Abstract
Risk-level drinking, drinking and driving, and alcohol-related violence are risk factors that result in injuries. The current study sought to identify which subgroups of patients experience the most behavioral change following a brief intervention. A secondary analysis of data from a brief alcohol intervention study was conducted. The sample (N=664) includes at-risk drinkers who experienced an injury and were admitted for care to a Level-1 trauma center. Injury-related items from the Short Inventory of Problems+6 were used to perform a latent transition analysis to describe class transitions participants experienced following discharge. Four classes emerged for the year before and after the current injury. Most individuals transitioned from higher risk classes into those with lower risk. Some participants maintained risky profiles, and others increased risks and consequences. Drinking and driving remained a persistent problem among study participants. Although a large portion of intervention recipients improved risks and consequences of alcohol use following discharge, more intensive intervention services may be needed for a subset of patients who showed little or no improvement.
Keywords: Screening and brief intervention, alcohol, injury, latent transition analysis
Introduction
Alcohol and Injury
Drinking at or above risk levels defined by the National Institute on Alcohol Abuse and Alcoholism (NIAAA, i.e., men: ≥5 drinks/day or ≥15 drinks/week; women: ≥4 drinks/day or ≥8 drinks/week)1 is the primary risk factor for injury in the US2 and is a major predictor of emergency3 and trauma care.4 In addition to risky drinking and injury, drinking and driving is a major contributor to non-fatal injury and is a significant predictor of injury cases admitted to trauma centers.5, 6 Nearly one-third of motor vehicle crashes involving alcohol result in injury.7 Alcohol use and violence are also primary predictors of injury.8–13 Violent offenses are often perpetrated by intoxicated individuals or are perpetrated on individuals who have been drinking.10, 14 Injury related risk behaviors, commonly associated with drinking, significantly contribute to the impact of alcohol use on public health.
Most people with alcohol use disorders do not receive help.15 In specific terms, roughly 90 percent of individuals in the US who needed treatment in 2008 for alcohol problems did not receive care.15 Screening and brief intervention (SBI) has been developed and tested in an effort to reduce alcohol-related injury or prevent their reoccurrence. SBI for injured individuals has been shown to reduce drinking,16–20 injury,21 drinking and driving,22 and drunk driving arrests.23 SBI for injured patients has also been demonstrated to increase the numbers of individuals who seek treatment for alcohol problems.20, 24 Research also indicates, however, that SBI does not clearly help all injured patients. Some studies have shown no significant changes in alcohol use reduction,25–28 alcohol-related adverse driving events,29–31 or future injury.32 Meta-analyses and systematic reviews of SBI for injured patients have also reported mixed results for the efficacy of SBI among injured patients.33–35
Analytical Advancement
In light of the mixed evidence for the effectiveness of SBI among injured patients, it may be helpful to extend the field’s current understanding regarding which intervention recipients experience the greatest change following discharge. Some secondary analyses have demonstrated promise for identifying how SBI can help specific subgroups of individuals;36–40 though, these analyses often do not capture the complex nature of alcohol-related injury and associated behaviors. It is evident from the literature that risk level alcohol use, drinking and driving, and alcohol-related violence have some interrelationship in often times lead to the need for injury care. What is not clear is how these behavioral factors for injury patients who receive SBI may combine to form patient profiles and if individuals with different profiles improve or worsen over time.
A potentially more complete approach for understanding changes among those receiving SBI is latent variable statistical modeling; that is to say, statistical models that work to identify unseen or unobserved constructs by combining a set of indicator variables.41–43 A method of latent variable modeling that could be especially helpful in the analysis and interpretation of findings from SBI studies is mixture modeling. Mixtures are used to draw out latent (or unobserved) subgroups or “classes” of individuals that exist within the data based on multiple indicators43, 44 and then capture changes that transpire among those groups across time.45, 46 The purpose of this secondary analysis was to develop longitudinal injury-related consequence and risk behavior profiles based on seven items from the Short Inventory of Problems (SIP)+6,47 and then to assess the changes patients with the different profiles experienced following the receipt of a brief alcohol intervention and discharge from a trauma center. The findings herein provide a clearer picture of the combination of risks and consequences individuals experience and then depict what changes in those behaviors are manifest across time.
Materials and Methods
Data Source
Data from a SBI randomized clinical trial conducted in a Level-1 trauma department were used in this project (NIAAA, R01 013824). The consort chart, specific methods of participant recruitment, and detailed descriptions of experimental and control conditions for this trial have been reported elsewhere.32, 48 All study participants were adults (≥18 years) who suffered a traumatic injury, were admitted to a Level-1 trauma center, and screened positive for risk-level drinking. Specifically, patients recruited for participation in the study had a clinical indication of intoxication upon admission to the trauma center (but not intoxicated at the time of recruitment), reported drinking six hours before the injury event, reported drinking at NIAAA risk levels,1 or responded positively to one or more items of the CAGE.49, 50 Informed consent was obtained from participants according to procedures approved by the university and medical center Institutional Review Boards. Following consent, participants were assigned to receive a brief motivational intervention or treatment as usual. The brief intervention consisted of a 15–30 minute brief motivational interviewing session between patients and study interventionists, and treatment as usual included patients receiving information only. This dataset contains 1,493 cases and includes self-reported information from baseline, six-, and 12-month assessments regarding alcohol use and alcohol risk information. The sample is comprised of 1,231 men and 262 women, of whom 668 are White, 288 are Black, and 537 are Hispanic. Follow up rates in this study have been reported elsewhere and are comparable to other brief intervention clinical trials.48
The main outcomes from the original trial found time effects for alcohol use48 among both groups and significant interaction effects for reductions in drinking among Hispanics48 and those dependent on alcohol.37 Data from the experimental group only were used in the present study because the intent of the current project was to conduct a descriptive longitudinal analysis of transitions among individual behavioral profiles based on injury-related consequence and risks of risk-level drinking for those participants who received SBI. In other words—the purpose of this project was to describe if individual intervention recipients’ profiles improved, stayed the same, or worsened following discharge from the trauma center.
