar]
- 11.Deese J, Corneli A. SCOPE Protocol: Strategies to Combine PrEP with Prevention Efforts. Version 2.0. April 2013
- 12.Medicines Control Council. Press release Medicines Control Council approves fixed-dose combination of tenofovir disoproxyl fumarate and emtricitabine for pre-exposure prophylaxis of HIV. Available from: http://www.mccza.com/documents/2e4b3a5310.11_Media_release_ARV_FDC_PrEP_Nov15_v1.pd (Last accessed January2, 2016)
- 13.AVAC. South Africa and Kenya Approval of Oral PrEP Should Spur Rollout. December 17, 2015. Available from: http://www.avac.org/blog/south-africa-and-kenya-approval-oral-prep (Last accessed January2, 2016)
- 14.Mugo NR, Ngure K, Kiragu M, Irungu E, Kilonzo N. The preexposure prophylaxis revolution: From clinical trials to programmatic implementation. Curr Opin HIV AIDS 2016;11:80–86 [DOI] [PMC free article] [PubMed] [Google Scholar]