Abstract
Introduction:
For many years, family blood donors have been considered less safe than volunteer non-remunerated blood donors and actively discouraged by international organisations and affluent countries support agencies for developing countries. In addition to safety, pressure and coercion was considered unethical. However these assumptions were not supported by evidence.
Aims of the study:
To assemble recently collected evidence to reopen the assessment whether or not the ban of family blood donors is justified.
Methods:
Review of old and recent literature through Pubmed and references from identified articles.
Results and Discussion:
Viral marker data comparing confirmed seroprevalence in 1st time volunteer non-remunerated donors (VNRD) and family/replacement donors (FRD) corrected for gender and age, show no significant difference between the two groups. Evidence has been provided that for both VNRD and FAD benevolence is more appropriate than altruism. The two groups merge for psychological attitude to donation for which knowing someone needing transfusion is a powerful incentive to give blood. Excluding a life or death situation found in areas where severe blood shortage justifies replacement donation, pressures are exerted on both VNRD and FRD. There is no evidence of coercion of FRD. FRDs therefore meet all criteria for VNRD and are willing to become VNRD and to repeat donation. Ostracising FRD is illegitimate and damaging to the blood supply in resource poor areas. In some countries no difference is made between the two groups of donors representing similar populations asked to give blood in different circumstances.
Conclusions:
FRDs remain a critical source of volunteer, non-remunerated, blood meeting all classical criteria of VNRD that should be considered legitimate and indispensable at this point in time instead of discouraged.
Keywords: Altruism, benevolence, blood donors, blood donation, blood supply, coercion, ethics, pressure
Introduction
In recent years, several principles constituting the basis on which blood transfusion in affluent countries (volunteer only, unpaid, centralized, separate from hospitals) have been challenged in resource poor countries. In several instances, these principles supported by WHO and other international organizations were proven unsupported by evidence. Most of these principles often considered as dogmas were developed over 50 years ago in a post-World War II era by a group of European and North American pioneers of transfusion. They led the development of a code of ethics defining blood donation as an altruistic behavior, therefore, to be performed without payment to donors. In parallel, a flourish of affluent national nonprofit organizations advocating volunteer nonremunerated blood donation as the only acceptable source of blood developed. Such donor selection was advocated to prevent the social and economic selection of paid donors on the basis of both ethics and a significantly increased risk of infectious agent transmission attached to the latter.[1] However, ethics or societal context or justification of policies have been developed strictly on the basis of affluent countries, specifically Western Europe, Australia, and North America under the assumption that recommendations and conclusions were universally acceptable and therefore globally suitable. Human morals and values such as altruism vary significantly between human groups and what is good and legitimate for one group does not necessarily apply to others.[2] As widely demonstrated for the failed export of Western models of democracy into other types of societies, export of Western blood donation models, even when endorsed by international bodies such as WHO, do not fit societies with largely different economic, cultural, and moral standards. As previously pointed out, in the limited field of transfusion, globalization of Western standards can be unintentionally counterproductive.[3] Here, we re-examine the bases of blood donation models.
Methods
For the purpose of this review, systematic research has been conducted into the available literature through PubMed, as well as the reference lists of articles, that could be printed free of charge. A considerable part of the literature reviewed regarding the issues discussed in sub-Saharan Africa (SSA) was previously published by one of the authors.[4] Additional data have been focusing in central and South America, as well as Asia. The data might differ from what is presented by WHO in its regular publication mostly because its source is governments and Departments of Health, while here we focused on published literature mostly at the individual blood center level.
The place of family/replacement donors
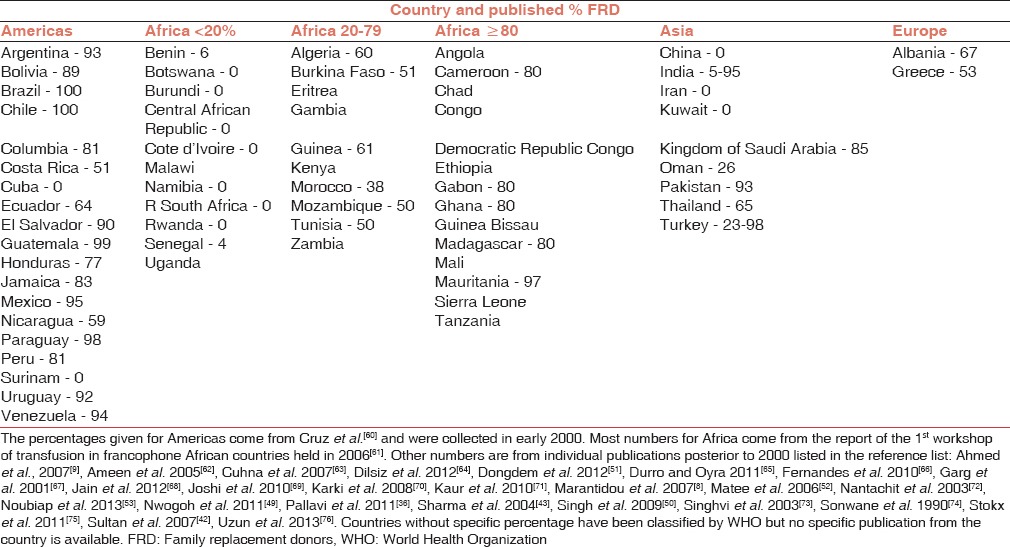
The ethical battle between nonremuneration and remuneration (compensation) was loosely supported by recent evidence of the lower level of safety.[1,5,6] This will not be the subject of the present article. In the middle of this dispute, reflected by a debate at the recent International Society of Blood Transfusion (ISBT) congress held in Amsterdam, June 2013 lie family donors (FD) and replacement donors (RD) often associated as family replacement donors (FRD) who provide the bulk of blood donations in resource poor countries for cultural and economic reasons.[7] These types of blood donors are present in all continents (mainly in Latin America, Africa, and Central Asia) and constitute approximately 20% (19 M) of global blood collections ranging between a few to 100% of the blood supply in mostly middle and low human development index countries [Table 1].[8,9] Nevertheless, they are ignored or actively discouraged by WHO and a range of governmental or nongovernmental organizations based in affluent countries.
