Abstract
Background:
Female patients hospitalized for a long duration in psychiatric hospitals are a special population with unique needs.
Aims and Objectives:
To assess rehabilitation needs of chronic female inpatients attending psychiatric rehabilitation services in a tertiary care psychiatric hospital.
Materials and Methods:
Rehabilitation needs of nine chronic female inpatients were assessed with an interview schedule developed by expert consensus. The needs were elicited from the patients. Perspectives of nursing staff, vocational instructors, and treating psychiatrists were also sought.
Results and Conclusion:
Most patients expressed the need for more incentives for working in day-care, variety in food and grooming items. The nursing staff felt many patients could be placed outside, and the family members should come more frequently to meet them. Vocational instructors felt that patients need more incentives, variety in food and work. Treating psychiatrists said that major barriers in discharging and placing them were nonavailability or poor involvement of family members. Services like supported housing, supported education and supported employment are necessary to cater to their complex needs.
Keywords: Chronic inpatients, day-care, female, rehabilitation needs
INTRODUCTION
Need can be defined as “whatever is required for health or comfort;” though there are various ways to look at it as normative, felt, expressed, fundamental, etc.[1] A person with psychiatric disorder needs all things that anybody needs to lead a good life.[2]
A person's need at a given point of time is likely to be influenced by different factors including type of illness,[3] stage of illness, response to treatment, age, gender,[4] socioeconomic status, support system, and place of stay. Some studies, however, show that needs of persons with severe mental illness are not related to age, gender and education.[5] Whereas persons recovered from these illnesses may express many needs; persons with severe negative symptoms may express minimal needs or no needs.
The needs arise due to dysfunction in various areas of life. Rehabilitation needs assessment help us understand gaps in existing services and resolving them. Some needs are unmet due to resource constraints or lack of awareness. Unmet needs further reduce the quality of life of persons with psychiatric illness.[5,6]
There are numerous studies assessing rehabilitation needs of persons with psychiatric illnesses. Numerous scales and schedules are available to explore rehabilitation needs of persons with psychiatric illness. These include needs for care assessment,[7] Camberwell assessment of needs (CAN),[8,9] and perceived rehabilitation needs questionnaires for people with schizophrenia.[10]
The most commonly used schedule in Indian studies for assessing rehabilitation needs are rehabilitation needs assessment scale (RNAS)[11] and CAN.[8,9] RNAS schedule collects purely qualitative information from patients (on 6 items) and caregivers (on 2 items), but does not require observer rating.[11] CAN is a family of questionnaires to assess needs of persons with mental health problems. It has clinical practice versions, research version, and short appraisal schedule version (CANSAS) for persons with severe mental illness.[9] It assesses needs of patients, family, and health care staff. There is a patient self-completion version of CANSAS.
The Indian studies have assessed rehabilitation needs in out-patient[11,12,13,14] or in-patient[15] set-up or both.[16,17] Studies have assessed rehabilitation needs from caregivers of persons with chronic mental illnesses in a community sample[18] and in inpatients.[19] The patients in these studies were suffering from schizophrenia,[6,11,12,14,16,19,20] chronic psychosis,[17] severe mental illness comprising bipolar disorder, schizophrenia, and psychosis not otherwise specified (NOS).[13,15,18] The main needs expressed in these studies were need for employment (65%) and help for family (55%);[11] accommodation for in-patients and help for family for outpatients;[16] social skills (80%), employment (65%), providing help to families (60%);[17] help for family and modification in families’ attitude toward them;[13] attitude modification, employment and help for family[14] and help for family, employment, vocational training and psychosocial modification.[20] A retrospective case records based study on needs of chronic psychiatric patients admitted in a tertiary hospital, reported the need for the development of community outreach programs, especially in areas where no psychiatric services are available.[15]
Kulhara et al. (2010) reported that patients expressed the need for welfare benefits, information about condition, money, help for psychotic symptoms and psychological distress.[12] In the same study, caregivers expressed the need for help in welfare benefits, psychological distress, money, company, and intimate relationships.[12] Caregivers in community sample expressed needs in areas of help for the family, employment and occupation, psychosocial modification and skills training.[18] Caregivers of in-patients with schizophrenia patients reported felt need in managing the behavior and social-vocational problems of patients; health issues of caregivers; education about schizophrenia; rehabilitation; and managing sexual and marital problems of patients.[19] In a study of 101 patients with schizophrenia, 42 had high unmet needs.[6] This was associated with poverty, lower education, and persistent psychopathology.[6]
In an Indian Psychiatric Society Multicentric study on assessment of health care needs of persons with severe mental illness, patients reported needs in money, welfare benefits, transport, information about the illness and treatment, relief of psychological distress, company, household skills, and intimate relationships.[21]
Psychiatric rehabilitation services (PRS) at the National Institute of Mental Health and Neurosciences (NIMHANS), Bengaluru runs a day-care center for in-patients and outpatients. At any given point of time, 40-50 day boarders and 25-30 inpatients avail these services. The center has a range of vocational sections including candle making, bakery, bamboo, weaving, plastic molding, tailoring, horticulture, carpentry, leather, printing, crafts, recreation, domestic skills, and computer section. Nine female patients admitted in a closed ward for many years (2-27 years) due to difficulty in discharging them attend various sections of their choice during the day.
