Supplemental Digital Content is available in the text
Abstract
Available systematic reviews showed uncertainty on the effectiveness of using acupuncture and related therapies for palliative cancer care.
The aim of this systematic review and meta-analysis was to summarize current best evidence on acupuncture and related therapies for palliative cancer care.
Five international and 3 Chinese databases were searched. Randomized controlled trials (RCTs) comparing acupuncture and related therapies with conventional or sham treatments were considered. Primary outcomes included fatigue, paresthesia and dysesthesias, chronic pain, anorexia, insomnia, limb edema, constipation, and health-related quality of life, of which effective conventional interventions are limited.
Thirteen RCTs were included. Compared with conventional interventions, meta-analysis demonstrated that acupuncture and related therapies significantly reduced pain (2 studies, n = 175, pooled weighted mean difference: −0.76, 95% confidence interval: −0.14 to −0.39) among patients with liver or gastric cancer. Combined use of acupuncture and related therapies and Chinese herbal medicine improved quality of life in patients with gastrointestinal cancer (2 studies, n = 111, pooled standard mean difference: 0.75, 95% confidence interval: 0.36–1.13). Acupressure showed significant efficacy in reducing fatigue in lung cancer patients when compared with sham acupressure. Adverse events for acupuncture and related therapies were infrequent and mild.
Acupuncture and related therapies are effective in reducing pain, fatigue, and in improving quality of life when compared with conventional intervention alone among cancer patients. Limitations on current evidence body imply that they should be used as a complement, rather than an alternative, to conventional care. Effectiveness of acupuncture and related therapies for managing anorexia, reducing constipation, paresthesia and dysesthesia, insomnia, and limb edema in cancer patients is uncertain, warranting future RCTs in these areas.
INTRODUCTION
Acupuncture is one of the major treatment modalities in Chinese medicine. It refers to a group of therapeutic techniques characterized by needle insertion into the skin, followed by either manual manipulation or electrical stimulation. Related therapies like acupoints injection and needleless procedures like moxibustion and transcutaneous electrical nerve stimulation are also often used separately or together with acupuncture. Acupuncture and related techniques have been widely used in managing various diseases and symptoms for more than 2000 years. Multiple theories were proposed to explain the mechanisms of actions, the most widely studied theory is the endorphin theory, where acupuncture stimulated release of neurotransmitter such as endorphin at spinal and supraspinal levels to modulate various physiological responses,1,2 which the physiological effects with acupuncture could be demonstrated by functional magnetic resonance imaging studies.3 On the other hand, 1 theory suggested possible association of acupuncture points with loose connective tissue anatomically.4 However, the exact mechanism remains unclear.5–7
Multidimensional factors contribute to various symptoms in cancer patients, including tumor invasion or metastasis, anemia, polypharmacy, treatment side effects, hypogonadism in male patients, autonomic dysfunction, and release of inflammatory cytokines.8–14 Fatigue is the most common complaint in palliative cancer patients. Limited pharmaceutical agents such as glucocorticoid had proved their efficacy but they were associated with profound side effects. Available evidence suggests that acupuncture and related therapies are generally safe treatment modalities when they are delivered by adequately trained practitioners.5–7 Acupuncture and related therapies are widely used in palliative cancer care among Chinese populations,15 and are gaining popularity globally. Effectiveness of these treatments, especially in the management of symptoms for which conventional medicine has limited to offer, would be of high interest among clinicians in palliative medicine. For instance, the National Institute for Health stated that acupuncture is a proven effective treatment modality for adult postoperative and chemotherapy nausea and vomiting.16 Clinical evidence on the potential effectiveness of acupuncture and related therapies for controlling fatigue, paresthesia and dysesthesias, chronic pain, anorexia, insomnia, limb edema, and constipation should be synthesized. Currently, 10 systematic reviews (SRs) have been conducted to assess the role of acupuncture and related therapies in palliative cancer care. One meta-analysis showed effectiveness of acupuncture and patient education on cancer-related fatigue.17 An SR demonstrated that acupuncture is an effective treatment for chemotherapy-induced nausea and vomiting, but its effectiveness for other areas with unmet needs is uncertain.18 Results from SRs by Lee et al19 and Bardia et al20 on treatment of cancer-related pain showed insufficient evidence to support of refute the effectiveness of acupuncture. One SR by O’Regan et al21 identified potential roles of acupuncture in treatment of pain, nausea and vomiting, xerostomia, hot flushes, fatigue, anxiety, depression, and insomnia. Nevertheless, firm conclusion could not be drawn as well.
