Abstract
This paper explored the relationships between parental alcoholism, sense of belonging, resilience, and depressive symptoms in Koreans in the U.S. Data from 206 Koreans (Mean age = 28.4 years; 59.8% females) living in a Midwestern state were collected in 2009, using a web-based survey, which included Children of Alcoholic Screening Test, Sense of Belonging Instrument, Connor–Davidson Resilience Scale, and Beck Depression Inventory-II. Path analysis results revealed sense of belonging as the most powerful, and resilience as the second important factor, resisting depressive symptoms associated with parental alcoholism. Implications for practice and research and study limitations are discussed.
Keywords: Adult Children of Alcoholics, Sense of Belonging, Resilience, Depressive Symptoms, Koreans
Introduction
Resilience has been one of the popular subjects of interest in mental health areas. Resilience refers to a capacity to cope successfully with significant adversity or trauma (Agaibi & Wilson, 2005). Although adult children of alcoholics (ACOA) are a risk group for substance abuse, post-traumatic stress disorder (PTSD), or multiple emotional problems, resilient ACOAs may grow up striving to adapt, survive and succeed under these stressful conditions (Johnson, Gryczynski, & Moe, 2011; Kim & Lee, 2011; Vitaro, Assaad, & Carbonneau, 2005). One of the key factors associated with resilience has been reported to be sense of belonging, which also protects individuals from depressive symptoms (Chassin et al., 2004).
The relationships among depressive symptoms, sense of belonging, and resilience have rarely been studied, and studies with Asian, especially Korean ACOAs are scarce. Korea has the 13th highest alcohol consumption in the world in both adults and teenagers. The lifetime rate of alcoholism has been reported from 14 to 20% in adults (Kim & Lee, 2011; Korean Ministry of Health and Welfare [KMHW], 2011a). There are some distinctive cultural or sociological factors which increase alcoholism among Korean people, including a very common, yet unhealthy choice of drinking as a coping mechanism at times of stress, and the irresistible, oftentimes authoritative, social pressure to make people drink even against their own will (KMHW, 2011b). Such a society, where these factors are rife, may inhibit ACOAs from seeking any outside help for the problems related to growing up in alcoholic families.
Early research on ACOAs focused on risk factors, and generally concluded that growing up with alcoholic parents increases ACOAs' risk for developing negative consequences, including alcohol or other substance abuse, or conduct disorders, as well as emotional problems like depression (E.g., Bartek, Lindeman, & Hawks, 1999; Sher, Walitzer, Wood, & Brent, 1991). Many studies reported that ACOAs exhibit symptoms of depression significantly more than those from non-alcoholic families (Hall & Webster, 2002; Lease, 2002). ACOAs may use substances to cope with their stresses related to having grown up in alcoholic families (Hussong & Chassin, 2004) and that ACOAs' risk for depression may be traced to a stressful childhood or dysfunctional family dynamics (Lease, 2002; Werner & Johnson, 2004). However, such stereotyping of ACOAs may limit their potentials to develop without adverse outcomes and demonstrate positive adjustment.
Resilient ACOAs are more likely to overcome adverse life consequences and achieve successful adjustment, even after having been exposed to cumulative stressful situations in their families (Chassin et al., 2004; Haase, 2004). ACOAs' resilience may moderate or mediate depressive symptoms, despite adversity due to parental alcoholism. Studies showed that a lack of, or decreased sense of belonging is highly correlated with depressive symptoms (Choenarom, Williams, & Hagerty, 2005; McLaren, Gomez, Bailey, & Van Der Horst, 2007); Examination of sense of belonging and resilience together in ACOAs can provide useful insights into how these protective factors may work against depressive symptoms.
This study explored relationships among parental alcoholism, sense of belonging, resilience, and depressive symptoms along with other important factors, using path analysis. We particularly focused on examining whether resilience and sense of belonging mediate negative effects of parental alcoholism on depressive symptoms in a group of Korean people. A framework first was formulated for path analysis on the basis of literature of ACOAs' depressive symptoms and important influencing factors, including family-related components (Figure 1). The following premises or hypotheses were considered: (1) ACOAs' resilience is their acquired capacity to translate the life adversities associated with parental alcoholism into desirable outcomes (Agaibi & Wilson, 2005; Lee & Cranford, 2008); (2) ACOAs' desirable outcomes in this study refer to experiencing no or few depressive symptoms (Carle & Chassin, 2004); (3) ACOAs' resilience may moderate or mediate depressive symptoms, despite adversity due to parental alcoholism (Haeffel & Grigorenko, 2007; Southwick, Vythilingam, & Charney, 2005); (4) familial and individual level factors can either reduce or enhance resilience to resist depressive symptoms in ACOAs (Haase, 2004; Tusaie & Dyer, 2004); (5) familial factors include family functioning, parental mental health problems, domestic violence experiences, and parenting (Chassin et al., 2004; Vitaro et al., 2005); (6) individual factors include attachment and sense of belonging (McLaren et al., 2007; Mylant, Ide, Cuevas, & Meehan, 2002).
Figure 1.
