Abstract
Background and Aims:
Ventilator-associated pneumonia (VAP) is a major challenge in intensive care units (ICUs). This challenge is even more discernible in a neurological setting owing to the predispositions of patients. Data on VAP in the neurology and neurosurgery ICUs (NNICUs) are scanty in developing countries. This study was conducted to find out the occurrence of VAP, its risk factors, microbiological profile, and antibiotic resistance in patients admitted to the NNICU of a tertiary care institute in India.
Materials and Methods:
Endotracheal aspirate and blood samples were collected from 100 patients admitted to the NNICU. Complete blood count, microscopic examination, culture and sensitivity testing of aspirate were done. Chest x-ray was also performed to aid in the diagnosis of VAP.
Results:
Incidence rate of VAP was found to be 24%. Acinetobacter baumannii was the most common pathogen (24.3%) isolated from patients with VAP, and all of these isolates were sensitive to meropenem. Duration of mechanical ventilation (P < 0.0001) and associated comorbid illness (P = 0.005) were found to be significantly associated with VAP, and the duration of mechanical ventilation was found to be the only independent risk factor (P < 0.0001).
Conclusions:
This study highlights the risks and microbiological perspective of ventilator use among neurology patients so that adequate preventive strategies can be adopted on time.
Keywords: Healthcare-associated infections (HAI), neurosurgery, ventilator-associated pneumonia (VAP)
Introduction
Ventilator-associated pneumonia (VAP) is defined as pneumonia that occurs 48 h later or thereafter following endotracheal intubation, characterized by the presence of a new or progressive infiltrate, signs of systemic infection (fever and altered white blood cell count), changes in sputum characteristics, and detection of a causative agent.[1] Nosocomial pneumonias, including VAP, are the leading cause of infections in a hospital setting.[2] Intubation and mechanical ventilation are associated with 6- to 21-fold increased risk of acquiring pneumonia in hospital settings.[3]
Specific neurological and neurosurgical intensive care has gained importance in the last few decades.[4] However, it is still a new and evolving concept in developing countries such as India. Neurosurgical intensive care is primarily usually aimed at care of unconscious patients, monitoring and treatment of raised intracranial pressure, mechanical ventilator support, specific treatment for underlying neurological illness, and management of comorbid medical conditions and complications.[5]
There are several risk factors responsible for intensive care unit (ICU) outcome and mortality. Healthcare-associated infections (HAIs) are major contributors, while type of disease and its severity score, invasive procedures or intervention, and the length of the ICU stay are other factors. HAI rates especially depend on the disease severity and the exposure to invasive devices (such as ventilators, urinary catheters, or central venous catheters).
There are number of studies regarding incidence, prevalence, risk factors, and the impact of nosocomial/HAI on mortality and outcome in multidisciplinary ICUs; however, owing to the limited facility of separate neurological and or neurosurgical ICUs (NNICUs) in developing countries, only a few studies are available in reference to HAI in the NNICU-setting and still fewer regarding VAP among these patients.[6,7]
Available data about HAI or nosocomial infection in other medical and surgical ICU patients cannot be extrapolated to the NNICU patients, because patients with neurological disorder due to their altered mental state or motor disability are at greater risk of aspiration pneumonia.
The present research was conducted to study the occurrence and pattern of VAP in the NNICU; its risk factors, microbiologic profile, and resistance pattern were also studied. The study aimed to help the clinicians to better understand the contributing factors and disease outcome in patients who acquire VAP in the NNICU and also to establish preventive measures against these infections in the management of severely ill patients with neurological disorders.
Materials and Methods
This prospective observational study was carried out in the NNICU and microbiology departments of a tertiary care institution located in New Delhi. One hundred consecutive patients admitted to the NNICU were studied. This study was started after obtaining ethical clearance from Institutional Ethics Committee. Written informed consent was obtained from the subjects and their caregivers after explaining the purpose of the study to them.
Study group
Patients hospitalized for more than 24 h in the NNICU of the hospital.
Some patients died within the first 24-h period and the patients whose duration of ICU stay was less than 24 h were excluded from the study. Data were recorded regarding demographic details, duration of hospital stay, neurological diagnosis of the patient and its severity, comorbid illness(s), respiratory symptoms (if any), microorganism(s) isolated after culture, and antibiotic sensitivity profile. Clinical scores for general disease severity was measured using the Acute Physiology and Chronic Health Evaluation (APACHE II) index[8] and consciousness impairment score was measured using the Glasgow Coma Scale (GCS)[9] on admission and subsequently. Finally, disease outcome was noted.
