Abstract
Objectives:
Cross sectional studies have reported a tremendous amount of stress in caregivers of patients with Alzheimer's disease (AD) and Mild Cognitive Impairment (MCI). The present study aimed at evaluating the perceived stress in caregivers of patients with AD and MCI compared to controls.
Materials and Methods:
Caregivers of patients diagnosed with Alzheimer's disease/Mild Cognitive Impairment were recruited at the Memory Clinic of Neurology Department of a Tertiary Care Hospital in Northern India. The controls included caregivers of patients with chronic medical and psychiatric disorders. Caregivers were interviewed using Perceived Stress Scale (PSS) and the patients were assessed using The Blessed Activity of Daily Living (ADL), Mini Mental State Examination (MMSE) and Clinical Dementia Rating scale. The perceived stress of caregivers was compared amongst both groups and correlated with the severity of illness and activities of daily living of the patients.
Results:
Caregivers of a total of 31 patients of AD/MCI (Males = 24, Females = 7), and 30 controls (Males = 18, Females = 12) were interviewed. PSS Score was 23.29 ± 7.17 in cases and 7.5 ± 3.12 in controls. ADL Score was 7.97±5.53 in cases and 0.00 in controls. There was a significant difference between the PSS and ADL scores between those with AD and controls (P < 0.0001). Caregivers of patients with MCI had lower PSS scores compared to AD caregivers but significantly higher scores compared to caregivers of other chronic disorders. Similarly, correlation between Perceived Stress and ADL was significant (P < 0.001).
Conclusions:
Present study shows that caregivers of patients with AD/MCI have a high perceived stress compared to caregivers of patients with other chronic illness.
Keywords: Alzheimer's disease, caregiver stress, mild cognitive impairment
Introduction
Caregiving and Nursing are stressful jobs.[1] There are two main types of caregivers in India. First category consists of professionally trained staffs that include nurses, trained attendants and health workers. They are few in numbers considering a large population base. Second category is of those who impart care giving on regular basis (i.e. family members and relatives) and are closer to the patient. Spouses, sons, daughters, daughter in laws and parents are the usual caregivers (informal caregivers). Caregiver burden is influenced by patient's behavioral and cognitive status, hours involved in care, stress, social isolation, gender, relationship to the patient, availability of support resources, and caregiver characteristics.[1,2]
There are several predictors of the caregiver stress in patients with Alzheimer's disease (AD) and Mild Cognitive Impairment (MCI).[3] Among Indian patients, it has been shown that caregiver burden is more common in those cases with behavioral and psychological symptoms of dementias (BPSD). Patients at times become so burdened by the caregiver stress that they resort to drugs of alternative system of medicine too apart from the mainstream drugs as well.[4] A recent study evaluating impact of caring for a person with dementia supported the need for scaling up caregiver support, education and training.[5] Furthermore, there are suggestions that interventions aimed at managing caregiver stress could be useful.[6] Several deficiencies in dementia care exist in India. Therefore, there is a need felt for educating and supporting caregivers of dementia patients.[7]
Perceived stress experienced by caregivers of AD patients puts significant strain on them. There is a significant conversion of MCI to AD in due course of time. Though clinically and pathophysiologically heterogeneous, we took it as a unitary group, because common hallmark of both of them is impaired cognition. So that is why, both categories have been included in the current study. It has often been said that India has joint family norms that acts as a shock absorber in stressful situations and hence caregiver stress could potentially be less. Caregiver burden posed by AD/MCI in Indian patients has been studied. However, there is no study regarding the perceived stress experienced by AD/MCI caregivers and its correlation with the impairment in ADL in Indian subjects. Also, some of the studies have reported high burden on caregivers of patients with chronic medical and psychiatric illnesses. We could not find any Indian study comparing the caregiver's perceived stress among these disorders and AD/MCI. Therefore, the present study was aimed at evaluating if the perceived stress felt by AD caregivers was significantly different compared to the perceived stress in caregivers of patients with other major medical and psychiatric disorders. Additionally, we were interested in knowing the important predictors of caregiver stress in Indian population.
