Abstract
Objective
Previous studies have shown that ulcerative colitis (UC) is associated with the presence of lamina propria non-invariant (Type II) NKT cells producing IL-13 and mediating epithelial cell cytotoxicity. Here we sought to define the antigen(s) stimulating the NKT cells and to quantitate these cells in the UC lamina propria.
Design
Detection of Type II NKT cells in UC lamina propria mononuclear cells (LPMCs) with lysosulfatide loaded tetramer and quantum dot-based flow cytometry and staining. Culture of UC LPMCs with lyso-sulfatide glycolipid to determine sulfatide induction of epithelial cell cytotoxicity, IL-13 production and IL-13Rα2 expression. Blinded quantum dot-based phenotypic analysis to assess UC LPMC expression of IL-13Rα2, CD161 and IL-13.
Results
Approximately 36% of UC LPMC were lyso-sulfatide tetramer positive whereas few if any control LPMC were positive. When tested, the positive cells were also CD3 and IL-13Rα2 positive. Culture of UC LPMC with lyso-sulfatide glycolipid showed that sulfatide stimulates UC LPMC production of IL-13 and induces UC CD161+ LPMC-mediated cytotoxicity of activated epithelial cells; in addition, lyso-sulfatide induces enhanced expression of IL-13Rα2. Finally, blinded phenotypic analysis of UC LP MC using multi-color quantum dot staining technology showed that approximately 60% of the LPMC bear both IL-13Rα2 and CD161 and most of these cells also produce IL-13.
Conclusion
These studies show that UC lamina propria is replete with Type II NKT cells responsive to lyso-sulfatide glycolipid and bearing IL-13Rα2. Since lyso-sulfatide is a self-antigen these data suggest that an autoimmune response is involved in UC pathogenesis.
Keywords: IBD, Ulcerative colitis, Intestinal T cells, Cytokines
Introduction
Previous studies of a murine model of ulcerative colitis (UC), oxazolone-colitis, as well as human UC have provided evidence that these forms of intestinal inflammation are marked by the presence of lamina propria CD4+ T cells that by several criteria are Type II (non-invariant) NKT cells. Moreover these studies showed that upon stimulation these NKT cells produce IL-13 and exhibit cytotoxicity for epithelial cells that is augmented by IL-13 1-3. While these previous studies suggested that NKT cells play an important pathogenic role in UC, they did not address two important questions. First, they did not define a glycolipid antigen responsible for TCR stimulation of the NKT cells and for thus initiating or maintaining the UC inflammatory process. Second, they did not identify an NKT cell surface marker that could be used to quantitatively assess or functionally evaluate these NKT cells in the lamina propria of patients with ulcerative colitis.
In the present studies we address these unanswered questions. We establish first using CD1d-tetramer binding studies that the lamina propria of UC patients contains a substantial population of CD3+ T cells whose TCR binds lyso-sulfatide glycolipid, an endogenous glycolipid antigen previously shown to stimulate Type II NKT cells 4-7. Further evidence that UC NKT cells have TCRs responsive to sulfatide glycolipid came from studies showing that this antigen stimulates UC lamina propria cells to secrete IL-13 and to exhibit enhanced epithelial cell cytotoxicity. In addition, we show that sulfatide glycolipid antigen up-regulates T cell expression of IL-13Rα2, a high-affinity IL-13 receptor. Finally, we performed extensive studies of the phenotype of IL-13Rα2-expressing cells and using this receptor as a UC NKT cell marker obtained evidence that NKT cells make up the majority of cells in the UC lamina propria.
Materials and Methods
Patient Population
Sixty-four patients (pts) admitted to the Cleveland Clinic (Cleveland, OH) and the NIH Clinical Center contributed colonic tissue for these studies. These included 31 ulcerative colitis patients with severe (26 pts) or moderate (5 pts) disease based on the criteria of Truelove8 and 21 Crohn's disease patients with severe (18 pts) or moderate (3 pts) disease based on the criteria of De Dombal9; all CD patients had colonic involvement only. Patients with adenocarcinoma of the colon (n=12) who contributed the normal margin zone tissue that served as controls. The Institutional Review Boards of the Cleveland Clinic and the National Institute of Allergy and Infectious Disease, NIH approved collection of surgical specimens. Informed consent was obtained from all patients.
Preparation of Lamina Propria Mononuclear Cells
Lamina propria mononuclear cells (LPMC) were isolated from freshly obtained surgical specimens from IBD and non-IBD control patients as previously described 1. For determination of ex vivo LPMC cytokine production for IL-13, IFN-γ or IL-4, LPMC were cultured as previously described1 and as determined in the Supplementary information.
Real-time PCR
Aliquots of LPMC cells obtained from ulcerative colitis, Crohn's disease and control individuals were subjected to RNA extraction using RNeasy tissue kit (Qiagen Valencia Calif). A total of 100 ng template RNA was reversed transcribed with Superscript III RT-PCR kit (Invitrogen, Carlsbad Calif). Primer sequences for IL-13Rα2, IL-13Rα1, CD161, IL-17A and β-actin are as listed in Supplementary information.
Protein synthesis inhibition assay
A protein synthesis inhibition assay (as described in Supplemental information) was employed to secondarily assay the surface expression of IL-13Rα2 on LPMC 10,11.
Quantum Dot Immunostaining of LPMC cells
LPMC cells from UC, CD or control individuals were subjected to in situ histochemical (IHC) staining using a modified Quantum dot (Q dot) technique as described in Supplementary information 12.
Detection of sulfatide glycolipid-loaded CD1d-tetramer-binding cells
LPMC were stained with unloaded or loaded tetramer and underwent flow cytometric and Q-dot staining analysis as indicated in Supplemental information.
Statistical Analysis
Statistical differences were assessed using the Student t test and Bonferroni correction analysis for multiple parameter correlation. All values of p < 0.05 were considered statistically significant.