Model and Analytic Approach
The specific mixture modeling approach selected for this project was latent transition analysis (LTA).45, 46, 51 LTA models are longitudinal applications of cross-sectional latent class analyses (LCA). LCAs are statistical models that identify unique subgroups or profiles based on similar responses to variables from within a single population of individuals.44, 45, 52, 53 LTA was selected as the analytical approach for this project in order to describe the transition patterns between latent classes of intervention recipients from the year before and after participants current injury admission and discharge. The LTA carried out in this project followed modeling building procedures outlined in the literature53,54,59 by first establishing cross-sectional LCAs of injury-related risks and consequences at the two different time points and then incorporating those models into a single LTA model.
The first LCA model depicts subclasses of participant injury-related risks and consequences assessed at baseline of the SBI study. Specifically, this baseline model depicts participants’ risks and consequences profiles in the year prior to admission to the trauma center. The second LCA model depicts participants’ profiles based on the 12-month follow up assessment and includes the same risks and consequences captured in the first model, but for the year after discharge. These cross-sectional latent class models were established using the Akaike Information Criterion (AIC), Adjusted Bayesian Information Criterion (ABIC), and Bootstrapped Likelihood Ratio Test (BLRT).46, 51, 54 Following the establishment of the cross-sectional LCAs, these models were combined into a single LTA longitudinal model to examine if transitions between behavioral profiles occurred (i.e., if individuals who were categorized within a class at time-one transitioned into another class at time-two).
Models parameters for the LTA were freely estimated, without imposing full or partial model constraints.45, 46 Imposing parameter constraints forces profiles to take on specific attributes. In the current analysis, for instance, imposing full constraints on the time-two model based on information from the time-one model would cause the classes from the both models to exactly mirror one another. The decision to allow the classes to estimate freely in the current analysis was based on the assessment of differences in the classes46 at time-one compared to time-two. The free estimation of parameter values was judged for this LTA to have the ability to represent the most accurate changes among study participants by not forcing profiles and transitions to fit specific requirements. All analyses were conducted using Mplus 6.55 In addition to the latent models developed and tested, descriptive analyses of participant demographic characteristics were calculated using IBM SPSS 1956 and are reported.
Variables and Sample Size
Table 1 contains the variables utilized in the cross-sectional measurement models. Items from the SIP+6 were selected for analysis in this study.47,57 The seven items selected from the SIP+6 are the injury-related risks consequences of risk-level drinking that are among those identified factors that lead to emergency and trauma care.28, 58, 59 Each of the seven items were yes (coded as 1) and no (coded as 0) statements, indicating the participants had participated in the behavior or not. The time periods measured the 12-month period prior to patients’ current trauma center admission and 12 months after discharge. For the 12 months previous to the injury admission, the Cronbach’s alpha for the seven indicators was 0.84, and for the 12 months following discharge, the alpha was 0.70. Validity of these seven items has not been specifically examined. However, previous research has established validity and reliability for the full measure containing all items from the SIP+6.60
Table 1.
Observed indicators from 12 months before and after SBI
| Observed Indicator |
|---|
| I have driven a motor vehicle after having three or more drinks (SIP+6) |
| I have taken foolish risks when I have been drinking (SIP) |
| I have gotten into a physical fight while drinking (SIP+6) |
| I have been arrested for driving under the influence of alcohol (SIP+6) |
| I have had an accident while drinking or intoxicated (SIP) |
| While drinking or intoxicated, I have been physically hurt, injured or burned (SIP+6) |
| While drinking or intoxicated, I have injured someone else (SIP+6) |
In terms of number of cases required to adequately power the model estimated, a standard convention for latent variable modeling with multiple time points suggests approximately five to ten cases per parameter estimated.61 The LTA in the current project contains 71 parameters. Therefore, the current sample (N=664) contains sufficient cases for model estimation.
Results
Study Sample and Characteristics
The total number of participants who were assigned to the intervention group at baseline was 737. However, due to attrition at follow up in the parent study, 73 participants were missing all data in the combined six- and 12-month follow up assessments. Therefore, 664 participants were included in the current LTA. These participants were mostly males (n=571, 86%), and their average age was 33 years (SD=11.5). Whites were the largest racial/ethnic group (n=303, 45.6%) followed by Hispanic (n=228, 34.3%) and Black (n=133, 20%, 20.1%) participants. Approximately one-third of participants were married (n=188, 28.3%), had a high school diploma/GED (n=241, 36.3%) or some high school education (n=245, 36.9%), and were not employed (n=211, 31.8%). Most injuries participants sustained were unintentional (n=522, 78.6%), and participants reported heavy drinking an average of 62 percent of days in the previous year (SD=0.4), with an average maximum amount consumed of 14 (SD=10.9) standard drinks (about 0.6 fluid ounces of pure alcohol, e.g. one 12 ounces of beer or 5 ounces of table wine).
Proportional and mean difference tests (results not shown) were conducted to examine whether demographic characteristics for participants assigned to receive the intervention at baseline (N=737) and those participants who were included in the present LTA (N=664) differed significantly. Similar to the significant follow up differences reported in the main outcomes paper of the parent study by Field et al.,48 Hispanic (standardized residual=1.8) participants included in the LTA were more likely (χ2=6.9, df=2, p=0.04) to have not completed the follow ups compared to White (standardized residual = −1.6) and Black (standardized residual =0.1) participants. No other significant differences emerged between participants who received the intervention at baseline and those included in the current study.
