Abstract
Context:
Antenatal depression is not easily visible, though the prevalence is high. The idea of conducting this study was conceived from this fact.
Aims and Objectives:
The aim of this study was to estimate the prevalence of antenatal depression and identify the risk factors, for early diagnosis and intervention.
Settings and Design:
The study conducted in a Tertiary Care Hospital was prospective and cross-sectional.
Materials and Methods:
Pregnant women between 18 and 40 years of age were studied. The sample size comprised 318 women. They were assessed using Edinburgh Postnatal Depression Scale (EPDS) score, Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition Axis I Disorders, Life Event Stress Scale (LESS), and Life Distress Inventory (LDI).
Statistical Analysis Used:
The Statistical Package for Social Sciences (SPSS) Version 15 software was used to measure percentages, mean, correlation, and P < 0.05 were considered significant.
Results:
Prevalence of antenatal depression in the study was 12.3%. Correlation of the sociodemographic factors, obstetric factors, LDI, and LESS with EPDS scores showed statistical significance for unplanned pregnancy, distress associated with relationships, physical health, financial situation, social life, presence of personality disorder, being a homemaker, and higher educational status.
Conclusion:
The study showed a high prevalence rate of depression and identified risk factors.
Keywords: Antenatal depression, prevalence, risk factors, tertiary care
INTRODUCTION
Antenatal depression is of immense public health importance, as it can adversely affect both the mother and the child. On reviewing literature, we found few Indian studies. What is known about this condition is mainly from Western studies. There is no epidemiological data. There is a need to understand antenatal depression in terms of its prevalence, and the risk factors, that could be used to identify it.
MATERIALS AND METHODS
This was a prospective, cross-sectional study done in an outpatient Department of Obstetrics in a Tertiary Care Hospital, Bengaluru. This study was conducted from November 2013 to May 2014, after obtaining Institutional Ethics Committee approval. During this period, 318 pregnant women between 18 and 40 years of age, in any trimester, without any history of psychotic disorder, substance abuse, or co-morbid medical illness attending routine antenatal checkup were assessed and selected for the study. All 318 women gave informed consent and were screened for depression using Edinburgh Postnatal Depression Scale (EPDS) score. Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) Axis I Disorders (SCID-I) was used for diagnosis of depression. A semi-structured proforma for sociodemographic and obstetric details, Life Event Stress Scale (LESS) and Life Distress Inventory (LDI) were used. The evaluation was done by a trained clinical psychologist and psychiatrists.
All pregnant women in the study went through a detailed physical examination and a detailed clinical workup, including history, and mental status examination.
Edinburgh postnatal depression scale score
The EPDS score is a 10-item screening tool for postnatal depression[1,2] and has also been validated for screening pregnant women for depression.[3] Scores of 10 and above indicate possible depression. It has also been validated for the Indian population.[4]
Structured clinical interview for diagnostic and statistical manual of mental disorders, fourth edition axis i disorders
It is a standardized and semi-structured interview for making the major DSM-IV Axis I diagnosis.[5]
Life event stress scale
This is a 41-item inventory of stressful life events in the past 12 months. Total scores of 0-149 indicate low susceptibility to stress-related illness, 150-299 indicate medium susceptibility, and a score of more than 300 indicates high susceptibility to stress-related illness.
Life distress inventory
The LDI is an 18-item self-rating inventory intended to measure the current level of distress experienced across 18 areas of life. Factor analysis indicated that the instrument measures distress related to marital concerns, career concerns, outside activities (OA), self and family (SF), and life satisfaction/optimism.[6]
Statistical analysis
The study data were analyzed on the Statistical Package for the Social Sciences (SPSS) version-15 software (SPSS Inc., 233 South Wacker Drive, 11th Floor, Chicago, IL), with P < 0.05 taken to be statistically significant. Data were expressed in terms of mean and percentages. Correlation of EPDS scores with various risk factors was done.