Results
LPMC of UC is populated by NKT cells that bind Lyso-Sulfatide-Loaded Tetramer
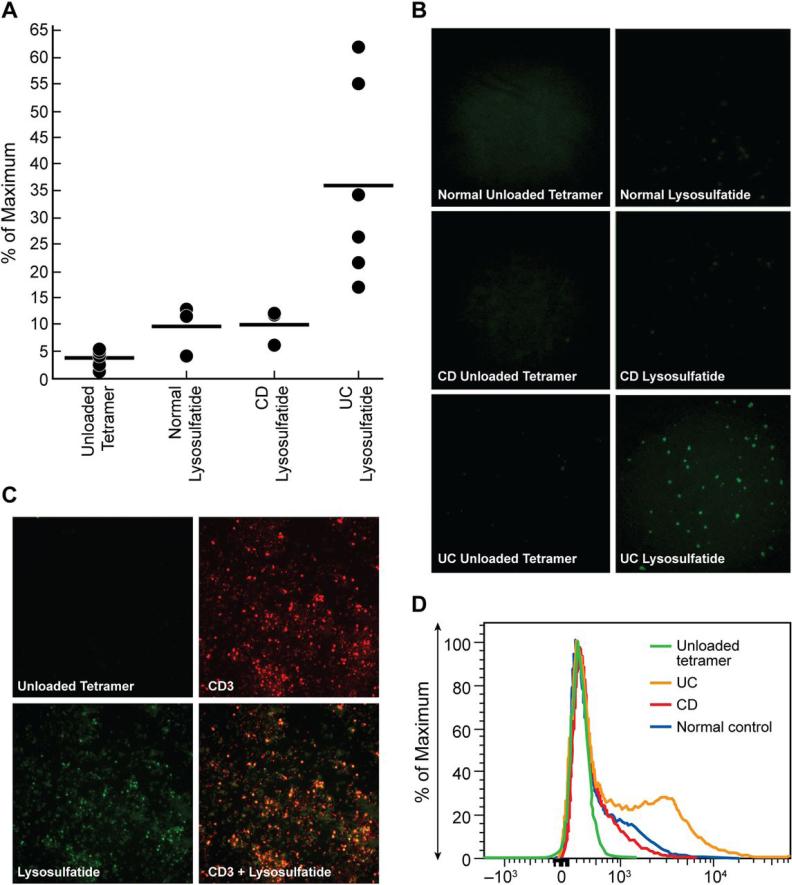
As noted above, inflamed UC tissue contains Type II (non-invariant) NKT cells that do not express Vα24 and do not respond to α-galactosylceramide 1. We therefore considered the possibility that these cells have TCRs that recognize one or more of the sulfatide family of glycolipids, i.e., self-glycolipids that have recently been shown to stimulate Type II NKT cells 4-7. To examine this possibility, we generated sulfatide-loaded CD1d tetramers using individual sulfatide isoforms previously shown to have NKT cell stimulatory activity14,15: ceramide-galactoside-3-sulfate (ceramide sulfatide) and sphingosine-1-galactoside-3-sulfate (lyso-sulfatide). We then incubated LPMC purified from UC and control lamina propria tissue with sulfatide-loaded tetramers and subjected the cells to a highly sensitive quantum dot (Q-dot) staining technique that maximizes detection of stained cells in dispersed cell populations (See Methods and Supplementary Information)12. Finally, we enumerated tetramer–positive cells by blinded counting of stained cells in dispersed cell populations using both visual observation and computer analysis; alternatively, we enumerated tetramer-positive cells by flow cytometry. We found that LPMC's from UC patients contained a population of lyso-sulfatide tetramer-positive cells that was not only approximately 4-5 fold greater than in LPMC's from Crohn's disease or normal control patients (Figure 1A), but also characterized by far greater tetramer staining intensity (Figure 1B). Indeed, while the low level staining characterizing Crohn's disease and normal control LPMC was observed by examination of slides by light microscopy, it was too faint for photographic display. Further studies indicated that these lyso-sulfatide positive cells in UC LPMC were indeed T cells as they were concomitantly positive for the T cell marker CD3 (Figure 1C). Similar results were obtained when tetramer staining was analyzed by flow cytometry (Figure 1D). It should be noted that cells in UC LPMC did not exhibit significant binding of ceramide sulfatide-loaded tetramers (Supplemental Figure 1), possibly reflecting the fact that they have TCRs that bind this form of sulfatide with an affinity below that necessary to detect tetramer binding using the technique presently available.
Figure 1.
(A) Purified LPMCs were isolated from UC (n=6), CD (n=3) and control patient populations (n=3) and subjected to Q dot staining analysis to detect binding of lyso-sulfatide tetramer. Percent expression of lyso-sulfatide tetramer binding is shown. Percent expression represents lyso-sulfatide binding for each patient sample minus expression of binding for unloaded tetramer of each patient sample. All data sets from each patient were performed in triplicate. For staining percentage comparison p < 0.01 ulcerative colitis vs Crohn's disease or normal controls and p value < 0.0001 for staining intensity with no statistical difference for Crohn's disease vs normal controls for percentage staining (p > 0.9) or staining intensity (p > 0.4) (B) Purified LPMCs were isolated from UC (n=6), CD disease (n=3) and control patients (n=3) and subjected to Q dot staining to detect binding of lysosulfatide tetramer. One representative staining experiment is shown. (C) Purified LPMCs were isolated from UC patient population (n=2), and subjected to Q dot staining to detect binding of lyso-sulfatide tetramer and CD3, range 52-58 % Lyso-sulfatide+/CD3+. (D) Purified LPMCs were isolated from UC (n=6), CD (n=3) and control patient populations (n=3) were subjected to Q dot staining for flow cytometry analysis to detect binding of lyso-sulfatide tetramer. Mean MFI for normal control 886, Crohn's disease 726, Ulcerative colitis 2076.