Classes and Conditional Item Probabilities
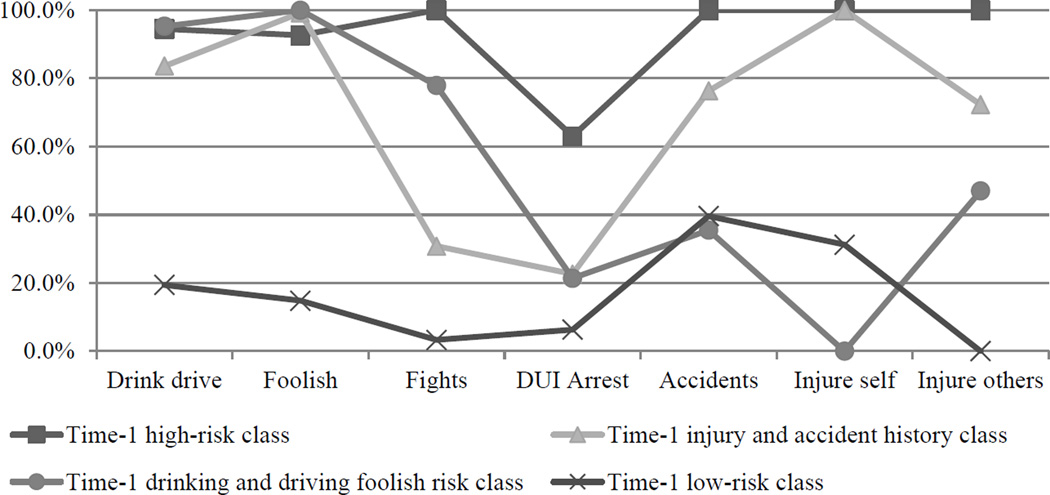
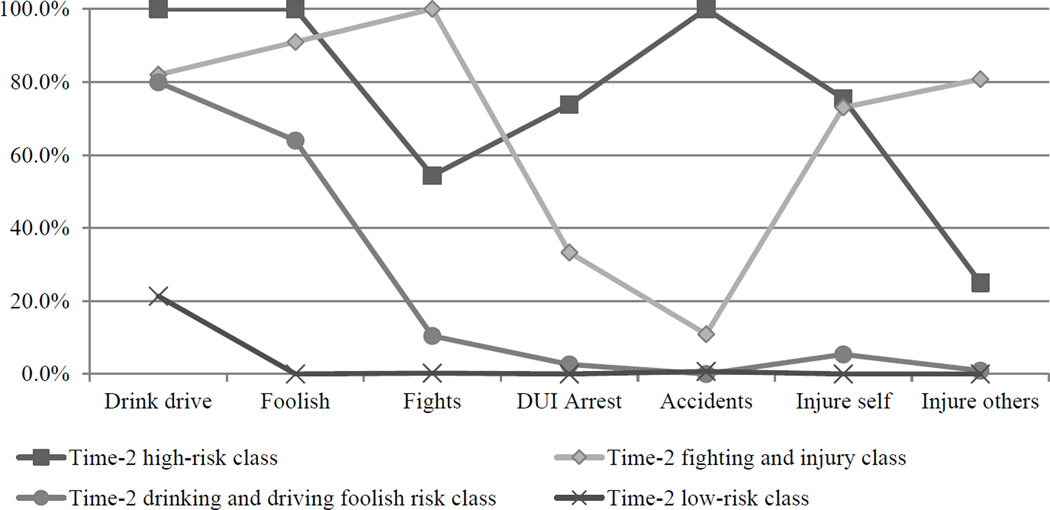
Four classes of participants were identified in the year before the current injury and in the year after the current injury (see Table 2). Figures 1 and 2 plot the conditional item probabilities for each time point for the four class solutions. The four classes for time-one were labeled: time-1 high-risk, time-1 injury and accident history, time-1 drinking and driving foolish risk, and time-1 low-risk class. The classes for time-two were labeled: time-2 high-risk class, time-2 fighting and injury, time-2 drinking and driving foolish risk, and time-2 low-risk (Class labels are the authors’ attempts at describing the class characteristics using the minimum amount of words; as a result, these labels may be somewhat subjective).
Table 2.
Numbers of classes identified from data
| 12 months before SBI | ||||
| Classes | AIC | ABIC | BLRT | |
| 2 | 1749.87 | 1768.11 | 0.00 | |
| 3 | 1736.90 | 1764.86 | 0.00 | |
| 4 | 1735.18 | 1772.86 | 0.02 | |
| 5 | 1742.55 | 1789.95 | 0.37 | |
| 12 months after SBI | ||||
| 2 | 1472.35 | 1483.82 | 0.00 | |
| 3 | 1433.99 | 1451.58 | 0.00 | |
| 4 | 1423.86 | 1447.56 | 0.00 | |
| 5 | 1429.73 | 1459.56 | 0.50 | |
Figure 1.
Conditional item probabilities for four class solution one year before SBI
Figure 2.