There are no published studies about rehabilitation needs of chronic female inpatients in India. The current study was planned to assess rehabilitation needs of this special population to help us understand and cater to their needs.
Aim
To assess the rehabilitation needs of chronic female inpatients attending day-care in PRS, NIMHANS, Bengaluru, Karnataka, India.
MATERIALS AND METHODS
Interview schedule
Due to unique needs of this special population, an interview schedule was developed by expert consensus [Box 1]. Focused group discussion was done among the authors of the paper, after going through available scales/schedules.[8,9,10,11] The schedule included needs like accommodation, safety, diet, grooming, privacy, illness management, family, relationships, sexual, recreation, education, occupation, vocational training, financial, emotional, spiritual and any other needs. The participants were asked “In addition to whatever facilities you are availing here, do you need anything else?” before applying the interview schedule. They were asked to elaborate on their responses.
Box 1.
Rehabilitation needs of chronic inpatients
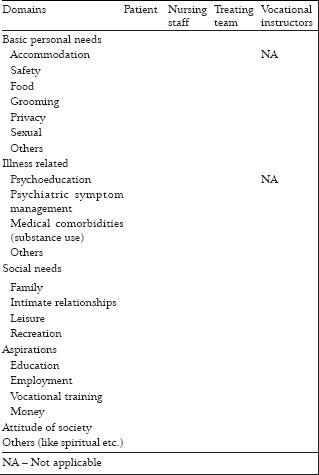
As the patients resided in the hospital, their interactions were limited to nursing staff, hospital attenders, vocational instructors in day-care and treating team. The perspectives of nursing staff in patient's ward, vocational section instructor of the day-care section attended by the patient and treating psychiatrist (senior resident in psychiatry) were also independently sought.
Sample
Nine female inpatients hospitalized for more than 1-year and attending day-care in PRS were included in this study. Informed consent was obtained from the patients for the study. Assent was sought from the treating team. Sociodemographic details were collected using proforma designed for the study. The diagnosis made by the treating unit was noted. Information on rehabilitation needs was collected based on interview schedule. Institute ethics committee clearance was obtained for the study.
RESULTS
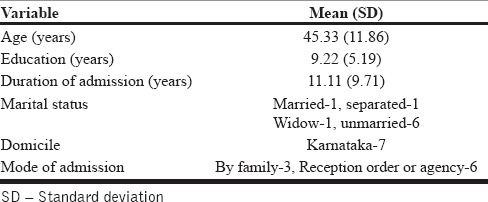
The sociodemographic details are mentioned in Table 1. Four patients were diagnosed with Schizophrenia, four patients with bipolar affective disorder and one patient was diagnosed with mental retardation with epilepsy with psychosis NOS.
Table 1.
Sociodemographic details
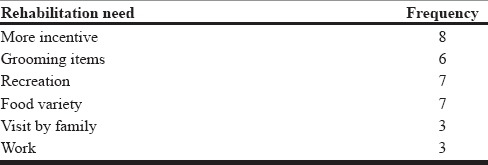
Detailed interview about rehabilitation needs was not possible for the patient with mental retardation with epilepsy with psychosis NOS due to her symptomatic status. However, she was functioning well at the vocational section. Hence, rehabilitation needs have been mentioned for eight patients from patient's perspective [Table 2] and nine patients from perspective of nursing staff, treating team and vocational instructors [Tables 3–5].
Table 2.
Rehabilitation needs: Patient's perspective (n = 8)
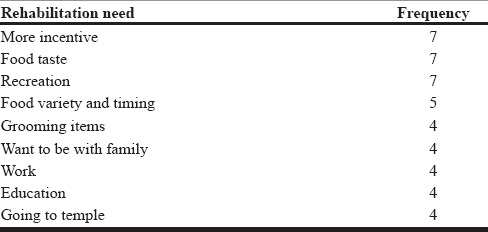
Table 3.