Data collection
During the study period, a daily surveillance of patients was conducted from the time of admission to 48 h after discharge from the NNICU. Each subject was followed up over the entire stay in ICU. The number of ventilator days was recorded.
Sample collection and investigations
Endotracheal aspirate and blood samples were collected from each subject in sterile vials and transported to laboratory as soon as possible for culture and sensitivity testing. Complete blood count and microscopic examination of aspirate were also conducted. Chest x-ray was done to aid in the diagnosis of VAP.
The diagnosis of VAP was confirmed on the basis of presence of a new or progressive radiographic infiltrate plus at least two of three clinical features (fever, body temperature >38°C, leukocytosis or leukopenia, and purulent secretions). The etiologic agent of pneumonia was identified by semiquantitative cultures of endotracheal aspirates.[1]
The rate of incidence of VAP was calculated as VAP/1000 ventilator days and ventilator utilization ratio calculated as number of ventilator days/number of patient days.
Statistical analysis
Values were expressed as mean ± SD. Pearson's Chi-square test and Fisher's exact test were used in univariate analysis. All statistical analysis was employed Statistical Package for the Social Sciences (SPSS) version 20.0 software (SPSS-Inc., Chicago, US) to ascertain statistical significance. P < 0.05 was taken as statistically significant in all tests.
Results
Demographic profile of studied patients in the NNICU
A total of 100 patients from the NNICU were recruited in the study. Their age and sex are given in Table 1.
Table 1.
Age and sex of studied patients in the NNICU
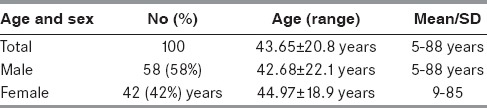
Total duration of the NNICU stay of these patients was 1,967 days, and the mean duration of the NNICU stay was 19.67 ± 17 days (ranged 3-123 days).
Primary diagnosis of studied patients in the NNICU
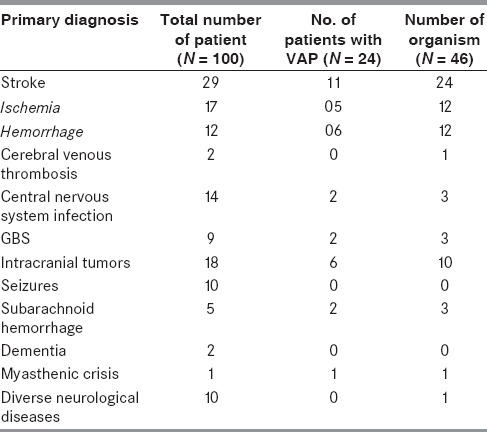
Stroke was the most common diagnosis (29%) among the studied subjects followed by intracranial tumors (18%). Rest of the patients presented with central nervous system (CNS) infections (14%), seizures (10%), Guillain–Barré syndrome (GBS) (9%), subarachnoid hemorrhage (5%), dementia (2%), cerebral venous thrombosis (2%), myasthenic crises (1%), and diverse neurological diseases (10%). Presence of VAP in studied subjects in the NNICU based on individual primary diagnosis is shown in Table 2.
Table 2.
VAP in studied subjects in relation to primary diagnosis
Seven of the patients were diagnosed with cardiovascular disease (CAD) and left ventricular dysfunction and three had history of pulmonary tuberculosis (treated). Two patients were known case of chronic obstructive pulmonary disease (COPD).
Ventilator-associated pneumonia (VAP)
Out of 100 patients in the NNICU, pneumonia was detected in 35 patients (35%). Twenty four patients were found to have VAP. Altogether 37 pathogens were isolated in patients with VAP. A single microorganism was isolated in 14 of 24 patients (58.3%). The bacterial isolates were found in endotracheal aspirates (83.3%) and blood samples (8.3%). In two subjects (8.3%), no organism could be isolated. Nineteen patients had early VAP (occurring within 4 days but after 48 h of hospitalization or tracheal intubation), whereas 5 had late VAP that occurred after 4 days of hospitalization or tracheal intubation. Ventilator utilization ratio was 0.42 and VAP rate was 29.3%. Risk factors for development of VAP are presented in Table 3.