Conditional item probabilities for four class solution one year after SBI
Year Prior to Injury
Figure 1 contains the class profiles for the year prior to the injury. The first class is labeled the time-1 high-risk class. This class contains 341 individuals (51.3%) and represents the group with the highest probabilities of endorsing each of the seven SIP+6 items. All time-1 high-risk class members endorsed four of the seven items at 100 percent; the item with the lowest probability of endorsement in the time-1 high-risk class was drunk driving arrests, with a 63 percent probability of endorsement. The second class is labeled the time-1 injury and accident history class. This class contains 143 (21.5%) individuals. All 143 members had injured themselves while drinking in the year before their current injury admission, and they were the second most likely of any class to have experienced an accident (76.3%) and to have injured others (72.3%). The third class is labeled the time-1 drinking and driving foolish risk class. This class contains 25 individuals (4%). Nearly all class members had driven after drinking (95.3%); all had done foolish things while drinking, and over three-quarters had been in fights (77.9%). The last class was labeled the time-1 low-risk class. This class included 155 (23.3%) individuals. These study participants had the lowest probabilities of endorsements of each of the seven SIP+6 items compared to the other classes, with having an accident (39.6%) being the highest item probability in the class.
Year after Injury
Figure 2 contains the class profiles for the year following the injury and discharge from the trauma center (although the following class labels possess some overlap between the year prior to and after the injury, the labels are not intended to imply that the classes are exactly similar in constitution). The first class is labeled the time-2 high-risk class. This class contains 22 individuals (3.3%). The time-2 high-risk class of individuals contained the highest probabilities of item endorsement, with all class members endorsing three items at 100 percent; the lowest probability of item endorsement in class time-2 high-risk class was injuring others, at 25 percent. The second class was labeled the time-2 fighting and injury class. This class contains 23 study participants (3.4%). All members of this class had been in fights while drinking, and this class had the highest probability of injuring others (80.8%) and the second highest probability of injuring self (73%). The third class was labeled the time-2 drinking and driving foolish risk class. This class contains 359 individuals (54.1%). This class was primarily characterized by drinking and driving (79.9%) and doing foolish things while drinking (64%). The fourth class was labeled the time-2 low-risk class. This class contains 260 individuals (39.2%), with most individuals endorsing none of the risk consequences except for drinking and driving, which had a 21.3 percent probability of endorsement.
Transitions
As is shown in Table 3, the largest number of participants who transitioned from one profile to another were those 310 individuals who moved from the time-1 high-risk class into the time-2 drinking and driving foolish risk class (a class with some of the lowest risk at time-two with the exception of drinking and driving and foolish risks while drinking). Another transition for the time-1 high-risk class included members transitioning into the time-2 high-risk class (4.4% n=15) and the time-2 fighting and injury class (4.4% n=15). Nearly all individuals in the time-1 injury and accident history class moved to the time-2 low-risk class (94.4%; n=135). Individuals in the time-1 injury and accident history class also transitioned into the time-2 high-risk class (4.2%, n=6) and time-2 fighting and injury class (1.4%, n=2). The only transition that occurred for the time-1 drinking and driving foolish risk class was that each of these participants moved into the time-2 drinking and driving foolish risk class. Members of the time-1 low-risk class transitioned into the time-2 low-risk class (80%, n=124), the time-2 fighting and injury class (3.9%, n=6), and the time-2 drinking and driving foolish risk (15.5%, n=24).
Table 3.
Percent of classes transitioning (total individuals in transition class)
| Year following injury and intervention classes | ||||
|---|---|---|---|---|
| Baseline classes | Time-2 high risk |
Time-2 fighting and injury class |
Time-2 drinking and driving foolish risk |
Time-2 low risk |
| Time-1 high risk | 4.4% (15) | 4.4% (15) | 90.9% (310) | 0.3% (1) |
| Time-1 injury and accident history | 4.2% (6) | 1.4% (2) | 0% (0) | 94.4% (135) |
| Time-1 drinking and driving foolish risk | 0.0% (0) | 0.0% (0) | 100% (25) | 0.0% (0) |
| Time-1 low risk | 0.6% (1) | 3.9% (6) | 15.5% (24) | 80.0% (124) |
Discussion
The results of this latent transition analysis demonstrated that four groups of individuals experienced injury-related risks and consequences of risk-level drinking in the year before and the year following their current injury and intervention. This study also demonstrated many individuals transition from baseline classifications into other groups across time—with most transitions appearing to be in many respects positive. Such transitions represent positive patient improvement that could be the base of reinforcement within intervention sessions aimed at encouraging additional change and improvement. Nevertheless, other transitions demonstrated marginal improvement and indicate possibly needed future research examine methods to enhance more positive transitions.
The results of this study possibly illuminate previously reported mixed findings of SBI studies. For instance, time-1 low risk participants either stayed low risk or became worse at time-two. While remaining low risk is desirable, such transitions raise potential questions regarding whether low risk groups who remain low risk possibly washout treatment effects in clinical studies. Future research should compare the influence of these latent classes and transitions in relation to participants in control conditions.
The findings herein also appear to be consistent with those previously reported that have demonstrated individuals with higher levels of alcohol use severity make substantial changes following the receipt of a brief intervention.37 Indeed, while some studies have struggled to identify clear improvements for alcohol use among injured populations,28 the combination of alcohol-related risks and consequences may better describe the constellation of changes individuals experience following an injury and SBI. However, the current application of latent transition analysis is new to the SBI field, and therefore, the results of this secondary analysis are provisional and require further replication in order to substantiate its findings. Such replications would provide important evidence to support the reliability of the results of this study.
Translation into Practice via EHR
This study provides a first glimpse into the classes that exist among a sample of injured patients who drink at risk levels. If future research can replicate the findings herein with extensions to models that better examine and explain potential causal relationships, clinical applications of how to actually determine classes at the bedside would be important. Both the Affordable Care Act and the HITECH legislation include important mandates that direct the establishment and integration of electronic health records (EHR) into practice in order to coordinate, facilitate, and improve patient care.62–64 It is in such a record keeping environment that mixture model algorithms (such as those used in the current LTA) could be imbedded so as to provide class assignment output to clinicians following the entry into an EHR system of patient responses to the seven items used in this analysis. Further, information systems like the National Trauma Data Bank65 could also be adapted to interface with EHRs and provide a nationally representative sample of profiles to providers within clinical settings. In addition to class assignment, personalized feedback could also be provided as part of output delivered to clinicians for patients. Personalized feedback based on transition probabilities could guide providers to tailor interventions to include topics such as drinking and driving and/or warning of possible continued or increased risk.