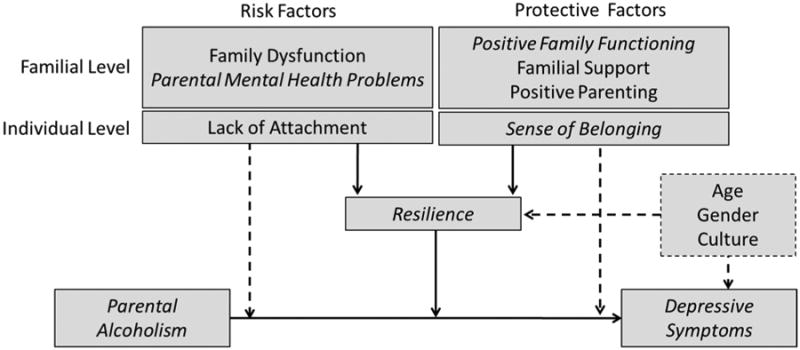
A Framework for Path Analysis: Sense of Belonging, Resilience and Depressive Symptoms in Adult Children of Alcoholics.
Methods
Participants
Voluntary community participants in Midwestern cities, who were self-identified Korean males or females, responded to an anonymous web-based survey in the study. All were aged 18 or older and the sample consisted of undergraduate or graduate students and immigrants in the United States. A total of 219 responded to the web survey either in English or in Korean. The data from 206 respondents (94.1%) were selected because 13 respondents (5.9%) did not complete the majority of questionnaires in the survey. More than half were female with a mean age of 28.4 years (S.D. = 6.9, ranged from 18 to 76 years). As shown in Table 1, three-fourths were either undergraduate or graduate students, and half were employed in either full-time or part-time positions. More than half lived in the United States for five years or less.
Table 1. Demographic Characteristics of Korean Respondents (N = 206).
| Variable | Category | Frequency (%) |
|---|---|---|
| Country of birth | USA | 22 (11.0) |
| Korea | 178 (89.0) | |
|
| ||
| Sex | Male | 80 (40.2) |
| Female | 119 (59.8) | |
|
| ||
| Marital status | Never married | 120 (61.2) |
| Married | 76 (38.8) | |
|
| ||
| Employment status | Student, not employed | 78 (39.0) |
| Student, employed as part time | 39 (19.5) | |
| Student, employed as full time | 31 (15.5) | |
| Not a student, not employed | 25 (12.5) | |
| Not a student, employed as part time | 6 (3.0) | |
| Not a student, employed as full time | 17 (8.5) | |
| Other | 4 (2.0) | |
|
| ||
| Length of stay in the US | Less than 1 year | 42 (21.0) |
| 1-2 years | 48 (24.0) | |
| 3-5 years | 46 (23.0) | |
| 6-10 years | 30 (15.0) | |
| More than 10 years | 34 (17.0) | |
|
| ||
| Loss of parent(s) at an early age | Yes | 8 (4.0) |
| No | 190 (96.0) | |
|
| ||
| Parents' marital status | Separated or divorced | 7 (3.8) |
| Never separated or divorced | 176 (96.2) | |
Note. () indicates valid percentages. No significant difference was found at p < 0.05.
Measures
Beck Depression Inventory-II (BDI-II)
Depressive symptoms were assessed using the BDI-II (Beck, Steer, & Brown, 1996) which measures the severity of depression, focusing on several major symptoms, among normal and psychiatrically hospitalized samples (E.g., Segal, Coolidge, Cahill, & O'Riley, 2008; Wilcox, Field, Prodromidis, & Scafidi, 1998). The BDI-II is a 21-item self-report inventory which asks respondents about their feelings for the past two weeks. Each item is scored from 0 to 3 (“symptom is not present” to “symptom is severe”), with higher scores indicating more depressive symptoms. Cronbach's α in this study was .90.
A short version of the Children of Alcoholics Screening Test (CAST-6)
The CAST-6 (Hodgins, Maticka-Tyndale, el-Guebaly, & West, 1993) is a shortened version of the 30-item CAST, which was originally developed by Jones (1983). The items are in a true or false response-scale and ask about adult children's feelings, attitudes, perceptions, and experiences as they relate to their parents' drinking behavior. Havey and Dodd (1995) concluded that the CAST-6 has an almost identical diagnostic function as the 30-item CAST with 93% to 98% stability of classifying COAs. In addition, the CAST mean score was used as a continuous variable to address variation of the effect of parental alcoholism on outcome variables (Vail, Protinsky, & Prouty, 2000). In this study, Cronbach's α was 0.89.
Sense of Belonging Instrument-Psychological (SOBI-P)
The SOBI-P is an 18-item self-report measure assessing an individual's experience of feeling valued and the perception of fit or connectedness within a system or environment (e.g., “In general, I don't feel a part of the mainstream of society,” “I feel like a piece of a jigsaw puzzle that doesn't fit into the puzzle”) (Hagerty & Patusky, 1995, p. 11). Respondents were asked to reflect on the past month, and to give ratings on a 4-point Likert-type scale (1=strongly disagree; 4=strongly agree), with higher scores indicating a greater sense of belonging. Cronbach's α with the study sample was .93.
