Abstract
Excessive use of alcohol has been identified as a major contributor to the global burden of disease. Excessive use of alcohol is a component cause of more than 200 disease and injury conditions. Alcohol use has been associated with increased morbidity and mortality across all regions of the world including South-East Asia. Epidemiological as well as clinic-based studies from Western countries have reported a high prevalence of co-occurrence of alcohol use disorder and psychiatric disorders. The research has established the clinical relevance of this comorbidity as it is often associated with poor treatment outcome, severe illness course, and high service utilization. Understandably, dual disorders in from of alcohol use disorders and psychiatric disorders present diagnostic and management challenge. The current article is aimed to review systematically the published Indian literature on comorbid alcohol use disorders and psychiatric disorders.
Keywords: Alcohol, comorbidity, dual diagnosis, dual disorders, mood disorders, psychosis, schizophrenia, sexual disorders, substance use disorders
INTRODUCTION
Excessive use of alcohol has been identified as a major contributor to the global burden of disease. It causes 5.9% of all deaths globally. In addition, it is responsible for 5.1% of the disability-adjusted life years.[1] Excessive use of alcohol is a component cause of more than 200 disease and injury conditions. Alcohol use has been associated with increased morbidity and mortality across all regions of the world including South-East Asia.[2]
Epidemiological[3,4,5,6] as well as clinic based[7,8] studies from Western countries have reported a high prevalence of comorbidity of alcohol use disorder and psychiatric disorders. The research has established the clinical relevance of this comorbidity as it is often associated with poor treatment outcome, severe illness course, and high service utilization. Understandably, dual disorders in form of alcohol use disorders and psychiatric disorders present diagnostic and management challenge. Hence, it is important to study systematically the dual disorders. The current article is aimed to review systematically the published Indian literature on co-occurring alcohol use disorders and psychiatric disorders.
MATERIALS AND METHODS
Search strategy
Electronic database of PubMed and IndMed were searched for relevant publications. The search was carried out in May 2015 and included publications until (and including May 2015). For PubMed, Boolean search was carried out using a combination of “Diagnosis, Dual (Psychiatry)” AND “India.” Furthermore, all the publications listed using the search term “Diagnosis, Dual (Psychiatry)” were screened for Indian studies on co-occurring alcohol use disorders and psychiatric disorders. Electronic database of IndMed offers a simple search using keywords. Hence the search was carried out using different terms including “Alcohol;” “Cannabis;” “Opioids;” “Inhalants;” “Sedatives;” “Hallucinogens;” “Stimulants;” “Cocaine;” “Amphetamine type stimulants;” “Buprenorphine;” “Pentazocine;” “Dextropropoxyphene;” “Heroin;” “Opium;” “Afeem;” “Smack;” “Morphine;” “Bhang;” “Charas;” “Ganja;” “Hashish;” “Benzodiazepines;” “Zolpidem;” “Toluene;” “Lysergic Acid Diethylamide;” “Ketamine;” “Caffeine;” “Nicotine;” “Tobacco.” Electronic archives of Indian Journals on Psychiatry and Psychological Medicine were also searched for relevant studies. Additional published material was identified from the bibliography of the studies screened and evaluated. Furthermore, the relevant publications were selected from the bibliography of earlier reviews on the related topics.
Study selection
For the purpose of the present review, English language peer-reviewed studies conducted among human subjects were included. Animal studies were excluded from the present review.
Data extraction
Information was extracted using a structured proforma from the publications that met the above-mentioned inclusion and exclusion criteria. Data were extracted pertaining to co-occurring alcohol use disorders and psychiatric disorders. Furthermore, the publications that assessed various psychoactive substances (including alcohol use) and psychiatric disorders were also included in the review. The information was extracted by two authors using predefined criteria.
RESULTS
Publication selection and characteristics
The search results and publication selection have been presented in Figure 1.
Figure 1.
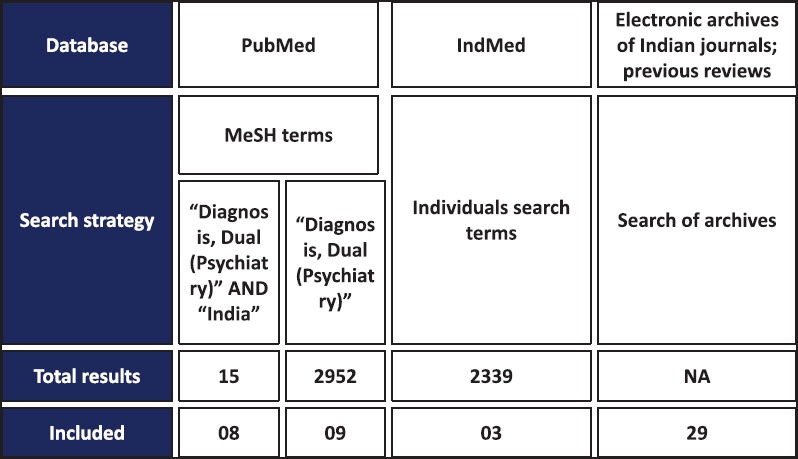
Search results using different search strategies for literature on co-occurring psychiatric disorders and alcohol use disorders
A total of 15 manuscripts were found following a search using Boolean search terms “Diagnosis, Dual (Psychiatry)” AND “India.” Ten of these publications were relevant and were included in the review. PubMed search with “Diagnosis, Dual (Psychiatry)” resulted in 2957 studies of which nine were relevant and included in the review. Twenty-seven relevant publications were found through IndMed and Indian Journals on Psychiatry and Psychological Medicine. A total of 13 publications on co-occurring alcohol use disorder and psychiatric disorders were included in the current review [Table 1].