Rehabilitation needs: Nursing staff's perspective for nine patients
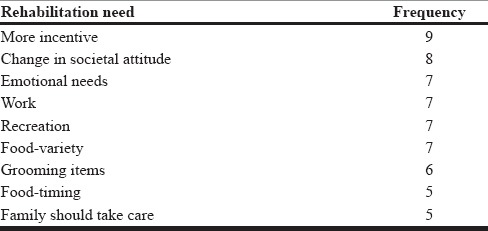
Table 5.
Rehabilitation needs: Vocational instructor's perspective for nine patients
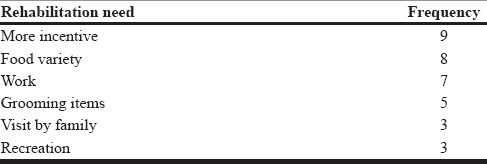
Table 4.
Rehabilitation needs: Treating team's perspective for nine patients
The patients were staying in the closed ward as either they did not have any close family members (5) or their family was not willing to take them home currently (4). The family of one patient who claimed she was married couldn’t be traced.
They were attending the following vocational sections: bamboo (3), computer (2), tailoring (1), mat weaving (1), leather (1), and craft section (1).
To the question “In addition to whatever facilities you are availing here do you need anything else?” 8 out of 9 reported that they did not want anything else. Only one patient reported that she wanted a “light job.” They reported their needs only after asking specifically about each of the item. Most of the patients and all hospital staff interviewed felt that the hospital provided the patients safe, clean accommodation, and enough privacy.
In terms of food, both patients and hospital staff felt that breakfast was provided early. They felt that more variety in food and better taste was needed. The treating doctors felt that more nutritious and less oily food should be provided to these patients; though one of the doctors felt that the food given here was okay as the patient had never complained. Patients expressed unmet needs in grooming such as talcum powder, soap, paste, shampoo, ornaments, etc. which they required when they went out of the ward for day-care. Patients expressed unmet needs in recreation like listening to music, watching TV, and reading books. Four of them also wanted to go to a temple once in a while.
Everyone interviewed expressed the need for increasing monthly incentives, which can enable patients to have food of their choice occasionally and buy items for grooming. Most of the patients wanted incentives from Rs. 150/month to Rs. 1500-2000/month. Only two of them expressed that they need to earn up to Rs. 5000-6000/month. Similar expectations were from the nursing staff about the patients. Treating psychiatrists and vocational section instructors wished that the patients should get more incentives but did not specify any amount. One of the doctors was not aware about how much incentives patient was getting and could not comment.
The nursing staff felt that only two patients needed to stay in closed ward and rest of them could be placed outside or sent out to work. They also expressed need for change in society's attitude toward patients. Three patients also expressed need for change in society's attitude toward patient.
Some interesting suggestions by the treating doctors were about having facilities of listening to music and beauty-parlor facilities for the patients. They also felt that patients should not have uniforms in these closed wards. The senior residents felt that the therapists should see them like other patients.
DISCUSSION
Most of them felt safe in the hospital premises and had enough privacy. The most commonly expressed rehabilitation needs were more incentive for attending day-care, change in food timing, more variety in food, avenues for recreation and more involvement by family.
Five out of nine patients were symptomatic, but were referred to day-care as the treating team felt that they were fit to engage in activities. The patient who could not be interviewed in detail was highly productive in the section she was attending. This shows that symptom status may not correlate with functioning for patients.
Patients expressed needs only after being asked specifically about each need. This could be due to different reasons. Probably they were not asked about the needs previously or they might not have felt the need to express themselves or they did not think that these needs might be fulfilled. This highlights the fact that patients may not spontaneously come out with their needs and have to be specifically asked about it.
Both patient and staff felt that patients had enough privacy, even though they stayed in general wards (15-20 patients in one ward) and used common toilets. The possible reason is that patients may have got used to living in the same environment.
The hospital staff felt that seven of them could be sent for work, but only four among those seven patients expressed interest in working. This could be due to various reasons. They felt secure in the hospital atmosphere where their basic needs were met. They might not be confident of opportunities and support from the society. They did not have felt need to earn and support themselves. Age could have been an important factor. Only two of them were around 30 years of age. Others were 40 or more than 40 years of age (5 of them in 40s and 2 in 60s).