RESULTS
In our study, major depressive episode was diagnosed in six patients (1.9%) using SCID-I, 10.4% (n = 33) had possible depression as per EPDS scores and one patient reported active suicidal thoughts. The prevalence of subsyndromal antenatal depression is 5-fold that of syndromal depression.
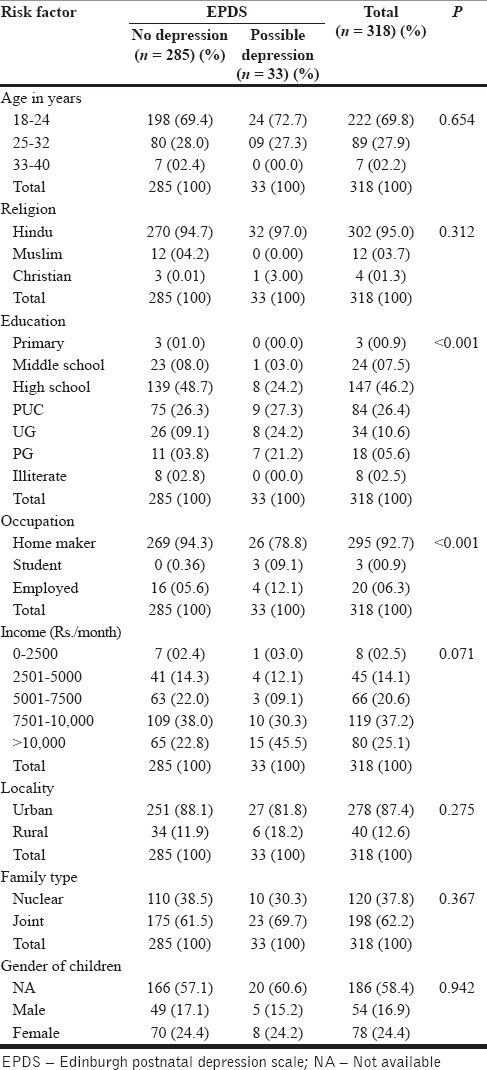
Of the 318 women analyzed, 69.8% were in the age group of 18-24 years with the mean age of 23.2 years, 95% were Hindus, 91.6% had at least more than 8 years of formal education, and 92.7% were homemakers. All the women were married and living with their spouse. Family income of 62.3% of the women was more than 7500 Rs./month, 87.4% lived in urban areas, with 62.2% came from joint family settings. Table 1 shows the correlation of sociodemographic variables with EPDS scores.
Table 1.
Correlation of sociodemographic risk factors with EPDS scores
In our sample of pregnant women, 32 (10%) were in the first trimester, 72 (22.5%) in the second trimester, and 214 (67.5%) in the third trimester. Thirty-three (10.4%) women had scores of 10 or more on EPDS score indicating possible depression, with 19 (57.6%) in the third trimester, 10 (30.3%) in the second trimester, and 4 (12.1%) in the first trimester. Major depressive episode was diagnosed in six patients (1.9%), of which four were in the third trimester and one each in first and second trimesters. The current pregnancy was reported as unplanned by 5 (1.6%) women, and 70 (22.1%) women had at least one abortion in the past with a majority of them. Viz, 58 (82.8%) having a single abortion. Primigravidae constituted more than half (57%) of the study population, 94 (29.6%) women reported normal delivery in the past while 43(13.4%) had a caesarean section. Table 2 shows the correlation of obstetric variables with EPDS scores.
Table 2.
