Abstract
Background and Aims:
Bupivacaine is available in isobaric and hyperbaric forms for intrathecal use and opioids are used as additives to modify their effects. The aim of this study was to compare the efficacy and haemodynamic effect of intrathecal isobaric bupivacaine-fentanyl mixture and hyperbaric bupivacaine-fentanyl mixture in common urological procedures.
Methods:
One hundred American Society of Anesthesiologists physical status 1 and 2 patients undergoing urological procedures were randomized into two groups. Group 1 received 3 ml of 0.5% isobaric bupivacaine with 25 μg fentanyl while Group 2 received 3 ml of 0.5% hyperbaric bupivacaine with 25 μg fentanyl. The parameters measured include heart rate, blood pressure, respiratory rate, onset and duration of motor and sensory blockade. Student's unpaired t-test and the χ2 test were used to analyse the results, using the SPSS version 11.5 software.
Results:
The haemodynamic stability was better with isobaric bupivacaine fentanyl mixture (Group 1) than with hyperbaric bupivacaine fentanyl mixture (Group 2). The mean onset time in Group 1 for both sensory block (4 min) and motor block (5 min) was longer compared with Group 2. The duration of sensory block (127.8 ± 38.64 min) and motor block (170.4 ± 27.8 min) was less with isobaric bupivacaine group compared with hyperbaric bupivacaine group (sensory blockade 185.4 ± 16.08 min and motor blockade 201.6 ± 14.28 min). Seventy percent of patients in Group 2 had maximum sensory block level of T6 whereas it was 53% in Group 1. More patients in Group 1 required sedation compared to Group 2.
Conclusion:
Isobaric bupivacaine fentanyl mixture was found to provide adequate anaesthesia with minimal incidence of haemodynamic instability.
Keywords: Bupivacaine, fentanyl, hyperbaric, isobaric, spinal anaesthesia
INTRODUCTION
The advantages of spinal anaesthesia are its rapidity in onset, safety and reliability. The baricity of a solution is the ratio of the density of solution to that of the cerebrospinal fluid (CSF). The importance of isobaric spinal anaesthesia is that the distribution of drug is not dependent on the positioning of the patient during the injection of drug. For an anaesthetic drug to become hyperbaric, the baricity should be above 1.0015 at 37°C. This can be achieved by adding dextrose to the solution. For hyperbaric solutions the distribution depends on the positioning of the patient. Addition of other drugs to local anaesthetics may help in reducing the dosage of local anaesthetics, reduce adverse effects and prolong the duration of anaesthesia.
Most of the previous studies were conducted using either hyperbaric or isobaric bupivacaine for lower limb procedures and caesarean sections, and additives were rarely added.[1,2] The purpose of this study was to compare the efficacy of isobaric bupivacaine with fentanyl and hyperbaric bupivacaine with fentanyl for spinal anaesthesia and to study the haemodynamic effects and recovery in common infraumbilical urological surgeries.
METHODS
This was a prospective randomized double blinded study. Written informed consent was taken from the patients after explaining the procedure in detail and Ethical Committee approval was obtained. The study was conducted for a period of 3 years. Hundred adult patients undergoing elective infraumbilical urological procedures, under spinal anaesthesia were selected. The randomization was performed by block randomization technique into two groups. The concealment was achieved by computer generated block selection.
Group 1 patients (study group) received 3 ml of preservative free 0.5% isobaric bupivacaine, 15 mg (Neon pharmaceuticals) with fentanyl 25 μg (Fendrop®-Sun pharma) making a total volume of 3.5 ml of drug. Group 2 patients (control group) received 3 ml of preservative free 0.5% hyperbaric bupivacaine, 15 mg (Anawin®-Neon pharmaceuticals) with fentanyl 25 μg making a total volume of 3.5 ml of study drug.
Patients aged between 18 and 60 years of both genders, belonging to the American Society of Anesthesiologists (ASA) physical status 1 and 2 were included. The patients excluded were those who refused spinal anaesthesia, who were hypovolaemic, uncooperative and those with spinal deformity or pre-existing neurological deficit.