The nursing staff expressed concern regarding the change in societal attitude towards patients, but only three patients expressed the need for change. Patients again might have got used to the environment in the hospital, and their interaction with the society had reduced significantly. A similar view was not expressed by either treating team or vocational instructors as they might be with the patient for limited time, but nursing staff were observing these patients more closely. The nursing staff also felt that the patients’ emotional needs were not met.
Vocational instructors’ expressed need that patients should get more incentives, have more variety in food and they should be engaged in work.
The patients had material needs like variety and taste of food, some grooming items, and an increase in incentives. They were happy with other services provided. At the time of the study, they were getting an incentive of Rs. 60/month. The patients expected incentive was as low as Rs. 150/month. It is possible that patients had got “used to” living in the current situation with limited needs and were unaware about increasing costs of things in the outside world. The hospital authorities were sensitized about this, and the incentive has recently been increased to Rs. 700/month.
Most of the patients had expressed passive recreation needs (listening to music, watching TV); they did not express much active recreation (going out, playing games etc.). This suggests that they might have got used to spend time just sitting in the ward in their free time. Services need to be tailor-made[1] for each patient to meet their needs.
We had included sexual needs in the schedule, but we did not probe it specifically as it was a sensitive issue. Patients themselves did not express about it spontaneously.
Many of the expressed needs could be met if the patients were placed back in the community. An important barrier was a lack of family support. There were no close family members for some patients. For others, family members were not willing to take them home. Some of them could not adjust in nongovernmental organizations when they were placed outside and came back to the hospital again.
In future, careful admissions should be planned to avoid families abandoning patients in the ward. For prolonged admissions where family members cannot stay with the patient, families should make regular visits to meet the patients and should take them out for a short duration. In those with poor family support, attempts to reintegrate patients back to the community should be pursued at the earliest. Else, patients may become comfortable in the hospital, which may make attempts in community reintegration difficult. As evidenced in the present study, long-term hospitalization can reduce aspirations for independent living of patients.
For chronic patients who are hospitalized due to poor family support, the hospital atmosphere may not be geared to cater to their complex aspirational/emotional needs. Such patients are in a state of “handicaptivity”[22] who are left with little options other than accepting the security of a hospital due to lack of better available alternatives. National Human Rights Commission, India (2012) recommends that authorities may find some jobs for fully recovered patients on nominal remunerations within the hospital to rehabilitate them.[23] Positive social role models, avenues to take up a career/studies, fulfillment of social milestones (like getting married, being financially independent, becoming parents) and support in their pursuits is necessary to help them in their road to recovery. It is important to develop services like supported housing, supported education and supported employment to cater to their complex needs. Such supported approaches will be helpful in social reintegration, reduce stigma, improve quality life, and reduce disability and dependency on the hospital set-up.
Limitations
Small sample size, interviews were not audio-taped, emotional needs were not asked from patients once the nursing staff expressed about them.
CONCLUSION
There are unique unmet rehabilitation needs of this special population. Most patients do not express their needs spontaneously and have to be probed. Tailor-made interventions and supported approaches are required to meet their needs.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Asadi-Lari M, Packham C, Gray D. Need for redefining needs. Health Qual Life Outcomes. 2003;1:34. doi: 10.1186/1477-7525-1-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anthony W. The experience of mental illness: An introduction to psychiatric rehabilitation. In: Pratt CW, Gill KJ, Barrett NM, Roberts MM, editors. Psychiatric Rehabilitation. 3rd. San Diego: Academic Press, Elsevier; 2014. [Google Scholar]