Correlation of obstetric risk factors with EPDS scores
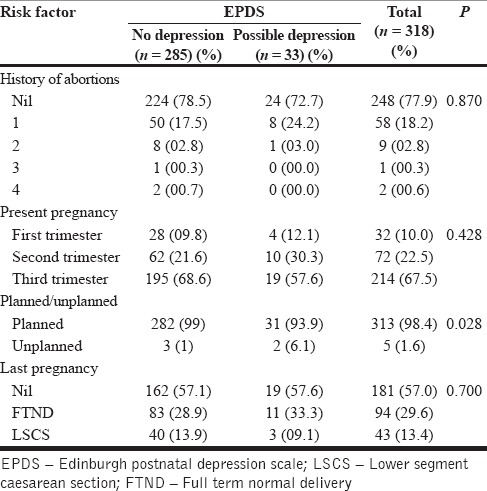
Two women were diagnosed with personality disorders and both qualified for major depressive episode. One was diagnosed with Borderline Personality Disorder and one was diagnosed with Avoidant Personality Disorder (DSM-IV — Text Revision [DSM IV — TR]). Thirty-six women had scores indicating medium to high susceptibility to stress-related illness on LESS with the most common stressors being death of close family member, change in family members health, and change in sleep habits in the past 12 months. On the LDI, 3 women reported more than moderate distress in factors related to relationship with others, physical health, financial situation, and social life. Correlation of the above sociodemographic factors, obstetric factors, LDI, and LESS, with EPDS scores showed statistical significance for higher educational status (P < 0.001), being a homemaker (P < 0.001), unplanned pregnancy(P = 0.028), presence of personality disorder (P < 0.001), and distress associated with relationship with others, physical health, financial situation, and social life (P < 0.001).
DISCUSSION
The antenatal period is a vulnerable period for the mother and the developing fetus. During this period, there are profound physiological and emotional changes in the mother. Thus, depression during pregnancy has deleterious effects on both the fetus and the mother. It can easily be misattributed to normal physiological changes that occur in pregnancy, e.g., disturbed sleep and changes in appetite.
The adverse effects of depression on the fetus start in the antenatal period, with intrauterine growth retardation may continue postpartum, as failure to thrive.[7,8] Also, there is a higher probability of developmental delays, including intellectual disability,[9] poor bonding with the mother, and problems in psychological development in the child.[10,11] Depression in pregnancy is no different from that occurring in any other period. It increases the risk of postpartum depression.[12,13] Depressed mothers are less likely to attend antenatal clinics, and are more prone to substance abuse.[14]
Prevalence of depression in pregnancy ranges from 6% to 25%.[15,16] A systematic review of depression in the three trimesters showed a prevalence rate of 7.4% in the first trimester, 12.8% in the second trimester and 12% during the third trimester.[17] The two Indian studies on antenatal depression reported prevalence rates of 9.8%[18] and 17%.[19]
In our study, major depressive episode was diagnosed in six patients (1.9%) using SCID-I, 10.4% (n = 33), and had possible depression as per EPDS scores, a total of 12.3%. One patient reported active suicidal thoughts. Previous studies have also reported a higher prevalence of depression with self-rating questionnaires (EPDS, Beck Depression Inventory [BDI] scores) than with structured clinical interviews (SCID, M.I.N.I. International Neuropsychiatric Interview).[20] However, only few studies have used both SCID and rating scales. The two studies on antenatal depression from India have also used self-rating questionnaires for diagnosis of depression, viz. BDI.[18] and Hospital Anxiety and Depression Scale[19] with prevalence rates of 9.8% and 17%, respectively. Thus, a significant number of pregnant women, who do not meet the full diagnostic criteria for major depressive episode, have subsyndrome depression. There is lack of information about the role of subsyndrome depressive symptoms on the well-being of mother-child dyad.