Drinking and Driving
A majority of patients nearly eliminated DUI arrests in the year after discharge. This result appears to be consistent with findings from previous studies that have also documented improvements in drinking and driving-related arrests following SBI.23, 66 Furthermore, both Monti et a.l22 and Runge et al.24 have previously reported that individuals who experienced car crashes and subsequently received care in an emergency or trauma settings experience significant improvements following SBI. While the current study does not include car crashes as an indicator, the findings herein possibly support these previous studies and suggest that future research should include alcohol-related car crashes as a profile indicator that is likely influential in class membership and class transitions across time.
However, despite the improvement noted in the current study for drinking and driving arrests and possible future directions for research for motor vehicle crashes, a large portion of the current study participants reported driving after consuming three or more drinks in the year following their discharge from the trauma center. Given the lethal potential for drinking and driving, further research is needed to elucidate why DUI arrests appear to improve but drinking and driving remains problematic. However, regardless of why differences between DUI arrests and drinking and driving episodes may exist, clinicians delivering SBI may nevertheless consider a universal inclusion of drinking and driving as a part of intervention sessions with patients. Some limited drinking and driving messaging already exists within SBI guides produced by the American College of Surgeons as well as the American Public Health Association.67, 68 If drinking and driving messaging becomes standard in SBI guides and practice, future episodes possibly may be prevented.
Limitations
Strengths of this study include the new application of LTA modeling to brief intervention analysis and the identification of previously unknown subgroups of patients and their improvements following the receipt of SBI. In spite of these strengths, the parent trial upon which the current project was based was not designed to answer the specific questions addressed in this secondary analysis. Given this novel application of LTA in a secondary analysis, classes and transition probabilities were allowed to estimate freely. Though this approach provides the clearest statistical picture of changes among injury-related risks and consequences classes, class transitions and conditional item probabilities are more difficult to interpret as they are not uniform across time. Future analyses may benefit from using information from the present or similar studies in examining models for which some level of invariance is imposed to increase uniformity and facilitate interpretation of results. Aside from possible challenges in analysis and interpretation, three of the classes that emerged from the data were relatively small in size, ranging from 3.3 to 4 percent of the sample. These smaller classes raise the question of whether these groups are artifacts of the analysis or true subgroupings. Replication of the current study would alleviate this uncertainty. However, given the fact that two of these smaller classes were groups at time two with higher levels of risk, these small class sizes may represent positive findings of desired behavior changes among patients.
Conclusion
Exceeding NIAAA risk drinking guidelines, driving under the influence of alcohol, and alcohol-related violence are among the primary risk factors that result in injuries that require medical care in the nation’s emergency and trauma centers. It is not clear from the extant research literature which individuals make positive changes following the receipt of brief interventions. The current study sought to identify which groups of individuals experience the most behavioral change following a brief intervention. The LTA conducted in this study demonstrated that four subclasses of participants could be identified in the year before and the year after the intervention based on injury-related risks and consequences classes.
Most individuals transitioned from classes with higher endorsements of injury-related risk and consequences into classes with lower endorsements. Nevertheless, drinking and driving remains a persistent issue in the year following the SBI service delivery. Replications of these findings could provide the necessary support for accreditation or practice level enhancements to deliver specific drinking and driving information to patients. Additionally, some transition classes experienced little or no positive change from time-one to time-two. Future research should focus on how to better service those whose behavioral profiles do not improve following SBI services and discharge. Such evidence can be used to likewise improve accreditation standards and service delivery for injured patients who drink at risk levels.
Implications for Behavioral Health
Trauma centers are among the key locations for the delivery of SBI for injured individuals who exceed risk-drinking thresholds. However, these locations are often among those that struggle with financial viability.69–71 Furthermore, the research evidence is not clear regarding which injured patients benefit the most from SBI services. Therefore, limited behavioral health resources are being delivered without a clear understanding patient benefit. The findings of this paper suggest that specific subgroups of patients exist who receive SBI, and some of those subgroups improve more than others. Possessing a clearer understanding of which patients improve to the greatest extent following discharge stands to improve patient care and costs for health systems.
Acknowledgments
This secondary analysis was supported by grant number 1R36HS021394from the Agency for Healthcare Research and Quality. The data used for this study was collected in a study funded by the National Institute on Alcohol Abuse and Alcoholism: R01013824 and Clinical Trials Registry: NCT00132262. These funding sources did not have input into the design, execution, interpretation, or write-up of this study.
The work for this secondary data analysis was conducted at The University of Texas at Austin, the UT School of Public Health, and the Johns Hopkins School of Medicine. The original screening and brief intervention clinical study was conducted at Parkland Hospital in Dallas, TX.
Footnotes
Conflicts of Interests
None
Contributor Information
Gerald Cochran, Email: jcochran@jhu.edu, Johns Hopkins University School of Medicine, Department of Psychiatry and Behavioral Sciences, Behavioral Pharmacology Research Unit, 5510 Nathan Shock Drive, Baltimore, MD 21224, USA, Phone: (410) 550-6756, Fax: (410) 550-0030.
Craig Field, The University of Texas at Austin, School of Social Work, Health Behavior Research and Training Institute, 1717 West 6th St. Ste. 295, Austin TX, 78703.