Table 1.
Publications that have explored co-occurring alcohol use disorders and psychiatric disorders in Indian setting (arranged in ascending order of year of publication)
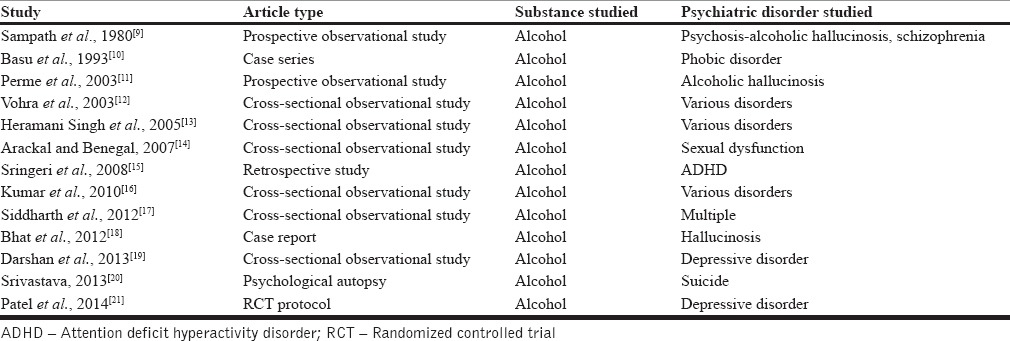
Furthermore, 22 publications on various psychoactive substances (including alcohol use) and psychiatric disorders were included in the current review [Table 2].
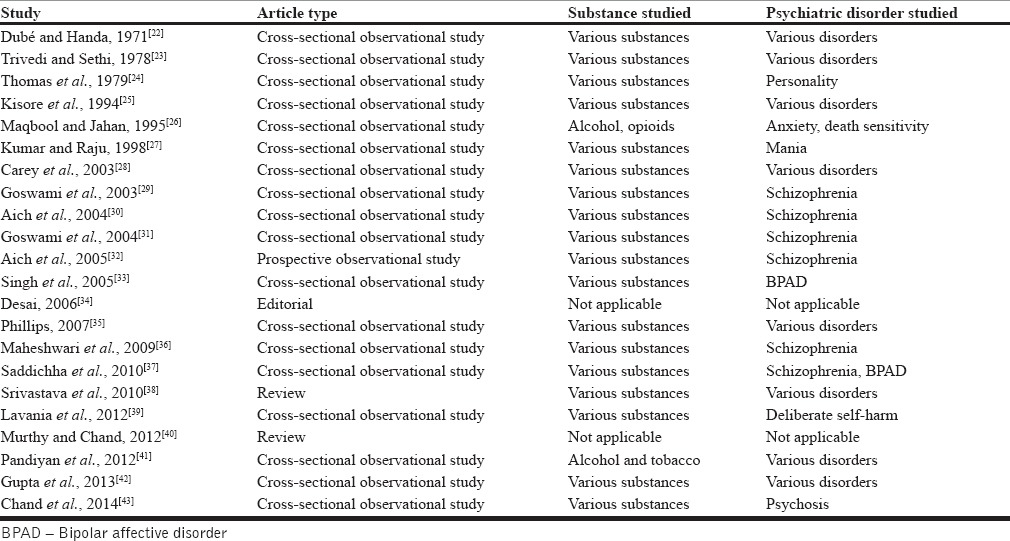
Table 2.
Publications that have explored co-occurring various substance (including alcohol) use disorders and psychiatric disorders in Indian setting (arranged in ascending order of year of publication)
Types of publications
Twenty-three publications included in the current review were cross-sectional observational studies.[12,13,14,16,17,19,22,23,24,25,26,27,28,29,30,31,35,36,37,39,41,42,43] Other publication types on dual disorders from India included reviews (three publications),[33,38,44] prospective observational studies (three publications),[9,11,32] case reports/series (two publications),[10,18] retrospective chart review (one publication),[15] randomized controlled trial (RCT) protocol (one publication),[21] psychological autopsy (one publication),[20] and editorial (one publication).[34]
Study population
Almost all the studies have been conducted among male subjects with the exception of few that have been conducted among female subjects[41] or have included female subjects.[19,20] Most of the studies have been conducted among individuals seeking treatment. One study was conducted among the general population.[22] One study was conducted among family members and treatment staff.[35]
Psychoactive substances studied
Alcohol was the psychoactive substance studied in 13 Indian publications on dual disorders.[9,10,11,12,13,14,15,16,17,18,19,20,21] Twenty-two publications reported findings on various psychoactive substances including alcohol.[22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43]
Psychiatric disorders studied
Psychoses (including schizophrenia and alcohol-related psychosis) were studied in 10 publications.[9,11,18,29,30,31,32,36,37,43] Other psychiatric disorders studied include bipolar affective disorder (BPAD) (three publications),[27,33,37] depressive disorders (two publications),[19,21] anxiety disorders two publications),[10,26] sexual dysfunction (two publications),[14,17] deliberate self-harm/suicide (two publications),[20,39] attention deficit hyperactivity disorders (ADHDs) (one publications),[15] and personality disorders (one publication).[24] More than one psychiatric disorder was explored in 14 publications.[12,13,16,17,20,22,23,25,28,35,37,38,41,42]
Time trends in publications on co-occurring alcohol use disorders and psychiatric disorders
The first published journal article on co-occurring alcohol use disorder and psychiatric disorders dates back to 1970s. There has been a steady increase in the proportion of dual disorders publications on alcohol since 1980s. Furthermore, alcohol remains one of the commonly included psychoactive substances in publications on dual disorders involving more than one psychoactive substance since 1990s [Figure 2].