The applicability of these available SRs is limited for a number of reasons. First, some SRs had less restrictive inclusion criteria for the study design, which included randomized controlled studies (RCTs), observational studies, and even case series studies.19,22 Including studies with less rigorous designs may jeopardize trustworthiness of the conclusion. Second, details on the baseline treatment, as well as interventions used in control groups were often not provided by either the SR authors or the primary study authors.22 Poor reporting makes it difficult to generalize evidence to clinical practice, even when the intervention is found to be effective. Lastly, many of these SRs were conducted more than 5 years ago. New primary studies have been published during the last 5 years, and an up-to-date SR focusing on this area is urgently needed.
We have conducted an updated SR on acupuncture and related therapies for symptom management in palliative cancer care. The objective of this study is to evaluate current best evidence on the potential role of acupuncture and related therapies in managing common cancer symptoms that pose substantial challenges to conventional care, including fatigue, paresthesia and dysesthesias, chronic pain, anorexia, insomnia, limb edema, constipation, and health-related quality of life. In order to overcome the shortcomings of previous SRs, strict inclusion criteria on study design and reporting quality were adopted in the current SR. Evidence from this SR may support the development of pragmatic collaboration model between conventional and complementary medical practice.
METHODS
This SR and meta-analysis was reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses checklist. Ethical approval was not necessary since all the analyses were conducted based on data retrieved from previous published SRs and trials.
Inclusion Criteria
To be included, the primary studies have to satisfy the following criteria:
Randomized controlled trials comparing acupuncture and/or related therapies with a valid comparison that allows evaluation of the net effect of acupuncture and/or related therapies.
Patients who are diagnosed with any type of cancer.
Any form of acupuncture or related techniques were considered, including needle-based acupuncture (including electroacupuncture), as well as other techniques, including auricular acupuncture, laser acupuncture, acupressure, acupoints injection, moxibustion, and transcutaneous electrical nerve stimulation.
Randomized controlled trials with control groups that have used any type of interventions without acupuncture or related treatments listed above. Control interventions may include conventional treatment, behavioral therapies, Chinese herbal medicine treatment, sham acupuncture, waiting list, or no treatment.
Randomized controlled trials reporting 1 or more of the following predefined primary outcomes measured with validated instruments were included: fatigue, paresthesia and dysesthesias, chronic pain, anorexia, insomnia, limb edema, constipation, and health-related quality of life.
Randomized controlled trials that reported details on treatment prescription and follow-up duration for both acupuncture and control group to ensure the usefulness of synthesized evidence.
Literature Search
Comprehensive literature search was conducted by searching both international and Chinese databases, including the Cochrane Central Register of Controlled Trials, MEDLINE, Embase, CINAHL Plus, the Allied and Complementary Medicine Database,23 Chinese Biomedical Databases, Wanfang Digital Journals, and Taiwan Periodical Literature Databases. Specialized search filter for clinical trials were used in MEDLINE24 and Embase.25 Detailed search strategies and related results for each database are reported in Appendix 1. No language restriction was set during the literature search.
Literature Selection, Data Extraction, and Risk of Bias Assessment
All the retrieved citations were screened and assessed for their eligibility according to the inclusion criteria. The following data were extracted from each included RCT: characteristics of the study, including first author's name, year of publication, country in which the trial was conducted, eligibility criteria, and sample size; details on patient characteristics, acupuncture and related therapies, and control interventions and outcomes; effect on each interested outcomes and adverse effects related to acupuncture and related therapies; and information on risk of bias.