Pre-operative evaluation was performed and patients were pre-medicated with diazepam 5 mg the night before surgery and on the morning of surgery.
The patients were shifted onto the operating table and intravenous access was obtained with an 18 gauge cannula. The patients were pre-loaded with 10 ml/kg of crystalloids. Monitors such as pulse oximeter, electrocardiogram, non-invasive BP were connected.
Lumbar puncture was performed under aseptic precautions, in the left lateral position, at L3-L4 space. Using a 25 gauge Quincke Babcock spinal needle, spinal anaesthesia was performed by an anaesthesiologist blinded to the drug injected. The drug syringes were prepared before injection by another anaesthesiologist who was not involved in the study. Three ml of isobaric/hyperbaric bupivacaine (15 mg) with fentanyl 25 μg was injected intrathecally according to the study groups allocated. Patients were placed in the supine position immediately. After 10 min patients were put in lithotomy position.
Intra-operative and post-operative assessments were performed by an anaesthesiologist blinded to the patient allocation and study drugs. The following parameters were evaluated: The primary outcome measures were heart rate (HR) variation, blood pressure (BP) variation, respiratory rate (RR) variation, onset and duration of sensory and motor block.
Time of onset of sensory block was assessed as the time interval between completion of injection of local anaesthetic solution to the onset of complete loss of sensation to pinprick in the anterior axillary line bilaterally at T10 level by a hypodermic needle every 5 min for 15 min. Maximum level of sensory blockade was taken as the level achieved after 20 min of completion of injection of local anaesthetic solution. Duration of sensory block was assessed by 2 segments regression time.
Motor block assessed by modified Bromage scale. Time of onset of motor blockade was assessed as the time interval between injection of local anaesthetic solution to the establishment of grade 4 on the Bromage scale. Duration of motor blockade was assessed as the time interval between completion of local anaesthetic injection, to patient's ability to flex feet.
Side effects such as giddiness, nausea/vomiting, shivering, respiratory depression were noted.
In case of an inadequate subarachnoid block or if the duration of spinal anaesthesia did not last longer than the duration of surgery, patients were supplemented with intravenous sedation/general anaesthesia.
Sample size of 50 each was arrived at based on pilot study (where onset and duration of block were delayed with use of hypobaric bupivacaine) for a power of 80% and α error of 0.05.
Statistical analysis was performed using the SPSS version 11.5 software (SPSS Inc., 233 South Wacker Drive, 11th Floor Chicago, IL, USA). The tests used for statistical analysis were the Student's unpaired t-test and the χ2 test. Student's unpaired t-test ANOVA with repeated measurement was used.
RESULTS
One hundred patients of either sex and between 18 and 60 years of age participated in this study. Each group had 50 patients each and there were no dropouts from the study.
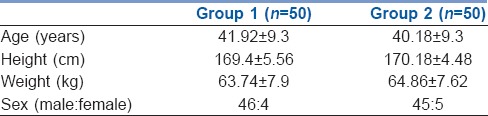
Demographic characteristics were similar in both groups [Table 1]. The mean age for the Group 1 was 41.9 years; while that for Group 2 was 40.2 years. The average height (in centimetres) in both the groups was comparable. (169.4 ± 5.56 and 170.18 ± 4.48 in Group 1 and Group 2 respectively) and so was the weight (in kilogram) (63.74 ± 7.9 and 64.86 ± 7.62 respectively). The gender distribution was also comparable.
Table 1.
Demographic characteristics
The comparison of mean systolic BP (SBP) values between the two groups showed that the differences were significant from the 5 min interval onwards (P < 0.05) between the two study groups. In Group 2, there was a sharp fall in the SBP after 5 min until 15 min, unlike in Group 1 where there was more stable SBP [Figure 1]. Mean diastolic BP (DBP) values between the two groups showed that the DBP in Group 1 was stable compared to Group 2. The statistical analysis showed that the differences were significant from 5 min interval onwards up to 15 min interval (P < 0.05) between the two study groups. The mean DBP fell from the 5 to the 15 min, but was maintained following the administration of fluids and vasopressors in Group 2 [Figure 2].
Figure 1.