Table 1.
Percentage of FRD in the blood supply of four continents
Developing ethics in blood transfusion
The first attempt at defining ethics in blood transfusion took place in Paris in 1978 at the time ethics in medicine and Ethics Committees started being put into place.[10] At that time the issues were: Donor safety, control of plasma derivatives, and definition of ethics rules and regulation possibly leading to legislation. Donor informed consents were drafted and preliminarily used. The use of drugs to improve the yield of cytapheresis was a particular concern. In pre-HIV Africa, hepatitis B virus (HBV) transmission was a concern although testing was considered unaffordable. “To the concept of noncommercialization is linked the principle of voluntary blood donation on the higher plane of human solidarity. This should not prevent, however, from finding means of dealing with any inconvenience and discomfort. Formulas could be conceived which would lead certainly not to remuneration, but to compensation or at least to an adequate counterpart. The elements of the latter must be found and defined in accordance, morally, with medical ethics.” The issue of the type of donor was mentioned only for cytapheresis: “Family members are excellent donors because they are highly motivated, however, most donors are unrelated donors, who are enrolled as members of the donor panel. Occasionally friends or colleagues of the recipient who are especially motivated, are used.”
Altruism being challenged
The main pillar of the case for volunteer nonremunerated donors (VNRD)-only blood donation is altruism. However, the current ISBT codes of ethics, documents released by WHO or other international bodies do not utilize the word altruism but indicate that “blood donation shall be voluntary and nonremunerated.”[11,12] This behavior has been equaled to altruism by Titmuss and his followers, as well as by the abundant literature examining the phenomenon of blood donation.[13] Altruism is defined in the Oxford English dictionary as: “Disinterested and selfless concern for the well-being of others.” This does not distinguish whether others are anonymous patients or a patient known to the donor or whether the patient is my daughter, my mother, my classmate, my co-worshipper, my work colleague or member of my community. In any case, the reality of pure altruism as conceived by the ISBT pioneers in the late 1970s and glorified by Titmuss has been challenged by experimental psychological studies mostly conducted in the USA, the UK, and Australia.[14,15,16] These investigators demonstrated experimentally that, according to the theory of planned behavior, vision of self-identity, fitting a subjective social, and moral norm feeling of being in control to decide giving or not giving blood, preventing anticipated regrets of not donating were demonstrable benefits underlying giving blood for the first time or repeating blood donation. In addition, experimental evidence was provided that “although motivations for helping can appear altruistic, those motivations may be ultimately egoistic in nature.”[17] In simple language, multiple studies consistently indicate that, “helping others is helping oneself” although “self-other overlap is also real in the genetic sense” particularly with related others such as siblings, parents, and offspring. In other words, whether others are unknown (as for VNRD) or known (as for FRD), helping oneself is a definite motivation for helping others such as by giving blood.[18] At the psychological level, the apparent difference in motivation between VNRD and FRD falls into the same general scheme of behavior. In both types of donors, the psychological frame of donation is rather benevolence (a mixture of altruism and self-interest) dominated by the benefit called “warm glow” (I donate because it makes me feel good) while evidence of empathy for or reciprocity expected from the recipient was not found.[19] The latter two potential mechanisms would most likely be demonstrable in the situation of FRD, who give blood because of empathy with the patients he/she knows and from whom some reciprocity might be at some point expected. A VNRD study conducted in Italy showed that donors who knew someone who needed transfusion or who had been transfused gave more blood units than those who did not.[20] However, no psychological studies or evaluation have been done in the “banned” FRD. Other authors[21] raised the issue of beneficence: An act that helps others. This concept appears more universal, irrespective of cultures, with the difference that it can be chosen or rejected by VNRDs but feeling more obligatory for FRDs who know the person to be helped.
Characterizing family (replacement) donors
According to the current ISBT code of ethics, FRD is nonremunerated but are assumed submitted to “coercion,” meeting the first but not the second element in the definition of what a blood donor should be. The ISBT code of ethics published in 1980 already indicated: “No pressure of any kind must be brought to bear upon the donor”[22] and as modified in 2006: “No coercion should be brought to bear upon the donor”.[12] In a recent document, advisers to WHO indicate: “In many countries, systems based on family/replacement donation often lead to coercion and place undue burden on patients’ families and friends to give blood.”[23] This statement is essentially unjustified as unsupported by evidence and ethically unsound since the blood collected under the pressure of life or death outcome is the result of blood shortage related to the incapacity of governments and blood systems to ensure adequate health care for patients. Pressure, even coercion or payment could be considered acceptable when the survival of patients depends on the collected blood.
