Abstract
Objectives
To examine the presence of a dose-response relationship between work hours and incident cardiovascular disease (CVD) in a representative sample of U.S. workers.
Methods
Retrospective cohort study of 1,926 individuals from the Panel Study of Income Dynamics (1986–2011) employed for at least 10 years. Restricted cubic spline regression was used to estimate the dose-response relationship of work hours with CVD.
Results
A dose-response relationship was observed in which an average workweek of 46 hours or more for at least 10 years was associated with increased risk of CVD. Compared to working 45 hours per week, working an additional 10 hours per week or more for at least 10 years increased CVD risk by at least 16%.
Conclusions
Working more than 45 work hours per week for at least 10 years may be an independent risk factor for CVD.
BACKGROUND
Cardiovascular disease (CVD), a group of disorders of the heart and blood vessels, affects more than one in three U.S. adults and is the leading cause of mortality in the U.S.1 Despite declining numbers of CVD-attributable deaths since the 1980s,1 morbidity and mortality due to CVD are projected to remain high for at least the next several decades, with the estimated prevalence of CVD exceeding 40 percent by 2030.2
Numerous studies have reported a positive association between long work hours (e.g., work hour durations in excess of a standard work week) and increased CVD risk,3–6 although the finding is not universal.7 Similarly, most, 8, 9 but not all,10 recent meta-analyses examining CVD or the more limited diagnosis of coronary heart disease have demonstrated an association with long work hours. Changes in the activity of the autonomic, sympathetic, and/or parasympathetic nervous systems have been suggested as potential mechanisms through which working long hours influences cardiovascular health, as has increased blood pressure.11 Substantial evidence exists that working long hours is associated with many CVD-related risk factors (e.g., hypertension,12, 13 heart rate variability,14 smoking,15 physical inactivity,15 stress15, 16 and depression17), and it has been suggested that increasing work hour durations may have a dose-response relationship with CVD.9, 18
To our knowledge, no study has focused on evaluating the presence of a dose-response relationship between continuous measures of weekly work hour durations and CVD. Further, there currently exists no study on the relationship between average weekly work hour estimates and CVD using longitudinal data from a large, representative sample of U.S. workers. The purpose of the present study was to assess the association between work hours and incident CVD, including the presence of a dose-response relationship, in a representative sample of U.S. workers drawn from the Panel Study of Income Dynamics (PSID) and followed for a minimum of 10 years.
METHODS
Study Population
We conducted a retrospective cohort study utilizing existing data collected from participants enrolled in the PSID, which has been described in detail elsewhere.19, 20 Briefly, the PSID is an ongoing longitudinal survey of a representative sample of U.S. households performed annually from 1968 until 1997 and biennially since 1999.20 Participants have been surveyed on their work hours since 1968 and on specific health outcomes, including CVD, since 1999. The PSID response rates have been over 90% since 197020; currently, more than 22,000 individuals in 9,000 families are active participants in the PSID sample.19
In the present study, we included PSID participants aged 18 years or older at baseline (1986) and followed them through 2011. Individuals were included who reported non-zero work hours for a minimum of 10 years. Those under the age of 18 in 1986 (n=10,279) and those reporting fewer than 10 years of non-zero work hour data over the study duration (n=8,603) were excluded. Participants also had to be free of CVD during the first 10 years of non-zero work hours. We excluded those who reported CVD before accumulating 10 years of non-zero work hours (n = 467) or at baseline (n = 658), as well as those missing CVD data (n = 364). In addition, participants with other prevalent chronic health conditions or disabilities at baseline (n = 529) or missing those data (n = 119) were excluded. The final sample for these analyses included 1,926 workers.
Data Collection
For each year in the study, the total annual hours of work was calculated from self-reported data for the previous year using information on the number of jobs worked; the mean number of hours worked per week per job; the amount of overtime worked per week, on average; the number of weeks of worked missed for any reason (i.e., illness, vacation, strike, unemployment, or layoff); and the start and stop dates for up to four jobs. The total annual hours of work for each year was divided by 50 weeks to generate the total number of work hours per week in the previous year on all jobs.
For the outcome of CVD, participants were asked to report if they had ever been told by a physician that they had angina, coronary heart disease, congestive heart failure, a heart attack, high blood pressure/hypertension, or stroke. The first affirmative report of any of these CVD-related conditions was coded as incident CVD.