Risk factors for depression in pregnancy include low income, low educational attainment[21] childhood abuse,[22] family history of psychiatric illness, past history of depression, premenstrual symptoms,[23,24] unplanned pregnancy,[25] history of previous abortions,[26] low self-esteem,[27] antenatal anxiety,[28] low social support, marital conflicts,[29] medical problems, stressful life events, single status, domestic violence,[30,31] and unemployment.[32]
Most of the women (69.8%) in the current study were in the age group of 18-24 years, which is in keeping with the sociocultural aspect of early marriage and childbirth in the Indian society. Majority of the women were educated for more than 8 years, of whom 11% (n = 32) had scores of ≥10, indicating possible depression on EPDS score (P < 0.01). Only 6.3% of the women were employed and 92.8% were homemakers. Thus, being educated and unemployed was significantly associated with depression, which may be due to unfulfilled aspirations. This finding is contrary to previous studies which have reported low educational status, as a risk factor for antenatal depression.[21,29] Family income was not significantly associated with depression, which may be due to the fact that majority of women had family income in the middle class range. About 87.7% of the patients were from urban areas, of which 62.6% lived in a joint family. This is contrary to the general trend of increasing number of nuclear families in both rural and urban areas.
Only five women (1.6%) reported the current pregnancy as unplanned, which may be due to the joint family set up, wherein, the planning of the family structure is given importance. Though the gender of the children from past pregnancy was not statistically significant, 3 (50%) of the women diagnosed with major depressive episode expressed significant apprehension that the current pregnancy could result in a female child, and this apprehension increased as the due date approached. This reflects the cultural aspects and the risk of domestic violence which the mother may have to suffer if a female child is born.[33]
Two of the patients were diagnosed with personality disorders, for which the inter-rater reliability among the researchers was good. One of the patients was diagnosed with avoidant personality disorder and the other with borderline personality disorder (DSM-IV — TR), and both were diagnosed with major depressive episode, making personality disorder a possible risk factor.
Among the above variables — unplanned pregnancy (P = 0.028), the presence of personality disorders (P < 0.001) were significantly associated with depression.
Three women reported more than moderate distress on LDI and the distress was mostly associated with factors related to SF (relationship with relatives, physical health, and financial situation) and OA (recreation/leisure, social life). Also, 11.3% (n = 36) of women had medium to high susceptibility to stress-related illness with death of close family member, change in family members health, and change in sleep habits in the past 12 months being the most common stressful life events.
CONCLUSION
This study included a large sample size. Evaluation for depression was done using both SCID and a self-rating questionnaire, which allowed us to compare the prevalence of major depressive disorder with subsyndromal depressive symptoms.
Also, detailed mental status examination, done by psychiatrists, helped identify personality disorders, using DSM-IV — TR. Comprehensive evaluation of risk factors for depression including sociodemographic and obstetric in a large sample of pregnant women was done. Limitation of the study was that it was conducted in a tertiary care hospital, and hence the findings cannot be generalized to the general population.