Figure 2.
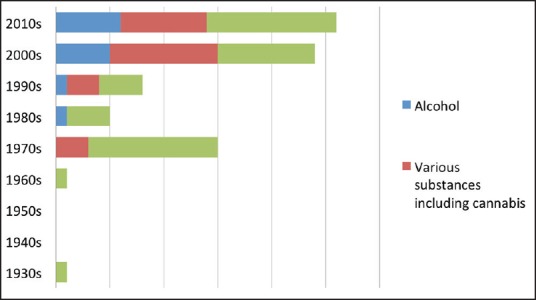
Time trends of publications on co-occurring alcohol use disorder and psychiatric disorders from India
Alcohol use disorders and psychotic disorders
Three publications included in the current review studied co-occurring alcohol use disorders and psychoses.[9,11,18]
Sampath et al.[9] did a comparative study between patients with paranoid schizophrenia (n = 30) and alcoholic hallucinosis (n = 30). Statistically significant findings included a more frequent presentation of delusion of grandiosity, somatic passivity, thought echo, thought broadcast in the patients with paranoid schizophrenia while anxiety, visual hallucinations and hallucinations in multiple modalities were more frequently seen in patients with alcoholic hallucinosis. The illness recovery and outcome of patients with alcoholic hallucinosis was significantly better and more patients with paranoid schizophrenia had first-degree relatives with schizophrenia.
Perme et al.[11] evaluated 52 individuals with a diagnosis of psychotic disorder (predominantly hallucinatory) associated with alcohol use after a 3-year period following diagnosis. Four distinct patient groups emerged with 56% having no hallucinations following abstinence; 21% having no further hallucinatory experiences despite relapsing into alcohol use; 13.5% having experienced hallucinations despite abstaining from alcohol use; and 9.5% having persistent symptoms along with continued alcohol intake. The study concluded that a previous episode of alcoholic hallucinosis was a significant predictor for the development of chronic hallucinosis.
Bhat et al.[18] reported a case of an alcohol-dependent individual who presented with a co-existing symptom constellation of auditory, visual and tactile hallucinations and deterioration in personal care which persisted during periods of abstinence. The individual tested seropositive for human immunodeficiency virus and magnetic resonance imaging brain revealed bilateral lateral ventricle enlargement with narrowing of the lower end of aqueduct of sylvius. He responded well to antipsychotic medications.
Alcohol use disorders and mood disorders
Three publications included in the current review studied co-occurring alcohol use disorders and mood disorders.[19,21,27]
Darshan et al.[19] conducted an online survey of IT professionals to screen for professional stress, depressive symptoms and hazardous drinking. One hundred and twenty-nine interviews were conducted using the snowballing technique. Around 14% of the study population was found to have harmful alcohol use. Professionals experiencing stress were 5.9 times more likely to indulge in harmful drinking as opposed to those who were not stressed while those who were at risk for developing depression had a 4.1 times higher prevalence of harmful alcohol use. Both the findings were observed to be statistically significant.
Patel et al.[21] have published the protocol to study the efficacy of nonpharmacological interventions in patients with comorbid alcohol dependence as well as depressive disorder. The results of the trial have not yet been published.
A study by Kumar and Raju[27] has been described in subsequent sections as it included various psychiatric disorders.
Alcohol use disorders and anxiety disorders
Two publications included in the current review studied co-occurring alcohol use disorders and anxiety disorders.[10,26]
Basu et al.[10] documented two cases of alcohol dependence with comorbid agoraphobia. Both individuals presented with nearly two decades of alcohol use with the onset of phobic symptoms after 2 years and 5 years of onset of alcohol use, respectively. The authors highlighted the phenomenon of “abstinence phobias” through these two cases. Maqbool and Jahan[26] explored for psychopathology in individuals with opioid dependence (n = 120) and alcohol dependence (n = 120). On comparison, the opioid-dependent individuals scored significantly higher on death sensitivity as compared to the alcohol dependent individuals. Individuals who had lower scores on sensation seeking scale had a significantly higher score on the state anxiety scale.
Alcohol use disorders and sexual disorders
Two publications included in the current review studiedco-occurring alcohol use disorders and sexual disorders.[14,17]
Arackal and Benegal[14] assessed 100 inpatient male subjects with a diagnosis of alcohol dependence. Seventy-two percent of the subjects were found to have one or more sexual disorders with premature ejaculation, low sexual desire, and erectile dysfunction being the most common. The number of sexual dysfunction complaints correlated with the amount of alcohol consumed per day.
A study by Siddharth et al.[17] has been described in subsequent sections as it included various psychiatric disorders.
Alcohol use disorders and attention deficit hyperactivity disorder
One publication included in the current review studied co-occurring alcohol use disorders and ADHDs.[15]
Sringeri et al.[15] carried out a retrospective study to establish a relationship between alcohol use and comorbid attention deficit disorder of adult type (ADD) (n = 70). There was an overrepresentation of adult ADHD in the subjects with an early onset of alcohol dependence. The individuals with a childhood history of ADHD or adult ADD had a higher preponderance of developing early onset alcohol use (OR = 5.8).