Occupational data from each survey wave were collected and dichotomized as follows: industry (service vs. non-service), occupation (manual vs. non-manual), pay status (hourly vs. salary), and employment type (self-employed vs. employed by other). Socio-demographic data were also collected, including age, sex, marital status (married/cohabitating vs. not married/not cohabitating), education level (did not complete high school; high school diploma; or, college degree), and race/ethnicity (White, non-Hispanic; Black, non-Hispanic; Hispanic; or, other). In addition, household membership data were collected, including number of children in the household, household and individual income (e.g., annual household income, annual individual income by job, annual overtime income), household and individual expenses (e.g., monthly rent/mortgage payment, annual child care expenses), and health insurance status (yes/no).
Statistical Analysis
We first described, with frequencies and percentage or means and standard errors, the study sample according to its socio-demographic and occupational characteristics at baseline by CVD status at follow-up. Adjusted Wald tests and Pearson χ2 statistics were used to compare the means of continuous covariates and prevalence of categorical covariates, respectively.
Administrative censoring of those participants reporting an outcome event occurred following the first report; work hour data for cases was censored in the year in which the incident case was reported and no subsequent data specific to that outcome were analyzed on those individuals. The relative risk (RR) of incidence CVD and 95% confidence intervals (CI) were estimated using Poisson regression in relation to the average weekly hours worked, adjusting for age, sex, education, race/ethnicity, and pay status; an offset variable was used to adjust for variations in exposure duration for years worked. Covariates were paired with each other and with the exposure of interest to assess the presence of interaction. Because it has been suggested that part-time workers may be at greater risk of CVD than full-time workers,11 a stratified analysis of part-time (participants averaging <35 work hours per week (WH/w) over the study duration) and full-time (averaging ≥35 WH/w over the study duration) workers was performed.
A Lowess smoothing curve and a plot of work hour quartile coefficients versus means were visually inspected to assess the linearity of the exposure variable in the Poisson model, both of which indicated departure from linearity. As a result, a Poisson restricted cubic spline model was selected for the analysis of the dose-response relationship for work hours (i.e., a continuous measure of average work hours per week over the study duration) and CVD, which took into account clustering (i.e., household membership) and probability weighting and which used robust standard errors.21, 22 Restricted cubic splines were preferred due to their flexibility in modeling the underlying functional form, given that they allow a parabolic curve to connect the line segments at the points of intersection23 and reduce the instability of the estimates at the tails of the curve.24 The optimal number of segments was selected by introducing an increasing number of knots at subsequent quantiles into the model. The best fitting model was defined as the one that minimized the Akaike Information Criterion (AIC)25; that model had three knots placed at 35.01, 40.06, and 46.12 work hours per week.
We tested the performance of the restricted cubic spline model against other candidate models (i.e., Poisson log-linear; Poisson quadratic model, in which a quadratic term for the exposure was added to the model; Poisson step function, in which the exposure was categorized; the Poisson restricted linear spline model); all models under consideration (including the cubic spline model) were constructed as a set of hierarchical regression models. The restricted cubic spline model was chosen based on its relative performance in terms of parsimony (i.e., degrees of freedom) and model fit (i.e., the Hosmer Lemeshow goodness-of-fit statistic and the Bayesian Information Criteria). The linear and cubic spline models were superior to the other models in terms of model fit but not degrees of freedom; the cubic spline model performed better than the linear spline model in terms of degrees of freedom.
Because coefficients associated with cubic spline segments are not themselves interpretable, the cubic spline regression coefficients were used to generate the equation for the cubic spline regression. We then introduced specific work hour durations into the cubic spline equation and calculated the relative risks (RRs) of those work hour durations against a reference duration of 45 work hours per week. We selected an average of 45 work hours per week as our basis for comparison in order to reflect the patterns of work typically reported by U.S. workers26 and to generate more conservative comparisons relative to 40 hours of work per week.
All analyses were performed using Stata/SE software (version 13.1; Stata Corp, College Station, TX).
RESULTS
Table 1 presents baseline descriptive statistics for the entire study population (n = 1,926). Slightly more than half of participants were male (52.4%). The mean age of participants was 32.8 years (SE: 0.3; range: 18 – 65, data not shown). White, non-Hispanic individuals comprised the largest racial/ethnic group (88.8%), followed by Black, non-Hispanics (6.2%), and Hispanics (3.2%). The majority of participants worked in service industries (70.5%) and in non-manual occupations (73.5%). They were also more likely to be employed by others (i.e., not self-employed; 84.1%) and to be salaried (45.6%). Participants averaged 39.2 hours of work per week (S.E.: 0.3; range: 0 – 103.2, data not shown).
Table 1.