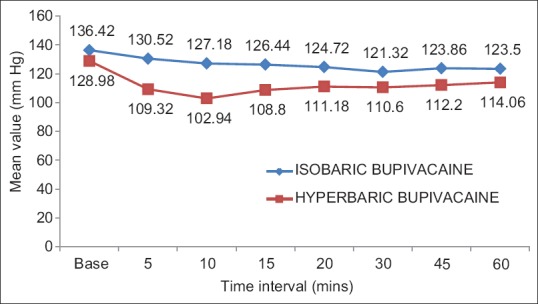
Comparison of mean systolic blood pressure changes between groups. P < 0.05 from 5 min onwards
Figure 2.
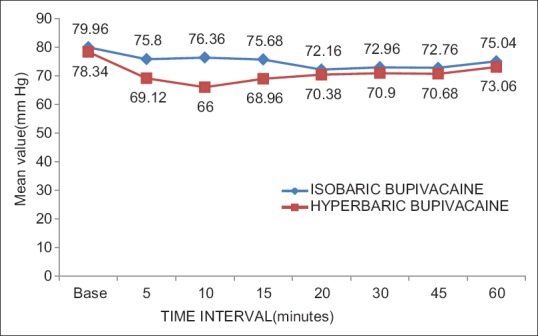
Comparison of mean diastolic blood pressure changes between groups. P < 0.05 from 5 min onwards
The comparison of the mean HR values between the two groups showed no statistical significance between the two study groups. The comparison of the mean RR values between the two groups showed no statistical significance between the two study groups.
The mean onset time of sensory block in isobaric bupivacaine group was 4 min (mean - 4.78, standard deviation [SD] - 2.93) whereas for hyperbaric bupivacaine group the corresponding values observed were 1 min (mean - 1.05, SD - 0.312). The mean onset of motor block in isobaric bupivacaine group was 5 min (mean - 5.54, SD - 2.79) whereas for hyperbaric bupivacaine group the onset of motor block took 1 min (mean - 1.23, SD - 0.193). The statistical analysis showed significant differences in both sensory and motor block onset (P < 0.05) between the two study groups whereas there was a delay in the onset of both motor and sensory block in Group 1 [Figure 3].
Figure 3.
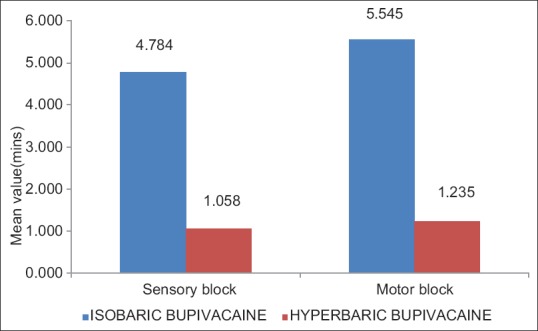
Onset of sensory and motor block
The mean duration of sensory block in Group 1 was 127.8 min (±SD 38.6) whereas for Group 2 the same was 185.4 min (± SD 16.08). The mean duration of motor block in Group 1 was 170.4 min (±SD 27.8), whereas for Group 2, it was 201.6 min (±SD 14.28) [Figure 4]. The statistical analysis showed the differences were significant in both the duration of sensory and motor block (P < 0.05) between the two study groups. The duration of sensory and motor block was much shorter in Group 1]. In Group 2, 70% of patients had a a maximum sensory level of T6 whereas in Group 1, most patients (52%) had a maximum sensory level of T10.
Figure 4.
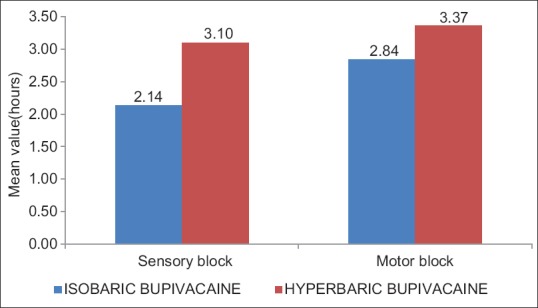
Mean duration of sensory block and motor block
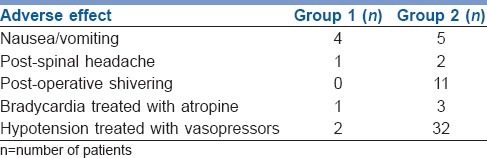
Increased incidence of post-operative shivering, hypotension and bradycardia were noted in Group 2 as compared with Group 1 [Table 2]. Forty two percent patients in Group 1 required supplemental sedation after spinal anaesthesia for anxiolysis and 8% in Group 2.