Alcohol use disorders and various psychiatric disorders
Six publications included in the current review studied co-occurring alcohol use disorders and various psychiatric disorders.[12,13,16,17,20,25]
Kisore et al.[25] cross-sectionally observed psychiatric comorbidity in alcohol dependent and opioid dependent treatment-seeking individuals. They found psychiatric comorbidity among 65.55% individuals with alcohol dependence and 56.6% individuals with opioid dependence. The most common psychiatric comorbidity among those with alcohol dependence was that of mood disorders (46.2%) followed by sexual dysfunction (30.8%). Two and three comorbid diagnoses were present in 32.5% and 27.9% of the patients, respectively. It was seen that the psychiatric comorbidity usually preceded the substance use disorder.
Vohra et al.[12] interviewed 30 consecutive patients of alcohol dependence who presented for the 1st time at a tertiary care center. Seventy-six percent of the individuals were found to have a diagnosable axis I disorder while 40% had an axis II disorder. Depressive disorder (52.1%) and cluster B personality disorders (58.3%) were the most common axis I and II disorders. Those with a dual diagnosis belonged to a younger age group and had frequent hospitalization.
Heramani Singh et al.[13] carried out a comparative analysis of 100 alcohol dependent individuals against healthy controls to look for psychiatric disorders. In the alcohol using group, 92% of the subjects had an additional psychiatric disorder as opposed to a rate of 12% in the healthy controls. Depression was found to be the most common diagnosis among the index group (26%), followed by anti-social personality disorder (21%) and phobia (16%).
Kumar et al.[16] cross-sectionally assessed 37 patients with alcohol dependence in an out-patient clinic in North India for comorbid psychiatric disorders. The patients were diagnosed with psychiatric disorders using Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders, 4th Edition, Text Revision (SCID I and II). Around 65% patients had comorbid illness out of which 50% patients presented with a mood disorder, 45.8% had an anxiety disorder and 25% patients had a psychotic disorder. Two patients were diagnosed with a personality disorder, anti-social personality disorder and paranoid personality disorder respectively. The diagnoses reported were not mutually exclusive with at least 25% of the patients having three comorbid diagnoses.
A case-control study by Siddharth et al.[17] compared the prevalence of psychiatric morbidity and psychosexual dysfunction among subjects with alcohol dependence and healthy matched controls. A significantly higher prevalence of sexual disorders was seen among alcohol dependents with the most common diagnosis being erectile dysfunction (28%), followed by loss of libido (26%), delayed ejaculation (10%), excessive libido (8%), and premature ejaculation (4%). Depression was found among 28% of the study subjects. Other psychiatric disorders included anxiety disorders (10%), personality disorders (8%), BPAD (4%), and psychotic disorders (4%).
Srivastava[20] carried out a psychological autopsy of 100 suicide completers and described their sociodemographic and psychological profile. Treatment seeking behavior prior to attempting suicide was also determined. The sample had a high rate of psychiatric morbidity with a majority having major depressive disorder (54%) and alcohol use disorder (45%). A comorbid presentation of the two disorders together was elicited in a large number of the victims.
Various substance use disorders (including alcohol) and psychiatric disorders
Eleven studies on dual disorders included subjects with various substance use disorders (including alcohol) and psychiatric disorders.[22,23,27,28,33,37,38,40,41,43,44]
Dubé and Handa et al.[22] conducted a household survey in Agra to explore the prevalence of substance use and psychiatric disorders. The survey included 16,725 persons and showed a 5% prevalence rate of dual diagnosis in the general population. Substance use was reported to be twice as common in individuals with psychiatric disorders as compared to those without a psychiatric disorder.
Trivedi and Sethi[23] reported a prevalence rate of 16.4% of substance abuse. Around 9% of the study subjects had abused alcohol, 5% cannabis, 2% minor tranquillizer and 0.7% barbiturates and 0.4% opium. Alcohol was significantly more abused by subjects with bipolar disorders and neurotic disorders, and cannabis was more abused by subjects with schizophrenia and bipolar disorders.
Kumar and Raju[27] assessed the prevalence rate of co-occurrence of substance use disorder among individuals with mania. The commonest substance abused was alcohol (38.7%; 14.9% dependent) followed by cannabis (26.7%; 8.9% dependent). Substance abusers had a relatively severe form of the manic disorder with more dysphoric and irritable mood states and grandiose and persecutory delusions. Also, these individuals had a poorer outcome of mania.
Basu and Gupta[44] reviewed the issues related to management of dual diagnosis disorders such as the ideal location of treatment (in-patient or out-patient), the focus of treatment (substance use or psychiatric illness), the kind of training health care providers require and the practical aspects of the models of care (sequential, parallel or integrated). The authors have informed about all three different models of care with most evidence being in favor of the integrated model in which the same clinician provides treatment for both components of dual diagnosis. The authors recommend that the psychosocial interventions should be implemented along with pharmacotherapy.
Carey et al.[28] reported an 8% prevalence of hazardous drinking in people with mental illness which was low as compared with rates reported from other countries. The study was aimed at psychometric evaluation of the alcohol use disorders identification test and short drug abuse screening test in individual with psychiatric disorders.
Goswami et al.[29] mapped the course of schizophrenia onto the course of substance use in a retrospective study design among 22 dual diagnosis patients with substance use disorders and schizophrenia. The time spent in various phases of schizophrenia (psychotic, nonpsychotic and remission phases) had no significant correlation with whether the subject was using or abstaining from the substance.