Sulfatide Glycolipids Induce UC NKT cell IL-13 Production
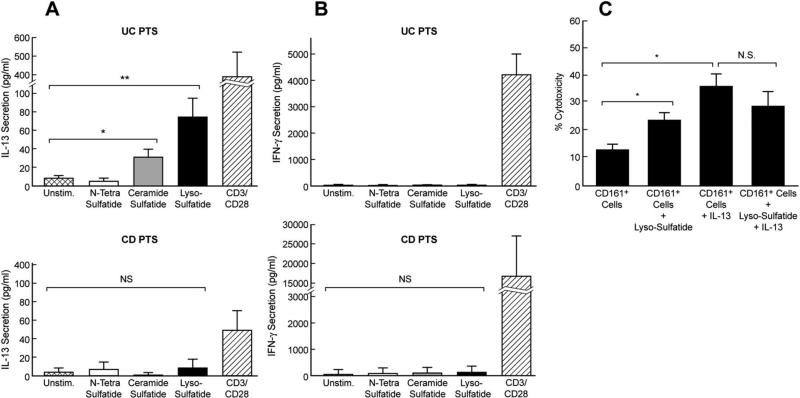
In a second approach to evaluating if UC NKT cells recognize a sulfatide glycolipid we determined if the latter stimulates NKT cells in UC LPMC to produce IL-13, a cytokine previously shown to be produced by UC NKT cells 1. In this case we stimulated the cells with lyso-sulfatide and ceramide sulfatide as well as an additional sulfatide family member also shown to stimulate NKT cells, N-tetrasulfatide (N-tetracosanoyl-sphingosyl-beta-D-galactoside-3-sulfate).14,15 We found that lyso-sulfatide and ceramide sulfatide stimulated UC LPMC to produce IL-13 (74 pg and 31pg/ml respectively) whereas N-tetra-sulfatide had no stimulatory effect (Figure 2A).
Figure 2.
Cytokine secretion by UC (upper panels of A & B) and CD (lower panels of A & B) LPMCs. (A) IL-13 and (B) IFN-γ secretion obtained from inflamed UC (n=3) and inflamed CD (n=3) tissues induced by either indicated sulfatide glycolipids or CD3/CD28 as previously indicated 1,4-7. Error bars represent 1 SD. * p ≤ 0.05 Ceramide sulfatide vs unstim , ** p ≤ 0.05 Lyso-sulfatide vs unstim, NS; Not statistically significant (C) Cytotoxicity of CD161+ T cells. HT-29 epithelial cells were pre-stimulated with LPS to induce increased expression of CD1d (data not shown). Purified UC lamina propria CD4+CD161+ T cells were cultured with target HT-29 cells at a ratio of 10:1 and in the presence or absence of lyso-sulfatide and/or IL-13, and the percentage of cytotoxicity was measured (n=3). Error bars represent 1SD. * p ≤ 0.05 , N.S.; Not statistically significant p ≥ 0.1.
Important negative results obtained in these studies included the fact that none of the sulfatides induced increased secretion of IFN-γ (Figure 2: the mean IFN-γ secretion of 32.7 pg/ml by cells stimulated with lyso-sulfatide was not different than that of unstimulated cells. In addition, LPMC from Crohn's disease patients were not stimulated by any of the sulfatides tested to produce measurable amounts of IL-13 or IFN-γ (Figure 2A and 2B: mean production of 9 and 210 pg/ml respectively by cells stimulated with lyso-sulfatide similar to that of unstimulated cells. Finally, none of the sulfatides induced either UC or CD LPMC to produce measurable amounts of IL-4 (data not shown).
In another series of studies involving additional UC patients we determined whether induction of IL-13 by lyso-sulfatide was inhibited by the presence of anti-CD1d. We found that addition of optimal amounts of anti-CD1d to cultures of LPMC led to a statistically significant decrease in IL-13 secretion (range 41-63%; p < 0.04). In contrast, addition of anti-MHC class II had no effect on the level of lysosulfatide induced IL-13 secretion (data not shown). These results indicate that lyso-sulfatide stimulation was acting, at least in part, via CD1d-mediate sulfatide presentation to NKT cells.
Lyso-Sulfatide Stimulation of UC LPMC Enhances CD161+ T Cell Cytotoxicity of Epithelial Cells
In other studies also addressing the capacity of UC LPMC to recognize and respond to a sulfatide glycolipid we determined whether the most active sulfatide in the IL-13 secretion study, lyso-sulfatide, induces cytotoxicity of LPS-stimulated HT-29 epithelial cells, i.e., epithelial cells expressing surface CD1d (see Methods). In this case we evaluated the cytotoxic potential of purified CD4+CD161+ LP cells rather than whole LPMC's, since, in a prior study, we have shown that this cell subpopulation mediates epithelial cell cytotoxicity1. We found that CD4+CD161+ LP cells obtained from lamina propria of UC patients exhibited considerable baseline cytotoxic activity (mean 12.4%) in the absence of any added sulfatide (Figure 2C). It is likely that this was due to the fact that normal epithelial cells display sulfatide glycolipids on their cell surface and therefore can stimulate cytotoxic activity by CD161+ T cells in the absence of added sulfatide glycolipid 16; thus, the true baseline may be better represented by that exhibited by purified CD4+CD161+ LP cells obtained from CD patients (2.9%) which do not respond to the sulfatide glycolipids studied here (data not shown). Thus, addition of lysosulfatide led to a significant further enhancement of cytotoxicity when compared to the UC cell baseline.
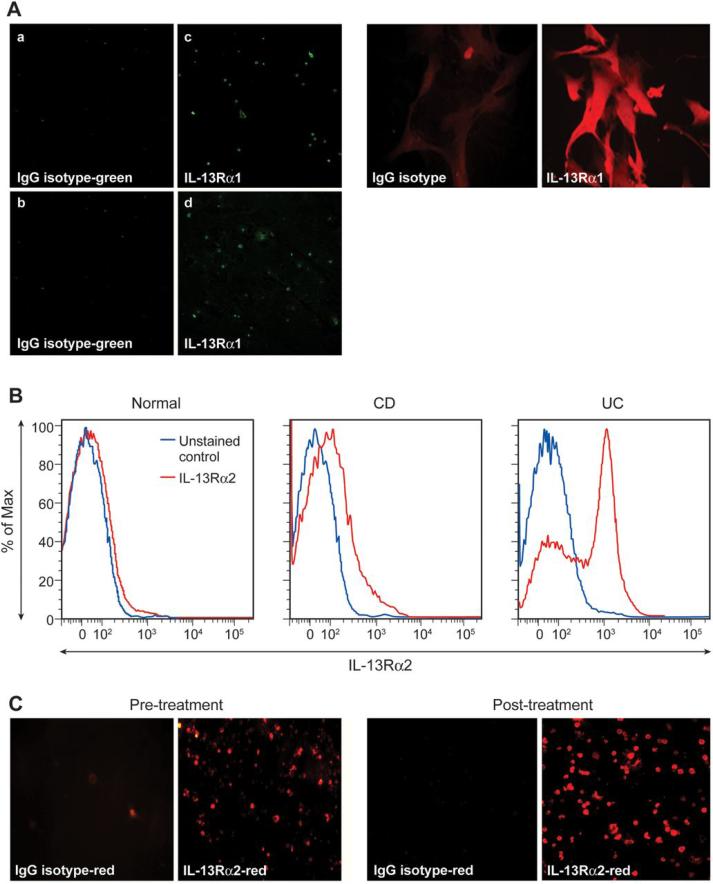
Lyso-Sulfatide Stimulation of UC LPMC Induces Up-regulation of IL-13Rα2
In previous studies we observed that IL-13 augmented UC NKT cell cytotoxicity of an epithelial target cells 1. This implied that UC NKT cells bear an IL-13 receptor and prompted us to determine if lysosulfatide stimulation of UC LPMC induces such receptor expression. In initial studies we assessed IL-13Rα1 expression in LPMCs employing a Q-dot-based in situ histochemical staining technique. We found that IL-13Rα1 was barely detectable in UC LPMC (+1 low staining intensity) and stained cells comprised a relatively low fraction of UC LPMC that was not augmented by lyso-sulfatide stimulation (34 ± 5.3% pre-lyso-sulfatide and 35 ± 4.1% post-lyso-sulfatide stimulation) (Figure 3A). This result was corroborated by the fact that UC LPMC displayed no detectable IL-13Rα1 receptor mRNA expression pre- and post-lyso-sulfatide stimulation (data not shown).