Table 2.
Incidence of adverse effects
DISCUSSION
Subarachnoid block is one of the most popular techniques but has the disadvantages of sympathetic and motor block resulting in hypotension, bradycardia and immobility. Sensory blockade with reduction in complications can be achieved by adding drugs such as opioids, hence, local anaesthetics combined with opioids are the appropriate choice.
There are numerous benefits of using opioids with local anaesthetics for spinal anaesthesia compared to systemic opioids in the perioperative period, like superior analgesia with shorter time to ambulation, fewer pulmonary complications, earlier return of bowel function, earlier hospital discharge rates, and a decreased stress response.
Better haemodynamic stability was observed with use of isobaric bupivacaine plus fentanyl compared to hyperbaric bupivacaine plus fentanyl mixture in the present study. The time of onset of sensory blockade in hyperbaric and isobaric solution groups were not much different clinically and so was the case with respect to the onset of motor blockade. The duration of both sensory and motor block was prolonged with hyperbaric than isobaric bupivacaine fentanyl mixture which was clinically significant.
Hallworth et al.[1] studied the effect of position and baricity on the spread of intrathecal bupivacaine. The patients were given 10 mg of hyperbaric, isobaric or hypobaric bupivacaine in combined spinal epidural technique either in sitting or right lateral position. They found that baricity had no effect on spread of sensory levels in lateral position compared to sitting position. In the sitting position hypobaric bupivacaine produced higher sensory levels (T2) than hyperbaric bupivacaine. Increased baricity produced less motor blockade which was evident in lateral position. The isobaric mixture was injected in the L3-4 space getting a median maximum sensory level of T2 and for hyperbaric it was T3. The isobaric mixture was not affected by posture unlike the hyperbaric or the hypobaric mixture.[1] Based on this study we decided to keep the left lateral position as the standard position for the spinal anaesthesia procedure. Unlike the study above, we were able to observe only a mean maximum sensory block level of T10 in the majority (52%) of our cases with only 4% ascending up to a T4 level using the isobaric mixture.
The isobaric solution produced a mean spread of analgesia to T2 which was quite unlike our study where T10 was the mean. There was variation in the level of hyperbaric spread, which was T3 in the above study, while it was T6 in our study. The difference could be attributed to the use of combined spinal epidural technique used in the above mentioned study and also may be due to the variation in the drug dosage and addition of fentanyl to the study drug. The isobaric solution produced a more predictable level of blockade compared to the hyperbaric solution. Placing the patient in the lithotomy position did not show any significant difference in the level of sensory blockade.[1]
In a study comparing intrathecal isobaric/hyperbaric bupivacaine combined with fentanyl or morphine for patients undergoing caesarean section, isobaric bupivacaine 9 mg with either 200 μg morphine or 25 μg fentanyl and hyperbaric bupivacaine 12.5 mg with either 200 μg morphine or 25 μg fentanyl were administered. It was found that there was a significant drop in BP in 1st min in all the four groups. Intrathecal morphine with isobaric bupivacaine had the longest duration of analgesia. The visual analogue scale score in post-operative period was highest for intrathecal fentanyl with isobaric bupivacaine and was lesser for hyperbaric bupivacaine fentanyl group. This was similar to our findings where duration of analgesia was longer for hyperbaric bupivacaine fentanyl group.[3]