Goswami et al.[31] contrasted the psychopathology of patients with schizophrenia who use psychoactive substances (alcohol [n = 22], cannabis and opioids [n = 22]) with patients of schizophrenia who did not use these substances. Alcohol was being used more commonly as a self-medicating agent as compared to opioids and cannabis. In general, patients with dual diagnosis reported lesser emotional distress and mitigation of certain symptoms as one of the purposes of using substance.
Singh et al.[33] compared the quality of life of dual diagnosis patients having bipolar disorder with those having individual disorders. Nearly half of the sample (47.5%) was dependent on alcohol. Patients with dual diagnosis scored significantly poorly on all four domains of quality of life that is, physical health, psychological health, environment and social relationships. In addition, severity of alcohol dependence in this subset of patients had a negative correlation with the quality of life scores.
Saddichha et al.[37] did a comparative analysis of patients with substance use disorders and comorbid schizophrenia (n = 31) and BPADs (n = 31) with patients of “pure” substance use disorders (n = 32). The two groups were matched for age, sex and tobacco use. The amount of substance being used was higher in the group with dual diagnosis, the most frequently used substance was cannabis followed by alcohol. The onset of substance use preceded the onset of the comorbid mental disorder in all. All the patients in the group with schizophrenia and 80% of the patients with BPADs were diagnosed with cannabis dependence while 28% of the participants in the group with no comorbid psychiatric disorder reported cannabis dependence. Conversely, there was no significant difference in the rate of alcohol dependence among the groups with 80% of all patients interviewed being dependent on it.
A review of Indian literature on psychiatric comorbidities by Srivastava et al.[38] explored various comorbidities including dual disorders of substance use and psychiatric disorders. However, the review was limited in comprehensiveness and included only a limited number of Indian studies on dual disorders.
Murthy and Chand[40] in their review of research on management of dual diagnosis specifically focused on the management of patients with substance use with comorbid BPAD and schizophrenia among other psychiatric disorders. The authors found the integrated treatment approach to be superior with a low attrition rate.
The additive effect of substance use as well the occupational distress faced by commercial sex workers seeking psychiatric treatment has been studied by Pandiyan et al.[41] Most common substances used by the study subjects were alcohol (100%), tobacco (74%), opioids (14%), cocaine (6%), and cannabis (6%). The prevalence rate for depression, anxiety and somatic symptoms was found to be 71%, 42%, and 35%, respectively.
Chand et al.[43] screened for psychoactive substance use among treatment naive first episode psychosis patients who presented to an urban treatment setting. They noted a prevalence rate of 20% for substance dependence. Rates of cannabis abuse/dependence were lower in the patients with first-episode psychosis as compared to the data from the Western world. However, the prevalence rate of alcohol dependence in patients with psychosis was higher as compared to previous community studies.
Studies on compliance to treatment and service delivery for individuals with co-occurring alcohol use disorders and psychiatric disorders
Maheshwari et al.[36] compared the compliance to medications among patients with schizophrenia with and without comorbid substance users. Significant rates of noncompliance were found in the substance using individuals. They had more infrequent follow-ups and were irregular with their medications as well. Nicotine was the most commonly used substance in this group followed by alcohol.
Phillips 2007 conducted in-depth semi-structured interviews of 25 care providers of dual diagnosis patients who worked in two Northern states of India. Common substances used were tobacco, alcohol, cannabis and heroin. Depressive and anxiety disorders were commonly seen in these patients with alcohol use while schizophrenia was usually observed in cannabis dependent individuals. A deficiency in the proper care of patients with dual diagnosis by both the family members as well as medical staff was a finding consistently reported by the respondents.
DISCUSSION
There is relatively limited published literature on dual disorders from India. There is no previously published comprehensive review on this theme. In fact, earlier reviews of Indian research on substance use disorders[45] and comorbidity[38,46] have included less than half of the published Indian research articles on dual disorders. The current review included English language literature among human subjects published from India.
A total of 35 relevant studies were included in the review. The majority of the studies were conducted among males with only one being exclusively conducted among female subjects. Also females, even when included, constituted a small fraction of overall sample except for the studies among relatives of probands with substance use disorders where females have constituted a sizable proportion of study subjects. Similarly, all the studies included adult subjects, and no study has been conducted among children, adolescents and elderly. Almost all the studies have been conducted among treatment seeking population. Only few have explored dual disorders in the general population. Even these studies have explored a limited geographical region.
The majority of the published studies have used cross-sectional observational design with only a few studies that have used a case-control design. Some studies have followed up study subjects prospectively. There is a handful of case reports and only one RCT, findings of which are yet to be published. There are no comprehensive reviews, and the published reviews have discussed only selected issues related to dual disorders.