Materials and Methods
The study was conducted in the Out Patient Department (OPD) of the Neurology department, Psychiatry department and Medicine department of a tertiary care hospital in Northern India. The study was approved by the Institutional Ethics Committee.
Patients attending Memory Clinic in Department of Neurology were assessed for AD/MCI. Subjects were selected randomly from the General Outpatient Department. After initial General Physical, Neurological and Neuropsychological Examination, patients were evaluated using the National Institute of Neurological and Communicative Disorders and Stroke and the Related Disorders Association (NINCDS–ADRDA) criteria for the diagnosis of AD.[8] Clinical Dementia Rating (CDR) scale was used for the diagnosis of MCI (0.5 score on CDR).[9] Mini Mental State Examination (MMSE) was done for assessing severity of dementias.[10] The primary caregivers of those with a diagnosis AD/MCI were interviewed using Perceived Stress Scale (PSS)[11] and the patients were assessed on shorter version of Blessed Activity of Daily Living Scale.[12] An attempt was made to know association of caregiver stress (PSS) with severity of dementia and ADL scores.
The Perceived Stress Scale is the most widely used psychological instrument for measuring the subjective perception of stress. It measures the degree to which situations in one's life are appraised as stressful.[11] The questions are of a general nature and are relatively free of content specific to any sub-population group. Hence, it is appropriate for use in caregivers. The questions in the PSS are 10 in number, Likert type and ask about feelings and thoughts during the last month. The PSS has a high internal consistency of 0.85 (Cronbach co-efficient) and test-retest reliability.[13] The Blessed ADL Scale was described by Blessed, Tomlinson and Roth in 1965 and consisted of 11 questions.[12] However, the modified version of the scale consisting of 13 questions was described by Erkinjuntti et al.[14] It is divided into two parts: In the first part, 10 activities are covered, the scores are rated as 0, 0.5 and 1 and in the second part there are four possible points to select, from 0 to 4. This scale is helpful in the evaluation of the degree of disability and in the planning of social support.
The controls were selected randomly from the Department of Psychiatry and Medicine. The inclusion criteria for controls included caregivers of patients with chronic medical or psychiatric disorders for at least past 1 year, absence of any other co-morbid medical condition and cognitive impairment, staying in contact with the patient for most period of illness and willing to give informed written consent. The control caregivers were also evaluated on PSS and control patients on ADL scale, and the respective scores were compared with caregivers of AD/MCI. Appropriate parametric and non-parametric tests were used for analysis, which have been described further. The statistical analysis was done using the SPSS 17. A P-value of less than 0.05 was considered significant, considering the power of study to be 90%.
Results
Caregivers of a total of 31 patients with a diagnosis of Alzheimer's disease (n = 24) and Mild Cognitive Impairment (n = 7) were recruited. All 7 MCI cases were males. The mean age of patients was 72.35 ± 9.85 years and the mean duration of illness was 4.5 ± 0.7 years. There were a total of 20 male and 11 female caregivers. The mean age of caregivers of patients with AD/MCI was 69 ± 11.86 years [Table 1].
Table 1.
Comparison of different parameters amongst the two groups
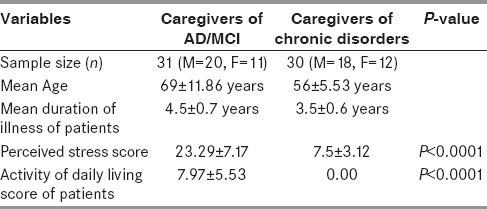
A total of 30 patients in the controls were taken. The controls were the caregivers of patients with Osteoporosis (n = 12), Diabetes and Hypertension (n = 6), and Psychiatric illnesses which included anxiety disorders, depression and psychosomatic disorders (n = 10). There were a total of 18 male and 12 female caregivers. Mean duration of illness in case of controls was 3.5 ± 0.6 years. The mean age of control caregivers was 56 ± 5.53 years [Table 1].