In another study comparing intrathecal isobaric and hyperbaric bupivacaine anaesthesia for lower abdominal surgeries, 20 mg bupivacaine was used without additives. There was no statistically significant haemodynamic variation between the two groups. It was found that the onset of analgesia and motor blockade was faster with isobaric bupivacaine and the duration of analgesia was prolonged with isobaric bupivacaine, which was contrary to our findings where hyperbaric bupivacaine had a faster onset and a longer duration of analgesia.[4]
In a Cochrane analysis comparing six studies including 394 patients with intrathecal hyperbaric and isobaric bupivacaine,[5] the results were almost similar to our study. It was found that hyperbaric bupivacaine had rapid onset of analgesia and requirement for supplemental analgesia were also less. However variability in the dose, use of adjuvant drugs and differences in the technique used for regional anaesthesia should be taken into consideration.[5]
In another study comparing isobaric and hyperbaric bupivacaine 10 mg, with 25 μg fentanyl for elective caesarean sections, it was found that there was no statistically significant difference in the onset of sensory blockade and time to reach maximal (T4) level. However, isobaric bupivacaine took more time for two dermatomes sensory level regression below T4 and resulted in prolonged block duration, as against our findings where hyperbaric drug had a longer duration of blockade.[6]
Dextrose free solutions of bupivacaine can be slightly hypobaric compared to CSF; the sitting position is likely to cause a greater cephalad spread.[7] Under controlled clinical conditions, for example, Axelsson et al. found that decreasing the volume of drug injected decreased the level of anaesthesia to T10-11 level, but a volume <1.5 ml was not associated with a further decrease in level of anaesthesia.[2] With increasing volume there was an increase in the duration of analgesia and the onset time for complete motor blockade was less. Time to maximum cephalad spread took about 15–18 min in all groups. Time for 2–3 segment regression was on an average between 1.5 and 2 h and the rate of regression was similar in all groups (while using 3 ml the rate of regression was 101 ± 15.4 min to reach a T10 level). Based on this study we took 3 ml as standard volume of bupivacaine in our study. Though we added 25 μg of fentanyl to the mixture, we did not find considerable difference in the results.
Our study results correlated with the studies by Chambers et al. and Møller et al.[8,9] There was a similar fall in SBP following the administration of spinal anaesthesia with the hyperbaric mixture.[9] In our study, the duration of action of bupivacaine was less with the isobaric group. In general, 3 ml of bupivacaine injected into the lumbar subarachnoid space produces anaesthesia to T7-8 level and making the volume of drug above or below this produces proportionately higher or lower level of anaesthesia.[2,8,9,10]
Hypobaricity of plain or glucose-free bupivacaine solutions has been demonstrated in studies[11] but frequently they are referred to as ‘isobaric’ in literature.[12,13] More recently, several studies using high precision equipment to accurately measure the density of commonly used intrathecal drugs and human CSF at 37°C have confirmed that plain bupivacaine is indeed hypobaric in comparison with human CSF.[14]
In another study comparing ropivacaine (12 mg) and bupivacaine (8 mg) with 20 μg fentanyl, it was found that lower doses of local anaesthetics provide effective analgesia when supplemented with additives. In our study, we decided to use 15 mg of drug, as it was the basic dose used in our daily practice as an academic hospital, where the duration of surgery is unpredictable. The study subjects in our study belonged to ASA 1-2 whereas in the other study it was geriatric patients of ASA 2-3 which required lesser dosage in view of the possible adverse effects.[15]
One limitation of our study was that we could have optimized the dose (<15 mg) of local anaesthetic solution in pilot study. In addition, the visual analogue scores could have been included in the assessment criteria.