Connor-Davidson Resilience Scale (CD-RISC)
The CD-RISC was developed with a wider range of respondents, including community samples, primary care outpatients, and clinical trials of PTSD (Connor & Davidson, 2003). The CD-RISC is a 25-item self-report scale with a 5-point Likert-type response format (0=rarely true and 4=true nearly all the time). The CD-RISC was validated by factor analysis, but its original five-factor solution (i.e., personal competence and tenacity, positive affects against stress, positive acceptance and secure relationships with others, control, and spiritual influence) has been found unstable in different cultural groups (Campbell-Sills & Stein, 2007; Jørgensen & Seedat, 2008); thus, the overall CD-RISC score has been used in analysis. Cronbach's α in this study was .92.
Social Support Questionnaire (SSQ-6)
The SSQ-6 (Sarason, Sarason, Shearin, & Pierce, 1987) was used to measure social support for comparing the effects of sense of belonging and social support. The SSQ-6 consists of the items to identify persons in the respondents' environment that can help in the situation described by the item. The respondents were also asked to evaluate on a 6-point scale their level of satisfaction with the support they perceived (1=very unsatisfied; 6=very satisfied). The SSQ-6 measured quantities and qualities of actual support that the Korean respondents received in the given situations, whereas the SOBI-P focused on more comprehensive aspects of the individual's connections or perceived fit to families, friends, and environment. Cronbach's α in this study was 0.93.
Family Adaptability and Cohesion Evaluation Scale-III (FACES-III)
Family functioning was measured using FACES-III (Olson, Portner, & Lavee, 1985), which is composed of two subscales—family adaptability and family cohesion. Family adaptability means the changeable range of a family system, and family cohesion means the emotional intimacy in a family. Both parts include ten items each scaled from 1 to 4. Cronbach's α for family cohesion subscale was .86; for family adaptability subscale .79.
Family-Related and Other Variables
The survey included items to ask whether respondents had any experience being exposed to domestic violence during childhood (i.e., being either a victim or witness of physical, emotional, verbal, and sexual violence in the family). Also, all respondents were asked if they thought that their parents (including alcoholic parents) had mental health problems other than alcohol abuse. Identifying these additional risk factors was important to distinguish certain individuals who may not be explained by the factors in the formulated framework of the current study. Also, these risk factors were considered when analyzing and discussing the study results. Respondents' age, sex, education, and occupation were also asked along with the families' socio-economic status in the demographic questionnaire.
Procedure
Participants completed quantitative questionnaires in a web-based survey. The Web was employed, as it has been considered efficient and maximizing study respondents' privacy and anonymity for respondents who may worry about exposing experiences related to having alcoholic parents (Dillman, 2007). The web also provides potential respondents easier access to the survey. After approval was obtained from the Institutional Review Board (IRB) at the University of Michigan, advertising flyers were posted in the community boards (paper version) in Midwestern cities as well as web boards (web version) when available, upon official permissions. The advertising flyer in both English and Korean included a web address (URL) to the survey and on-line consent form. Both language versions of the consent form and the questionnaires were available, so each voluntary participant was able to choose the language by clicking either version. The individuals were asked to read and sign the on-line consent form and agreed to participate by clicking the “CONTINUE” button. The consent form addressed the following: introduction and purpose of the study; IRB approval; anonymity and privacy of the data collected; risks and benefits of participation; available community mental health resources; and investigator and IRB contact information. In addition, the consent form indicated that data collection was in blind assessment, in which names or emails were automatically not associated with any data (anonymity), that they may leave any question blank if they were unable or did not wish to answer it, and that they could stop answering at any time if they felt uncomfortable or upset. The entire survey took 30 minutes or less. Upon completion, each participant was asked to email the investigator with a request for a $10 gift card which was given to participants as a token of appreciation for their participation time. Data was collected over a five week period.
Data Analysis
The data collected in the study was entered into the Statistical Package for the Social Sciences (SPSS) Windows Version 17.0. Path analysis was conducted with the help of analysis of a moment structures (AMOS version 8.0). Prior to path analysis, initial descriptive analyses were conducted to explore their socio-demographic and background characteristics. Multivariate analyses, including multiple regression analyses and series of path analyses, were conducted to explore the relationships of depressive symptoms with resilience, family functioning, parents' mental health problems, and a sense of belonging.
Results
Relationships among Major Study Variables
Table 2 reports the Pearson product-moment correlation coefficients among the study variables as well as their descriptive statistics. There were moderate to strong negative correlations in the relationships of depressive symptoms with resilience and sense of belonging. Sense of belonging was more strongly correlated with levels of depressive symptoms than social support. Domestic violence experience and parental alcoholism were very weakly or rarely correlated with depressive symptoms; instead they showed correlations to sense of belonging. Parental alcoholism was moderately correlated with numbers of parental mental health problems and respondents' domestic violence experiences.