The mean Perceived Stress Score was 23.29 ± 7.17 in caregivers of patients with AD/MCI while the mean ADL Score of patients with AD/MCI was 7.97 ± 5.53. Similarly, the mean PSS in caregivers of controls was 7.5 ± 3.12 while the Activity of Daily Living Score was = 0.00 in the control patients [Table 1]. There was a significant difference in the PSS and ADL scores between AD/MCI group compared with controls (P = <0.0001) using the paired t-test. Perceived stress in MCI group was significantly less compared to those with AD but more compared to other chronic illnesses (P = <0.001).
In AD/MCI group, correlation between MMSE and PSS (females) was significant (Coefficient of determination = 0.3204). Likewise correlation between MMSE and PSS (Both sexes) was significant too (Coefficient of determination = 0.2197). Similarly, correlation between Perceived Stress and Activity of Daily Living was significant (Correlation Coefficient = 0.2437). There was a modest but significant correlation between these two signifying when perceived stress is high, then activity of daily living are likely to be impaired [Figure 1]. Correlation between MMSE scores and Activity of Daily Living Score was highly significant (Coefficient of determination = 0.5095) signifying that impaired cognition affects the activities of daily living. The PSS score and hence, the burden and stress of care-giving correlated with caregivers of male patients, more duration of illness, increasing age of patients and impaired cognition of patients (P < 0.01).
Figure 1.
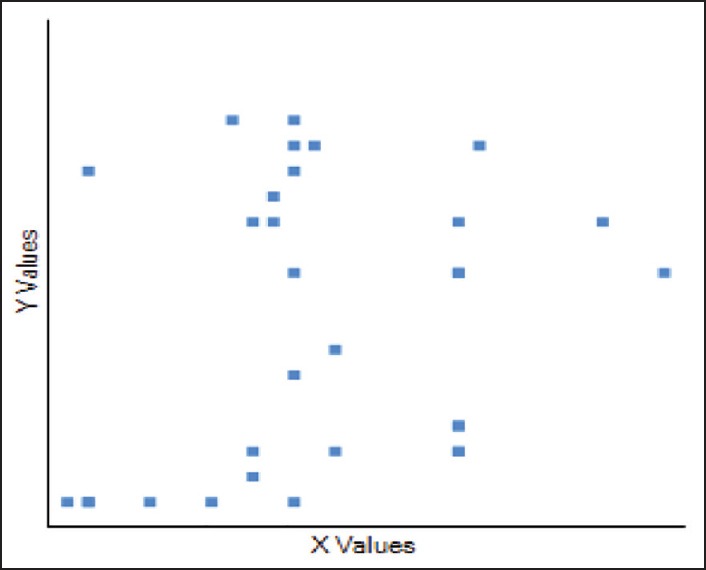
Correlation between perceived stress and activity of daily living-correlation coefficient = 0.2437 (P = <0.001). X-axis denotes the perceived stress, while y-axis denotes
Discussion
Caring and nursing are stressful jobs. There are varieties of stresses, strains, psychological and physical consequences of care giving. The job is demanding and hence a significant amount of research effort has been directed towards this. In India, the little work has been done in this area, its determinants, predictors and methods to alleviate the same, inspite that India has a rapidly growing elderly population.
The purpose of this study design was to assess the perceived stress in caregivers of patients with AD/MCI, to compare it with stress in caregivers of patients with other chronic disorders and to evaluate the statistical difference between scores of two conditions. In the present study, both differed significantly in terms of the stress perceived by the caregivers (P = <0.0001). AD/MCI posed a significantly higher stress to caregivers as compared to caregivers of patients with other chronic illnesses. The perceived stress in MCI group was significantly less compared to those with AD, showing that patients with MCI are not as impaired and dependent on caregivers, as are the patients with AD. However, it was statistically significant and more compared to the caregivers of other chronic illnesses (P = < 0.001). This might suggest that patients with MCI have difficulties in activities which involve caregiver involvement such as self care, remembering and taking medications which puts burden upon the caregivers.