Demographic and Occupational Characteristics of Study Sample at Baseline by Cardiovascular Disease Status: Panel Study of Income Dynamics, 1986–2011.
| All | Incident cardiovascular diseasea
|
P-valueb | ||
|---|---|---|---|---|
| Cases | Non-cases | |||
| n = 1,926 | n = 822 (40.7%) | n = 1,104 (59.3%) | ||
| Sex | 0.109c | |||
| Male | 979 (52.4) | 446 (56.3) | 533 (51.5) | |
| Female | 947 (47.6) | 376 (43.7) | 571 (48.5) | |
| Age (years) | <0.001d | |||
| Mean (Standard Error) | 32.8 (0.3) | 35.5 (0.4) | 30.9 (0.3) | |
| Educational level (highest completed) | 0.325c | |||
| Did not complete high school | 159 (7.0) | 79 (7.3) | 80 (7.1) | |
| High school diploma | 1,187 (60.2) | 491 (58.2) | 696 (59.4) | |
| College degree | 580 (32.8) | 252 (34.5) | 328 (33.5) | |
| Race/Ethnicity | <0.001c | |||
| White, non-Hispanic | 1439 (88.8) | 549 (84.8) | 890 (92.3) | |
| Black, non-Hispanic | 415 (6.2) | 233 (8.5) | 182 (4.2) | |
| Hispanic | 43 (3.2) | 24 (3.8) | 19 (2.3) | |
| Other | 24 (1.8) | 13 (2.9) | 11 (1.2) | |
| Marital status | 0.223c | |||
| Married/cohabitating | 1,591 (83.1) | 664 (79.8) | 927 (82.6) | |
| Not married or cohabitating | 335 (16.9) | 158 (20.2) | 177 (17.4) | |
| Number of children in the household | 0.043d | |||
| Mean (Standard Error) | 1.11 (0.04) | 1.18 (0.06) | 1.04 (0.05) | |
| Employment status | 0.045c | |||
| Self-employed | 216 (15.9) | 104 (18.4) | 112 (13.7) | |
| Employed by others | 1423 (84.1) | 617 (81.6) | 806 (86.3) | |
| Industry | 0.357c | |||
| Services | 1,159 (70.5) | 497 (69.7) | 662 (72.4) | |
| Non-services | 486 (29.5) | 224 (30.3) | 262 (27.6) | |
| Occupational social class | 0.347c | |||
| Manual | 488 (26.5) | 228 (28.2) | 260 (25.6) | |
| Non-manual | 1170 (73.5) | 499 (71.8) | 671 (74.4) | |
| Pay status | 0.285c | |||
| Salaried | 695 (45.6) | 290 (44.9) | 405 (49.2) | |
| Hourly | 737 (39.5) | 335 (39.2) | 402 (37.8) | |
| Other arrangement | 227 (14.9) | 103 (15.9) | 124 (13.0) | |
| Work hours per week | 0.032d | |||
| Mean (Standard Error) | 36.3 (0.4) | 37.5 (0.7) | 35.5 (0.6) | |
Proportions adjusted for probability weighting.
All calculations take into account clustering and probability weighting.
Pearson χ2 test.
Adjusted Wald test.
At study baseline, those who developed CVD were older, more likely to be non-white, and reported a greater number of children residing in the household compared to non-cases; they were also more likely to be self-employed. Differences in baseline mean work hours were noted between outcome groups, with participants with CVD at follow-up having reported an average work week at baseline that was two hours longer than that of participants without CVD at follow-up (37.5 versus 35.5 hours, respectively; p-value: 0.032). No differences were observed for other demographic and occupational characteristics by outcome status.
Over the study duration, 822 participants (or 42.7%) reported physician-diagnosed incident CVD. Individuals who developed CVD were more likely to report working full-time than those who did not develop CVD (72.8% versus 67.2%, respectively; p-value: 0.038), and they worked an average of 1.5 hours more per week than those who did not develop CVD (40.1 versus 38.6 hours, respectively; p-value: 0.012). The mean number of survey waves for which participants reported work hour data was 16.3 (S.E.: 0.1) out of 19 waves of follow-up, with a statistically significant difference seen between those who did and did not develop CVD (14.5 versus 17.5 waves, respectively; p-value < 0.001); this was expected due to post-event censoring of work hour data. Additionally, the mean time to diagnosis for those who developed incident CVD was 17.4 years (S.E.: 0.2). Among those individuals averaging full-time work weeks, 88.0% reported working full time for the entirety of the study duration; among part-time workers, 66.7% reported working part time for the entire study duration.
There was no evidence of an elevated risk of CVD for each increasing hour of work per week (RR: 1.00; 95% C.I.: 1.00 – 1.01; p-value: 0.356) in the univariate analysis (Table 2). However, adjusting for age, sex, race/ethnicity, and pay status, there was evidence of a 1% increase in the risk of CVD for each additional hour worked per week, on average, for a minimum of 10 years (RR: 1.01; 95% CI: 1.00 – 1.02; p-value: 0.014). The same 1% increase in CVD risk was observed among full-time workers but not among part-timers (Table 3). No significant results were seen in the tests for interaction using conventional criteria (i.e., interaction term p-value <0.05).