Figure 3.
UC LPMC IL-13Rα1 and IL-13Rα2 expression. (A) Left panel: UC LPMC cells stimulated in vitro with lyso-sulfatide and subjected to Q dot staining for IL-13Rα1. One representative Q dot staining of UC LPMC depicting IL-13Rα1 expression, pre-treatment (top left panel) and post-treatment with lyso-sulfatide (bottom left panel) is shown. Right panel: Glioblastoma cell line (U251) which has a high expression of IL-13Rα1 served as a positive control. (B) Purified LPMC were obtained from UC, CD and control patient populations and subjected to Q dot staining FACS analysis for IL-13Rα2. One representative histogram from each group depicting % expression of IL-13Rα2 is shown. Range of expression for each group: UC 48-65% (n=5), CD 4.0-8.3% (n=3), controls 1.8-4.0 % (n=3). (C) UC LPMC cells stimulated in vitro with lyso-sulfatide and subjected to Q dot staining for IL-13Rα2 and CD161 expression. One representative Q dot staining of UC LPMC depicting IL-13Rα2, CD161 and IL-13Rα2/CD161 expressing cells is shown (n=3).
A very different result, however, was found applying the same approaches to assessment of UC LPMC IL-13Rα2 expression. In this case, the LPMCs displayed a much higher baseline percentage of detected stained cells bearing IL-13Rα2 than LPMCs from CD or control patients as well as greatly increased levels of IL-13Rα2 mRNA (Figure 3B and Supplemental Figure 2). In addition, quantitative assessment of staining data using both computer analysis and visual observation disclosed that the percentage of IL-13Rα2+ cells in UC LPMC populations increased from a baseline value of 61 ± 5.6% to a lyso-sulfatide stimulated value of 79 ± 7.8% (p < 0.05) (Figure 3C); thus, lyso-sulfatide stimulation of LPMC induced a substantial increase in the number of cells bearing this receptor and augmented the intensity of IL-13Rα2 staining on individual cells.
In complementary studies to verify the above effect of lyso-sulfatide on UC LPMC IL-13Rα2 expression, we measured changes in lyso-sulfatide-induced IL-13Rα2 expression on individual cells in a cell lysis assay dependent on targeting cell surface IL-13Rα2 with increasing concentrations of IL-13-Pseudomonas-exotoxin (IL-13-PE), an agent that reacts specifically with and then induces cytotoxicity of IL-13Rα2-bearing cells. In this assay cell lysis by IL-13-PE pre- and post-exposure of cells to lyso-sulfatide is assessed by changes in the capacity of unlysed cells to incorporate leucine (a measure of protein synthesis); in addition, since cell lysis by IL-13-PE is dependent on the density of IL-13Rα2 expression on individual cells, the rate of decrease in leucine incorporation with increasing IL-13PE concentration is a measure of lyso-sulfatide-induced IL-13Rα2 expression in individual cells (10,11).
These cell-lysis studies showed that the rate of leucine incorporation decrease by UC LPMC was enhanced post-lyso-sulfatide exposure compared to pre-lyso-sulfatide exposure (Supplemental Figure 3). Thus, while approximately 10ng/ml of IL-13-PE was required to achieve a 50% decrease in protein synthesis in cells pre-lyso-sulfatide exposure, only 1 ng/ml of IL-13-PE was necessary for the same decrease post-lyso-sulfatide exposure. These results are consistent with those obtained with the quantum-dot staining studies in showing that lyso-sulfatide induces an increased number of IL-13Rα2 expressing cells; however, they go a step further in showing that lyso-sulfatide also induces an increased concentration of IL-13Rα2 on individual cells. Of note, no change in leucine incorporation was observed in studies of CD and normal control LP cells indicating that these cells exhibit little, if any, IL-13Rα2 expression.