CONCLUSION
Intrathecal isobaric bupivacaine-fentanyl mixture may be associated with better haemodynamic stability and lesser duration of both sensory and motor blockade, thereby enabling quicker recovery from anaesthesia in urological and infra umbilical surgeries as compared with hyperbaric bupivacaine fentanyl mixture
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Hallworth SP, Fernando R, Columb MO, Stocks GM. The effect of posture and baricity on the spread of intrathecal bupivacaine for elective cesarean delivery. Anesth Analg. 2005;100:1159–65. doi: 10.1213/01.ANE.0000149548.88029.A2. [DOI] [PubMed] [Google Scholar]
- 2.Axelsson KH, Widman GB, Sundberg AE, Hallgren S. A double-blind study of motor blockade in the lower limbs. Studies during spinal anaesthesia with hyperbaric and glucose-free 05% bupivacaine. Br J Anaesth. 1985;57:960–70. doi: 10.1093/bja/57.10.960. [DOI] [PubMed] [Google Scholar]
- 3.Saracoglu A, Saracoglu KT, Eti Z. Comparative study of fentanyl and morphine in addition to hyperbaric or isobaric bupivacaine in combined spinal anaesthesia for caesarean section. Arch Med Sci. 2011;7:694–9. doi: 10.5114/aoms.2011.24141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mochamat H, Yusmein U, Bambang S, Untung W. Comparison of intrathecal use of isobaric and hyperbaric bupivacaine during lower abdomen surgery. J Anesthesiol. 2014;10:1155–10. [Google Scholar]
- 5.Sia AT, Tan KH, Sng BL, Lim Y, Chan ES, Siddiqui FJ. Use of hyperbaric versus isobaric bupivacaine for spinal anaesthesia for caesarean section. Cochrane Database Syst Rev. 2013;5 doi: 10.1002/14651858.CD005143.pub2. CD005143. [DOI] [PubMed] [Google Scholar]
- 6.Gurmukh D, Gauhar A. Spinal anaesthesia for caesarean section: Plain vs hyperbaric bupivacaine. J Pak Med Assoc. 2012;12:620–5. [PubMed] [Google Scholar]
- 7.Kalso E, Tuominen M, Rosenberg PH. Effect of posture and some CSF characteristics on spinal anaesthesia with isobaric 0.5% bupivacaine. Br J Anaesth. 1982;54:1179–84. doi: 10.1093/bja/54.11.1179. [DOI] [PubMed] [Google Scholar]
- 8.Chambers WA, Edstrom HH, Scott DB. Effect of baricity on spinal anaesthesia with bupivacaine. Br J Anaesth. 1981;53:279–82. doi: 10.1093/bja/53.3.279. [DOI] [PubMed] [Google Scholar]
- 9.Møller IW, Fernandes A, Edström HH. Subarachnoid anaesthesia with 0.5% bupivacaine: Effects of density. Br J Anaesth. 1984;56:1191–5. doi: 10.1093/bja/56.11.1191. [DOI] [PubMed] [Google Scholar]
- 10.Pitkänen M, Haapaniemi L, Tuominen M, Rosenberg PH. Influence of age on spinal anaesthesia with isobaric 0.5% bupivacaine. Br J Anaesth. 1984;56:279–84. doi: 10.1093/bja/56.3.279. [DOI] [PubMed] [Google Scholar]
- 11.Blomqvist H, Nilsson A. Is glucose-free bupivacaine isobaric or hypobaric? Reg Anesth. 1989;14:195–8. [PubMed] [Google Scholar]
- 12.Abuzaid H, Prys-Roberts C, Wilkins DG, Terry DM. The influence of diamorphine on spinal anaesthesia induced with isobaric 0.5% bupivacaine. Anaesthesia. 1993;48:492–5. doi: 10.1111/j.1365-2044.1993.tb07068.x. [DOI] [PubMed] [Google Scholar]
- 13.Biboulet P, Deschodt J, Aubas P, Vacher E, Chauvet P, D’Athis F. Continuous spinal anesthesia: Does low-dose plain or hyperbaric bupivacaine allow the performance of hip surgery in the elderly? Reg Anesth. 1993;18:170–5. [PubMed] [Google Scholar]
- 14.Fettes PD, Jansson JR, Wildsmith JA. Failed spinal anaesthesia: Mechanisms, management, and prevention. Br J Anaesth. 2009;102:739–48. doi: 10.1093/bja/aep096. [DOI] [PubMed] [Google Scholar]
- 15.Erturk E, Tutuncu C, Eroglu A, Gokben M. Clinical comparison of 12 mg ropivacaine and 8 mg bupivacaine, both with 20 microg fentanyl, in spinal anaesthesia for major orthopaedic surgery in geriatric patients. Med Princ Pract. 2010;19:142–7. doi: 10.1159/000249581. [DOI] [PubMed] [Google Scholar]