Table 2. Correlations between the Major Study Variables for Korean Respondents (N = 206).
| Variable (Measurement) | 1. | 2. | 3. | 4. | 5. | 5-a) | 5-b) | 6. | 8. | 9. |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Depressive Symptoms (BDI-II) | 1.00 | |||||||||
| 2. Sense of Belonging (SOBI-P) | -.42*** | 1.00 | ||||||||
| 3. Resilience (CD-RISC) | -.60*** | .43*** | 1.00 | |||||||
| 4. Social Support (SSQ-6) | -.28*** | .42*** | .33*** | 1.00 | ||||||
| 5. Family Functioning (FACES-III) | ||||||||||
| 5-a) Family Cohesion | -.13 | .32*** | .37*** | .32*** | 1.00 | |||||
| 5-b) Family Adaptability | -.06 | .18** | .26*** | .21** | .66*** | 1.00 | ||||
| 6. Number of Parental Mental Health Problem | .18* | -.12 | -.02 | -.09 | -.19** | -.20** | 1.00 | |||
| 8. Number of Experiences with Domestic Violence | .12 | -.19** | -.08 | -.16* | -.38*** | -.33*** | .49*** | 1.00 | ||
| 9. Parental alcoholism (CAST-6) | .17* | -.22** | -.10 | -.21** | -.18* | -.14 | .39*** | .44*** | 1.00 | |
|
| ||||||||||
| Mean | 8.89 | 58.65 | 70.61 | 28.35 | 35.92 | 30.84 | 0.83 | 0.78 | 0.82 | |
| S.D. | 8.05 | 9.38 | 14.04 | 7.51 | 7.14 | 6.38 | 1.10 | 1.55 | 1.64 | |
| Range | 0-42 | 21-72 | 6-100 | 4-36 | 10-50 | 14-50 | 0-5 | 0-7 | 0-6 | |
Note.
p < 0.05,
p < 0.01,
p < 0.001.
With important correlates found in the previous bivariate analyses, several series of multiple regression analyses were performed. Only those variables showing statistically significant association with the major variables were entered into final regression models (Table 3). The overall model of depressive symptoms explained 37.3% of the variance, with only sense of belonging (b = -0.45, p < 0.001) and resilience (b = -0.26, p < 0.001) appearing to be significant predictors in the model. In the next model of sense of belonging, there are three significant predictors, including resilience (b = 0.29, p < 0.001), social support (b = 0.26, p < 0.001), and the number of domestic violence experiences (b = 0.45, p < 0.05). The overall model explained 40.9% of the variance. Lastly, for resilience, social support (b = 0.24, p < 0.01) and family cohesion (b = 0.27, p < 0.01) were significant predictors. The overall model of resilience explained 20% of the variance.
Table 3. Predictors of Depressive Symptoms, Sense of Belonging, and Resilience in Korean Respondents (Controlling for Demographic and Background Variables) (N = 206).
| Independent Variables\Dependent Variables | Depressive Symptoms | Sense of Belonging* | Resilience | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||||
| B | β | p | B | β | p | B | β | p | ||
| Sense of Belonging | -.39 | -.45 | .00 | |||||||
| Resilience | -.16 | -.26 | .00 | .20 | .29 | .00 | ||||
| Social Support | .02 | -.01 | .84 | .31 | .26 | .00 | .41 | .24 | .00 | |
| Family Cohesion | .10 | .10 | .29 | .12 | .10 | .29 | .49 | .27 | .00 | |
| Family Adaptability | .05 | .04 | .64 | -.04 | -.03 | .70 | .11 | .05 | .55 | |
| Parental Alcoholism | .14 | .03 | .68 | -.64 | -.12 | .10 | -.24 | -.03 | .69 | |
| Number of Parental Mental Health Problems | .30 | .04 | .75 | 1.24 | .15 | .13 | .18 | .02 | .84 | |
| Number of Domestic Violence Experiences | -.21 | -.04 | .70 | 2.53 | .45 | .05 | .55 | .07 | .42 | |
| Complete Model | R | .61 | .64 | .44 | ||||||
| R2 | .37 | .41 | .20 | |||||||
| p | .00 | .00 | .00 | |||||||
Direct and Mediation Effects of Major Study Variables in the Path Model
Significant influencing and mediating factors found from the previous analyses were entered into the path analysis model to examine the hypothesized relationships among all the variables (Tomarken & Waller, 2005). In the initial model explaining depressive symptoms, exogenous variables were parental alcoholism, family cohesion, family adaptability, the numbers of parental mental health problems and domestic violence experiences. The mediating variables in the model were sense of belonging, resilience, and social support. After several series of path analyses, the best model was found, as shown in Figure 2. The standardized path coefficients calculated by AMOS is shown in the figure.
Figure 2. Results of the Path Model for Depressive Symptoms among Korean Respondents (N = 206).