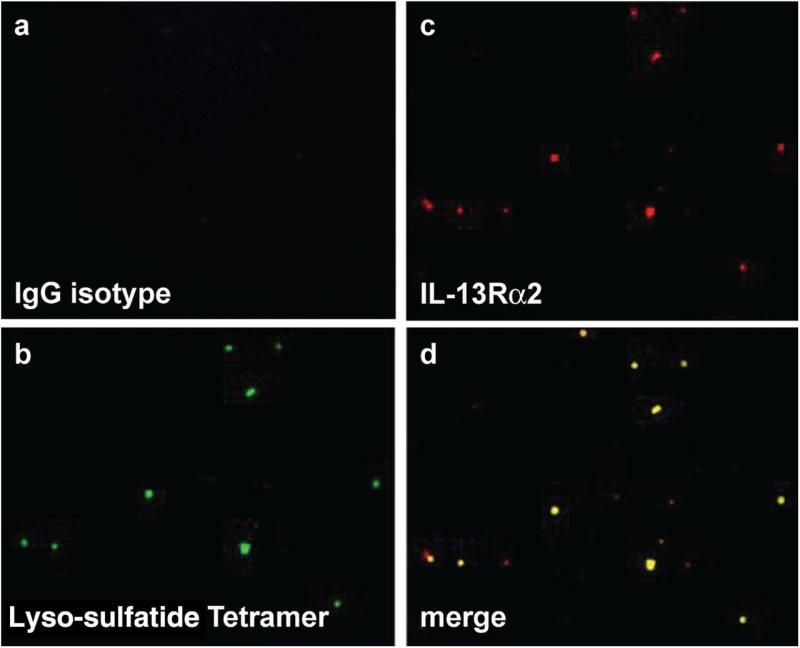
Expression of IL-13Rα2 on Lamina Propria Cells in Patients with Ulcerative Colitis
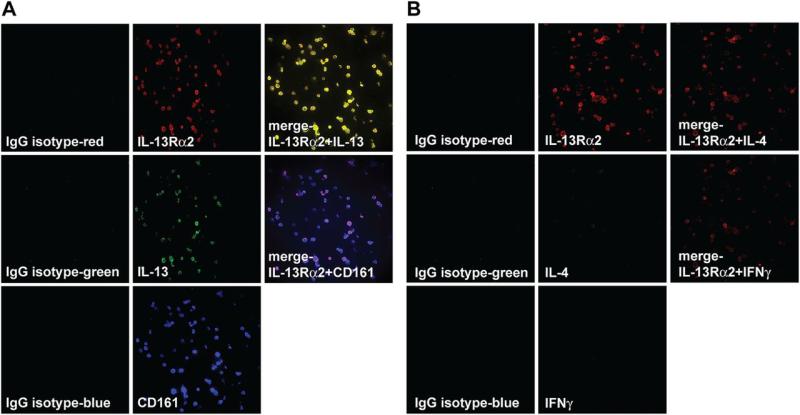
Given the above relationship of IL-13Rα2+ cells to lyso-sulfatide stimulation we next determined the expression of this receptor on lyso-sultatide-loaded tetramer-positive UC LPMCs using dual Q-dot staining. We found that, indeed, virtually all tetramer-positive cells co-expressed IL-13Rα2 (Figure 4) whereas in contrast these dual staining cells were absent in CD LPMC populations. This result suggested that IL-13Rα2 could be used as a marker of NKT cells in UC lamina propria and prompted us to conduct studies of the phenotype and frequency of IL-13Rα2-positive cells in the UC lamina propria. In initial semi-quantitative staining studies of LPMC we found that IL-13Rα2-bearing cells were numerous in these populations and frequently co-express IL-13 and CD161 (Figure 5A). Moreover, the IL-13Rα2-bearing cells did not co-express IL-4 or IFN-γ (Figure 5B) and did not co-express CD14, the latter ruling out expression by inflammatory macrophages (data not shown).
Figure 4.
Purified LPMCs isolated from ulcerative colitis patients (n=5) were subjected to Q dot staining to detect IL-13Rα2 expression and binding of lyso-sulfatide tetramer. Expression of cells demonstrating dual IL-13Rα2 staining and binding of lyso-sulfatide tetramer was 36 +/− 6 % (with a staining intensity of +3) while that of Crohn's disease (n=3) was 4 +/− 1% (data not shown) with a staining intensity of < +1)(p < 0.008) Data set from each patient was performed in triplicate.
Figure 5.
(A) Q dot staining of UC LPMC reveals CD161+ cells exhibit increased expression of IL-13Rα2 and IL-13. Purified LPMC obtained from inflamed UC tissue were subjected to Q dot staining and analyzed for expression of IL-13Rα2, IL-13, CD161 and for co-expression of these markers. One representative Q dot staining of UC LPMC is shown (n=7). (B) Purified LPMC obtained from inflamed UC tissue were subjected to Q dot staining and analyzed for expression of IL-13Rα2, IL-4, IFN-γ and for co-expression of these markers. Q dot study of UC LPMC shown is representative of 7 such studies of individual patients. One representative Q dot staining of UC LPMC is shown (n=7).
In subsequent and more quantitative studies, we subjected LPMC to staining studies in which cell counts were established by blinded computer analysis and visual assessment of stained cells. The results, depicted in Table 1, show that IL-13Rα2+ cells comprised 70.3 ± 9.4% of total dispersed lamina propria cells, a percentage not significantly different from that of CD161+ cells, 67 ± 7.6%; (p >0.5) moreover, these markers were generally present on the same cells since IL-13Rα2+/CD161+ double-positive cells comprised 58.7 ± 9.2% of the total LPMC dispersed cells (p > 0.07). In addition, IL-13+ cells comprised 65.7 ± 5.9% of the total cells, again not significantly different from the percentage of IL-13Rα2+ or CD161+ cells (p > 0.3, p > 0.5 respectively) and most of these cells also bore IL-13Rα2 since the percentage of IL-13Rα2+/IL-13+ cells was 58.4 ± 10.7%, a percentage equivalent to that of IL-13-bearing cells (p > 0.1) allowing for the fact that the detection of double positive cells was not as efficient as the detection of single positive cells. Finally, about 45-50% of the LPMC in UC were CD4+ T cells most of which were present in the IL-13Rα2+CD161+ population; in addition, in the one patient studied, 6% of LPMC were lightly stained CD8+ T cells. Overall, these studies provide definitive evidence that a large proportion of UC lamina propria cells bear markers associated with NKT cells, IL-13Rα2 and CD161, most, if not all of which secrete IL-13.
Table I.