Table 2.
Association between work hours and incident cardiovascular disease: Panel Study of Income Dynamics, 1986–2011.
| Variable | Univariate modela
|
Multivariate modela,b
|
||
|---|---|---|---|---|
| RR | (95% C.I.) | RR | (95% C.I.) | |
| Work Hours per Week^ | 1.00 | (1.00 – 1.01) | 1.01 | (1.00 – 1.02)* |
| Age | 1.03 | (1.02 – 1.04) | 1.03 | (1.03 – 1.04) |
| Sex | ||||
| Female | 1.00 | Referent | 1.00 | Referent |
| Male | 1.11 | (0.97 – 1.27) | 1.07 | (0.91 – 1.25) |
| Race/Ethnicity | ||||
| White, Non-Hispanic | 1.00 | Referent | 1.00 | Referent |
| Black, Non-Hispanic | 1.56 | (1.32 – 1.84) | 1.64 | (1.37 – 1.97) |
| Hispanic | 1.37 | (0.93 – 2.02) | 1.35 | (0.97 – 1.88) |
| Other | 1.50 | (1.00 – 2.25) | 1.28 | (0.87 – 1.89) |
| Pay Status | ||||
| Salaried | 1.00 | Referent | 1.00 | Referent |
| Hourly | 1.10 | (0.95 – 1.28) | 1.17 | (1.02 – 1.35) |
All calculations take into account clustering and probability weighting.
All calculations take into account clustering and probability weighting.
P value < 0.05
Continuous measure of average work hours per week over the study duration
Table 3.
Association between work hours and incident cardiovascular disease in part-time (averaging <35 work hours per week) and full-time (averaging ≥35 work hours per week) workers: Panel Study of Income Dynamics, 1986–2011.
| Variable | Part-Time Workers (n = 592)
|
Full-Time Workers (n = 1,334)
|
||||||
|---|---|---|---|---|---|---|---|---|
| Univariate modela
|
Multivariate modela,b
|
Univariate modela
|
Multivariate modela,b
|
|||||
| RR | (95% C.I.) | RR | (95% C.I.) | RR | (95% C.I.) | RR | (95% C.I.) | |
| Work Hours per Week^ | 0.98 | (0.96 – 1.00) | 0.99 | (0.96 – 1.02) | 1.01 | (1.00 – 1.02) | 1.01 | (1.00 – 1.02)* |
| Age | 1.02 | (1.01 – 1.03) | 1.04 | (1.02 – 1.05) | 1.04 | (1.03 – 1.04) | 1.04 | (1.03 – 1.05) |
| Sex | ||||||||
| Female | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent |
| Male | 1.29 | (0.93 – 1.80) | 0.89 | (0.60 – 1.31) | 1.06 | (0.89 – 1.27) | 1.04 | (0.84 – 1.29) |
| Race/Ethnicity | ||||||||
| White, Non-Hispanic | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent |
| Black, Non-Hispanic | 1.87 | (1.38 – 2.53) | 2.01 | (1.27 – 3.17) | 1.45 | (1.18 – 1.78) | 1.67 | (1.29 – 2.15) |
| Hispanic | 1.27 | (0.64 – 2.52) | 1.22 | (0.62 – 2.43) | 1.44 | (0.91 – 2.27) | 1.58 | (1.07 – 2.33) |
| Other | 1.59 | (0.78 – 3.27) | 1.75 | (0.95 – 3.23) | 1.47 | (0.92 – 2.34) | 1.39 | (0.85 – 2.25) |
| Pay Status | ||||||||
| Salaried | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent |
| Hourly | 1.26 | (0.90 – 1.75) | 1.21 | (0.85 – 1.71) | 1.07 | (0.91 – 1.27) | 1.15 | (0.96 – 1.39) |
All calculations take into account clustering and probability weighting.
All calculations take into account clustering and probability weighting.