The results of this study suggest that the prevalence of antenatal depression, as seen in hospitals, is only the tip of the iceberg. Syndromal depression in pregnant women is far exceeded by subthreshold depression.
It is possible that many of the subsyndromal cases become syndromal at a later date and hence the need for early detection. If the risk factors are kept in mind, and the index of suspicion is high, it would enable early detection, and intervention for antenatal depression.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150:782–6. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- 2.Leverton TJ, Elliott SA. Is the EPDS a magic wand? 1. A comparison of the Edinburgh Postnatal Depression Scale and health visitor report as predictors of diagnosis on the Present State Examination. J Reprod Infant Psychol. 2000;18:279–96. [Google Scholar]
- 3.Thorpe K. A study of the Edinburgh postnatal depression scale for use with parent groups outside the postpartum period. J Reprod Infant Psychol. 1993;11:119–25. [Google Scholar]
- 4.Fernandes MC, Srinivasan K, Stein AL, Menezes G, Sumithra R, Ramchandani PG. Assessing prenatal depression in the rural developing world: A comparison of two screening measures. Arch Womens Ment Health. 2011;14:209–16. doi: 10.1007/s00737-010-0190-2. [DOI] [PubMed] [Google Scholar]
- 5.First MB, Spitzer RL, Gibbon M, Williamson JB. Washington, DC: American Psychiatric Press Inc; 1996. Structure Clinical Interview for DSM-IV Axis I Disorder Clinical Version. [Google Scholar]
- 6.Thomas EJ, Yoshioka MR, Ager RD. Life distress inventory. In: Fischer J, Corcoran K, editors. Measures of Clinical Practice: A Sourcebook. Vol. 2. New York: Free Press; 1994. p. 267. [Google Scholar]
- 7.Rahman A, Iqbal Z, Bunn J, Lovel H, Harrington R. Impact of maternal depression on infant nutritional status and illness: A cohort study. Arch Gen Psychiatry. 2004;61:946–52. doi: 10.1001/archpsyc.61.9.946. [DOI] [PubMed] [Google Scholar]
- 8.Patel V, Prince M. Maternal psychological morbidity and low birth weight in India. Br J Psychiatry. 2006;188:284–5. doi: 10.1192/bjp.bp.105.012096. [DOI] [PubMed] [Google Scholar]
- 9.Moses-Kolko EL, Roth EK. Antepartum and postpartum depression: Healthy mom, healthy baby. J Am Med Womens Assoc. 2004;59:181–91. [PubMed] [Google Scholar]
- 10.Stewart RC. Maternal depression and infant growth: A review of recent evidence. Matern Child Nutr. 2007;3:94–107. doi: 10.1111/j.1740-8709.2007.00088.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Patel V, Rahman A, Jacob KS, Hughes M. Effect of maternal mental health on infant growth in low income countries: New evidence from South Asia. BMJ. 2004;328:820–3. doi: 10.1136/bmj.328.7443.820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Heron J, O’Connor TG, Evans J, Golding J, Glover V. ALSPAC Study Team. The course of anxiety and depression through pregnancy and the postpartum in a community sample. J Affect Disord. 2004;80:65–73. doi: 10.1016/j.jad.2003.08.004. [DOI] [PubMed] [Google Scholar]
- 13.Johanson R, Chapman G, Murray D, Johnson I, Cox J. The North Staffordshire Maternity Hospital prospective study of pregnancy-associated depression. J Psychosom Obstet Gynaecol. 2000;21:93–7. doi: 10.3109/01674820009075614. [DOI] [PubMed] [Google Scholar]
- 14.Zuckerman B, Amaro H, Bauchner H, Cabral H. Depressive symptoms during pregnancy: Relationship to poor health behaviors. Am J Obstet Gynecol. 1989;160(5 Pt 1):1107–11. doi: 10.1016/0002-9378(89)90170-1. [DOI] [PubMed] [Google Scholar]
- 15.Ryan D, Milis L, Misri N. Depression during pregnancy. Can Fam Physician. 2005;51:1087–93. [PMC free article] [PubMed] [Google Scholar]
- 16.Gavin NI, Gaynes BN, Lohr KN, Meltzer-Brody S, Gartlehner G, Swinson T. Perinatal depression: A systematic review of prevalence and incidence. Obstet Gynecol. 2005;106(5 Pt 1):1071–83. doi: 10.1097/01.AOG.0000183597.31630.db. [DOI] [PubMed] [Google Scholar]