The impact of caregiver stress on caregiver health has been studied. Emotional exhaustion, anxiety, depression are some of the psychiatric symptoms felt by caregivers.[7] Caregiver stress puts so much of strains on the caregivers, that it may even increase the risk of heart disease.[15] It may also impair quality of life.[16] Social support has been shown to be protective.[17] However, this was beyond the scope of the present study. Experience and research has shown that mental anguish and physical symptoms may contribute to caregiver dissatisfaction.[18,19,20,21] The caregivers use prescription medications and healthcare services more frequently than comparable non-caregiver population.[22,23,24] Primary caregivers also face a risk of an increasing mortality rate.[25]
Caregivers face a variety of challenges when a loved one develops Alzheimer's disease or any other chronic progressive disease. Adjusting to the problems the patients face and providing support is a big task.[26,27] As the disease progresses, the caregivers may be called upon to learn and adapt to changes in the patient and develop new skills to shoulder an increasing amount of responsibility. Also, the lack of appreciation for the efforts in caring for a person who is physically present but mentally and psychologically absent may lead to depression, anxiety, and other health problems.[22,28]
As found in the study, the impairment in activities of daily living correlates with perceived stress of caregivers. Many studies have supported the notion,[28,29] although some have disagreed.[2,30] This may be explained by a higher level of caregiver engagement following a decline in ADL, which might result in lowering of health related quality of life. Authors have suggested that decrease in ADL may be a reflection of disease progression. Hence, some studies suggest that moderate to severe disability among the patients is related to high caregiver burden.[28,29] Some earlier studies have also examined the predictors of PSS. Caregiver stress has been found to be more in caregivers who are advanced in age,[24,31] women[30,32,33] and those who reside with the patients than caregivers who are young, male and live apart from the patients.[29] Most of these findings are similar to present study. However, our study also signifies the importance of cognition of patients and the duration of illness as the contributing factors.
Dementia is a growing public health concern in India with rapid increase in ageing population.[34] No Indian study has evaluated and compared caregiver stress in dementia with other caregiver groups. However, some international studies have found more stress in dementia caregivers.[33,35] We also found the same results. In the present study, the overall PSS scores were also high. This was surprising, as traditionally, India is a joint family system driven society compared to nuclear families in western countries. So, it is expected that caregiving burden would be shared among most of the family members. However, that was not the case in our study.
Attempts are being done to reduce caregiver perceived stress. A number of interventions like yoga,[36,37] meditation[38] and web based interventions[39] have been found to be useful. All three of these non pharmacological options seem tempting as these could prove to be cost effective in a developing nation like India where financial burden upon patients’ caregivers could be very high. Unfortunately, there are no caregiver support programs in major medical institutions of India. There is perhaps an unmet need of identifying uniform and cost effective interventions that could be used for dementia caregivers. That may aid in better care giving. Similar care giving interventions in some other countries have been successful.
Major strengths of the current study lies in the fact that it has compared the stress of caregivers in AD/MCI with other chronic disorders, which helps to determine the grading of perceived stress. This study is the first one in India to do so. Also, the PSS scores were correlated with different variables to assess the predictors of caregiver stress in Indian population. The sample of patients were recruited from Delhi, which being the capital and a metropolitan town, could be considered to have a representative sample as people from all walks of life are likely to be included. However, modest sample size of the study is the major limitation. We have not taken into account the socio-economic details of patients into account while considering the perceived stress. For example, in a patient below poverty line with osteoporosis and fracture; stress could potentially be very high. Moreover, the severity of chronic medical/psychiatric disorders was not taken into account and this could have potentially affected the PSS score. Therefore, systematic studies need to be undertaken, especially in India, to assess for caregiver burden in dementia and other chronic illnesses and for formulating adequate management strategies for caregivers as well.