P value < 0.05
Continuous measure of average work hours per week over the study duration
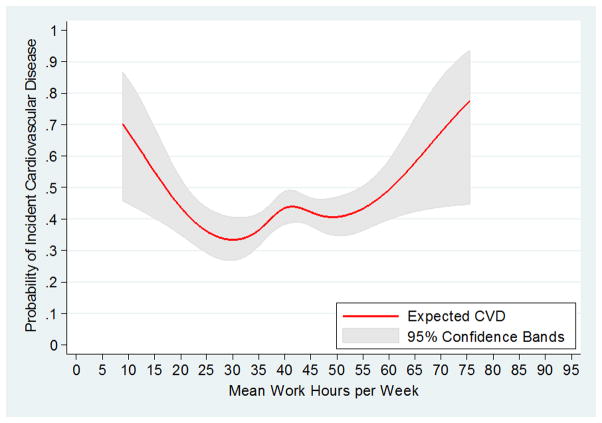
In our examination of a dose-response relationship using the restricted cubic spline model, we observed a decrease in the risk of CVD as work hours increased among those who worked fewer than 30 hours per week (Figure 1). Among those who worked more than 30 hours per week, CVD risk increased as weekly work hours approached 40 hours per week, but declined again between 40 and 46 WH/w. Beginning at 46 WH/w, increasing work hours were progressively associated with increased risk of CVD. Evidence of a statistically significant departure from linearity was noted for the cubic spline function (p-value: 0.0274).
Figure 1.
Restricted cubic spline model for the relationship between long work hours and incident cardiovascular disease: Panel Study of Income Dynamics, 1986–2011.
Compared to those who worked on average 45 hours per week for ten years or more, we observed a 16% (RR: 1.16; 95% CI: 1.02 – 1.32) and a 35% (RR: 1.35: 95% CI: 1.07 – 1.72) increase in CVD risk in participants working 55 and 60 hours per week, respectively, over the same duration (Table 4). Evidence of increased risk of incident CVD continued as the average work hour durations increased to 75 hours per week.
Table 4.
Risk of cardiovascular disease at specific average weekly work hour durations compared to the risk at 45 hours of work per week, on average, for a minimum of 10 years, as estimated from cubic spline regression equation: Panel Study of Income Dynamics, 1986–2011.
| Weekly work hours | Multivariate modela,b
|
|
|---|---|---|
| RR | (95% C.I.) | |
| 45 | 1.00 | Referent |
| 50 | 1.03 | (0.96 – 1.10) |
| 55 | 1.16 | (1.02 – 1.32) |
| 60 | 1.35 | (1.07 – 1.72) |
| 65 | 1.52 | (1.10 – 2.10) |
| 70 | 1.74 | (1.14 – 2.64) |
| 75 | 2.03 | (1.19 – 3.48) |
All calculations take into account clustering and probability weighting.
Model adjusted for age, sex, race/ethnicity, and pay status (hourly vs. salaried).
DISCUSSION
To our knowledge, this is the first report of findings pertaining to an assessment of a dose-response relationship between work hours and incident CVD. In general, we found that the risk of CVD increased as average weekly work hours increased. The shape of the dose-response curve suggested that the most substantial risk was among those working 46 hours per week or greater, on average, for at least ten years. However, we observed a difference in the risk profiles of part-time and full-time workers, as no association was seen between hours worked and CVD in part-time workers. This may indicate the existence of morbidities or habits in part-time workers that limit their work hours and influence their health, as individuals averaging part-time work weeks may be doing so for such disparate reasons as physical limitations, seasonal employment, or personal scheduling preferences. Additionally, it should be noted that CVD risk decreased among full-time workers between 40 and 46 WH/w, which may reflect a window in which work is protective due to its associated benefits, but without the excessive time burden that would preclude achieving adequate physical and psychological rest or engaging in beneficial physical activity.
There is a long history of research on the relationship between occupational stressors and CVD,27 and this study agrees with the findings of two recent meta-analyses, which presented evidence that the risk of CVD increased as working hours increased.9, 18 Kang et al. (2012) reported a 37 percent increase in the odds of CVD among those exposed to long work hours (the definition of which varied by study) compared to those unexposed (95% CI: 1.11 – 1.70), which was not influenced by age, geographical location, or study year. A subgroup analysis of participants working ≤55 hours per week attenuated the relationship between work hour duration and CVD (OR: 1.28; 95% CI: 0.85 – 1.91).18 Virtanen et al. (2012) demonstrated that working long hours (definition varied by study) was associated with an estimated 80 percent increase in the risk of CVD (RR: 1.80; 95% CI: 1.42 – 2.29). In a series of subgroup analyses, they reported that studies defining LWH as a threshold above 50 WH/w had substantially higher RRs than those studies defining LWH as a threshold equal to or below 50 WH/w (RR≤50 WH/w: 1.41; 95% CI: 1.14 – 1.74 vs. RR>50WH/w: 2.37; 95% CI: 1.56 – 3.59).9 However, neither analysis included data from a representative sample of U.S. workers, nor were they focused on the presence of a dose-response relationship. Kivimäki et al. (2015) found no evidence of a dose-response relationship between work hours and the more limited outcome of coronary heart disease (CHD). Additionally, no association was seen between work hours and CHD in a subgroup analysis restricted to U.S. samples, although it is unclear if the combined sample was representative of U.S. workers. In each of these meta-analyses, work hour data were dichotomized or categorized without explanation of the selection of the groupings. Given the lack of evidence for the use of a specific quantity of work hours or set of work hour categories as indicative of health risk, we utilized a continuous measure of work hours in these analyses.