Family donors are often labeled family/RD, which is aggregating the origin of the donors “family” (by extension other individuals connected to a patient in need of a transfusion: Friends, colleagues, acquaintances who know the patient) and the circumstances of the donation “replacement” (when a live-saving blood will not be transfused unless replaced). FDs become “replacement” donors when the blood collected is a sine qua non for the patient to be treated or when the blood center requires the family/acquaintances to manage replacing the blood transfused in order to maintain supply.[24] When the shortage is less pressing such as when the blood service has a bloodstock but insufficient supply to fully cover the clinical demand, donors are no longer taken for blood replacement but become simply contributors to the blood supply as FRD. For simplicity and to abide to a 25-year-old nomenclature we will continue calling them FRD although Family/Acquaintance donors (FAD) would be a better term to designate FD outside the replacement situation. Neither of these two types of donors is remunerated and could be considered volunteer if it was not for the considerable pressure and emotional charge put on “replacement” donors that clash with the currently adopted ISBT code of ethics. The circumstances leading to the collection of replacement blood remain frequent in SSA as described.[25,26,27] The development of VNRD motivation and retention programs promoted by governments or supported by affluent countries aid is providing some blood stock although a sizeable level of blood shortage remains in SSA countries.[28] Such shortage could be considerably relieved if FRDs were mobilized in circumstances of volunteerism, anonymity and absence of coercion. Recent data collected in Ghana clearly indicated that a minority of “family” donors were submitted to pressure from patient families but were not only willing to donate when asked but also prepared to repeat donation in conditions classically attributed to VNRD.[29] It can be argued that some FRDs might be reluctant to give blood for strangers or for patients admitted to another hospital. However, this concern has not been supported by evidence and was not mentioned by any FD in the Asenso-Mensah study.[29]
Pressure versus coercion
It would be naïve to think that VNRDs are not under pressure although of different types. In SSA where VNRDs are mostly secondary school students, peer pressure is considerable so that in some schools over 70% of students present themselves for blood donation.[30] This pressure is further increased when principals and teachers lead by giving blood themselves. Similarly, in religious communities, a pastor, a priest or an imam recommending giving blood during sermons or giving blood themselves, exert significant pressure on their flock. In Kumasi, Ghana where 20% of the population is Muslim, 30% of collected blood comes from Muslim donors encouraged by a proselytizing imam.[30] Family pressure, patient pressure, peer pressure, religious pressure, community pressure, all are pressures whether VNRD or FRD.
The Oxford English Dictionary defines pressure as: “The use of persuasion or intimidation to make someone do something; the influence or effect of someone or something” and as a verb: “Attempt to persuade or coerce (someone) into doing something.” Coercion is defined as: “The action or practice of persuading someone to do something by using force or threats.” Seen in this light, one could legitimately consider that what should be ethically reproachable is the pressure exerted by a cash payment for giving blood that unethically selects the deprived and disadvantaged populations.[31] One could consider that the television or newspaper advertisements or electronic personal messages blood centers broadcast, publish or send out to recruit donors can be classified as pressure.[32] This pressure can utilize the channel of self-satisfaction: “Feel good about yourself: Give blood” advertised by the American Red Cross or the supererogatory channel: “Do something amazing: Give blood” as advertised by the English NHSBT.[33] It is likely that these considerations explain the change of terms between the 1980 and 2006 ISBT code of ethics from “pressure” to “coercion.” Here, it could be argued that “replacement” donors are “coerced” by the risk of dying of someone they know. The pressure/coercion is then moral and emotional, not exerted by individuals, therefore not meeting the word definition.
As a result of this discussion, FRDs, as well as VNRDs, are both altruistic, and both submitted to pressures of various kinds but should not be considered as coerced. The study conducted in Kumasi, Ghana previously mentioned, clearly illustrates this point by showing that most FRDs gave blood “because they were asked” by patients or family members.[29] Interestingly, several studies looking at reasons why nondonors with the typical VNRD profile reported the same answer: “Because I was not asked or because the opportunity did not present itself” (Healy, 2000). FD are clearly nonremunerated, noncoerced and as, if not more, altruistic than VNRDs.
Should family replacement donors be banned? Is it justified?
Hence, why is it, that WHO in its recent declaration in Melbourne, Australia stigmatized FD indicating: “[experts] Believe that family replacement and paid donation can compromise the establishment of sustainable blood collection from voluntary nonremunerated blood donors.”[10] There is no evidence that this indeed takes place. In the follow-up document on self-sufficiency authored by a WHO expert group largely overlapping with the Melbourne group[23] several statements are made:
Volunteer nonremunerated donors have been demonstrated to be at lower risk of HIV and other transfusion-transmissible infections than paid and family/RD”
“Such systems (family/replacement donation) will inevitably act as a barrier to enabling national blood systems to develop appropriately alongside countries’ overall health systems.”
These documents and statements deserve scrutiny at several levels. The first statement has to do with the issue of blood safety according to the type of donors. Similar to the debate between volunteer and paid donors in affluent countries, the debate between VNRD and FRD in developing countries has been smouldering for many years during which many publications from Africa and Asia concluded that indeed VNRDs were safer, hence the WHO advisers’ statement [Table 2]. When examined closely, the evidence does not support this view often considered as dogma.[28] First, the statement associates paid and family/RD in terms of a safety risk for transfusion-transmissible infections when they should be clearly separated; the first being motivated by monetary benefits while the second by benevolence. This illegitimate association originates from previous reports that some donors presenting as FD are in fact remunerated undercover by families who cannot or are reluctant to produce a genuine FD but need replacement blood for the patient to survive or to be treated. This practice is a direct consequence of blood shortage and tends to disappear when supply improves. Paid donations are illegal in nearly all developing countries because of clear evidence of the lower level of viral safety.[9]
Table 2.