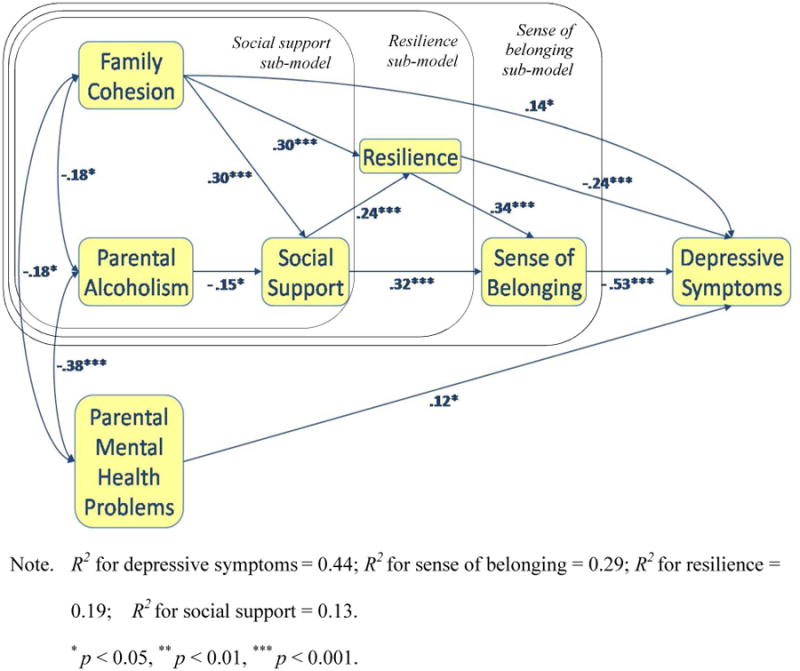
A good fit of the model was obtained: χ2 = 7.33, df = 8, p = .50, CFI = 1.00, NFI = .97, RFI = .91, RMSEA = .00. All beta weights were statistically significant at a significant level of .05. Consistent with the results from the hierarchical multiple regression analyses, depressive symptoms were predicted by sense of belonging (b = -.53, p < .001) and resilience (b = -.24, p < .001). Considering a significant indirect (mediated) effect of resilience (b = -.18), the standardized total (direct and indirect) effect of resilience on depressive symptoms was -.53. The number of parental mental health problems (p < .05) and family cohesion (p < .05) also had direct, yet relatively small, effects on depressive symptoms. Parental alcoholism only showed a small indirect effect on depressive symptoms (b = .12, p < .05). The other significant indirect effects on depressive symptoms were found from social support (b = -.27), family cohesion (b = -.21) and parental alcoholism (b = .04). Interestingly, there was a positive direct effect from family cohesion to depressive symptoms; however, when both direct and indirect effects of family cohesion were accounted, the beta weight of the total effect was -.07. These predictors all together explained 43.5% of the variance of depressive symptoms.
Looking at the three sub-models, 29.1% variance of sense of belonging was explained by the four predictors. Resilience (p < .001) and social support (p < .001) had direct effects, and social support (p < .001) also showed an indirect effect through resilience. The summed, standardized effect of social support on sense of belonging was .40. There were two more indirect effects from family cohesion (b = .22) and parental alcoholism (b = -.06). For the resilience sub-model, family cohesion (p < .001) and social support (p < .001) significantly explained resilience. Accounting its indirect effect as well, the total effect of family cohesion on resilience was b = .37. Another indirect, small effect was found from parental alcoholism on resilience (b = -.04). The model of resilience explained 19.4% of the variance. Lastly, social support was significantly predicted by family cohesion (p < .001) and parental alcoholism (p < .05). The model of social support explained 12.7% of the variance.
Discussion
The path analysis demonstrated that sense of belonging was the most powerful and proximal predictor of depressive symptoms in relation to parental alcoholism. This sense of belonging, along with social support and resilience, significantly mediated the negative effect of parental alcoholism. Other direct but small effects on depressive symptoms were found from family cohesion and the number of parental mental health problems. Parental alcoholism did not have a significant direct effect on depressive symptoms; instead, its negative effects were completely mediated by social support, resilience and sense of belonging. This finding suggests that ACOAs merit preventive intervention approaches that take protective factors into account, such as supportive interpersonal relationships, perceptions of the value of such relationships, and individual strengths or capacity to withstand stressors.
This study added more evidence that a higher level of sense of belonging has been reported to be associated with a less severe depression (Choenarom et al., 2005; Sangon, 2004; Turner & McLaren, 2011). The path model developed in the study clearly illustrated that the lack of sense of belonging is a major vulnerability factor for depressive symptoms. Stronger sense of belonging may help individuals to recognize more positive aspects of their relationships. Such perception of positivity from human relationships can help the individual to perceive rather positive aspects in their life and reduce potential deleterious effects of any sustained stress. It is important to note the difference between sense of belonging and social support to explain depressive symptoms in the path model. Although studies have used social support and sense of belonging interchangeably without clear distinction (Constantino, Kim, & Crane, 2005; Hale, Hannum, & Espelage, 2005), our results show that individual sense of belonging plays a different, much more significant role than that of social support, although both of them impact depressive symptoms.
Resilience, the second most significant factor in our model, focuses on an individual's gain and possibility in the face of adversities. As optimism, plasticity, and cognitive flexibility (e.g., positive appraisal and acceptance) have been commonly found in resilient people (Connor & Davidson, 2003; Southwick et al., 2005; Tusaie & Dyer, 2004), these people are more likely to have tolerance of negative affect by developing better problem-solving or coping skills or positive acceptance of change. Lately, in an effort to clarify more observable or measurable effects of resilience on health, an increasing number of studies have been focused on physical and even genetic biomarkers, including dehydroepiandrostrone (DHEA), neuropeptide Y, galanin, serotonin, the alpha-2 adrenergic gene and the dopamine gene (Carli et al., 2011; Das, Cherbuin, Tan, Anstey, & Easteal, 2011; Hunsberger, Austin, Chen, & Manji, 2009). The concept of resilience also has been integrated into clinical practice. A clinical trial with PTSD patients showed a significant association between venlafaxine extended release effect and individual resilience (Davidson et al., 2008).