Table 3.
Univariate analysis of risk factors for VAP
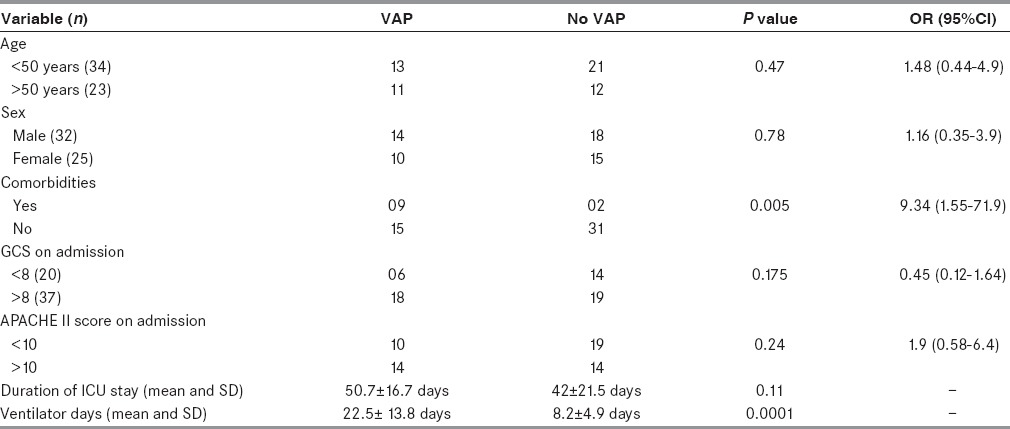
Increased duration of mechanical ventilation (P < 0.0001) and associated comorbid illness (P = 0.005) including chronic obstructive airway disease, diabetes mellitus, left ventricular dysfunction, and chronic kidney disease were significantly associated with VAP in univariate analysis. In multivariate analysis, duration of mechanical ventilation was the only independent risk factor (P < 0.0001). Incidence of VAP/1000 ventilators-days was 29.3%. Gram-positive organisms constituted 29.4% while gram-negative organisms constituted 70.5% of the isolated pathogens. Acinetobacter baumannii was the most common pathogen (26.4%) isolated from patients with VAP. There was no significant difference of bacterial pathogens between early and late onset VAP. Resistance rates of isolated organisms were also studied [Tables 4 and 5].
Table 4.
Resistance rates of common gram-negative pathogens to antibiotics (%) in VAP
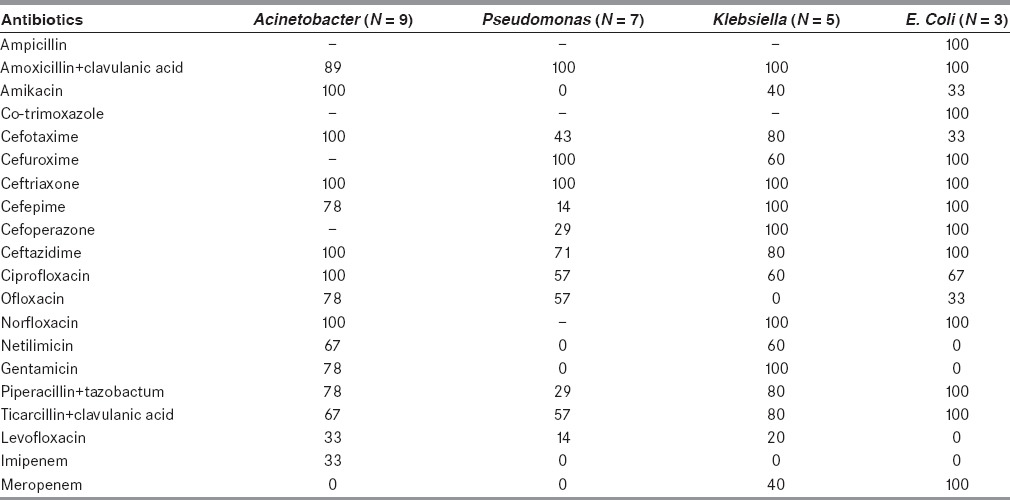
Table 5.