Conclusions
Caregiving is a tedious and thankless job, which may lead to many psychological and physical problems. Perceived stress experienced by caregivers of patients with AD/MCI is high. The findings suggest that caregiving for patients with dementia is much more stressful than caregiving in other chronic disorders. This may be attributed to increased dependence of AD/MCI patients on caregivers for activities of daily living, more so in later stages and due to increasing severity of problems despite management. Hence, the nursing interventions and management should be targeted towards both the patients as well as the caregivers to improve the functional abilities of individuals with dementia and for the wellbeing of caregivers. Appropriate support programs and management strategies should be devised for caregivers in India, considering the increased life expectancy of population (34) and the burden of dementia.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Sansoni J, Anderson KH, Varona LM, Varela G. Caregivers of Alzheimer's patients and factors influencing institutionalization of loved ones: Some considerations on existing literature. Ann Ig. 2013;25:235–46. doi: 10.7416/ai.2013.1926. [DOI] [PubMed] [Google Scholar]
- 2.Clyburn LD, Stones MJ, Hadjistavropoulos T, Tuokko H. Predicting caregiver burden and depression in Alzheimer's disease. J Gerontol B Psychol Sci Soc Sci. 2000;55:S2–13. doi: 10.1093/geronb/55.1.s2. [DOI] [PubMed] [Google Scholar]
- 3.Dhikav V, Anand KS. Caregiver burden of behavioral and psychological symptoms of dementia among Indian patients with Alzheimer's disease. Int Psychogeriatr. 2012;24:1531–2. doi: 10.1017/S1041610212000439. [DOI] [PubMed] [Google Scholar]
- 4.Dhikav V, Anand KS. Complementary and alternative medicine usage among Alzheimer's disease patients. Int Psychogeriatr. 2012;24:1361–2. doi: 10.1017/S1041610212000427. [DOI] [PubMed] [Google Scholar]
- 5.Prince M, Brodaty H, Uwakwe R, Acosta D, Ferri CP, Guerra M, et al. Strain and its correlates among carers of people with dementia in low-income and middle-income countries. A 10/66 Dementia Research Group population-based survey. Int J Geriatr Psychiatry. 2012;27:670–82. doi: 10.1002/gps.2727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gavrilova SI, Ferri CP, Mikhaylova N, Sokolova O, Banerjee S, Prince M. Helping carers to care – the 10/66 Dementia Research Group's randomized control trial of a caregiver intervention in Russia. Int J Geriatr Psychiatry. 2009;24:347–54. doi: 10.1002/gps.2126. [DOI] [PubMed] [Google Scholar]
- 7.Yilmaz A, Turan E, Gundogar D. Predictors of burnout in the family caregivers of Alzheimer's disease: Evidence from Turkey. Australas J Ageing. 2009;28:16–21. doi: 10.1111/j.1741-6612.2008.00319.x. [DOI] [PubMed] [Google Scholar]
- 8.McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM. Clinical diagnosis of Alzheimer's disease: Report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer's Disease. Neurology. 1984;34:939–44. doi: 10.1212/wnl.34.7.939. [DOI] [PubMed] [Google Scholar]
- 9.Morris JC. The Clinical Dementia Rating (CDR): Current version and scoring rules. Neurology. 1993;43:2412–4. doi: 10.1212/wnl.43.11.2412-a. [DOI] [PubMed] [Google Scholar]
- 10.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–98. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 11.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:386–96. [PubMed] [Google Scholar]
- 12.Blessed G, Tomlinson BE, Roth M. The association between quantitative measures of dementia and of senile change in the cerebral grey matter of elderly subjects. Br J Psychiatry. 1968;114:797–811. doi: 10.1192/bjp.114.512.797. [DOI] [PubMed] [Google Scholar]