Analysis of lamina propria cells by Q-dot staining.
| Mean Staining Intensity Mean ± SD (% positive cells) (range) |
IL-13Rα2 | CD161 | IL-13 | IL-4 | IFN-γ | IL-13Rα2 + CD161 | IL-13Rα2 + IL-13 |
|---|---|---|---|---|---|---|---|
| Ulcerative Colitis (n=7) | 3.3+ 70.3 ± 9.4a (58-84) |
3.4+ 67±7.6b (54-78) |
3+ 65.7±5.9c (58-74) |
1+ 8±1.9 (6-10) |
1+ 7.7±1.8 (6-10) |
3+ 58.7±9.2d (45-68) |
2.9+ 58.4±10.7e (39-70) |
| Crohn's Disease (n=6) | <1+ 9.2±3.1 (6-14) |
<1+ 7.8±2.0 (6-10) |
<1+ 9.5±4.0 (6-16) |
2+ 38±5.0 (30-44) |
2.5+ 56.5±6.1 (51-64) |
<1+ 5.5±1.5 (4-8) |
<1+ 6±1.4 (4-8) |
| Normal (n=4) | <<1+ 7±2.2 (5-10) |
<<1+ 6.3±1.3 (5-8) |
<<1+ 6.3±1.3 (5-8) |
1.25+ 15±2.6 (4-28) |
<<1+ 6±1.4 (5-8) |
<<1+ to 1+ 3.3±1 (2-4) |
<<1+ 5.8±1.7 (4-8) |
Statistical Analysis:
a vs b: p ≥ 0.5; a vs c: p ≥ 0.3; b vs c: p ≥ 0.5; b vs d: p ≥ 0.07; c vs e: p ≥ 0.1.
Concomitant studies of Crohn's disease LPMC disclosed that high-level expression of IL-13Rα2 and CD161 was a unique feature of UC cells. Thus, both IL-13Rα2 and CD161 was detected on only 5-10% of cells and the intensity of staining of these positive cells was quite low (Supplemental Figure 4). Likewise, only 6-16% of the cells exhibited IL-13 staining and the intensity of staining of these positive cells was low. Thus, UC LPMCs contained a significantly higher percentage of cells than Crohn's disease or control LPMCs of cells positive for IL-13, IL-13Rα2, CD161, IL-13Rα2/CD161 and IL-13/IL-13Rα2 (p < 0.007Bonferroni correction for multiple parameter analysis) whereas CD and control LPMCs exhibited no difference in these parameters (p > 0.1). In addition, while UC lamina propria cells revealed only low-level intensity and insignificant staining for IL-4 and IFN-γ, CD lamina propria cell populations exhibited strong IFN-γ staining and some low intensity IL-4 staining. With regard to the latter, it should be noted the IL-4 staining was not accompanied by detectable IL-4 secretion either in the present studies or in previous studies 17. IL-17A mRNA production in UC LPMCs was slightly greater than that of normal control but, decreased in comparison to that of CD LPMC (data not shown). Finally, whereas a substantial sub-population of UC LPMC CD161+ cells also expressed IL-5 virtually little of these cells expressed IL-17 (Supplemental Figure 5)
Secretion of IL-13 by UC LP Cells Following Treatment with IL-13-PE
Taking a more functional approach to relating IL-13Rα2 expression to NKT cells in UC, we measured IL-13 production by LPMC before and after culture with IL-13-PE using the latter to selectively eliminate IL-13Rα2-bearing cells. We found that prior exposure of LPMC from UC patients to IL-13-PE led to a significant decrease in the amount of IL-13Rα2+ cells (Supplemental Figure 6A). In addition, LPMC from UC patients pre-exposed to IL-13-PE and then activated with anti-CD3/anti-CD28 in vitro caused a mean 68% reduction in IL-13 secretion but no change in IFN-γ secretion (Supplemental Figure 6B and data not shown, respectively). This reduction was similar in magnitude to the reduction in the number of IL-13Rα2+ cells, suggesting that most if not all of IL-13 was in fact being produced by receptor-positive cells. Similar results were obtained when cytotoxicity was used as a read-out rather than IL-13 production in that again, the reduction in cytotoxicity was similar to the reduction in the number of CD161+ cells (Supplemental Figure 6C and 6D). While these results require verification with studies of additional patients they provide additional evidence that IL-13Rα2+ is a marker of LP NKT cells in UC patients.
Discussion
In previous studies we obtained several kinds of evidence suggesting that ulcerative colitis was associated with the presence of lamina propria non-invariant (Type II) NKT cells. Most importantly, we showed that in parallel with invariant NKT cells in the lamina propria of mice with oxazolone colitis (oxa-colitis) that produce IL-13 upon stimulation with α-GalCer, non-invariant CD161 cells in the UC lamina propria produce IL-13 when stimulated with CD1d-expressing APC's 1,2. In addition, we showed that the UC lamina propria contains T cells that are cytotoxic for LPS-stimulated epithelial cells and that this cytotoxicity is augmented by the presence of IL-13 1. In the present study we expand on these findings by showing that a substantial population of LPMC from UC patients bind sulfatide glycolipid-loaded CD1d tetramer and thus bear TCRs that react to a glycolipid previous shown to interact with non-invariant NKT cells 4-7. In addition, we show that UC LPMC can be stimulated by sulfatide glycolipid to produce IL-13 and to manifest cytotoxicity for LPS-stimulated epithelial cells that is substantially inhibited by the presence of anti-CD1d antibody. These new data not only provide strong new support for the idea that non-invariant NKT cells do in fact populate the LP of UC patients but may establish the identity of the TCR reactive antigen capable of stimulating these cells.
Staining of UC lamina propria cells with labeled lyso-sulfatide-loaded tetramers indicated that a very substantial fraction of these cell, approximately 36%, were in fact Type II NKT cells. However, this could be an under-estimate of the percentage of NKT cells in UC lamina propria because lyso-sulfatide might bind to the TCR of UC NKT cells with an affinity that is sub-optimal when compared to that of an as yet unidentified endogenous stimulatory sulfatide actually present in the UC lamina propria. As an alternative approach to NKT cell quantitation in UC we explored the possibility that IL-13Rα2 present on LPMCs could be a surrogate marker of the NKT cell subpopulation. Two observations suggested that was likely to be the case. First, stimulation of UC LPMC with sulfatide not only up-regulated the number of cells bearing IL-13Rα2, but also increased the level of expression of this receptor on individual cells. Second, dual staining of LPMC to identify tetramer-positive cells and IL-13Rα2-positive cells revealed that virtually all the tetramer-positive cells were also IL-13Rα2-positive.