Viral screening in VNRD and FRD in countries other than sub-Saharan Africa or post 2009
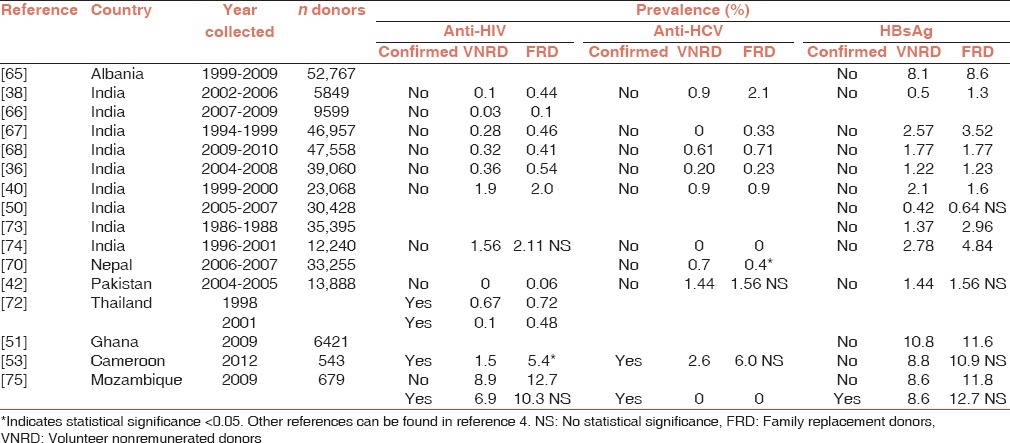
In addition, contrary to what the statement indicates, there is no supporting evidence of lower blood safety of genuine FD when comparison is conducted according to scientific epidemiological methods: Targeting first-time VNRD (the only group comparable to FRD because not biases by previously screening), using confirmed serological test results and correcting prevalence between groups for age and gender.[4] This article reviewed available literature from SSA, but many articles from Asia proved to suffer from the same shortcomings [Table 2]. In articles published in the last 10 years on viral marker comparisons between VNRD and FRD in the Indian subcontinent, none carried out assay confirmation and only one examined the impact of age in epidemiologic data[34,35,36,37,38,39,40,41,42,43] and Table 2. No studies account for the bias of repeat VNRDs in data analyses. However, two of these articles did not find differences between the two types of donors.[36,40] The study stratifying for age found no difference between VNRD and FRD for HBsAg prevalence but significantly less in VNRD for anti-HCV though without confirmation.[42]
In contrast, several studies appropriately conducted in Africa concluded at an absence of significant viral safety difference between first-time VNRD and FRD whether for HIV or HBV.[43,44,45,46,47,48] Interestingly, the article by Diarra,[45] concludes at higher safety of VNRD when biases are included in the analysis but at the same time provide a table comparing first-time VNRD and FD showing clearly no significant difference in confirmed viral marker prevalence. Other studies conducted without acknowledging the percentage of repeat VNRDs, without confirmation, without adjustment for age or gender in Africa or Asia showed an absence of significant difference in HBsAg prevalence (the only one interpretable without confirmation) between VNRD and FRD although most authors claimed higher safety of VNRDs.[42,45,49,50,51,52,53] Despite these major flaws in data interpretation (never mentioned by the authors), each article similarly concludes: “The results, which are in keeping with those of other studies, strongly indicate that RD are less suitable and that major emphasis should be made to encourage voluntary donors.”[54] It is on such scientifically unacceptable basis that the myth of VNRD being safer than FRD was built.
It is understood that in terms of risk of viral transmission, <25 years donor blood is safer and young female blood (except for HIV in SSA) would be even safer irrespective of being FRD or VNRD. The stratification of blood safety according to age or gender would certainly be based on the solid epidemiological ground but not according to being FRD or VNRD. Ultimately, there is solid evidence that repeat donation is the key to blood safety as it generally decreases confirmed viral markers by a factor of 2-4 in Zimbabwe.[55] The difficulty lies in that secondary school students who seem reluctant to repeat blood donation and in one study, the repeat rate ranged between 10% and 25% despite considerable efforts.[30] In contrast, older adult donors such as recruited in the FM radio station programs in Ghana spontaneously repeat donation at a 60-65% rate.[56] Therefore, donors at higher risk (the adults) provide the safest blood by repeating donation. This is why the blood program in Zimbabwe discards first-time donation and collects only subsequent donations.[55] Since 50-90% of VNRD donations in SSA are from first-time donors, such strategy would, therefore, be totally impractical in most developing countries, particularly in SSA.