- 13.Sreeramareddy CT, Shankar PR, Binu VS, Mukhopadhyay C, Ray B, Menezes RG. Psychological morbidity, sources of stress and coping strategies among undergraduate medical students of Nepal. BMC Med Educ. 2007;7:26. doi: 10.1186/1472-6920-7-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Erkinjuntti T, Hokkanen L, Sulkava R, Palo J. The Blessed dementia scale as a screening test for dementia. Int J Geriatr Psychiatry. 1988;3:267–73. [Google Scholar]
- 15.Mausbach BT, Chattillion E, Roepke SK, Ziegler MG, Milic M, von Känel R, et al. A longitudinal analysis of the relations among stress, depressive symptoms, leisure satisfaction, and endothelial function in caregivers. Health Psychol. 2012;31:433–40. doi: 10.1037/a0027783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Scholzel-Dorenbos CJ, Draskovic I, Vernooij-Dassen MJ, Olde Rikkert MG. Quality of life and burden of spouses of Alzheimer disease patients. Alzheimer Dis Assoc Disord. 2009;23:171–7. doi: 10.1097/wad.0b013e318190a260. [DOI] [PubMed] [Google Scholar]
- 17.Wilks SE, Croom B. Perceived stress and resilience in Alzheimer's disease caregivers: Testing moderation and mediation models of social support. Aging Ment Health. 2008;12:357–65. doi: 10.1080/13607860801933323. [DOI] [PubMed] [Google Scholar]
- 18.Taemeeyapradit U, Udomittipong D, Tepparak N. Characteristics of behavioral and psychological symptoms of dementia, severity and levels of distress on caregivers. J Med Assoc Thai. 2014;97:423–30. [PubMed] [Google Scholar]
- 19.Zvěřová M. Frequency of some psychosomatic symptoms in informal caregivers of Alzheimer's disease individuals. Prague's experience. Neuro Endocrinol Lett. 2012;33:565–7. [PubMed] [Google Scholar]
- 20.Cheng ST, Lau RW, Mak EP, Ng NS, Lam LC, Fung HH, et al. A benefit-finding intervention for family caregivers of persons with Alzheimer disease: Study protocol of a randomized controlled trial. Trials. 2012;13:98. doi: 10.1186/1745-6215-13-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vitaliano PP, Russo J, Scanlan JM, Greeno CG. Weight changes in caregivers of Alzheimer's care recipients: Psychobehavioral predictors. Psychol Aging. 1996;11:155–63. doi: 10.1037//0882-7974.11.1.155. [DOI] [PubMed] [Google Scholar]
- 22.Brodaty H, Green A. Defining the role of the caregiver in Alzheimer's disease treatment. Drugs and Aging. 2002;19:891–8. doi: 10.2165/00002512-200219120-00001. [DOI] [PubMed] [Google Scholar]
- 23.Schulz R, Martire LM. Family caregiving of persons with dementia: Prevalence, health effects, and support strategies. Am J Geriatr Psychiatry. 2004;12:240–9. [PubMed] [Google Scholar]
- 24.Serrano-Aguilar PG, Lopez-Bastida J, Yanes-Lopez V. Impact on health-related quality of life and perceived burden of informal caregivers of individuals with Alzheimer's disease. Neuroepidemiology. 2006;27:136–42. doi: 10.1159/000095760. [DOI] [PubMed] [Google Scholar]
- 25.Schulz R, Beach SR. Caregiving as a risk factor for mortality: The Caregiver Health Effects Study. JAMA. 1999;282:2215–9. doi: 10.1001/jama.282.23.2215. [DOI] [PubMed] [Google Scholar]
- 26.Carretero S, Garcés J, Ródenas F, Sanjosé V. The informal caregiver's burden of dependent people: Theory and empirical review. Arch Gerontol Geriatr. 2009;49:74–9. doi: 10.1016/j.archger.2008.05.004. [DOI] [PubMed] [Google Scholar]
- 27.Etters L, Goodall D, Harrison BE. Caregiver burden among dementia patient caregivers: A review of the literature. J Am Acad Nurse Pract. 2008;20:423–8. doi: 10.1111/j.1745-7599.2008.00342.x. [DOI] [PubMed] [Google Scholar]