Although family-related variables, including domestic violence experiences, showed some associations with sense of belonging and resilience in preliminary analyses, only family cohesion appeared significant in the path model. Interestingly, family cohesion has negative indirect impact as well as positive direct effect on depressive symptoms, although the total effect was negative. This finding can be difficult to interpret, yet, when considering the major aspect of family cohesion (i.e., the emotional intimacy in a family), it is possible to see two sides of family cohesion, especially within the alcoholic families. The closed system of alcoholic families can increase the risk of depressive symptoms by exacerbating effects of familial stressors and hindering possible support from outside, but within that intimate system, ACOAs may also find support to build up their resilience from both of their parents. Such a direct positive relationship between family cohesion and resilience was found in the path model.
Parental mental health problems affected the respondents' depressive symptoms, yet its effect was mediated by other familial exogenous variables in the path model. This may indicate that mental health problems within a family are transferred to next generation significantly via the shared environment in addition to genetic routes, as a twin study confirmed both family environmental and genetic factors accounting for an association between parental and juvenile depression (Silberg, Maes, & Eaves, 2010). Nevertheless and most importantly, the effect from parental mental health problems was much weaker than the effects of resilience and sense of belonging. Resilience and social support also mediated negative effects of parental alcoholism on the adult children's depressive symptoms. Therefore, clinical approaches to treatments of respondents at risk for depression should take sense of belonging, resilience, and social support into account.
Limitations
In this cross-sectional study, no data were collected about whether each respondent had been exposed to any clinical treatments, such as psychotherapy or pharmacological therapy. Such a history would help to tease out more accurate effects of the major variables. This study may have been influenced by the web-based method, which limits recruiting potential respondents with no or limited access to the Internet or a computer. Although most of the respondents might suffer from difficulty in adjusting to the new Western culture, any related issues, such as the level of acculturation, were not measured in this study. Acculturation may distinguish the stress experiences of the Koreans participants. Such effects could further contribute to their depressive symptoms. Also, only childhood maltreatment or trauma were assessed in this study; thus there was no way to determine whether they had a history of other types of trauma, which might influence their depressive symptoms, sense of belonging, resilience, and other major variables. Lastly, the sample of this study may not represent the general population.
Regardless of such limitations, this study has meaningful findings to develop better clinical approaches to ACOAs. Since the 1970s, most of the studies with alcoholic families have focused on the pathological and etiological processes of how parental alcoholism negatively influences the children. This study, however, had its focus on exploring buffering effects of sense of belonging and resilience. Our finding leads implications for the development of preventive intervention programs to enhance effective strategies for the respondents who report emotional problems.
Acknowledgments
*This project was supported in part by grants from the Rackham Graduate School (One-term Dissertation Fellowship) and the School of Nursing (Awards for New Investigators), University of Michigan.
Glossary
- Sense of belonging
the experience of personal involvement in a system or environment so that persons feel themselves to be valued and an integral part of that system or environment (Hagerty, Lynch-Sauer, Patusky, Bouwsema, & Collier, 1992, p. 173).
- Resilience
an individual's competent performance under adverse conditions (Carle & Chassin, 2004). For adult children of alcoholics, their resilience can help them to experience no or few depressive symptoms even with several life adversities associated with alcoholism of their parents.
References
- Agaibi CE, Wilson JP. Trauma, PTSD, and resilience: A review of the literature. Trauma, Violence & Abuse. 2005;6(3):195–216. doi: 10.1177/1524838005277438. [DOI] [PubMed] [Google Scholar]
- Bartek JK, Lindeman M, Hawks JH. Clinical validation of characteristics of the alcoholic family. Nursing Diagnosis. 1999;10(4):158–168. doi: 10.1111/j.1744-618x.1999.tb00047.x. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. BDI-II, Beck Depression Inventory: Manual. 2nd. San Antonio, Tex.: Psychological Corp; 1996. [Google Scholar]
- Campbell-Sills L, Stein M. Psychometric analysis and refinement of the Connor-davidson Resilience Scale (CD-RISC): validation of a 10-item measure of resilience. Journal of Traumatic Stress. 2007;20(6):1019–1028. doi: 10.1002/jts.20271. [DOI] [PubMed] [Google Scholar]
- Carle AC, Chassin L. Resilience in a community sample of children of alcoholics: its prevalence and relation to internalizing symptomatology and positive affect. Journal of Applied Developmental Psychology. 2004;25(5):577–595. [Google Scholar]