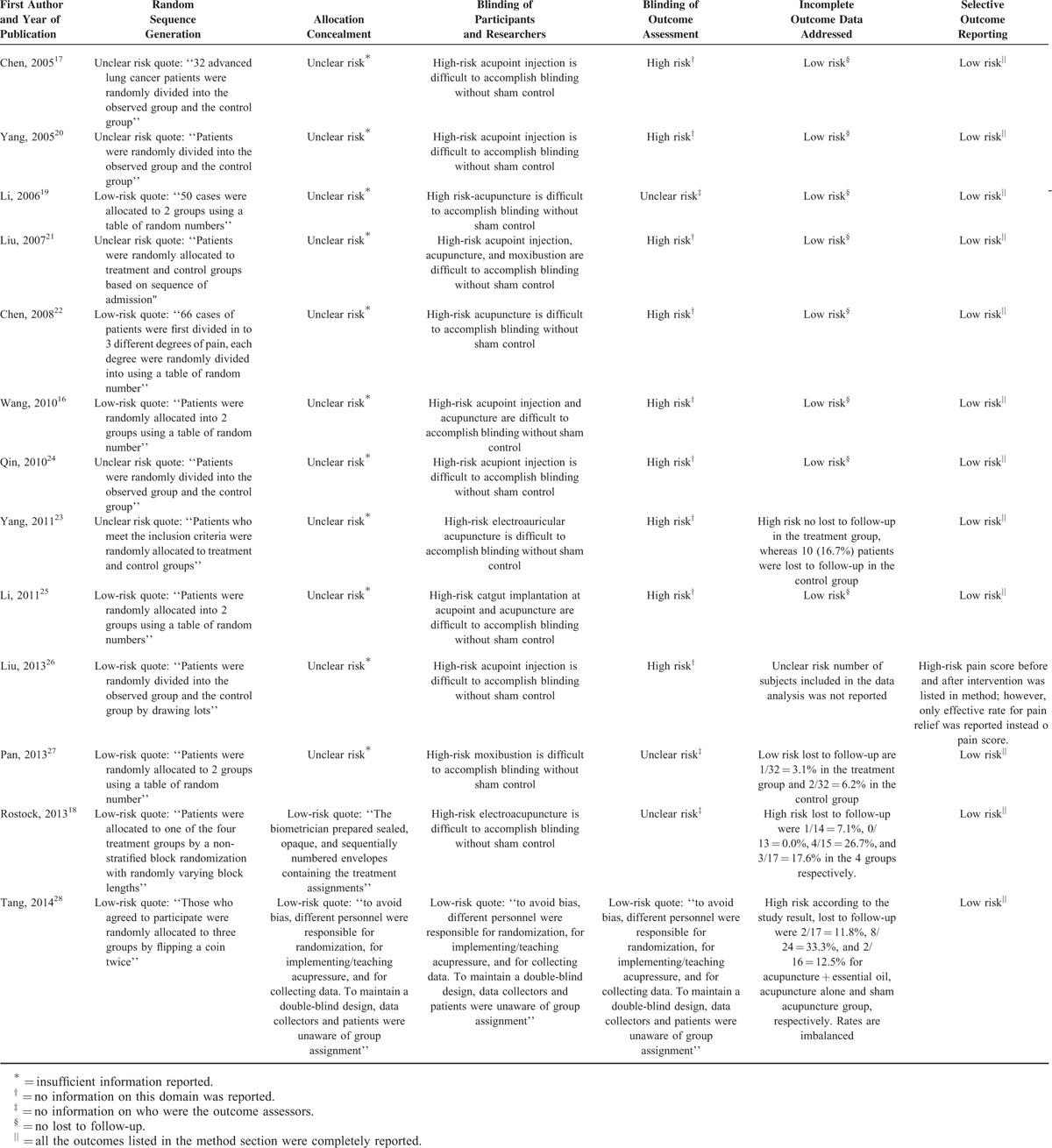
Risk of bias of included RCTs were assessed with the latest version of the Cochrane risk of bias tool,26 which assessed risk of bias in the domains of sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessments, incomplete outcome data, and selective outcome reporting. Each domain was judged to have low, high, or unclear risk of bias according to information provided by RCT authors.