- 28.Molyneux GJ, McCarthy GM, McEniff S, Cryan M, Conroy RM. Prevalence and predictors of carer burden and depression in carers of patients referred to an old age psychiatric service. Int Psychogeriatr. 2008;20:1193–202. doi: 10.1017/S1041610208007515. [DOI] [PubMed] [Google Scholar]
- 29.Conde-Sala JL, Garre-Olmo J, Turró-Garriga O, Vilalta-Franch J, López-Pousa S. Differential features of burden between spouse and adult-child caregivers of patients with Alzheimer's disease: An exploratory comparative design. Int J Nurs Stud. 2010;47:1262–73. doi: 10.1016/j.ijnurstu.2010.03.001. [DOI] [PubMed] [Google Scholar]
- 30.Campbell P, Wright J, Oyebode J, Job D, Crome P, Bentham P, et al. Determinants of burden in those who care for someone with dementia. Int J Geriatr Psychiatry. 2008;23:1078–85. doi: 10.1002/gps.2071. [DOI] [PubMed] [Google Scholar]
- 31.Rinaldi P, Spazzafumo L, Mastriforti R, Mattioli P, Marvardi M, Polidori MC, et al. ; Study Group on Brain Aging of the Italian Society of Gerontology and Geriatrics. Predictors of high level of burden and distress in caregivers of demented patients: Results of an Italian multicenter study. Int J Geriatr Psychiatry. 2005;20:168–74. doi: 10.1002/gps.1267. [DOI] [PubMed] [Google Scholar]
- 32.Thommessen B, Aarsland D, Braekhus A, Oksengaard AR, Engedal K, Laake K. The psychosocial burden on spouses of the elderly with stroke, dementia and Parkinson's disease. Int J Geriatr Psychiatry. 2002;17:78–84. doi: 10.1002/gps.524. [DOI] [PubMed] [Google Scholar]
- 33.Papastavrou E, Kalokerinou A, Papacostas SS, Tsangari H, Sourtzi P. Caring for a relative with dementia: Family caregiver burden. J Adv Nurs. 2007;58:446–57. doi: 10.1111/j.1365-2648.2007.04250.x. [DOI] [PubMed] [Google Scholar]
- 34.Bhattacharya P. Orlando, Florida: Institute of Chartered Financial Analysts of India; 2005. Implications of an Aging Population in India: Challenges and Opportunities. Presented at the Living to 100 and Beyond Symposium Sponsored by the Society of Actuaries; pp. 12–14. (1-40). [Google Scholar]
- 35.Sussman T, Regehr C. The influence of community-based services on the burden of spouses caring for their partners with dementia. Health Soc Work. 2009;34:29–39. doi: 10.1093/hsw/34.1.29. [DOI] [PubMed] [Google Scholar]
- 36.Danucalov MA, Kozasa EH, Ribas KT, Galduróz JC, Garcia MC, Verreschi IT, et al. A yoga and compassion meditation program reduces stress in familial caregivers of Alzheimer's disease patients. Evid Based Complement Alternat Med 2013. 2013 doi: 10.1155/2013/513149. 513149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Waelde LC, Thompson L, Gallagher-Thompson D. A pilot study of a yoga and meditation intervention for dementia caregiver stress. J Clin Psychol. 2004;60:677–87. doi: 10.1002/jclp.10259. [DOI] [PubMed] [Google Scholar]
- 38.Innes KE, Selfe TK, Brown CJ, Rose KM, Thompson-Heisterman A. The effects of meditation on perceived stress and related indices of psychological status and sympathetic activation in persons with Alzheimer's disease and their caregivers: A pilot study. Evid Based Complement Alternat Med 2012. 2012 doi: 10.1155/2012/927509. 927509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cristancho-Lacroix V, Kerhervé H, de Rotrou J, Rouquette A, Legouverneur G, Rigaud AS. Evaluating the efficacy of a web-based program (diapason) for informal caregivers of patients with Alzheimer's disease: Protocol for a randomized clinical trial. JMIR Res Protoc. 2013;2:e55. doi: 10.2196/resprot.2978. [DOI] [PMC free article] [PubMed] [Google Scholar]