Raul Caetano, Dallas Regional Campus, UT School of Public Health, 5323 Harry Hines Blvd., Dallas, Texas 75390
References
- 1.National Institute on Alcohol Abuse and Alcoholism. Helping patients who drink too much: A clinicians guide. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2007. [Google Scholar]
- 2.Centers for Disease Control and Prevention. Injury prevention & control: Injury response alcohol screening. Atlanta, GA: Centers for Disease Control and Prevention; 2010. [Google Scholar]
- 3.Cherpitel CJ, Ye Y. Drug use and problem drinking associated with primary care and emergency room utilization in the US general population: Data from the 2005 national alcohol survey. Drug and Alcohol Dependence. 2008;97:226–230. doi: 10.1016/j.drugalcdep.2008.03.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.MacLeod JBA, Hungerford DW. Alcohol-related injury visits: Do we know the true prevalence in U.S. trauma centres? Injury. 2010;41:847–851. doi: 10.1016/j.injury.2010.01.098. [DOI] [PubMed] [Google Scholar]
- 5.National Trauma Data Bank. National Trauma Data Bank annual report. Chicago, IL: American College of Surgeons; 2011. [Google Scholar]
- 6.Stoduto G, Vingilis E, Kapur BM, et al. Alcohol and drug use among motor vehicle collision victims admitted to a regional trauma unit: demographic, injury, and crash characteristics. Accident Analalysis and Prevention. 1993;25:411–420. doi: 10.1016/0001-4575(93)90070-d. [DOI] [PubMed] [Google Scholar]
- 7.National Highway Traffic Safety Administration. Traffic safety facts: 2009 data; Alcohol-impaired drivers involved in fatal crashes, by gender and state, 2007–2008. Washington, DC: NHTSA’s National Center for Statistics and Analysis; 2009. [Google Scholar]
- 8.Field C, Claassen C, O'Keefe G. Association of alcohol use and other high-risk behaviors among trauma patients. Journal of Trauma. 2001;50:13–19. doi: 10.1097/00005373-200101000-00002. [DOI] [PubMed] [Google Scholar]
- 9.Field C, O'Keefe G. Behavioral and psychological risk factors for traumatic injury. Journal of Emergency Medicine. 2004;26:27. doi: 10.1016/j.jemermed.2003.04.004. [DOI] [PubMed] [Google Scholar]
- 10.Collins JJ, Messerschmidt PM. Epidemiology of alcohol-related violence. Alcohol Health & Research World. 1993;17:93–100. [Google Scholar]
- 11.Macdonald S, Cherpitel CJ, Borges G, et al. The criteria for causation of alcohol in violent injuries based on emergency room data from six countries. Addictive Behaviors. 2005;30:103–113. doi: 10.1016/j.addbeh.2004.04.016. [DOI] [PubMed] [Google Scholar]
- 12.Brewer RD, Swahn MH. Binge Drinking and Violence. Journal of the American Medical Association. 2005;294:616–617. doi: 10.1001/jama.294.5.616. [DOI] [PubMed] [Google Scholar]
- 13.Cherpitel CJ. Alcohol and violence-related injuries: an emergency room study. Addiction. 1993;88:79–88. doi: 10.1111/j.1360-0443.1993.tb02765.x. [DOI] [PubMed] [Google Scholar]
- 14.Bureau of Justice Statistics. Victims who percieved offenders had been using alcohol, by type of crime, 1997–2008. Washington, DC: Bureau of Justice Statistics; 2010. Alcohol And Crime: Data from 2002 To 2008, Appendix table 1. [Google Scholar]
- 15.Substance Abuse and Mental Health Services Administration. Results from the 2010 National Survey on Drug Use and Health: National findings. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2009. [Google Scholar]
- 16.Antti-Poika I, Karaharju E, Roine RP, et al. Intervention of heavy drinking: A prospective and controlled study of 438 consecutive injured male patients. Alcohol and Alcoholism. 1988;23:115–121. [PubMed] [Google Scholar]
- 17.Bazargan-Hejazi S, Bing E, Bazargan M, et al. Evaluation of a brief intervention in an inner-city emergency department. Annals of Emergency Medicine. 2005;46:67–76. doi: 10.1016/j.annemergmed.2004.10.014. [DOI] [PubMed] [Google Scholar]
- 18.Gentilello L, Rivara F, Donovan D, et al. Alcohol interventions in a trauma center as a means of reducing the risk of injury recurrence. Annals of Surgery. 1999;230:473–480. doi: 10.1097/00000658-199910000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Haque A, Helmkamp J, Hungerford D, et al. Brief intervention for alcohol problems in a university hospital emergency department: a randomized controlled trial. Annals of Epidemiology. 2003;13:573. [Google Scholar]
- 20.Neumann T, Neuner B, Weiss-Gerlach E, et al. The effect of computerized tailored brief advice on at-risk drinking in subcritically injured trauma patients. Journal of Trauma. 2006;61:805–814. doi: 10.1097/01.ta.0000196399.29893.52. [DOI] [PubMed] [Google Scholar]
- 21.Dinh-Zarr T, Goss C, Heitman E, et al. Action with problem drinkers can cut risk of injury. Cochrane Database of Systematic Reviews. 2009 [Google Scholar]
- 22.Monti PM, Colby SM, Barnett NP, et al. Brief intervention for harm reduction with alcohol-positive older adolescents in a hospital emergency department. Journal of Consulting and Clinical Psychology. 1999;67:989–994. doi: 10.1037//0022-006x.67.6.989. [DOI] [PubMed] [Google Scholar]
- 23.Schermer CR, Moyers TB, Miller WR, et al. Trauma center brief interventions for alcohol disorders decrease subsequent driving under the influence arrests. Journal of Trauma. 2006;60:29–34. doi: 10.1097/01.ta.0000199420.12322.5d. [DOI] [PubMed] [Google Scholar]