Literature selection, data extraction, and risk of bias assessment were performed by 2 researchers (XW, XL) independently, with disagreement resolved by discussion and consensus. A third reviewer (VCC) was consulted if disagreement could not be resolved, and his judgment was used as the final decision.
Data Analysis
Effectiveness was measured with relative risk (RR) for dichotomous data and standardized mean difference, or weighted mean difference for continuous data. Total 95% confidence interval (CI) was used to account for the uncertainty of the estimation. Random effects model was used to account for the variations across trials27 during meta-analysis. I2 statistic was used to measure the heterogeneity across trials. I2 < 25% was considered as low level of heterogeneity, 25% to 50% as moderate level, and larger than 50% as high level.28 Funnel plot would be used to detect the potential presence of publication bias if more than 10 trials were available for 1 outcome.29 Stata Version 13.0 (STATA Corporation, College Station, TX) was used for the data analyses, with a 2-tailed significance level of 0.05. The protocol of this SR has been registered in PROSPERO (http://www.crd.york.ac.uk/PROSPERO/DisplayPDF.php?ID=CRD42015023934).
RESULTS
Study Selection
A total of 1704 citations were retrieved from the databases. Total 237 duplicates and 1402 citations were excluded based on title and abstract screening, and 65 citations were left for full-text assessment. Fifty-two were excluded for the following reasons: did not report prespecified outcomes (n = 20); the add-on effect of acupuncture could not be evaluated as it was not separated from other treatments (n = 7); no details reported on baseline or acupuncture treatment (n = 7); no acupuncture prescribed in the treatment group (n = 3); not a RCT (n = 5); did not use validated instruments for outcome assessment (n = 3); no details reported on time point for outcome measurement (n = 4); and recruited both cancer and noncancer patients (n = 2). At last, 13 RCTs30–42 were included. Details on the study selection process can be found in Figure 1.
FIGURE 1.

Flowchart of literature selection on randomized controlled trials of acupuncture for symptom management for cancer palliative care.
Characteristics of Included Randomized Controlled Trials
The 13 RCTs were published between 2005 and 2014, with 11 of them conducted in Mainland China, 1 in Taiwan and 1 in Germany. Eight RCTs included various types of cancer patients, and the remaining 5 RCTs were conducted in patients with gastric cancer (n = 2), liver cancer (n = 1), lung cancer (n = 1), and nonsmall cell lung cancer (n = 1). Various acupuncture modalities were used among the 13 RCTs, including acupoint injection (n = 4), needle acupuncture (n = 2), electroacupuncture (n = 2), and moxibustion (n = 1), the remaining 4 trials included more than 1 acupuncture modalities. As for the comparisons, 7 RCTs assessed the effectiveness of acupuncture and related therapies by comparing them with conventional interventions, 5 investigated the effect of acupuncture and related therapies as an add-on to conventional care, and the remaining trial assessed the efficacy of acupuncture by comparing it to sham acupuncture.
The most frequently reported outcome was pain (8 trials), followed by quality of life (3 trials). Respectively, 1 RCT reported evidence on constipation, anorexia, paresthesia and dysesthesia, fatigue, and insomnia. Details on characteristics of included RCTs are shown in Table 1.
TABLE 1.
Basic Characteristic of Included Randomized Controlled Trials on Acupuncture and Related Therapies for Symptom Management in Cancer Palliative Care

Risk of Bias of Included Randomized Controlled Trials
Majority of included RCTs had low risk of bias in the domains of sequence generation (8 trials), incomplete outcome data (9 trials), and selective outcome reporting (12 trials). However, methods on allocation concealment and blinding were poorly reported. Only 2 RCTs were judged to have low risk of bias for allocation concealment, whereas the remaining 11 had unclear risk of bias. Due to difficulties in blinding and subjective nature of interested outcomes, we judged 12 RCTs as having high risk of bias for blinding of participants and personnel, and 8 as having high risk of bias for blinding of outcome assessment. Only 1 RCT had low risk of bias for the 2 blinding-related domains. Details are reported in Table 2.