Studies on patients with co-occurring alcohol use disorders and psychiatric disorders have focused on the prevalence of various psychiatric disorders among them. Alcohol use disorders have been shown to have a particularly high rate of psychiatric comorbidity, alcohol dependence is commonly reported to be co-prevalent with mood disorders, anxiety spectrum disorders and sexual dysfunction. While some studies have reported on specific psychiatric disorders such as ADHD, psychoses, mood disorders, anxiety disorders and sexual disorders, others have explored the prevalence of more than one psychiatric disorders. Overall, those who abuse alcohol lead more stressful lives and suffer from cognitive impairment. Research on diverse population groups including software professionals has uniformly noted such impairment on assessment. Diagnosis of multiple comorbidities is not infrequent. The prevalence rate of mood disorders ranged from 26% to 71% across reviewed studies with depressive disorders being a commonly associated comorbidity. The presentation of anxiety spectrum disorders varied between 10% and 45.8% and included agoraphobia and panic disorders. Psychosexual disorders occurred commonly in patients with alcohol dependence and patients often reported multiple sexual dysfunction complaints. Often the symptoms of depression, anxiety and stress have been observed to predate alcohol use. Retrospective analysis of individuals with ADHD and ADD indicates their vulnerability to developing alcohol use disorders. Alcoholic hallucinosis has been reported to have a variable course and a large constellation of symptoms, which are distinct from those of schizophrenia. Studies have also mapped the course of schizophrenia and substance use among individuals with dual disorders and have found a significant association between the two. One study has presented a protocol for RCT for effectiveness and cost-effectiveness of lay counselor-delivered psychological treatments for harmful and dependent drinking and moderate to severe depression in primary care. Management of dual diagnosis poses a tough challenge, and an integrated model of treatment approach has been recommended as being more effective.
Limitations of the studies
The existing studies on dual disorders from India have various limitations. Many studies have explored specific substances and did not assess the possibility of use of other substances. Conversely many studies have overlooked the possibility of additional psychiatric disorders, which could have contributed to the high prevalence of the comorbidity in question.[14]
Most of the studies have stopped short of exploring environmental factors that might have acted in tandem with substance use to result in psychiatric disorders or could have caused substance use in the first place.[12,16,17] Only a few have taken into account additional personality factors and cognitive deficits.
Many studies have a small sample size,[12,16,29,41] and all barring few studies have focused on the treatment seeking population. Such limitations preclude generalizability of the findings to the community. Studies have included a sample of convenience and even did not specifically mention inclusion criteria.
Well controlled longitudinal studies on alcohol use and psychiatric comorbidity which could inform about the cause and effect relationship between the two are conspicuous by their absence. Most of the studies have been carried out cross-sectionally and hence failed to explore a causal association between the substance use disorders and psychiatric disorders.[12,15] This is true for the studies that explored course and outcome as well. Studies that have commented on the causal association between alcohol use and psychiatric disorders have failed to take into consideration the confounding role of other psychoactive substances.[37] Outcome criteria used in certain studies have been narrow and nonstandardized.[9]
In some studies, semi-structured interviewing techniques or screening questionnaires alone were used to diagnose problematic substance use and psychiatric symptoms.[19] Studies either failed to include a suitable control group[17] or the group has not been adequately matched.[13] The details of pattern and frequency of alcohol use were not mentioned in certain studies.
Another common methodological limitation of studies has been the absence of laboratory confirmation of psychoactive substance use or abstinence. The findings reported in the studies regarding the substance use were based on self-report by the study subjects. Reliability of self-report of substance use by treatment seeking individuals has been debated in Indian studies.[47] History of psychiatric morbidity that has been provided by patients has often not been corroborated by other reliable sources in some studies.[25] Similarly, information in some cross-sectional evaluations could have been inaccurate due to recall bias.[15,29]
Most of the studies among treatment-seeking individuals have come from tertiary care treatment centers. Hence, comparability with data from community remains debatable. There is a scarcity of community-based and laboratory-based research to obtain evidence for an etiological association between alcohol use and comorbid mental illness. Studies that have explored the course of psychiatric symptoms among individuals with alcohol use disorders and have attempted to prognosticate the dual diagnosis have either assessed the subjects over a brief follow-up period or have not frequently followed up the patients to intermittently assess the pattern of alcohol intake.[27]
The review on the management of dual disorders highlighted the lack of evidence on this issue from India.[40] Apart from the publication of the study protocol there has not been any original study on the management of comorbid alcohol use disorder sand psychiatric disorder from India so far.