No evidence has been provided in support of the second statement. There is evidence to the contrary that FD are essentially the same population as VNRDs but solicited for blood donation in different circumstances and constituted of donors of different age groups with little overlap.[29]
This review suggests strongly that WHO and its “expert” group continues to support their position of VNRD-only by opinions and convictions rather than by incorporating in their analyses and reasoning the multiple layers of new knowledge accumulated in the past 10 years. Dogmatic positions may have serious negative consequences for those who are not operating in affluent countries. Most developing countries that have followed the VNRD-only policy have not reached the commonly defined target of 10U/1000 inhabitants,[28,54] even when massively supported by external funding (Ala et al., 2012). Such target may have been reached if mobilizing FAD had been philosophically and pragmatically permitted adding, as experienced in Kumasi, Ghana, an extra 20-30% blood donations collected from FD without evidence of compromising blood safety permitted to reach the10U/1000 target for the past 3 years without external funding.[30] As suggested, a significant proportion of these FRDs is willing to become repeat donors when specific tools to retain them have been developed.[29,57] In Brazil, 30% of repeat donors come from the 50% of FD translated into approximately 10% of first-time FD becoming repeat donors.[58] Further to affecting the blood supply and survival of patients, being inclusive of FRDs would have decreased the cost of transfusion, made it more affordable and, therefore, more sustainable in many resource poor countries.[3,7]
Conclusions
The conclusion of this short review is that there is no ethical or safety reason to exclude FAD from participating in the blood supply. The motivations of FRDs are no more and no less altruistic than their VNRD counterpart, except that it appears stronger when someone known is the target or the trigger of blood donation.[19] These considerations totally justify the position adopted in South America, particularly in Brazil, where first-time VNRD and FRD are included in the same category of voluntary, nonremunerated donors, clearly separated from paid donors.[59] Many elements assembled in the past few years point clearly to an absence of epidemiological and social difference between first-time VNRD and FAD. Once blood collection obtained by moral coercion resulting of blood shortage as seen in several SSA countries is excluded, all ethical requirements formulated by ISBT or WHO are met by FAD. This inclusion should not be considered as going backward but as going forward in light of old data being scientifically scrutinized or of new, convincing evidence.[76]
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.van der Poel CL, Seifried E, Schaasberg WP. Paying for blood donations: Still a risk? Vox Sang. 2002;83:285–93. doi: 10.1046/j.1423-0410.2002.00239.x. [DOI] [PubMed] [Google Scholar]
- 2.Fehr E, Fischbacher U. The nature of human altruism. Nature. 2003;425:785–91. doi: 10.1038/nature02043. [DOI] [PubMed] [Google Scholar]
- 3.Ala F, Allain JP, Bates I, Boukef K, Boulton F, Brandful J, et al. External financial aid to blood transfusion services in sub-Saharan Africa: A need for reflection. PLoS Med. 2012;9:e1001309. doi: 10.1371/journal.pmed.1001309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Allain JP. Moving on from voluntary non-remunerated donors: Who is the best blood donor? Br J Haematol. 2011;154:763–9. doi: 10.1111/j.1365-2141.2011.08708.x. [DOI] [PubMed] [Google Scholar]
- 5.Eastlund T. Monetary blood donation incentives and the risk of transfusion-transmitted infection. Transfusion. 1998;38:874–82. doi: 10.1046/j.1537-2995.1998.38998409009.x. [DOI] [PubMed] [Google Scholar]
- 6.Farrugia A, Penrod J, Bult JM. Payment, compensation and replacement - The ethics and motivation of blood and plasma donation. Vox Sang. 2010;99:202–11. doi: 10.1111/j.1423-0410.2010.01360.x. [DOI] [PubMed] [Google Scholar]
- 7.Bates I, Hassall O. Should we neglect or nurture replacement blood donors in sub-Saharan Africa? Biologicals. 2010;38:65–7. doi: 10.1016/j.biologicals.2009.10.013. [DOI] [PubMed] [Google Scholar]
- 8.Marantidou O, Loukopoulou L, Zervou E, Martinis G, Egglezou A, Fountouli P, et al. Factors that motivate and hinder blood donation in Greece. Transfus Med. 2007;17:443–50. doi: 10.1111/j.1365-3148.2007.00797.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ahmed SG, Ibrahim UA, Hassan AW. Adequacy and pattern of blood donations in north-eastern Nigeria: The implications for blood safety. Ann Trop Med Parasitol. 2007;101:725–31. doi: 10.1179/136485907X241442. [DOI] [PubMed] [Google Scholar]
- 10. [Last accessed on 2013 May 22]. Available from: http://www.who.int/worldblooddonorday/MelbourneDeclarationWBDD09.pdf .
- 11.Ethics and Blood Transfusion; ISBT Symposium, Paris. 1978 Jul 23-29; [Google Scholar]
- 12. [Last accessed on 2013 May 22]. Available from: http://www.isbtweb.org/fileadmin/user_upload/ISBT_Code_of_Ethics/Code_of_ethics_new_logo_-_feb_2011.pdf .