- Carli V, Mandelli L, Zaninotto L, Roy A, Recchia L, Stoppia L, et al. Serretti A. A protective genetic variant for adverse environments? The role of childhood traumas and serotonin transporter gene on resilience and depressive severity in a high-risk population. European Psychiatry. 2011;26(8):471–478. doi: 10.1016/j.eurpsy.2011.04.008. [DOI] [PubMed] [Google Scholar]
- Chassin L, Carle AC, Nissim-Sabat D, Kumpfer KL, Maton KI, Schellenbach CJ, et al. Solarz AL. Investing in children, youth, families, and communities: Strengths-based research and policy. Washington, DC: American Psychological Association; 2004. Fostering resilience in children of alcoholic parents; pp. 137–155. [Google Scholar]
- Choenarom C, Williams RA, Hagerty BM. The role of sense of belonging and social support on stress and depression in individuals with depression. Archives of Psychiatric Nursing. 2005;19(1):18–29. doi: 10.1016/j.apnu.2004.11.003. [DOI] [PubMed] [Google Scholar]
- Connor KM, Davidson JRT. Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC) Depression and Anxiety. 2003;18(2):76–82. doi: 10.1002/da.10113. [DOI] [PubMed] [Google Scholar]
- Constantino R, Kim Y, Crane PA. Effects of a social support intervention on health outcomes in residents of a domestic violence shelter: a pilot study. Issues in Mental Health Nursing. 2005;26(6):575–590. doi: 10.1080/01612840590959416. [DOI] [PubMed] [Google Scholar]
- Das D, Cherbuin N, Tan X, Anstey KJ, Easteal S. DRD4-exonIII-VNTR moderates the effect of childhood adversities on emotional resilience in young-adults. Public Library of Science one. 2011;6(5):e20177. doi: 10.1371/journal.pone.0020177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson J, Baldwin D, Stein D, Pedersen R, Ahmed S, Musgnung J, et al. Rothbaum B. Effects of venlafaxine extended release on resilience in posttraumatic stress disorder: an item analysis of the Connor-Davidson Resilience Scale. International Clinical Psychopharmacology. 2008;23(5):299–303. doi: 10.1097/YIC.0b013e32830c202d. [DOI] [PubMed] [Google Scholar]
- Dillman DA. Mail and Internet Surveys: The tailored design method. 2nd. NJ: John Wiley & Sons, Inc; 2007. [Google Scholar]
- Haase JE. Resilience. In: Paterson SJ, Bredow TS, editors. Middle Range Theories: Application to nursing research. Philadelphia: Lippincott William & Wilkins; 2004. pp. 341–367. [Google Scholar]
- Haeffel GJ, Grigorenko EL. Cognitive vulnerability to depression: exploring risk and resilience. Child and Adolescent Psychiatric Clinics of North America. 2007;16(2):435–448. doi: 10.1016/j.chc.2006.11.005. [DOI] [PubMed] [Google Scholar]
- Hagerty BM, Patusky K. Developing a measure of sense of belonging. Nursing Research. 1995;44(1):9–13. [PubMed] [Google Scholar]
- Hale CJ, Hannum JW, Espelage DL. Social support and physical health: the importance of belonging. Journal of American College Health. 2005;53(6):276–284. doi: 10.3200/jach.53.6.276-284. [DOI] [PubMed] [Google Scholar]
- Hall CW, Webster RE. Traumatic symptomatology characteristics of adult children of alcoholics. Journal of Drug Education. 2002;32(3):195–211. doi: 10.2190/U29W-LF3W-748L-A48M. [DOI] [PubMed] [Google Scholar]
- Havey JM, Dodd DK. Classifying COAs with three variations of the CAST: Classification rates, stability, and gender differences. Addictive Behaviors. 1995;20(4):501–507. doi: 10.1016/0306-4603(95)00006-x. [DOI] [PubMed] [Google Scholar]
- Hodgins DC, Maticka-Tyndale E, el-Guebaly N, West M. The CAST-6: Development of a short-form of the Children of Alcoholics Screening Test. Addictive Behaviors. 1993;18(3):337–345. doi: 10.1016/0306-4603(93)90035-8. [DOI] [PubMed] [Google Scholar]
- Hunsberger JG, Austin DR, Chen G, Manji HK. Cellular mechanisms underlying affective resiliency: the role of glucocorticoid receptor- and mitochondrially-mediated plasticity. Brain Research. 2009;1293:76–84. doi: 10.1016/j.brainres.2009.06.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussong AM, Chassin L. Stress and coping among children of alcoholic parents through the young adult transition. Development and Psychopathology. 2004;16(4):985–1006. doi: 10.1017/s0954579404040106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson JL, Gryczynski J, Moe J. Treatment issues and interventions with young children and their substance-abusing parents. In: Straussner SLA, Fewell CH, editors. Children of Substance-Abusing Parents: Dynamics and Treatment. New York, NY: Springer Publishing Company, LLC; 2011. pp. 101–125. [Google Scholar]
- Jones JW. The Children of Alcoholics Screening Test: a validity study. Bulletin of the Society of Psychologists in Addictive Behaviors. 1983;2(3):155–163. [Google Scholar]
- Jørgensen I, Seedat S. Factor structure of the Connor-Davidson resilience scale in South African adolescents. International Journal of Adolescent Medicine and Health. 2008;20(1):23–32. [PubMed] [Google Scholar]
- Kim HK, Lee MH. Factors influencing resilience of adult children of alcoholics among college students. Journal of Korean Academy of Nursing. 2011;41(5):642–651. doi: 10.4040/jkan.2011.41.5.642. [DOI] [PubMed] [Google Scholar]
- Korean Ministry of Health and Welfare [KMHW] Korea Ranked 13th in Alcohol Consumption in the World. 2011a Retrieved October 11, 2011, from http://www.hp.go.kr/hpGuide/board.dia?method=detailViewPds&page=1&mnid=0303020000000000&totmnid=null&BR_IDX=6200&searchWord=&searchKind=&PDSTYPE=C04000002&emn=030102&PDSLOCTYPE=&pFlag=
- Korean Ministry of Health and Welfare [KMHW] Sociological Factors Associated with Alcoholism in Korea. 2011b Retrieved October 11, 2011, from http://www.hp.go.kr/hpGuide/hpPortalCont.dia?method=contDetailView&mnid=0301020302030000.