A notable finding from our study was the evidence of a dose-response effect, in which the number of hours worked per week for a minimum of ten years was positively associated with an increasing risk of CVD. Significant relationships between hours worked and CVD were found in each of the models under consideration in the present analyses. Compared to the cubic spline model, however, the other models may have lacked the flexibility to adequately capture the relationship between hours worked and CVD. Because cubic spline modeling accounts for variation among the data within categories as well as across categories, the resulting dose response curve does not assume linearity, as is the case with the Poisson model, and it may be less sensitive to category choice than models such as the step model.28
A strength of this study, then, is that we were able to construct a hierarchical set of nested regression models, which provided advantages over conventional regression models when adjusting for covariates that are strongly interrelated29 as well as when examining possible nonlinear relationships between exposure and risk.23, 30 Although we acknowledge that the selection of the best fitting model involved some subjective criteria, assigning categories or spline knots to produce better fitting models would have required a priori knowledge that is currently unavailable. Instead, an iterative process was undertaken to determine the best placement of the knots given the data, and the shape of the curve was assessed.
Restricted cubic spline regression offered the advantage of parsimony as well as smoothness and flexibility in the shape of the dose response curve and was considered superior to the other models under consideration. However, one drawback of cubic spline models is that the coefficients associated with the spline segments are not interpretable.31 As an alternative, specific work hour durations can be compared by entering those values into the regression equation. Using this method, we found evidence that a ten hour increase from 45 to 55 WH/w, on average, for a minimum of 10 years increased the risk of CVD by 16 percent. These results were not attenuated by sex, and no evidence of effect measure modification was found in terms of sex, industry, or occupation.
PSID data lacked several potentially influential covariates, including many known risk factors for CVD, which may have resulted in residual confounding. Our measures of interest (i.e., work hours, CVD status) were self-reported, which may have introduced bias into the analysis. However, validation studies have demonstrated strong agreement between medical records and most self-reported CVD-related symptoms and events32–34 as well as strong positive correlation between cross-sectional PSID self-reported total hours worked in the previous year and weekly work hours reported by employers.35 Although PSID data are nationally-representative of U.S. households, the proportion of Black (non-Hispanic) and Hispanic participants was reduced in our study sample due to non-response. Finally, given that the mean time to diagnosis was 17.4 years out of a 25 year follow-up period, these data provided adequate follow-up time for case development despite a five-year difference in mean age at baseline between those who would and would not develop CVD. This study benefits from the minimum period of ten years’ time at risk required for participant inclusion as well as the censoring of exposure data in the survey year an incident outcome was reported.
These analyses represent the first characterization of the dose-response relationship between hours worked and CVD as well as one of the few studies of long-term work hour exposure.36–38 Given that a recent study suggested that adding information on work hours to the Framingham risk score improved the predictive power of the model in low-risk working populations,37 future research on the health impacts of work hour durations should focus on improving our understanding of the potential for a threshold of effect of hours worked.
Acknowledgments
Funding:
Funding for this project was received from the National Institute for Occupational Safety and Health (Grant No. 5T42OH008421).
Footnotes
Conflicts of Interest:
None declared.
Contributor Information
Sadie H. Conway, Assistant Professor, University of Texas Health Science Center, School of Public Health, Houston, Texas, USA.