In further studies along these lines, we evaluated the number and phenotype of IL-13Rα2-bearing cells in UC lamina propria using a sensitive and unbiased in situ staining technique coupled with flow cytometry. This revealed that the majority of UC LPMC's bear IL-13Rα2 whereas only a small percentage of Crohn's disease or control LPMC's bear this receptor and then at a low expression level. In addition, the receptor-bearing cells also bear the NKT cell marker, CD161 and most are IL-13-producing cells. These latter findings provide additional support for the view that IL-13Rα2 is a valid marker of NKT cells in UC since CD161 is a known marker of NKT cells and IL-13 production, as noted previously in studies of both oxazolone colitis and UC patients 1,2. Additional support for the idea that IL-13Rα2 is an NKT cell marker in UC LP came from studies showing that IL-13-PE-mediated depletion of UC lamina propria cells led to greatly reduced level of IL-13 production and cytotoxic activity, both of which was proportional to the extent of depletion. Overall, these phenotypic studies of lamina propria cell populations provide strong evidence that IL-13Rα2+IL-13+CD161+ T cells make up the majority of cells in the inflamed UC mucosa.
The fact that UC NKT cells express IL-13Rα2 but little or no IL-13Rα1 was a somewhat unexpected characteristic of these cells although it was presaged by a previous study showing that this receptor is expressed in the lamina propria of oxazolone-colitis in Western blot studies that did not identify the cellular origin of the IL-13Rα2 18,19. Of interest, in this previous study down-regulation of IL-13Rα2 expression was shown to be associated with a reduced level of colitis. This correlates with the fact that sulfatide glycolipid induces NKT cell IL-13 production and the latter, in turn, stimulates NKT cell cytotoxic function.
The finding that UC is characterized by the presence of a lamina propria self-antigen (sulfatide)-responsive Type II NKT cell population invites a re-examination of the underlying pathogenesis of this disease. One important possibility that needs to be considered on the basis of this new information is that the key pathologic event occurring in UC consists of an abnormality in the way epithelial cells process and display a self-glycolipid (sulfatide) antigens perhaps in response to a “stress” signal from the luminal microbiota. Support for this possibility comes from a recent report that an epithelial cell-specific mutation of XBP1, an intra-cellular protein critical to the initiation of the endoplasmic reticulum stress response of secretory cells, is associated with hyper-responsive to an innate ligand and results in spontaneous intestinal inflammation or increased susceptibility to induced colitis 20. On this basis, one might speculate that while a proximal cause of UC is an NKT cell-mediated autoimmune-like response, the more basic cause of this disease lies in a defect in the way epithelial cells respond to the endogenous microbiome. This latter possibility finds support in a recent study by Olszak et al., which showed that neonatal germ-free mice exhibit increased LPs NKT cell infiltration and heightened oxazolone colitis, a mouse model of UC21.
Finally, the findings reported here showing that UC is characterized by the presence of NKT cells bearing IL-13Rα2 suggest that this receptor could be used as a marker that would distinguish UC from other forms of IBD and, at the same time, would provide insight into disease severity. In addition, since NKT cells which produce IL-13 may be the main effector cell driving UC inflammation, this receptor could also be targeted by potential UC therapeutic agents. The latter presently being investigated with therapeutic agents targeting IL-13.
Supplementary Material
What is already known on this subject?
A murine model of ulcerative colitis (UC), oxazolone colitis, as well as human UC are marked by the presence of CD4+ NKT cells; in UC these cells are Type II NKT cells that are non-invariant.
Upon activation, the NKT cells secrete large amounts of IL-13, a cytokine that is both cytotoxic for epithelial cells and that augments NKT cell cytotoxicity for epithelial cells.
What are the new findings?
The UC lamina propria is populated by a large number of Type II NKT cells recognized by their ability to bind lyso-sulfatide glycolipid-loaded CD1d-tetramer.
Lyso-sulfatide glycolipid stimulates UC lamina propria NKT cells to produce IL-13, exhibit increased epithelial cell cytotoxicity and display increase levels of IL-13Rα2.
IL-13Rα2-bearing cells in UC lamina propria constitute approximately 60% of the mononuclear cells present and co-express IL-13 and CD161.
How might it impact on clinical practice in the foreseeable future
The clinical severity of patients with UC might be assessed by quantitation of cells binding lyso-sulfatide-loaded tetramer and/or bearing IL-13Rα2.
UC could be treated by reducing the levels of lamina propria IL-13Rα2-bearing NKT cell or IL-13 levels.
Acknowledgements
This manuscript is dedicated to the continued memory of my father Abe Fuss, may others never know the words IBD.
This work was supported by the Intramural Research Program of NIAID, National Institutes of Health.
Abbreviations
- UC
Ulcerative colitis
- CD
Crohn's disease
- NKT
Natural killer T cell
- Oxa
Oxazolone
- LPMC
Lamina propria mononuclear cell
- Q dot
Quantum Dot
- PE
Pseudomonas exotoxin
Footnotes
Authors Contributions:
Ivan J. Fuss: study concept and design; acquisition of data; analysis and interpretation of data; drafting of the manuscript; critical revision of the manuscript for important intellectual content; statistical analysis
Bharat Joshi: study concept and design; acquisition of data; analysis and interpretation of data; drafting of the manuscript; critical revision of the manuscript for important intellectual content; statistical analysis
Zhiqiong Yang: acquisition of data; analysis and interpretation of data
Heba Degheidy,: acquisition of data; analysis and interpretation of data
Stefan Fichtner-Feigl: obtained technical or material support
Heitor de Souza: obtained technical or material support
Florian Rieder: obtained technical or material support
Franco Scaldaferri: obtained technical or material support
Anja Schirbel: obtained technical or material support
Melania Scarpa: obtained technical, or material support,
Chuli Yi: acquisition of data; analysis and interpretation of data
Lili Xu: acquisition of data; analysis and interpretation of data
Pamela Leland: acquisition of data; analysis and interpretation of data
Michael Yao: acquisition of data; analysis and interpretation of data
Peter Mannon: study concept and design; acquisition of data; analysis and interpretation of data; drafting of the manuscript; critical revision of the manuscript for important intellectual content
Raj K. Puri: study concept and design; analysis and interpretation of data; drafting of the manuscript; critical revision of the manuscript for important intellectual content; study supervision
Claudio Fiocchi: analysis and interpretation of data; drafting of the manuscript; critical revision of the manuscript for important intellectual content; obtained technical or material support; study supervision).
Warren Strober: study concept and design; analysis and interpretation of data; drafting of the manuscript; critical revision of the manuscript for important intellectual content; statistical analysis; study supervision.