- 24.Runge JW, Garrison H, Hall W, et al. Identification and referral of impaired frivers through emergency department protocols. Washington, DC: U.S. Department of Transportation; 2002. [Google Scholar]
- 25.Daeppen J-B, Gaume J, Bady P, et al. Brief alcohol intervention and alcohol assessment do not influence alcohol use in injured patients treated in the emergency department: a randomized controlled clinical trial. Addiction. 2007;102:1224–1233. doi: 10.1111/j.1360-0443.2007.01869.x. [DOI] [PubMed] [Google Scholar]
- 26.Dauer AR-M, Rubio ES, Gomez XM, et al. Early identification and brief intervention in alcohol-related traffic casualties: Preliminary results. Adicciones. 2003;15:191–202. [Google Scholar]
- 27.Dauer AR-M, Rubio ES, Coris ME, et al. Breif intervention in alcohol-postive traffic casualties: Is it worth the effort? Alcohol and Alcoholism. 2006;41:76–83. doi: 10.1093/alcalc/agh241. [DOI] [PubMed] [Google Scholar]
- 28.Soderstrom CA, Diclemente CC, Dischinger PC, et al. A controlled trial of brief intervention versus brief advice for at-risk drinking trauma center patients. Journal of Trauma. 2007;62:1102–1112. doi: 10.1097/TA.0b013e31804bdb26. [DOI] [PubMed] [Google Scholar]
- 29.Crawford MJ, Patton R, Touquet R, et al. Screening and referral for brief intervention of alcohol-misusing patients in an emergency department: a pragmatic randomised controlled trial. Lancet. 2004;364:1334–1339. doi: 10.1016/S0140-6736(04)17190-0. [DOI] [PubMed] [Google Scholar]
- 30.D'Onofrio G, Pantalon MV, Degutis LC, et al. Brief intervention for hazardous and harmful drinkers in the emergency department. Annals of Emergency Medicine. 2008;51:742–750. doi: 10.1016/j.annemergmed.2007.11.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sommers MS, Dyehous JM, Howe SR, et al. Effectiveness of brief interventions after alcohol-related vehicular injury: A randomized controlled trial. Journal of Trauma. 2006;61:523–533. doi: 10.1097/01.ta.0000221756.67126.91. [DOI] [PubMed] [Google Scholar]
- 32.Roudsari B, Caetano R, Frankowski R, et al. Do minority or white patients respond to brief alcohol intervention in trauma centers? A randomized trial. Annals of Emergency Medicine. 2009;54:285–293. doi: 10.1016/j.annemergmed.2009.01.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Daeppen J. A meta-analysis of brief alcohol interventions in emergency departments: few answers, many questions. Addiction. 2008;103:377–378. [Google Scholar]
- 34.Havard A, Shakeshaft A, Sanson-Fisher R. Systematic review and meta-analyses of strategies targeting alcohol problems in emergency departments: interventions reduce alcohol-related injuries. Addiction. 2008;103:368–376. doi: 10.1111/j.1360-0443.2007.02072.x. [DOI] [PubMed] [Google Scholar]
- 35.Nilsen P, Baird J, Mello M, et al. A systematic review of emergency care brief alcohol interventions for injury patients. Journal of Substance Abuse Treatment. 2008;35:184–201. doi: 10.1016/j.jsat.2007.09.008. [DOI] [PubMed] [Google Scholar]
- 36.Barnett NP, Apodaca TR, Magill M, et al. Moderators and mediators of two brief interventions for alcohol in the emergency department. Addiction. 2010;105:452–465. doi: 10.1111/j.1360-0443.2009.02814.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Field C, Caetano R. The effectiveness of brief intervention among injured patients with alcohol dependence: who benefits from brief interventions? Drug and Alcohol Dependence. 2010;111:13–20. doi: 10.1016/j.drugalcdep.2009.11.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mello MJ, Nirenberg TD, Longabaugh R, et al. Emergency department brief motivational interventions for alcohol with motor vehicle crash patients. Annals of Emergency Medicine. 2005;45:620–625. doi: 10.1016/j.annemergmed.2005.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Walton MA, Goldstein AL, Chermack ST, et al. Brief alcohol intervention in the emergency department: moderators of effectiveness. Journal of Studies on Alcohol and Drugs. 2008;69:550–560. doi: 10.15288/jsad.2008.69.550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lin JC, Karno MP, Lingqi T, et al. Do health educator telephone calls reduce at-risk drinking among older adults in primary care? Journal of General Internal Medicine. 2010;25:334–339. doi: 10.1007/s11606-009-1223-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Collins LM. Latent class and latent transition analysis: With applications in the social, behavioral, and health sciences. Hoboken: John Wiley & Sons, Inc.; 2010. [Google Scholar]
- 42.Kline RB. Principles and Practice of Structural Equation Modeling. 3rd. New York: Guilford Publications, Inc.; 2010. [Google Scholar]
- 43.Lee J. The Epistemology of mathematical and statistical modeling: A quiet methodological revolution. American Psychologist. 2010;65:1–12. doi: 10.1037/a0018326. [DOI] [PubMed] [Google Scholar]
- 44.McCutcheon AL. Latent class analysis. Newbury Park: Sage Publications; 1987. [Google Scholar]
- 45.Collins L, Lanza S. Latent class and latent transition analysis: With applications in the social, behavioral, and health sciences. Hoboken: John Wiley & Sons, Inc.; 2010. [Google Scholar]
- 46.Nylund KL. Latent transition analysis: Modeling extensions and an application to peer victimization. Los Angeles, CA: UCLA; 2007. [Google Scholar]