Lisa A. Pompeii, Associate Professor, University of Texas Health Science Center, School of Public Health, Houston, Texas, USA
Robert E. Roberts, Professor, University of Texas Health Science Center, School of Public Health, San Antonio, Texas, USA
Jack L. Follis, Assistant Professor, University of St. Thomas, Houston, Texas, USA
David Gimeno, Associate Professor, University of Texas Health Science Center, School of Public Health, San Antonio, Texas, USA
References
- 1.Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics--2015 update: A report from the American Heart Association. Circulation. 2015;131:e29–322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 2.Heidenreich PA, Trogdon JG, Khavjou OA, et al. Forecasting the future of cardiovascular disease in the united states: A policy statement from the American Heart Association. Circulation. 2011;123:933–944. doi: 10.1161/CIR.0b013e31820a55f5. [DOI] [PubMed] [Google Scholar]
- 3.Cheng Y, Du C, Hwang J, Chen I, Chen M, Su T. Working hours, sleep duration and the risk of acute coronary heart disease: A case–control study of middle-aged men in Taiwan. Int J Cardiol. 2014;171:419–422. doi: 10.1016/j.ijcard.2013.12.035. [DOI] [PubMed] [Google Scholar]
- 4.Spurgeon A, Harrington JM, Cooper CL. Health and safety problems associated with long working hours: A review of the current position. Occup Environ Med. 1997;54:367–375. doi: 10.1136/oem.54.6.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Virtanen M, Ferrie JE, Singh-Manoux A, et al. Overtime work and incident coronary heart disease: The Whitehall II prospective cohort study. Eur Heart J. 2010;31:1737–1744. doi: 10.1093/eurheartj/ehq124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tarumi K, Hagihara A, Morimoto K. A prospective observation of onsets of health defects associated with working hours. Ind Health. 2003;41:101–108. doi: 10.2486/indhealth.41.101. [DOI] [PubMed] [Google Scholar]
- 7.Szerencsi K, van Amelsvoort L, Prins M, Kant I. The prospective relationship between work stressors and cardiovascular disease, using a comprehensive work stressor measure for exposure assessment. Int Arch Occup Environ Health. 2014;87:155–164. doi: 10.1007/s00420-012-0840-y. [DOI] [PubMed] [Google Scholar]
- 8.Bannai A, Tamakoshi A. The association between long working hours and health: A systematic review of epidemiological evidence. Scand J Work Environ Health. 2014;40:5–18. doi: 10.5271/sjweh.3388. [DOI] [PubMed] [Google Scholar]
- 9.Virtanen M, Heikkila K, Jokela M, et al. Long working hours and coronary heart disease: A systematic review and meta-analysis. Am J Epidemiol. 2012;176:586–596. doi: 10.1093/aje/kws139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kivimäki M, et al. Long working hours and risk of coronary heart disease and stroke: A systematic review and meta-analysis of published and unpublished data for 603–838 individuals. Lancet. 2015 Aug 20; doi: 10.1016/S0140-6736(15)60295-1. [DOI] [PubMed] [Google Scholar]
- 11.Sokejima S, Kagamimori S. Working hours as a risk factor for acute myocardial infarction in Japan: Case-control study. BMJ. 1998;317:775–780. doi: 10.1136/bmj.317.7161.775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yoo DH, Kang MY, Paek D, Min B, Cho SI. Effect of long working hours on self-reported hypertension among middle-aged and older wage workers. Ann Occup Environ Med. 2014;26:25-014-0025-0. doi: 10.1186/s40557-014-0025-0. eCollection 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yang H, Schnall PL, Jauregui M, Su TC, Baker D. Work hours and self-reported hypertension among working people in California. Hypertension. 2006;48:744–750. doi: 10.1161/01.HYP.0000238327.41911.52. [DOI] [PubMed] [Google Scholar]
- 14.Kageyama T, Nishikido N, Kobayashi T, Kurokawa Y, Kabuto M. Commuting, overtime, and cardiac autonomic activity in Tokyo. Lancet. 1997;350:639. doi: 10.1016/S0140-6736(05)63328-4. [DOI] [PubMed] [Google Scholar]
- 15.Maruyama S, Morimoto K. Effects of long workhours on life-style, stress and quality of life among intermediate Japanese managers. Scand J Work Environ Health. 1996:353–359. doi: 10.5271/sjweh.153. [DOI] [PubMed] [Google Scholar]
- 16.House JS, Strecher V, Metzner HL, Robbins CA. Occupational stress and health among men and women in the Tecumseh Community Health Study. J Health Soc Behav. 1986:62–77. [PubMed] [Google Scholar]
- 17.Virtanen M, Stansfeld SA, Fuhrer R, Ferrie JE, Kivimäki M. Overtime work as a predictor of major depressive episode: A 5-year follow-up of the Whitehall II study. PloS One. 2012;7:e30719. doi: 10.1371/journal.pone.0030719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kang MY, Park H, Seo JC, et al. Long working hours and cardiovascular disease: A meta-analysis of epidemiologic studies. J Occup Environ Med. 2012;54:532–537. doi: 10.1097/JOM.0b013e31824fe192. [DOI] [PubMed] [Google Scholar]