CONCLUSION
The current review has examined the published literature from India on co-occurring alcohol use disorders and psychiatric disorders. A large proportion of the treatment seeking population with alcohol use disorders presented with psychiatric comorbidities. The commonly associated diagnosis included almost all the disorders including mood disorders, psychotic spectrum disorders, anxiety spectrum disorders as well as sexual dysfunction. Personality disorders were also commonly prevalent, and childhood ADHD poses a risk for developing substance use disorder in the future. The duration of alcohol use and the severity of dependence were correlated with presentation and severity of psychiatric symptoms. A high prevalence of dual diagnosis could either mean that the community rate of prevalence of dual disorders is high or that an additional diagnosis increases the chances of treatment seeking behavior by the individual and caregivers. First, this implies that patients presenting with substance use disorders should be screened for psychiatric comorbidity and vice-versa. Second, large-scale community-based studies are indicated for gathering systematic data and to assess the magnitude of a burden on the caregiver and community. There is ambivalence regarding the cause and effect relationship of dual diagnosis. Thus longitudinal studies should be carried out to explore further this relation.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.2014th ed. Geneva: World Health Organisation; 2014. World Health Organisation. Global Status Report on Alcohol and Health. [Google Scholar]
- 2.Balhara Y, Mathur S. Alcohol: A major public health problem-South Asian perspective. Addict Disord Their Treat. 2012;11:101–20. [Google Scholar]
- 3.Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- 4.Wells JE, Bushnell JA, Hornblow AR, Joyce PR, Oakley-Browne MA. Christchurch Psychiatric Epidemiology Study, Part I: Methodology and lifetime prevalence for specific psychiatric disorders. Aust N Z J Psychiatry. 1989;23:315–26. doi: 10.3109/00048678909068289. [DOI] [PubMed] [Google Scholar]
- 5.Bland RC. Psychiatric epidemiology. Can J Psychiatry. 1988;33:618–25. doi: 10.1177/070674378803300708. [DOI] [PubMed] [Google Scholar]
- 6.Andrews G, Slade T, Issakidis C. Deconstructing current comorbidity: Data from the Australian National Survey of Mental Health and Well-Being. Br J Psychiatry. 2002;181:306–14. doi: 10.1192/bjp.181.4.306. [DOI] [PubMed] [Google Scholar]
- 7.Schuckit MA, Tipp JE, Bergman M, Reich W, Hesselbrock VM, Smith TL. Comparison of induced and independent major depressive disorders in 2,945 alcoholics. Am J Psychiatry. 1997;154:948–57. doi: 10.1176/ajp.154.7.948. [DOI] [PubMed] [Google Scholar]
- 8.Darke S, Ross J. Polydrug dependence and psychiatric comorbidity among heroin injectors. Drug Alcohol Depend. 1997;48:135–41. doi: 10.1016/s0376-8716(97)00117-8. [DOI] [PubMed] [Google Scholar]
- 9.Sampath G, Kumar YV, Channabasavanna SM, Keshavan MS. Alcoholic hallucinosis and paranoid schizophrenia-a comparative (clinical and follow up) study. Indian J Psychiatry. 1980;22:338–42. [PMC free article] [PubMed] [Google Scholar]
- 10.Basu D, Raj L, Mattoo SK, Malhotra A, Varma VK. The agoraphobic alcoholic: Report of two cases. Indian J Psychiatry. 1993;35:185–6. [PMC free article] [PubMed] [Google Scholar]
- 11.Perme B, Vijaysagar KJ, Chandrasekharan R. Follow-up study of alcoholic hallucinosis. Indian J Psychiatry. 2003;45:244–6. [PMC free article] [PubMed] [Google Scholar]
- 12.Vohra AK, Yadav BS, Khurana H. A study of psychiatric comorbidity in alcohol dependence. Indian J Psychiatry. 2003;45:247–50. [PMC free article] [PubMed] [Google Scholar]
- 13.Heramani Singh N, Sharma SG, Pasweth AM. Psychiatric co-morbidity among alcohol dependants. Indian J Psychiatry. 2005;47:222–4. doi: 10.4103/0019-5545.43058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Arackal BS, Benegal V. Prevalence of sexual dysfunction in male subjects with alcohol dependence. Indian J Psychiatry. 2007;49:109–12. doi: 10.4103/0019-5545.33257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sringeri SK, Rajkumar RP, Muralidharan K, Chandrashekar CR, Benegal V. The association between attention-deficit/hyperactivity disorder and early-onset alcohol dependence: A retrospective study. Indian J Psychiatry. 2008;50:262–5. doi: 10.4103/0019-5545.44748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kumar V, Dalal P, Trivedi J, Kumar P. A study of psychiatric comorbidity in alcohol dependence. Delhi Psychiatry J. 2010;13:291–3. [Google Scholar]
- 17.Siddharth A, Verma K, Anand M, Harphul S, Lokesh J, Thalor K. Study of psychiatric morbidity and psychosexual dysfunctions in patients of alcohol dependence. Delhi Psychiatry J. 2012;15:379–84. [Google Scholar]
- 18.Bhat PS, Ryali V, Srivastava K, Kumar SR, Prakash J, Singal A. Alcoholic hallucinosis. Ind Psychiatry J. 2012;21:155–7. doi: 10.4103/0972-6748.119646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Darshan MS, Raman R, Rao TS, Ram D, Annigeri B. A study on professional stress, depression and alcohol use among Indian IT professionals. Indian J Psychiatry. 2013;55:63–9. doi: 10.4103/0019-5545.105512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Srivastava A. Psychological attributes and socio-demographic profile of hundred completed suicide victims in the state of Goa, India. Indian J Psychiatry. 2013;55:268–72. doi: 10.4103/0019-5545.117147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Patel V, Weobong B, Nadkarni A, Weiss HA, Anand A, Naik S, et al. The effectiveness and cost-effectiveness of lay counsellor-delivered psychological treatments for harmful and dependent drinking and moderate to severe depression in primary care in India: PREMIUM study protocol for randomized controlled trials. Trials. 2014;15:101. doi: 10.1186/1745-6215-15-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dubé KC, Handa SK. Drug use in health and mental illness in an Indian population. Br J Psychiatry. 1971;118:345–6. doi: 10.1192/bjp.118.544.345. [DOI] [PubMed] [Google Scholar]