Resistance rate of common gram-positive pathogens to antibiotics (%) in VAP
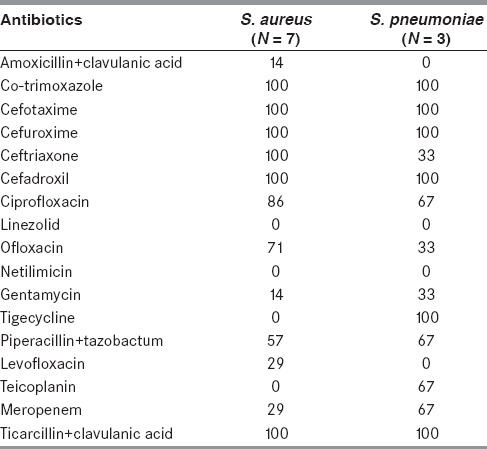
All the A. baumannii isolates were found to be sensitive to meropenem. Pseudomonas, Klebsiella and E. coli were 100% sensitive to imipenem, while resistance to imipenem was recorded in 33% of Acinetobacter isolates. All gram-negative organisms causing VAP were resistant to ceftriaxone (100%). All the gram-positive organisms were found to be sensitive to linezolid and netilmicin. Most of the cephalosporins were found to be resistant against gram-positive organisms [Tables 3 and 4].
Discussion
VAP is one of the frequent problems that patients develop during the ICU stay. It is the second most common nosocomial infection in the ICU and the most common among mechanically ventilated patients.[10,11] Several studies have been conducted regarding the same in multispeciality ICUs[12] and some in neurologic ICUs,[13] but data on VAP in patients admitted to the NNICU is meagre in low and middle income countries (LAMICs). In spite of the advances in the diagnostic modalities, treatment options, and preventive measures of VAP, it continues to be a major cause of morbidity and mortality among severely ill patients.[14] The problem further accentuates in patients with neurological diseases due to altered mental status and comorbidities.
Hence, this study was conducted in greater detail on the occurrence and pattern of VAP in the NNICUs. VAP complicated the course of 24% of our studied patients. In our study, the ventilator utilization ratio (0.42) was higher than that of the studies by Dettenkofer et al.[15] (0.22) and Yilmaz et al.[16] (0.07). Given the comparably high figure for ventilator use, more than three fourth cases of nosocomial or hospital-acquired pneumonia in our study were ventilator associated. VAP was responsible for 37% of all nosocomial pneumonia in Dettenkofer et al.'s study and authors attributed the less incidence of VAP to the low ventilator utilization ratio.[15]
VAP rate in our study was 29.3/1,000 ventilator-days. VAP per/1,000 ventilators-days were 12.8, 27.4, and 20.4 in other neurology specific ICU studies by Zolldann et al.,[17] Zolldann et al.,[18] and Dettenkofer et al.,[15] respectively.
The incidence of VAP reported is highly varied. It mainly varies according to the definition, the type of ICU, type of illness, the cohort studied, and the history of antibiotic exposure. The paucity of consensus regarding the most suitable method for the diagnosis of VAP also explains this variation in VAP incidence among different studies.
In the majority of reports from medical ICUs, the VAP frequencies varied from 6% to 52%, and incidence rate ranges from 13.2 to 51 per 1,000 ventilator days.[19,20] A study conducted in Athens in four multidisciplinary ICUs showed that tracheostomy, bronchoscopy, enteral feeding, duration of mechanical ventilation for >5 days, mean duration of central vein catheterization, APACHE II score >18 on admission, and acute physiology score >10 on admission had a significant association with VAP on univariate analysis. Also other studies have demonstrated that tracheostomy, multiple central venous line insertions, reintubation, duration of stay, and impaired consciousness are independent risk factors for the development of VAP.[14]
In the present study, increased duration of mechanical ventilation (P < 0.0001) and associated comorbid illness (P = 0.005) were significantly associated with VAP in univariate analysis. Present study revealed that duration of mechanical ventilation was an important risk factor for VAP as was reported in other studies as well. The mean duration of ventilation among non-VAP and VAP patients was 8.2 days and 22.5 days, respectively, which is similar to other studies.[21,22] All pneumonia patients in our study had bacterial isolation from respiratory secretions and none could be isolated from blood. Therefore, blood culture had very low sensitivity in determining the causative bacteria of pneumonia, as previously reported.