TABLE 2.
Risk of Bias of Included Randomized Controlled Trials on Acupuncture and Related Therapies for Symptom Management in Cancer Palliative Care
EFFECTS OF ACUPUNCTURE AND RELATED THERAPIES
Pain
Eight RCTs assessed the effect of acupuncture for reducing pain in cancer patients. Two RCTs31–36 measured pain with numerical rating scale (NRS), which measured pain with a 0 (no pain) to 10 (most intolerable pain) scale. Meta-analysis showed that, compared with conventional medicine (morphine sulfate controlled-release tablets or World Health Organization's 3-step ladder for cancer pain relief), acupuncture and related therapies significantly reduced pain (n = 175, weighted mean difference: −0.76, 95% CI: −0.14 to −0.39, I2 = 0.0%) (Figure 2). Two RCTs31,41 also suggested that acupuncture and related therapies had significantly shorter analgesic onset time as compared with conventional medicine (morphine) (Table 3). An RCT41 reported data on analgesic duration has shown that, when compared with intramuscular injection of morphine, acupoint injection of morphine had 7 additional hours of analgesic duration (n = 115, mean difference [MD]: 7.29 hours, 95% CI: 6.27–8.31 hours) in patients with advance cancer (Table 3). Among the remaining 5 RCTs,32,35,37,38,40 although pain was measured with visual analog scale (VAS) or NRS, results were reported as proportion of patient achieving satisfactory relief instead of VAS or NRS changes. Better effectiveness was described in acupuncture groups among all 5 studies, but no statistical significance was reached. Due to differences in the cutoff used to define satisfactory relief, data were not pooled in those 5 studies (Table 4).
FIGURE 2.

Meta-analysis on the effectiveness of acupuncture and related therapies for reducing pain score in cancer patients as compared with conventional medicine (comparison: acupuncture and related therapies versus conventional medicine).
TABLE 3.
Effectiveness of Acupuncture and Related Therapies for Symptom Management in Cancer Palliative Care: Outcomes Measured as Continuous Data

TABLE 4.
Effectiveness of Acupuncture and Related Therapies for Symptom Management in Cancer Palliative Care: Outcomes Measured as Dichotomous Data

Quality of Life
Four RCTs provided evidence on the effectiveness of acupuncture and related therapies for improving quality of life in cancer patients. Two studies34,42 reported quality of life-related scores measured with validated scales (Karnofsky Performance Status and Quality of Life Scale for cancer patients). Meta-analysis showed that the combination use of acupuncture and related therapies and Chinese herbal medicine slightly improved quality of life in patients with gastrointestinal cancer (n = 111, standardized mean difference: 0.75, 95% CI: 0.36–1.13) (Figure 3). Another RCT32 (n = 32) reported that nonsmall cell lung cancer patients who received the combination of acupoints injection of Astragalus extract with 3-step analgesic ladder medications had a significantly better quality of life than patients who received 3-step analgesic ladder medications only (33.3% versus 14.3%, RR: 2.00, 95% CI: 1.46–8.70) (Table 4). Another RCT33 (n = 60) failed to find any difference in quality of life among cancer patients who received electroacupuncture, hydroelectric baths, vitamin B or vitamin B placebo.
FIGURE 3.

Meta-analysis on the add-on effect of acupuncture and related therapies for improving quality of life score in cancer patients as compared with conventional care alone (comparison: acupuncture and related therapies + conventional care versus conventional care alone).
Anorexia
One RCT34 (n = 50) assessed the add-on effect of needle acupuncture on top of compounds Kushen injection for anorexia in patients with advanced gastrointestinal cancer. After 4 weeks treatment, a higher proportion of patients in the combined treatment group showed improvement on anorexia (59.3%) as compared with those who only received compounds Kushen injection (17.4%). However, the difference did not reach statistical significance (RR: 2.51, 95% CI: 0.94–6.72).