- 19.University of Michigan Institute for Social Research. PSID: Data on families since 1968. 2014. [Google Scholar]
- 20.McGonagle KA, Schoeni RF, Sastry N, Freedman VA. The Panel Study of Income Dynamics: Overview, recent innovations, and potential for life course research. Longitudinal and Life Course Studies. 2012:3. doi: 10.14301/llcs.v3i2.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.StataCorp LP. STATA Survey Data Reference Manual, Release 13. College Station, Texas: Stata Press; 2013. [Google Scholar]
- 22.Cummings P. Methods for estimating adjusted risk ratios. Stata Journal. 2009;9:175. [Google Scholar]
- 23.Witte JS, Greenland S. A nested approach to evaluating dose-response and trend. Ann Epidemiol. 1997;7:188–193. doi: 10.1016/s1047-2797(96)00159-7. [DOI] [PubMed] [Google Scholar]
- 24.Harrell FE, Jr, Lee KL, Pollock BG. Regression models in clinical studies: Determining relationships between predictors and response. J Natl Cancer Inst. 1988;80:1198–1202. doi: 10.1093/jnci/80.15.1198. [DOI] [PubMed] [Google Scholar]
- 25.Akaike H. Information theory and an extension of the maximum likelihood principle In: , editor. Selected Papers of Hirotugu Akaike. Springer; 1998. pp. 199–213. [Google Scholar]
- 26.Saad L. The “40-hour” workweek is actually longer -- by seven hours: Full-time U.S. workers, on average, report working 47 hours weekly. 2014 [Google Scholar]
- 27.Russek HI, Zohman BL. Relative significance of heredity, diet and occupational stress in coronary heart disease of young adults; based on an analysis of 100 patients between the ages of 25 and 40 years and a similar group of 100 normal control subjects. Am J Med Sci. 1958;235:266–277. doi: 10.1097/00000441-195803000-00003. [DOI] [PubMed] [Google Scholar]
- 28.Greenland S. Dose-response and trend analysis in epidemiology: Alternatives to categorical analysis. Epidemiology. 1995:356–365. doi: 10.1097/00001648-199507000-00005. [DOI] [PubMed] [Google Scholar]
- 29.Greenland S. Methods for epidemiologic analyses of multiple exposures: A review and comparative study of maximum-likelihood, preliminary-testing, and empirical-Bayes regression. Stat Med. 1993;12:717–736. doi: 10.1002/sim.4780120802. [DOI] [PubMed] [Google Scholar]
- 30.International Council on Mining and Metals. Good practice guidance on occupational health risk assessment. 2009 [Google Scholar]
- 31.Desquilbet L, Mariotti F. Dose-response analyses using restricted cubic spline functions in public health research. Stat Med. 2010;29:1037–1057. doi: 10.1002/sim.3841. [DOI] [PubMed] [Google Scholar]
- 32.Okura Y, Urban LH, Mahoney DW, Jacobsen SJ, Rodeheffer RJ. Agreement between self-report questionnaires and medical record data was substantial for diabetes, hypertension, myocardial infarction and stroke but not for heart failure. J Clin Epidemiol. 2004;57:1096–1103. doi: 10.1016/j.jclinepi.2004.04.005. [DOI] [PubMed] [Google Scholar]
- 33.Kehoe R, Wu SY, Leske MC, Chylack LT., Jr Comparing self-reported and physician-reported medical history. Am J Epidemiol. 1994;139:813–818. doi: 10.1093/oxfordjournals.aje.a117078. [DOI] [PubMed] [Google Scholar]
- 34.Paganini-Hill A, Chao A. Accuracy of recall of hip fracture, heart attack, and cancer: A comparison of postal survey data and medical records. Am J Epidemiol. 1993;138:101–106. doi: 10.1093/oxfordjournals.aje.a116832. [DOI] [PubMed] [Google Scholar]
- 35.Bound J, Brown CC, Duncan G, Rodgers WL. Measurement Error in Cross-Sectional and Longitudinal Labor Market Surveys: Results from Two Validation Studies. 1989 [Google Scholar]
- 36.Holtermann A, Mortensen OS, Burr H, Sogaard K, Gyntelberg F, Suadicani P. Long work hours and physical fitness: 30-year risk of ischaemic heart disease and all-cause mortality among middle-aged Caucasian men. Heart. 2010;96:1638–1644. doi: 10.1136/hrt.2010.197145. [DOI] [PubMed] [Google Scholar]
- 37.Kivimäki M, Batty GD, Hamer M, et al. Using additional information on working hours to predict coronary heart disease: A cohort study. Ann Intern Med. 2011;154:457–463. doi: 10.1059/0003-4819-154-7-201104050-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Netterstrøm B, Kristensen T, Jensen G, Schnor P. Is the demand-control model still a usefull tool to assess work-related psychosocial risk for ischemic heart disease? Results from 14 year follow up in the Copenhagen City Heart Study. Int J Occup Med Environ Health. 2010;23:217–224. doi: 10.2478/v10001-010-0031-6. [DOI] [PubMed] [Google Scholar]