- 13.Titmuss R. The Gift Relationship: From Human Blood to Social Policy. New York: Vintage; 1971. [Google Scholar]
- 14.Ferguson E, France CR, Abraham C, Ditto B, Sheeran P. Improving blood donor recruitment and retention: Integrating theoretical advances from social and behavioral science research agendas. Transfusion. 2007;47:1999–2010. doi: 10.1111/j.1537-2995.2007.01423.x. [DOI] [PubMed] [Google Scholar]
- 15.Masser BM, White KM, Hyde MK, Terry DJ. The psychology of blood donation: Current research and future directions. Transfus Med Rev. 2008;22:215–33. doi: 10.1016/j.tmrv.2008.02.005. [DOI] [PubMed] [Google Scholar]
- 16.Masser BM, Bednall TC, White KM, Terry D. Predicting the retention of first-time donors using an extended Theory of Planned Behavior. Transfusion. 2012;52:1303–10. doi: 10.1111/j.1537-2995.2011.03479.x. [DOI] [PubMed] [Google Scholar]
- 17.Maner JK, Luce CL, Neuberg SL, Robertson TE, Hofer B, Neuberg SL, et al. The effects of perspective taking on motivations for helping: Still no evidence for altruism. Pers Soc Psychol Bull. 2002;28:1601–10. [Google Scholar]
- 18.Cialdini RB, Brown SL, Lewis BP, Luce C, Neuberg SL. Reinterpreting the empathy-altruism relationship: When one into one equals oneness. J Pers Soc Psychol. 1997;73:481–94. [PubMed] [Google Scholar]
- 19.Ferguson E, Taylor M, Keatley D, Flynn N, Lawrence C. Blood donors’ helping behavior is driven by warm glow: More evidence for the blood donor benevolence hypothesis. Transfusion. 2012;52:2189–200. doi: 10.1111/j.1537-2995.2011.03557.x. [DOI] [PubMed] [Google Scholar]
- 20.Bani M, Strepparava MG. Motivation in Italian whole blood donors and the role of commitment. Psychol Health Med. 2011;16:641–9. doi: 10.1080/13548506.2011.569731. [DOI] [PubMed] [Google Scholar]
- 21.Snelling P. Challenging the moral status of blood donation. Health Care Ann. 2012;20:15. doi: 10.1007/s10728-012-0221-4. [DOI] [PubMed] [Google Scholar]
- 22.Transfusion Today. ISBT Newsbulletin. 1980 Dec 9;:2–9. [Google Scholar]
- 23.WHO Expert Group. Expert Consensus Statement on achieving self-sufficiency in safe blood and blood products, based on voluntary non-remunerated blood donation (VNRBD) Vox Sang. 2012;103:337–42. doi: 10.1111/j.1423-0410.2012.01630.x. [DOI] [PubMed] [Google Scholar]
- 24.Koster J, Hassall OW. Attitudes towards blood donation and transfusion in Bamenda, Republic of Cameroon. Transfus Med. 2011;21:301–7. doi: 10.1111/j.1365-3148.2011.01079.x. [DOI] [PubMed] [Google Scholar]
- 25.Mbanya DN, Takam D, Ndumbe PM. Serological findings amongst first-time blood donors in Yaoundé, Cameroon: Is safe donation a reality or a myth? Transfus Med. 2003;13:267–73. doi: 10.1046/j.1365-3148.2003.00453.x. [DOI] [PubMed] [Google Scholar]
- 26.Tagny CT, Owusu-Ofori S, Mbanya D, Deneys V. The blood donor in sub-Saharan Africa: A review. Transfus Med. 2010;20:1–10. doi: 10.1111/j.1365-3148.2009.00958.x. [DOI] [PubMed] [Google Scholar]
- 27.Kubio C, Tierney G, Quaye T, Nabilisi JW, Ziemah C, Zagbeeb SM, et al. Blood transfusion practice in a rural hospital in Northern Ghana, Damongo, West Gonja District. Transfusion. 2012;52:2161–6. doi: 10.1111/j.1537-2995.2012.03709.x. [DOI] [PubMed] [Google Scholar]
- 28.Allain JP. Volunteer safer than replacement donor blood: A myth revealed by evidence. Vox Sang ISBT Sci Ser. 2010;5:169–75. [Google Scholar]
- 29.Asenso-Mensah K, Achina G, Appiah R, Owusu-Ofori S, Allain JP. Can family or replacement blood donors become regular volunteer donors? Transfusion. 2014;54:797–804. doi: 10.1111/trf.12216. [DOI] [PubMed] [Google Scholar]
- 30.Owusu-Ofori S, Asenso-Mensah K, Boateng P, Sarkodie F, Allain JP. Fostering repeat donations in Ghana. Biologicals. 2010;38:47–52. doi: 10.1016/j.biologicals.2009.10.021. [DOI] [PubMed] [Google Scholar]
- 31.Petrini C. Production of plasma-derived medicinal products: Ethical implications for blood donation and donors. Blood Transfus. 2014;12(Suppl 1):s389–94. doi: 10.2450/2013.0167-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.France CR, France JL, Wissel ME, Kowalsky JM, Bolinger EM, Huckins JL. Enhancing blood donation intentions using multimedia donor education materials. Transfusion. 2011;51:1796–801. doi: 10.1111/j.1537-2995.2010.03033.x. [DOI] [PubMed] [Google Scholar]
- 33.Healy K. Embedded altruism: Blood collection regimes and European Union's donor population. Am J Sociol. 2000;105:1633–57. [Google Scholar]
- 34.Sidhu M, Kotwal U, Kapoor R, Raina T. Seroprevalence of human immunodeficiency virus, hepatitis B virus and hepatits C virus in blood donors of Jammu province: A tertiary care centre experience. Asian J Transfus Sci. 2013;7:162–3. doi: 10.4103/0973-6247.115601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jain R, Gupta G. Family/friend donors are not true voluntary donors. Asian J Transfus Sci. 2012;6:29–31. doi: 10.4103/0973-6247.95047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pallavi P, Ganesh CK, Jayashree K, Manjunath GV. Seroprevalence and trends in transfusion transmitted infections among blood donors in a university hospital blood bank: A 5 year study. Indian J Hematol Blood Transfus. 2011;27:1–6. doi: 10.1007/s12288-010-0047-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Meena M, Jindal T, Hazarika A. Prevalence of hepatitis B virus and hepatitis C virus among blood donors at a tertiary care hospital in India: A five-year study. Transfusion. 2011;51:198–202. doi: 10.1111/j.1537-2995.2010.02801.x. [DOI] [PubMed] [Google Scholar]