- 3.MacPherson R, Gregory N, Slade M, Foy C. Factors associated with changing patient needs in an assertive outreach team. Int J Soc Psychiatry. 2007;53:389–96. doi: 10.1177/0020764007078338. [DOI] [PubMed] [Google Scholar]
- 4.Arvidsson H. Gender differences in needs and care of severely mentally ill persons: Findings from a Swedish cross-sectional and longitudinal study. Int J Soc Psychiatry. 2010;56:424–35. doi: 10.1177/0020764009106631. [DOI] [PubMed] [Google Scholar]
- 5.Wiersma D. Needs of people with severe mental illness. Acta Psychiatr Scand Suppl. 2006;429:115–9. doi: 10.1111/j.1600-0447.2005.00728.x. [DOI] [PubMed] [Google Scholar]
- 6.Ernest S, Nagarajan G, Jacob KS. Assessment of need of patients with schizophrenia: A study in Vellore, India. Int J Soc Psychiatry. 2013;59:752–6. doi: 10.1177/0020764012456801. [DOI] [PubMed] [Google Scholar]
- 7.Brewin CR, Wing JK, Mangen SP, Brugha TS, MacCarthy B. Principles and practice of measuring needs in the long-term mentally ill: The MRC needs for care assessment. Psychol Med. 1987;17:971–81. doi: 10.1017/s0033291700000787. [DOI] [PubMed] [Google Scholar]
- 8.Phelan M, Slade M, Thornicroft G, Dunn G, Holloway F, Wykes T, et al. The Camberwell assessment of need: The validity and reliability of an instrument to assess the needs of people with severe mental illness. Br J Psychiatry. 1995;167:589–95. doi: 10.1192/bjp.167.5.589. [DOI] [PubMed] [Google Scholar]
- 9.Slade M, Thornicroft G, Loftus L, Phelan M, Wykes T. London: Gaskell; 1999. CAN: Camberwell Assessment of Need. [Google Scholar]
- 10.Wong AH, Tsang HW, Li SM, Fung KM, Chung RC, Leung AY, et al. Development and initial validation of perceived rehabilitation needs questionnaire for people with schizophrenia. Qual Life Res. 2011;20:447–56. doi: 10.1007/s11136-010-9767-5. [DOI] [PubMed] [Google Scholar]
- 11.Nagaswami V, Valecha V, Thara R, Rajkumar S, Menon MS. Rehabilitation needs of schizophrenic patients — A preliminary report. Indian J Psychiatry. 1985;27:213–20. [PMC free article] [PubMed] [Google Scholar]
- 12.Kulhara P, Avasthi A, Grover S, Sharan P, Sharma P, Malhotra S, et al. Needs of Indian schizophrenia patients: An exploratory study from India. Soc Psychiatry Psychiatr Epidemiol. 2010;45:809–18. doi: 10.1007/s00127-009-0126-1. [DOI] [PubMed] [Google Scholar]
- 13.Pillai RR, Sahu KK. Rehabilitation needs of persons with major mental illness in India. Int J Psychosoc Rehabil. 2010;14:95–104. [Google Scholar]
- 14.Pavithra SR, Niveditha S, Dharitri R. Rehabilitation needs of persons with schizophrenia and their families. Artha J Soc Sci. 2013;12:33–46. [Google Scholar]
- 15.Chadda RK, Pradhan SC, Bapna JS, Singhal R, Singh TB. Chronic psychiatric patients: An assessment of treatment and rehabilitation-related needs. Int J Rehabil Res. 2000;23:55–8. [PubMed] [Google Scholar]
- 16.Gandotra S, Paul SE, Daniel M, Kumar K, Raj HA, Sujeetha B. A preliminary study of rehabilitation needs of in-patients and out-patients with schizophrenia. Indian J Psychiatry. 2004;46:244–55. [PMC free article] [PubMed] [Google Scholar]
- 17.Singh TB, Kaloiya GS, Kumar S, Chadda RK. Rehabilitation need assessment of severely mentally ill and effect of intervention. Delhi Psychiatry J. 2010;13:109–16. [Google Scholar]
- 18.Prafulla S, Murthy SK, Ramaprasad D. Family burden and rehabilitation need of beneficiaries of a rural mental health camp in a southern state of India. Int J Psychosoc Rehabil. 2010;15:5–11. [Google Scholar]
- 19.Jagannathan A, Thirthalli J, Hamza A, Hariprasad VR, Nagendra HR, Gangadhar BN. A qualitative study on the needs of caregivers of inpatients with schizophrenia in India. Int J Soc Psychiatry. 2011;57:180–94. doi: 10.1177/0020764009347334. [DOI] [PubMed] [Google Scholar]
- 20.Shihabuddeen I, Bilagi S, Krishnamurthy K, Chandran M. Rehabilitation needs and disability in persons with schizophrenia and the needs of the care givers. Delhi Psychiatry J. 2012;15:118–21. [Google Scholar]
- 21.Grover S, Avasthi A, Shah S, Lakdawala B, Chakraborty K, Nebhinani N, et al. Indian Psychiatric Society multicentric study on assessment of health-care needs of patients with severe mental illnesses. Indian J Psychiatry. 2015;57:43–50. doi: 10.4103/0019-5545.148520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Deegan P. Silence: What We Don’t Talk about in Rehabilitation. [Last accessed on 2015 Apr 23]. Available from: https://www.patdeegan.com/pat-deegan/lectures/silence .
- 23.New Delhi: National Human Rights Commission; 2012. National Human Rights Commission. Care and treatment in mental health institutions. Some glimpses in the recent period; p. 157. [Google Scholar]