The Corresponding Author has the right to grant on behalf of all authors and does grant on behalf of all authors, a non exclusive (work performed as a US government employee) on a worldwide basis to the BMJ Publishing Group Ltd and its Licensees to permit this article (if accepted) to be published in Gut editions and any other BMJPGL products to exploit all subsidiary rights, as set out in our license.
No authors have competing interests but, declare the issuance of a patent broadly relevant to this work to Drs. Fuss and Strober, for the use of inhibitors of IL-13 in the treatment of ulcerative colitis.
References
- 1.Fuss IJ, Heller F, Boirivant M, et al. Nonclassical CD1d-restricted NK T cells that produce IL-13 characterize an atypical Th2 response in ulcerative colitis. J. Clin. Invest. 2004;113:1490–97. doi: 10.1172/JCI19836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Heller F, Fuss IJ, Nieuwenhuis EE, et al. Oxazalone colitis, a Th2 colitis model resembling ulcerative colitis, is mediated by IL-13-producing NK-T cells. Immunity. 2002;17:629–38. doi: 10.1016/s1074-7613(02)00453-3. [DOI] [PubMed] [Google Scholar]
- 3.Heller F, Florian P, Bojarski C, et al. Interleukin-13 is the key effector Th2 cytokine in ulcerative colitis that affects epithelial tight junctions, apoptosis, and cell restitution. Gastroenterology. 2005;129:550–64. doi: 10.1016/j.gastro.2005.05.002. [DOI] [PubMed] [Google Scholar]
- 4.Shamshiev A, Gober HJ, Donda A, et al. Presentation of the same glycolipid by different CD1 molecules. J. Exp. Med. 2002;195:1013–21. doi: 10.1084/jem.20011963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jahng A, Maricic I, Aguillera C, et al. Prevention of autoimmunity by targeting a distinct, noninvariant CD1d-reactive T cell population reactive to sulfatide. J. Exp. Med. 2004;199:947–57. doi: 10.1084/jem.20031389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zajonc DM, Maricic I, Wu D, et al. Structural basis for CD1d presentation of a sulfatide derived from myelin and it's implications for autoimmunity. J. Exp. Med. 2005;202:1517–26. doi: 10.1084/jem.20051625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wu D, Xing GW, Poles MA, et al. Bacterial glycolipids and analogs as antigens for CD1d-restricted NKT cells. Proc. Natl. Acad. Sci. USA. 2005;102:1351–56. doi: 10.1073/pnas.0408696102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Truelove S, Witts LF. Cortisone in ulcerative colitis: a final report on a therapeutic trial. Br. Med. J. 1955;2:1041–46. doi: 10.1136/bmj.2.4947.1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.De Dombal FT, Burton IL, Clamp SE, et al. Short term course and prognosis of Crohn's disease. Gut. 1974;15:435–9. doi: 10.1136/gut.15.6.435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shimamura T, Fujisawa T, Husain SR, et al. Interleukin 13 mediates signal transduction through interleukin 13 receptor α2 in pancreatic ductal adenocarcinoma: role of IL-13 Pseudomonas exotoxin in pancreatic cancer surgery. Clin. Cancer Res. 2010;16:577–86. doi: 10.1158/1078-0432.CCR-09-2015. [DOI] [PubMed] [Google Scholar]
- 11.Debinski W, Miner R, Leland P, et al. Receptor for interleukin (IL) 13 does not interact with IL4 but receptor for IL4 interacts with IL13 on human glioma cells. J. Biol. Chem. 1996;271:22428–33. doi: 10.1074/jbc.271.37.22428. [DOI] [PubMed] [Google Scholar]
- 12.Joshi BH, Puri RA, Leland P, et al. Identification of interleukin-13 receptor α2 chain overexpression in situ in high-grade diffusely infiltrative pediatric brainstem glioma. Neuro Oncol. 2008;10:265–74. doi: 10.1215/15228517-2007-066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liu Y, Goff RD, Zhou D, et al. A modified α-galactosyl ceramide for staining and stimulating natural killer T cells. J. Immunological Methods. 2006;312:34–9. doi: 10.1016/j.jim.2006.02.009. [DOI] [PubMed] [Google Scholar]
- 14.Roy KC, Maricic I, Khurana A, et al. Involvement of secretory and endosomal compartments in presentation of an exogenous self-glycolipid to type II NKT cells. J. Immunol. 2008;180:2942–50. doi: 10.4049/jimmunol.180.5.2942. [DOI] [PubMed] [Google Scholar]
- 15.Blomqvist M, Rhost S, Teneberg S, et al. Multiple tissue-specific isoforms of sulfatide activate CD1d-restricted type II NKT cells. Eur. J. Immunol. 2009;39:1726–35. doi: 10.1002/eji.200839001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jansson L, Tobias J, Jarefjäll C, et al. Sulfatide recognition by colonization factor antigen CS6 from enterotoxigenic Escherichia coli. PLoS One. 2011;4:e4487. doi: 10.1371/journal.pone.0004487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fuss IJ, Neurath M, Boirivant M, et al. Disparate CD4+ lamina propria (LP) lymphokine secretion profiles in inflammatory bowel disease. Crohn's disease LP cells manifest increased secretion of IFN-γ, whereas ulcerative colitis LP cells manifest increased secretion of IL-5. J. Immunol. 1996;157:1261–70. [PubMed] [Google Scholar]
- 18.Fichtner-Feigl S, Young CA, Kitani A, et al. IL-13 signaling via IL-13R α2 induces major downstream fibrogenic factors mediating fibrosis in chronic TNBS colitis. Gastroenterology. 2008;135:2003–13. doi: 10.1053/j.gastro.2008.08.055. [DOI] [PubMed] [Google Scholar]
- 19.Fichtner-Feigl S, Strober W, Kawakami K, et al. IL-13 signaling through the IL-13alpha2 receptor is involved in induction of TGF-beta1 production and fibrosis. Nat. Med. 2006;12:99–106. doi: 10.1038/nm1332. [DOI] [PubMed] [Google Scholar]
- 20.Kaser A, Lee AH, Franke A, et al. XBP1 links ER stress to intestinal inflammation and confers genetic risk for human inflammatory bowel disease. Cell. 2008;134:743–56. doi: 10.1016/j.cell.2008.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Olszak T, An D, Zeissig S, et al. Microbial exposure during early life has persistent effects on natural killer T cell function. Science. 2012;336:489–93. doi: 10.1126/science.1219328. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.