- 38.Arora D, Arora B, Khetarpal A. Seroprevalence of HIV, HBV, HCV and syphilis in blood donors in Southern Haryana. Indian J Pathol Microbiol. 2010;53:308–9. doi: 10.4103/0377-4929.64295. [DOI] [PubMed] [Google Scholar]
- 39.Panda M, Kar K. HIV, hepatitis B and C infection status of the blood donors in a blood bank of a tertiary health care centre of Orissa. Indian J Public Health. 2008;52:43–4. [PubMed] [Google Scholar]
- 40.Shinde SV, Puranik GV. A study-screening of blood donors for blood transmissible diseases. Indian J Hematol Blood Transfus. 2007;23:99–103. doi: 10.1007/s12288-008-0006-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pahuja S, Sharma M, Baitha B, Jain M. Prevalence and trends of markers of hepatitis C virus, hepatitis B virus and human immunodeficiency virus in Delhi blood donors: A hospital based study. Jpn J Infect Dis. 2007;60:389–91. [PubMed] [Google Scholar]
- 42.Sultan F, Mehmood T, Mahmood MT. Infectious pathogens in volunteer and replacement blood donors in Pakistan: A ten-year experience. Int J Infect Dis. 2007;11:407–12. doi: 10.1016/j.ijid.2006.10.004. [DOI] [PubMed] [Google Scholar]
- 43.Sharma RR, Cheema R, Vajpayee M, Rao U, Kumar S, Marwaha N, et al. Prevalence of markers of transfusion transmissible diseases in voluntary and replacement blood donors. Natl Med J India. 2004;17:19–21. [PubMed] [Google Scholar]
- 44.Allain JP, Sarkodie F, Asenso-Mensah K, Owusu-Ofori S. Relative safety of first-time volunteer and replacement donors in West Africa. Transfusion. 2010;50:340–3. doi: 10.1111/j.1537-2995.2009.02444.x. [DOI] [PubMed] [Google Scholar]
- 45.Diarra A, Kouriba B, Baby M, Murphy E, Lefrere JJ. HIV, HCV, HBV and syphilis rate of positive donations among blood donations in Mali: Lower rates among volunteer blood donors. Transfus Clin Biol. 2009;16:444–7. doi: 10.1016/j.tracli.2009.09.004. [DOI] [PubMed] [Google Scholar]
- 46.Loua A, Nze Nkoure G. Relative safety of first-time volunteer and replacement donors in Guinea. Transfusion. 2010;50:1850–1. doi: 10.1111/j.1537-2995.2010.02718.x. [DOI] [PubMed] [Google Scholar]
- 47.Mbanya DN, Feunou F, Tayou TC. Volunteer or family/replacement donations: Are the tides changing? Transfusion. 2010;50:1849–50. doi: 10.1111/j.1537-2995.2010.02656.x. [DOI] [PubMed] [Google Scholar]
- 48.Tazi-Mokha A, Soulaymani A, Mokhtari A, Alami R. Blood donation in Morocco: A 20-year retrospective study of blood collection in the Rabat blood centre. Transfus Med. 2012;22:173–80. doi: 10.1111/j.1365-3148.2012.01138.x. [DOI] [PubMed] [Google Scholar]
- 49.Nwogoh B, Ikpomwen OD, Isoa EM. Donor blood procurement and the risk of transfusion transmissible viral infections in a tertiary health facility in South-South Nigeria. Niger Med J. 2011;52:227–9. doi: 10.4103/0300-1652.93793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Singh K, Bhat S, Shastry S. Trend in seroprevalence of Hepatitis B virus infection among blood donors of coastal Karnataka, India. J Infect Dev Ctries. 2009;3:376–9. doi: 10.3855/jidc.246. [DOI] [PubMed] [Google Scholar]
- 51.Dongdem JT, Kampo S, Soyiri IN, Asebga PN, Ziem JB, Sagoe K. Prevalence of hepatitis B virus infection among blood donors at the tamale teaching Hospital, Ghana (2009) BMC Res Notes. 2012;5:115. doi: 10.1186/1756-0500-5-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Matee MI, Magesa PM, Lyamuya EF. Seroprevalence of human immunodeficiency virus, hepatitis B and C viruses and syphilis infections among blood donors at the Muhimbili National Hospital in Dar es Salaam, Tanzania. BMC Public Health. 2006;6:21. doi: 10.1186/1471-2458-6-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Noubiap JJ, Joko WY, Nansseu JR, Tene UG, Siaka C. Sero-epidemiology of human immunodeficiency virus, hepatitis B and C viruses, and syphilis infections among first-time blood donors in Edéa, Cameroon. Int J Infect Dis. 2013;17:e832–7. doi: 10.1016/j.ijid.2012.12.007. [DOI] [PubMed] [Google Scholar]
- 54.Dahourou H, Tapko JB, Kienou K, Nebie K, Sanou M. Recruitment of blood donors in Burkina Faso: How to avoid donations from family members? Biologicals. 2010;38:39–42. doi: 10.1016/j.biologicals.2009.10.017. [DOI] [PubMed] [Google Scholar]
- 55.Mapako T, Mvere DA, Chitiyo ME, Rusakaniko S, Postma MJ, van Hulst M. Human immunodeficiency virus prevalence, incidence, and residual transmission risk in first-time and repeat blood donations in Zimbabwe: Implications on blood safety. Transfusion. 2013;53:2413–21. doi: 10.1111/trf.12311. [DOI] [PubMed] [Google Scholar]
- 56.Allain JP, Sarkodie F, Boateng P, Asenso K, Kyeremateng E, Owusu-Ofori S. A pool of repeat blood donors can be generated with little expense to the blood center in Sub-Saharan Africa. Transfusion. 2008;48:735–41. doi: 10.1111/j.1537-2995.2007.01599.x. [DOI] [PubMed] [Google Scholar]