- Lease SH. A model of depression in adult children of alcoholics and nonalcoholics. Journal of Counseling and Development. 2002;80(4):441–451. [Google Scholar]
- Lee H, Cranford JA. Does resilience moderate the associations between parental problem drinking and adolescents' internalizing and externalizing behaviors?: a study of Korean adolescents. Drug and Alcohol Dependence. 2008;96(1):213–221. doi: 10.1016/j.drugalcdep.2008.03.007. [DOI] [PubMed] [Google Scholar]
- McLaren S, Gomez R, Bailey M, Van Der Horst RK. The association of depression and sense of belonging with suicidal ideation among older adults: applicability of resiliency models. Suicide and Life-Threatening Behavior. 2007;37(1):89–102. doi: 10.1521/suli.2007.37.1.89. [DOI] [PubMed] [Google Scholar]
- Mylant M, Ide B, Cuevas E, Meehan M. Adolescent children of alcoholics: vulnerable or resilient? Journal of the American Psychiatric Nurses Association. 2002;8(2):57–64. [Google Scholar]
- Olson DH, Portner J, Lavee Y. FACES III. St. Paul, MN: Family Social Science, University of Minnesota; 1985. [Google Scholar]
- Sangon S. Predictors of depression in Thai women. Research and Theory for Nursing Practice: An International Journal. 2004;18(2):243–260. doi: 10.1891/rtnp.18.2.243.61276. [DOI] [PubMed] [Google Scholar]
- Sarason IG, Sarason BR, Shearin EN, Pierce GR. A brief measure of Social Support: practical and theoretical implications. Journal of Social and Personal Relationships. 1987;4(4):497–510. doi: 10.1177/0265407587044007. [DOI] [Google Scholar]
- Segal DL, Coolidge FL, Cahill BS, O'Riley AA. Psychometric properties of the Beck Depression Inventory—II (BDI-II) among community-dwelling older adults. Behavior Modification. 2008;32(1):3–20. doi: 10.1177/0145445507303833. [DOI] [PubMed] [Google Scholar]
- Sher KJ, Walitzer KS, Wood PK, Brent EE. Characteristics of children of alcoholics: putative risk factors, substance use and abuse, and psychopathology. Journal of Abnormal Psychology. 1991;100(4):427–448. doi: 10.1037//0021-843x.100.4.427. [DOI] [PubMed] [Google Scholar]
- Silberg JL, Maes H, Eaves LJ. Genetic and environmental influences on the transmission of parental depression to children's depression and conduct disturbance: an extended Children of Twins study. Journal of Child Psychology and Psychiatry. 2010;51(6):734–744. doi: 10.1111/j.1469-7610.2010.02205.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Southwick SM, Vythilingam M, Charney DS. The Psychobiology of depression and resilience to stress: implications for prevention and treatment. Annual Review of Clinical Psychology. 2005;1(1):255–291. doi: 10.1146/annurev.clinpsy.1.102803.143948. [DOI] [PubMed] [Google Scholar]
- Tomarken AJ, Waller NG. Structural Equation Modeling: strengths, limitations, and misconceptions. Annual Review of Clinical Psychology. 2005;1(1):31–65. doi: 10.1146/annurev.clinpsy.1.102803.144239. [DOI] [PubMed] [Google Scholar]
- Turner L, McLaren S. Social support and sense of belonging as protective factors in the rumination–depressive symptoms relation among Australian women. Women & Health. 2011;51(2):151–167. doi: 10.1080/03630242.2011.558004. [DOI] [PubMed] [Google Scholar]
- Tusaie K, Dyer J. Resilience: a historical review of the construct. Holistic Nursing Practice. 2004;18(1):3–8. doi: 10.1097/00004650-200401000-00002. quiz 9-10. [DOI] [PubMed] [Google Scholar]
- Vail MO, Protinsky H, Prouty A. Sampling issues in research on adult children of alcoholics: adolescence and beyond. Adolescence. 2000;35(137):113–119. [PubMed] [Google Scholar]
- Vitaro F, Assaad JM, Carbonneau R. Resilient Children of Parents Affected by a Dependency. 2005 Retrieved July 9, 2007, from http://www.hc-sc.gc.ca/hl-vs/pubs/adp-apd/child-resilient-enfant/index_e.html.
- Werner EE, Johnson JL. The role of caring adults in the lives of children of alcoholics. Substance Use & Misuse. 2004;39(5):699–720. doi: 10.1081/ja-120034012. [DOI] [PubMed] [Google Scholar]
- Wilcox H, Field T, Prodromidis M, Scafidi F. Correlations between the BDI and CES-D in a sample of adolescent mothers. Adolescence. 1998;33(131):565–574. [PubMed] [Google Scholar]