- 47.Center on Alcoholism, Substance Abuse, and Addictions. Short inventory of problems (SIP-2R) Alburquerque, NM: Center on Alcoholism, Substance Abuse, and Addictions; 1994. [Google Scholar]
- 48.Field C, Caetano R, Harris TR, et al. Ethnic differences in drinking outcomes following a brief alcohol intervention in the trauma care setting. Addiction. 2010;105:62–73. doi: 10.1111/j.1360-0443.2009.02737.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kitchens JM. Does this patient have an alcohol problem? Journal of the American Medical Association. 1994;272:1782–1787. [PubMed] [Google Scholar]
- 50.Ewing JA. Detecting alcoholism. The CAGE questionnaire. Journal of the American Medical Association. 1984;252:1905–1907. doi: 10.1001/jama.252.14.1905. [DOI] [PubMed] [Google Scholar]
- 51.Muthen L, Muthen B. Mplus short courses topic 6, categorical latent variable modeling using Mplus: Longitudinal Data. Los Angeles: Mplus; 2009. [Google Scholar]
- 52.Lanza ST, Collins LM, Lemmon DR, et al. PROC LCA: A SAS procedure for latent class analysis. Structural Equation Modeling. 2007;14:671–694. doi: 10.1080/10705510701575602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Connell CM, Cook EC, Aklin WM, et al. Risk and protective factors associated with patterns of antisocial behavior among nonmetropolitan adolescents. Aggressive Behaviors. 2011;37:98–106. doi: 10.1002/ab.20370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Nylund KL, Asparouhov T, Muthén BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Structural Equation Modeling. 2007;14:535–569. [Google Scholar]
- 55.Muthen B, Muthen L. Mplus. 6. Vol. 6. Los Angeles, CA: 2010. [Google Scholar]
- 56.IBM. SPSS. Vol. 19. Chicago, IL: IBM; 2011. [Google Scholar]
- 57.Center on Alcoholism, Substance Abuse, and Addictions. Drinker inventory of consequences (DrInC-2L) Alburquerque, NM: Center on Alcoholism, Substance Abuse, and Addictions; 1995. [Google Scholar]
- 58.Longabaugh R, Woolard RE, Nirenberg TD, et al. Evaluating the effects of a brief motivational intervention for injured drinkers in the emergency department. Journal of Studies on Alcohol. 2001;62:806–816. doi: 10.15288/jsa.2001.62.806. [DOI] [PubMed] [Google Scholar]
- 59.Schaus JF, Sole ML, McCoy TP, et al. Alcohol screening and brief intervention in a college student health center: a randomized controlled trial. Journal of Studies on Alcohol And Drugs Supplement. 2009:131–141. doi: 10.15288/jsads.2009.s16.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Forcehimes AA, Tonigan J, Miller W, et al. Psychometrics of the Drinker Inventory of Consequences (DrInC) Addictive Behaviors. 2007;32(8):1699–1704. doi: 10.1016/j.addbeh.2006.11.009. [DOI] [PubMed] [Google Scholar]
- 61.Muthén B, Curran P. General longitudinal modeling of individual differences in experimental designs: A latent variable framework for analysis and power estimation. Psychological Methods. 1997;2(4):371–402. [Google Scholar]
- 62. HealthIT.gov. Policy, regulation, and strategy: Behavioral health initiative (Overview) http://www.healthit.gov/policy-researchers-implementers/behavioral-health-initiative-overview.
- 63.Mechanic D. Seizing opportunities under the Affordable Care Act for transforming the mental and behavioral health system. Health Affairs. 2012;31:376–382. doi: 10.1377/hlthaff.2011.0623. [DOI] [PubMed] [Google Scholar]
- 64.Molfenter T, Capoccia V, Boyle M, et al. The readiness of addiction treatment agencies for health care reform. Substance Abuse Treatment, Prevention, and Policy. 2012;7:16–23. doi: 10.1186/1747-597X-7-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.National Trauma Data Bank. National Trauma Data Bank. http://www.facs.org/trauma/ntdb/index.html. [Google Scholar]
- 66.Davis H, Beaton S, Worley A, et al. The effectiveness of screening and brief intervention on reducing driving while intoxicated citations. Population Health Management. 2012;15:52–57. doi: 10.1089/pop.2011.0003. [DOI] [PubMed] [Google Scholar]
- 67.American College of Surgeons. Alcohol screening and brief intervention (SBI) for trauma patients: COT quick guide. Chicago, IL: American College of Surgeons; n.d. [Google Scholar]
- 68.American Public Health Association. Alcohol screening and brief intervention: A guide for public health practitioners. Washington DC: National Highway Traffic Safety Administration, U.S. Department of Transportation; 2008. [Google Scholar]
- 69.Bazzoli G, Kang R, Hasnain-Wynia R, et al. An update on safety-net hospitals: coping with the late 1990s and early 2000s. The nation's hospital safety net is holding, but dangerous waters lie ahead. Health Affairs. 2005;24(4):1047–1056. doi: 10.1377/hlthaff.24.4.1047. [DOI] [PubMed] [Google Scholar]
- 70.Selzer D, Gomez G, Jacobson L, et al. Public hospital-based level I trauma centers: Financial survival in the new millennium. Journal of Trauma. 2001;51(2):301–307. doi: 10.1097/00005373-200108000-00012. [DOI] [PubMed] [Google Scholar]
- 71.Shen Y, Hsia R, Kuzma K. Understanding the risk factors of trauma center closures: Do financial pressure and community characteristics matter? Medical Care. 2009;47(9):968–978. doi: 10.1097/MLR.0b013e31819c9415. [DOI] [PMC free article] [PubMed] [Google Scholar]