In our study, 37 pathogens were isolated from VAP. Of these strains, 26 (79%) were gram-negative bacteria and the most frequently isolated pathogens were A. baumannii (24.3%) and Pseudomonas aeruginosa (19%). Staphylococcus aureus was the most frequent gram-positive pathogen. Acinetobacter spp. (22.4%) and S. aureus (16.3%) were the two most commonly isolated strains as reported in Dettenkofer et al.'s study.[15] Studies performed in non-neurological ICUs have revealed polymicrobial etiology of VAP in about 30-70% of the cases.[23] In a study conducted by Combes et al.,[24] more than one microorganism was isolated in 48% of the VAP cases. In another two studies performed in medical ICUs of India by Mukhopadhyay et al.[25] and Singhal et al.[26] 12.3% and 16.3% of VAP cases, respectively, demonstrated the presence of more than one organism. Similar to results from previous studies, carbapenems were found to be an effective antibiotic for A. baumannii and other gram-negative pathogens-associated VAP.[27,28]
To conclude, 24% of the patients developed VAP. A. baumannii was the most common pathogen (24.3%) isolated from patients with VAP. Meropenem was found to be the most sensitive antibiotic against A. baumannii-associated VAP. In multivariate analysis, duration of mechanical ventilation was found to be the only independent risk factor (P < 0.0001) for VAP.
Hence, VAP is a big challenge in the setting of neurological ICUs. This study highlights the risk factors associated with VAP so that adequate preventive measures can be implemented. Understanding the microbiological milieu of neurological ICUs and their resistance pattern could aid in prompt diagnosis and early and effective treatment of the affected patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.American Thoracic Society; Infectious Diseases Society of America. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2005;171:388–416. doi: 10.1164/rccm.200405-644ST. [DOI] [PubMed] [Google Scholar]
- 2.Behnia M, Logan SC, Fallen L, Catalano P. Nosocomial and ventilator-associated pneumonia in a community hospital intensive care unit: A retrospective review and analysis. BMC Res Notes. 2014;7:232. doi: 10.1186/1756-0500-7-232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Weber DJ, Rutala WA, Mayhall CG. Nosocomial respiratory tract infections and Gram negative pneumonia. In: Fishman AP, Elias JA, Fishman JA, Grippi MA, Kaiser LR, Senior RM, editors. Pulmonary Disease and Disorders. 3rd ed. New York: McGraw-Hill; 1998. pp. 2213–27. [Google Scholar]
- 4.Schmutzhard E. New developments and perspectives of intensive neurology. Wien Klin Wochenschr. 1999;111:713–8. [PubMed] [Google Scholar]
- 5.Meena AK, Prasad VS, Murthy JM. Neurological intensive care in India — Disease spectrum and outcome. Neurol India. 2001;49(Suppl 1):S1–7. [PubMed] [Google Scholar]
- 6.Shafer SQ, Brust JC, Healton EB, Mayo JB. Hospital-acquired morbidity on a neurology service. J Natl Med Assoc. 1993;85:31–5. [PMC free article] [PubMed] [Google Scholar]
- 7.Heckmann JG, Kraus J, Niedermeier W, Erbguth F, Druschky A, Schoerner C, et al. Nosocomial pneumonias in a neurology intensive care unit. Dtsch Med Wochenschr. 1999;124:919–24. doi: 10.1055/s-2007-1024452. [DOI] [PubMed] [Google Scholar]
- 8.Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: A severity of disease classification system. Crit Care Med. 1985;13:818–29. [PubMed] [Google Scholar]
- 9.Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974;2:81–4. doi: 10.1016/s0140-6736(74)91639-0. [DOI] [PubMed] [Google Scholar]
- 10.Hunter JD. Ventilator associated pneumonia. BMJ. 2012;344:e3325. doi: 10.1136/bmj.e3325. [DOI] [PubMed] [Google Scholar]