- 23.Trivedi J, Sethi B. Drug abuse in psychiatric patients. Indian J Psychiatry. 1978;21:345–8. [Google Scholar]
- 24.Thomas MG, Mohan D, Sahasi G, Prabhu GG. Personality and attitude correlates of drug abuse amongst students of a high school in Delhi: A replicated study. Indian J Med Res. 1979;69:990–5. [PubMed] [Google Scholar]
- 25.Kisore P, Lal N, Trivedi JK, Dalal PK, Aga VM. A study of comorbidity in psychoactive substance dependence patients. Indian J Psychiatry. 1994;36:133–7. [PMC free article] [PubMed] [Google Scholar]
- 26.Maqbool S, Jahan A. State anxiety and death sensitivity among smack addicts and alcoholics. J Indian Acad Appl Psychol. 1995;21:103–8. [Google Scholar]
- 27.Kumar PN, Raju SS. Impact of substance abuse comorbidity on psychopathology and pattern of remission in mania. Indian J Psychiatry. 1998;40:357–63. [PMC free article] [PubMed] [Google Scholar]
- 28.Carey KB, Carey MP, Chandra PS. Psychometric evaluation of the alcohol use disorders identification test and short drug abuse screening test with psychiatric patients in India. J Clin Psychiatry. 2003;64:767–74. doi: 10.4088/jcp.v64n0705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Goswami S, Singh G, Mattoo SK, Basu D. Courses of substance use and schizophrenia in the dual-diagnosis patients: Is there a relationship? Indian J Med Sci. 2003;57:338–46. [PubMed] [Google Scholar]
- 30.Aich TK, Sinha VK, Khess CR, Singh S. Demographic and clinical correlates of substance abuse comorbidity in schizophrenia. Indian J Psychiatry. 2004;46:135–9. [PMC free article] [PubMed] [Google Scholar]
- 31.Goswami S, Mattoo SK, Basu D, Singh G. Substance-abusing schizophrenics: Do they self-medicate? Am J Addict. 2004;13:139–50. doi: 10.1080/10550490490435795. [DOI] [PubMed] [Google Scholar]
- 32.Aich T, Sinha V, Khess C, Singh S. Substance abuse co-morbidity in schizophrenia: An inpatient study of course and outcome. Indian J Psychiatry. 2005;47:33–8. [Google Scholar]
- 33.Singh J, Mattoo SK, Sharan P, Basu D. Quality of life and its correlates in patients with dual diagnosis of bipolar affective disorder and substance dependence. Bipolar Disord. 2005;7:187–91. doi: 10.1111/j.1399-5618.2004.00173.x. [DOI] [PubMed] [Google Scholar]
- 34.Desai NG. Comorbidity in psychiatry: Way forward or a conundrum? Indian J Psychiatry. 2006;48:75–7. doi: 10.4103/0019-5545.31593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Phillips PA. Dual diagnosis: An exploratory qualitative study of staff perceptions of substance misuse among the mentally ill in Northern India. Issues Ment Health Nurs. 2007;28:1309–22. doi: 10.1080/01612840701686468. [DOI] [PubMed] [Google Scholar]
- 36.Maheshwari SK, Gupta S, Sharan P. Medication non-compliance and substance abuse in schizophrenia. Nurs J India. 2009;100:201–3. [PubMed] [Google Scholar]
- 37.Saddichha S, Sur S, Sinha BN, Khess CR. How is substance use linked to psychosis?. A study of the course and patterns of substance dependence in psychosis. Subst Abus. 2010;31:58–67. doi: 10.1080/08897070903442699. [DOI] [PubMed] [Google Scholar]
- 38.Srivastava A, Sreejayan K, Joseph AM, Sharma PS. Indian research on comorbidities. Indian J Psychiatry. 2010;52(Suppl 1):S246–9. doi: 10.4103/0019-5545.69240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lavania S, Ram D, Praharaj SK, Khan AH, Pattojoshi A. Deliberate self-harm in nondepressed substance-dependent patients. J Addict Med. 2012;6:247–52. doi: 10.1097/ADM.0b013e31826508c0. [DOI] [PubMed] [Google Scholar]
- 40.Murthy P, Chand P. Treatment of dual diagnosis disorders. Curr Opin Psychiatry. 2012;25:194–200. doi: 10.1097/YCO.0b013e328351a3e0. [DOI] [PubMed] [Google Scholar]
- 41.Pandiyan K, Chandrasekhar H, Madhusudhan S. Psychological morbidity among female commercial sex workers with alcohol and drug abuse. Indian J Psychiatry. 2012;54:349–51. doi: 10.4103/0019-5545.104822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gupta M, Kumar K, Garg PD. Dual diagnosis vs. triple diagnosis in HIV: A comparative study to evaluate the differences in psychopathology and suicidal risk in HIV positive male subjects. Asian J Psychiatr. 2013;6:515–20. doi: 10.1016/j.ajp.2013.06.012. [DOI] [PubMed] [Google Scholar]
- 43.Chand P, Thirthalli J, Murthy P. Substance use disorders among treatment naïve first-episode psychosis patients. Compr Psychiatry. 2014;55:165–9. doi: 10.1016/j.comppsych.2013.07.075. [DOI] [PubMed] [Google Scholar]
- 44.Basu D, Gupta N. Management of “dual diagnosis” patients: Consensus, controversies and considerations. Indian J Psychiatry. 2000;42:34–47. [PMC free article] [PubMed] [Google Scholar]
- 45.Murthy P, Manjunatha N, Subodh BN, Chand PK, Benegal V. Substance use and addiction research in India. Indian J Psychiatry. 2010;52(Suppl 1):S189–99. doi: 10.4103/0019-5545.69232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kumar V, Kumar P, Bhatia M, Jhanjee A. Substance abuse and Comorbidity. Delhi Psychiatry J. 2010;13:36–42. [Google Scholar]
- 47.Balhara YP, Jain R, Sundar AS, Sagar R. Use of cotinine urinalysis to verify self-reported tobacco use among male psychiatric out-patients. Lung India. 2012;29:217–20. doi: 10.4103/0970-2113.99102. [DOI] [PMC free article] [PubMed] [Google Scholar]