- 17.Bennett HA, Einarson A, Taddio A, Koren G, Einarson TR. Prevalence of depression during pregnancy: Systematic review. Obstet Gynecol. 2004;103:698–709. doi: 10.1097/01.AOG.0000116689.75396.5f. [DOI] [PubMed] [Google Scholar]
- 18.Ajinkya S, Jadhav PR, Srivastava NN. Depression during pregnancy: Prevalence and obstetric risk factors among pregnant women attending a tertiary care hospital in Navi Mumbai. Ind Psychiatry J. 2013;22:37–40. doi: 10.4103/0972-6748.123615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mina S, Balhara YPS, Verma R, Mathur S. Anxiety and depression amongst the urban females of Delhi in Ante-partum and Post-partum period. Delhi Psychiatry J. 2012;15:347–51. [Google Scholar]
- 20.Roomruangwong C, Epperson CN. Perinatal depression in Asian women: Prevalence, associated factors, and cultural aspects. Asian Biomed. 2011;5:179–93. [Google Scholar]
- 21.Rahman A, Creed F. Outcome of prenatal depression and risk factors associated with persistence in the first postnatal year: Prospective study from Rawalpindi, Pakistan. J Affect Disord. 2007;100:115–21. doi: 10.1016/j.jad.2006.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rodgers CS, Lang AJ, Twamley EW, Stein MB. Sexual trauma and pregnancy: A conceptual framework. J Womens Health (Larchmt) 2003;12:961–70. doi: 10.1089/154099903322643884. [DOI] [PubMed] [Google Scholar]
- 23.Lteif Y, Kesrouani A, Richa S. Depressive syndromes during pregnancy: Prevalence and risk factors. J Gynecol Obstet Biol Reprod (Paris) 2005;34(3 Pt 1):262–9. doi: 10.1016/s0368-2315(05)82745-0. [DOI] [PubMed] [Google Scholar]
- 24.Leigh B, Milgrom J. Risk factors for antenatal depression, postnatal depression and parenting stress. BMC Psychiatry. 2008;8:24. doi: 10.1186/1471-244X-8-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Iranfar S, Shakeri J, Ranjbar M, NazhadJafar P, Razaie M. Is unintended pregnancy a risk factor for depression in Iranian women? East Mediterr Health J. 2005;11:618–24. [PubMed] [Google Scholar]
- 26.Marcus SM, Flynn HA, Blow FC, Barry KL. Depressive symptoms among pregnant women screened in obstetrics settings. J Womens Health (Larchmt) 2003;12:373–80. doi: 10.1089/154099903765448880. [DOI] [PubMed] [Google Scholar]
- 27.Bolton HL, Hughes PM, Turton P, Sedgwick P. Incidence and demographic correlates of depressive symptoms during pregnancy in an inner London population. J Psychosom Obstet Gynaecol. 1998;19:202–9. doi: 10.3109/01674829809025698. [DOI] [PubMed] [Google Scholar]
- 28.Field T, Diego M, Hernandez-Reif M, Schanberg S, Kuhn C, Yando R, et al. Pregnancy anxiety and comorbid depression and anger: Effects on the fetus and neonate. Depress Anxiety. 2003;17:140–51. doi: 10.1002/da.10071. [DOI] [PubMed] [Google Scholar]
- 29.Lau Y, Keung DW. Correlates of depressive symptomatology during the second trimester of pregnancy among Hong Kong Chinese. Soc Sci Med. 2007;64:1802–11. doi: 10.1016/j.socscimed.2007.01.001. [DOI] [PubMed] [Google Scholar]
- 30.Da Costa D, Larouche J, Dritsa M, Brender W. Psychosocial correlates of prepartum and postpartum depressed mood. J Affect Disord. 2000;59:31–40. doi: 10.1016/s0165-0327(99)00128-7. [DOI] [PubMed] [Google Scholar]
- 31.Rahman A, Iqbal Z, Harrington R. Life events, social support and depression in childbirth: Perspectives from a rural community in the developing world. Psychol Med. 2003;33:1161–7. doi: 10.1017/s0033291703008286. [DOI] [PubMed] [Google Scholar]
- 32.Andajani-Sutjahjo S, Manderson L, Astbury J. Complex emotions, complex problems: Understanding the experiences of perinatal depression among new mothers in urban Indonesia. Cult Med Psychiatry. 2007;31:101–22. doi: 10.1007/s11013-006-9040-0. [DOI] [PubMed] [Google Scholar]
- 33.Mahapatro M, Gupta RN, Gupta V, Kundu AS. Domestic violence during pregnancy in India. J Interpers Violence. 2011;26:2973–90. doi: 10.1177/0886260510390948. [DOI] [PubMed] [Google Scholar]