- 57.Ashraf TM, Smit Sibinga CT. Blood donation and donor motivation in Oman. Transfusion. 2012;52(Suppl):244A–5. [Google Scholar]
- 58.Carneiro-Proietti AB, Sabino EC, Sampaio D, Proietti FA, Gonçalez TT, Oliveira CD, et al. Demographic profile of blood donors at three major Brazilian blood centers: Results from the International REDS-II study, 2007 to 2008. Transfusion. 2010;50:918–25. doi: 10.1111/j.1537-2995.2009.02529.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Barreto CC, Sabino EC, Gonçalez TT, Laycock ME, Pappalardo BL, Salles NA, et al. Prevalence, incidence, and residual risk of human immunodeficiency virus among community and replacement first-time blood donors in São Paulo, Brazil. Transfusion. 2005;45:1709–14. doi: 10.1111/j.1537-2995.2005.00575.x. [DOI] [PubMed] [Google Scholar]
- 60.Cruz JR, Pérez-Rosales MD. Availability, safety, and quality of blood for transfusion in the Americas. Rev Panam Salud Publica. 2003;13:103–10. doi: 10.1590/s1020-49892003000200010. [DOI] [PubMed] [Google Scholar]
- 61.First workshop on blood transfusion organization in francophone African countries (Premier colloque sur l’organisation de la Transfusion Sanguine dans les pays d’Afrique francophone) Alger. 2006 [Google Scholar]
- 62.Ameen R, Sanad N, Al-Shemmari S, Siddique I, Chowdhury RI, Al-Hamdan S, et al. Prevalence of viral markers among first-time Arab blood donors in Kuwait. Transfusion. 2005;45:1973–80. doi: 10.1111/j.1537-2995.2005.00635.x. [DOI] [PubMed] [Google Scholar]
- 63.Cunha L, Plouzeau C, Ingrand P, Gudo JP, Ingrand I, Mondlane J, et al. Use of replacement blood donors to study the epidemiology of major blood-borne viruses in the general population of Maputo, Mozambique. J Med Virol. 2007;79:1832–40. doi: 10.1002/jmv.21010. [DOI] [PubMed] [Google Scholar]
- 64.Dilsiz G, Yenicesu I, Belen FB, Celik B, Ozturk G. Trends in hepatitis B and hepatitis C virus seropositivity among blood donors over 15 years screened in the blood bank of a university hospital. Transfus Apher Sci. 2012;47:95–100. doi: 10.1016/j.transci.2012.05.008. [DOI] [PubMed] [Google Scholar]
- 65.Durro V, Qyra S. Trends in prevalence of hepatitis B virus infection among Albanian blood donors, 1999-2009. Virol J. 2011;8:96. doi: 10.1186/1743-422X-8-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Fernandes H, D’souza PF, D’souza PM. Prevalence of transfusion transmitted infections in voluntary and replacement donors. Indian J Hematol Blood Transfus. 2010;26:89–91. doi: 10.1007/s12288-010-0044-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Garg S, Mathur DR, Garg DK. Comparison of seropositivity of HIV, HBV, HCV and syphilis in replacement and voluntary blood donors in western India. Indian J Pathol Microbiol. 2001;44:409–12. [PubMed] [Google Scholar]
- 68.Jain R, Aggarwal P, Gupta GN. Need for nucleic acid testing in countries with high prevalence of transfusion-transmitted infections. ISRN Hematol. 2012;2012:718671. doi: 10.5402/2012/718671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Joshi SR, Shah Al-Bulushi SN, Ashraf T. Development of blood transfusion service in Sultanate of Oman. Asian J Transfus Sci. 2010;4:34–40. doi: 10.4103/0973-6247.59390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Karki S, Ghimire P, Tiwari BR, Rajkarnikar M. Seroprevalence of anti HCV antibodies among blood donors in Kathmandu valley, Nepal. Kathmandu Univ Med J (KUMJ) 2008;6:491–6. doi: 10.3126/kumj.v6i4.1741. [DOI] [PubMed] [Google Scholar]
- 71.Kaur G, Basu S, Kaur R, Kaur P, Garg S. Patterns of infections among blood donors in a tertiary care centre: A retrospective study. Natl Med J India. 2010;23:147–9. [PubMed] [Google Scholar]
- 72.Nantachit N, Robison V, Wongthanee A, Kamtorn N, Suriyanon V, Nelson KE. Temporal trends in the prevalence of HIV and other transfusion-transmissible infections among blood donors in northern Thailand, 1990 through 2001. Transfusion. 2003;43:730–5. doi: 10.1046/j.1537-2995.2003.00395.x. [DOI] [PubMed] [Google Scholar]
- 73.Singhvi A, Pulimood RB, John TJ. The prevalence of markers for hepatitis B and human immunodeficiency viruses, malarial parasites and microfilaria in blood donors in a large hospital in south India. Indian J Med Sci. 2003;57:405–7. [PubMed] [Google Scholar]
- 74.Sonwane BR, Birare SD, Kulkarni PV. Prevalence of seroreactivity among blood donors in rural population. J Trop Med Hyg. 1990;93:178–82. [PubMed] [Google Scholar]
- 75.Stokx J, Gillet P, De Weggheleire A, Casas EC, Maendaenda R, Beulane AJ, et al. Seroprevalence of transfusion-transmissible infections and evaluation of the pre-donation screening performance at the Provincial Hospital of Tete, Mozambique. BMC Infect Dis. 2011;11:141. doi: 10.1186/1471-2334-11-141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Uzun B, Güngör S, Demirci M. Seroprevalence of transfusion transmissible infections among blood donors in western part of Turkey: A six-year study. Transfus Apher Sci. 2013;49:511–5. doi: 10.1016/j.transci.2013.02.039. [DOI] [PubMed] [Google Scholar]


