The properties of a diagnostic or screening test are often described using sensitivity and specificity or predictive values, as described in previous Notes.1,2 Likelihood ratios are alternative statistics for summarising diagnostic accuracy, which have several particularly powerful properties that make them more useful clinically than other statistics.3
Each test result has its own likelihood ratio, which summarises how many times more (or less) likely patients with the disease are to have that particular result than patients without the disease. More formally, it is the ratio of the probability of the specific test result in people who do have the disease to the probability in people who do not.
A likelihood ratio greater than 1 indicates that the test result is associated with the presence of the disease, whereas a likelihood ratio less than 1 indicates that the test result is associated with the absence of disease. The further likelihood ratios are from 1 the stronger the evidence for the presence or absence of disease. Likelihood ratios above 10 and below 0.1 are considered to provide strong evidence to rule in or rule out diagnoses respectively in most circumstances.4 When tests report results as being either positive or negative the two likelihood ratios are called the positive likelihood ratio and the negative likelihood ratio.
The table shows the results of a study of the value of a history of smoking in diagnosing obstructive airway disease.5 Smoking history was categorised into four groups according to pack years smoked (packs per day × years smoked). The likelihood ratio for each category is calculated by dividing the percentage of patients with obstructive airway disease in that category by the percentage without the disease in that category. For example, among patients with the disease 28% had 40+ smoking pack years compared with just 1.4% of patients without the disease. The likelihood ratio is thus 28.4/1.4 = 20.3. A smoking history of more than 40 pack years is strongly predictive of a diagnosis of obstructive airway disease as the likelihood ratio is substantially higher than 10. Although never smoking or smoking less than 20 pack years both point to not having obstructive airway disease, their likelihood ratios are not small enough to rule out the disease with confidence.
Table 1.
Likelihood ratios are ratios of probabilities, and can be treated in the same way as risk ratios for the purposes of calculating confidence intervals6
|
Smoking habit (pack years)
|
Obstructive airway disease
|
|||
|---|---|---|---|---|
| Yes (n (%)) | No (n (%)) | Likelihood ratio | 95% CI | |
| ≥40 | 42 (28.4) | 2 (1.4) | (42/148)/(2/144)=20.4 | 5.04 to 82.8 |
| 20-40 | 25 (16.9) | 24 (16.7) | (25/148)/(24/144)=1.01 | 0.61 to 1.69 |
| 0-20 | 29 (19.6) | 51 (35.4) | (29/148)/51/144)=0.55 | 0.37 to 0.82 |
| Never smoked or smoked for <1 yr | 52 (35.1) | 67 (46.5) | (52/148)/67/144)=0.76 | 0.57 to 1.00 |
| Total | 148 (100) | 144 (100) | ||
Calculation of post-test probabilities using likelihood ratios
Pretest probability = p1 =0.1
pretest odds = p1/(1-p1) = 0.1/0.9 = 0.11
post-test odds = pretest odds×likelihood ratio
post-test odds = o2 = 0.11×20.43 = 2.27
Post-test probability = o2/(1+ o2) = 2.27/3.37 = 0.69
Likelihood ratios are ratios of probabilities, and can be treated in the same way as risk ratios for the purposes of calculating confidence intervals.6
For a test with only two outcomes, likelihood ratios can be calculated directly from sensitivities and specificities.1 For example, if smoking habit is dichotomised as above or below 40 pack years, the sensitivity is 28.4% (42/148) and specificity 98.6% (142/144). The positive likelihood ratio is the proportion with obstructive airway disease who smoked more than 40 pack years (sensitivity) divided by the proportion without disease who smoked more than 40 pack years (1-specificity), 28.4/1.4 = 20.3, as before. The negative likelihood ratio is the proportion with disease who smoked less than 40 pack years (1-sensitivity) divided by the proportion without disease who smoked less than 40 pack years (specificity), 71.6/98.6 = 0.73. However, unlike sensitivity and specificity, computation of likelihood ratios does not require dichotomisation of test results. Forcing dichotomisation on multicategory test results may discard useful diagnostic information.
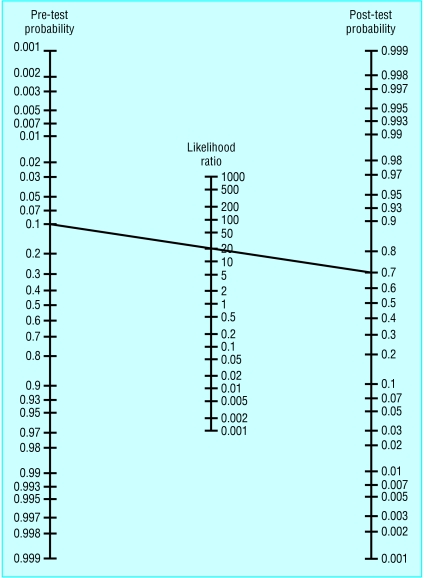
Likelihood ratios can be used to help adapt the results of a study to your patients. To do this they make use of a mathematical relationship known as Bayes theorem that describes how a diagnostic finding changes our knowledge of the probability of abnormality.3 The post-test odds that the patient has the disease are estimated by multiplying the pretest odds by the likelihood ratio. The use of odds rather than risks makes the calculation slightly complex (box) but a nomogram can be used to avoid having to make conversions between odds and probabilities (figure).7 Both the figure and the box illustrate how a prior probability of obstructive airway disease of 0.1 (based, say, on presenting features) is updated to a probability of 0.7 with the knowledge that the patient had smoked for more than 40 pack years.
Figure 1.
Use of Fagan's nomogram for calculating post-test probabilities7
In clinical practice it is essential to know how a particular test result predicts the risk of abnormality. Sensitivities and specificities1 do not do this: they describe how abnormality (or normality) predicts particular test results. Predictive values2 do give probabilities of abnormality for particular test results, but depend on the prevalence of abnormality in the study sample and can rarely be generalised beyond the study (except when the study is based on a suitable random sample, as is sometimes the case for population screening studies). Likelihood ratios provide a solution as they can be used to calculate the probability of abnormality, while adapting for varying prior probabilities of the chance of abnormality from different contexts.
References
- 1.Altman DG, Bland JM. Diagnostic tests 1: sensitivity and specificity. BMJ 1994;308: 1552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Altman DG, Bland JM. Diagnostic tests 2: predictive values. BMJ 1994;309: 102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sackett DL, Straus S, Richardson WS, Rosenberg W, Haynes RB. Evidence-based medicine. How to practise and teach EBM. 2nd ed. Edinburgh: Churchill Livingstone, 2000: 67-93.
- 4.Jaeschke R, Guyatt G, Lijmer J. Diagnostic tests. In: Guyatt G, Rennie D, eds. Users' guides to the medical literature. Chicago: AMA Press, 2002: 121-40.
- 5.Straus SE, McAlister FA, Sackett DL, Deeks JJ. The accuracy of patient history, wheezing, and laryngeal measurements in diagnosing obstructive airway disease. CARE-COAD1 Group. Clinical assessment of the reliability of the examination-chronic obstructive airways disease. JAMA 2000;283: 1853-7. [DOI] [PubMed] [Google Scholar]
- 6.Altman DG. Diagnostic tests. In: Altman DG, Machin D, Bryant TN, Gardner MJ, eds. Statistics with confidence. 2nd ed. London: BMJ Books, 2000: 105-19.
- 7.Fagan TJ. Letter: Nomogram for Bayes theorem. N Engl J Med 1975;293: 257. [DOI] [PubMed] [Google Scholar]