- 11.Afshari A, Pagani L, Harbarth S. Year in review 2011: Critical care — Infection. Crit Care. 2012;16:242. doi: 10.1186/cc10425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kalanuria AA, Zai W, Mirski M. Ventilator-associated pneumonia in the ICU. Crit Care. 2014;18:208. doi: 10.1186/cc13775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Josephson SA, Moheet AM, Gropper MA, Nichols AD, Smith WS. Ventilator-associated pneumonia in a neurologic intensive care unit does not lead to increased mortality. Neurocrit Care. 2010;12:155–8. doi: 10.1007/s12028-009-9285-x. [DOI] [PubMed] [Google Scholar]
- 14.Ibrahim EH, Tracy L, Hill C, Fraser VJ, Kollef MH. The occurrence of ventilator-associated pneumonia in a community hospital: Risk factors and clinical outcomes. Chest. 2001;120:555–61. doi: 10.1378/chest.120.2.555. [DOI] [PubMed] [Google Scholar]
- 15.Dettenkofer M, Ebner W, Els T, Babikir R, Lucking C, Pelz K, et al. Surveillance of nosocomial infections in a neurology intensive care unit. J Neurol. 2001;248:959–64. doi: 10.1007/s004150170048. [DOI] [PubMed] [Google Scholar]
- 16.Yilmaz GR, Cevik MA, Erdinc FS, Ucler S, Tulek N. The risk factors for infections acquired by cerebral hemorrhage and cerebral infarct patients in a neurology intensive care unit in Turkey. Jpn J Infect Dis. 2007;60:87–91. [PubMed] [Google Scholar]
- 17.Zolldann D, Spitzer C, Häfner H, Waitschies B, Klein W, Sohr D, et al. Surveillance of nosocomial infections in a neurologic intensive care unit. Infect Control Hosp Epidemiol. 2005;26:726–31. doi: 10.1086/502610. [DOI] [PubMed] [Google Scholar]
- 18.Zolldann D, Poetter C, Hilker R, Neveling M, Waitschies B, Klein W, et al. Periodic surveillance of nosocomial infections in two neurology intensive care units. A valuable tool for quality management in intensive care. Anaesthesist. 2003;52:690–6. doi: 10.1007/s00101-003-0528-5. [DOI] [PubMed] [Google Scholar]
- 19.Alp E, Voss A. Ventilator associated pneumonia and infection control. Ann Clin Microbiol Antimicrob. 2006;5:7. doi: 10.1186/1476-0711-5-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Joseph NM, Sistla S, Dutta TK, Badhe AS, Parija SC. Ventilator-associated pneumonia in a tertiary care hospital in India: Incidence and risk factors. J Infect Dev Ctries. 2009;3:771–7. doi: 10.3855/jidc.396. [DOI] [PubMed] [Google Scholar]
- 21.Cook DJ, Reeve BK, Guyatt GH, Heyland DK, Griffith LE, Buckingham L, et al. Stress ulcer prophylaxis in critically ill patients. Resolving, discordant meta-analyses. JAMA. 1996;275:308–14. [PubMed] [Google Scholar]
- 22.Gadani H, Vyas A, Kar AK. A study of ventilator-associated pneumonia: Incidence, outcome, risk factors and measures to be taken for prevention. Indian J Anaesth. 2010;54:535–40. doi: 10.4103/0019-5049.72643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Torres A, Carlet J. Ventilator-associated pneumonia. European Task Force on ventilator-associated pneumonia. Eur Respir J. 2001;17:1034–45. doi: 10.1183/09031936.01.17510340. [DOI] [PubMed] [Google Scholar]
- 24.Combes A, Figliolini C, Trouillet JL, Kassis N, Wolff M, Gibert C, et al. Incidence and outcome of polymicrobial ventilator-associated pneumonia. Chest. 2002;121:1618–23. doi: 10.1378/chest.121.5.1618. [DOI] [PubMed] [Google Scholar]
- 25.Mukhopadhyay C, Bhargava A, Ayyagari A. Role of mechanical ventilation and development of multidrug resistant organisms in hospital acquired pneumonia. Indian J Med Res. 2003;118:229–35. [PubMed] [Google Scholar]
- 26.Singhal R, Mohanty S, Sood S, Das B, Kapil A. Profile of bacterial isolates from patients with ventilator associated pneumonias in a tertiary care hospital in India. Indian J Med Res. 2005;121:63–4. [PubMed] [Google Scholar]
- 27.Muno z-Price LS, Weinstein RA. Acinetobacter infection. N Engl J Med. 2008;358:1271–81. doi: 10.1056/NEJMra070741. [DOI] [PubMed] [Google Scholar]
- 28.Martin-Loeches I, Deja M, Koulenti D, Dimopoulos G, Marsh B, Torres A, et al. EU-VAP Study investigators: Potentially resistant microorganisms in intubated patients with hospital-acquired pneumonia: The interaction of ecology, shock and risk factors. Intensive Care Med. 2013;39:672–81. doi: 10.1007/s00134-012-2808-5. [DOI] [PubMed] [Google Scholar]