Constipation
An RCT39 (n = 100) assessed the effectiveness of acupoint injection with vitamin B as compared with oral phenolphthalein for reducing constipation caused by slow-release morphine tablets. A higher proportion of patients in the acupoint injection group showed improvement (92.0% versus 70.0%). However, the difference was of no statistical significance (RR: 1.16, 95% CI: 0.84–1.63).
Fatigue
A 3-arm RCT43 (n = 57) explored the efficacy of acupressure plus essential oil, and acupressure alone for cancer-related fatigue by comparing them with sham acupressure in lung cancer patients. Fatigue was measured with Chinese versions of the 37 items Tang Fatigue Rating Scale.44 Each item is rated on a Likert scale ranging from 1 to 10, with higher scores indicating more severe fatigue. Data from the acupressure plus essential oil group and acupressure only groups were combined during data analysis. After 5 months of treatment, patients in the acupressure plus essential oil group and acupressure group showed significantly lower fatigue score (MD: −0.63, 95% CI: −1.22 to −0.04). We conducted sensitivity analysis within study by excluding the acupressure group that had a high lost to follow-up. Significant difference was still observed between acupressure plus essential oil and sham acupressure group (Table 3).
Insomnia
The same 3-arm RCT43 also investigated the efficacy of acupressure plus essential oil, and acupressure alone for insomnia in lung cancer patients. Sleep quality was measured with the 19-item Pittsburgh Sleep Quality Index.45 With each item rated on a 0 to 3 Likert scale, a lower total score indicates better sleep quality. Results showed that after 5-month treatment, patients in the acupressure plus essential oil and acupressure only group had better quality of sleep than that of patients in the sham acupressure group (Pittsburgh Sleep Quality Index score: 7.5 versus 10.1). However, this difference did not reach statistical significance (MD: −0.57, 95% CI: −1.16 to 0.02) (Table 3).
Paresthesia and Dysesthesia
A 4-arm RCT33 compared electroacupuncture with hydroelectric baths, vitamin B and vitamin B placebo in managing chemotherapy-induced peripheral neuropathy (CIPN) including paresthesia among cancer patients. Severity of CIPN was measured with a NRS, scoring from 0 to 10, with a higher score indicating higher severity of CIPN. During analysis, data from hydroelectric baths and vitamin B groups were combined. When compared with electroacupuncture group, no significant difference was found at follow-up on 21 days (MD: −0.13, 95% CI: −0.78 to 0.51) or 84 days (MD: −0.09, 95% CI: −0.73 to 0.55).
Adverse Events
Four RCTs31,35,41,42 reported information on adverse events. Patients in control group generally had more adverse events than those in the acupuncture group. However, only 231,42 RCTs reported acupuncture induced side effects, including dizziness during needle insertion (5/30), subcutaneous bleeding (3/30), and mild burn, which was observed in few cases when moxibustion was inappropriately conducted, which was judged by the original RCT.27
DISCUSSION
Results from 13 RCTs with 969 cancer patients were summarized in this SR. Acupuncture and related therapies significantly reduced pain in cancer patients with a quicker analgesic effect and longer analgesic duration when compared with conventional medicine. Acupressure or acupressure plus essential oil showed significant efficacy in reducing fatigue in lung cancer patients when compared with sham acupressure. Existing evidence also suggested that the additional use of acupuncture and related therapies with conventional or Chinese herbal medicine might improve quality of life in cancer patients. Overall, acupuncture and related therapies only caused minor side effects. On the other hand, available evidence did not show any differences on the following comparisons: the combined use of acupuncture and conventional care versus conventional care alone for treating anorexia; acupuncture and related therapies versus conventional medicine for reducing constipation, paresthesia and dysesthesia; and acupressure or acupressure plus essential oil versus sham acupressure for improving insomnia.
This SR has presented an updated view on the clinical applicability of acupuncture and related therapies for symptom management, especially in controlling pain and fatigue. Previous SRs19,20,46 showed inconclusive results for the efficacy of acupuncture and related therapies in cancer pain control due to a lack of “high quality” studies. Results from our SR suggested clinicians may consider acupuncture and related therapies for cancer related pain, in particular when pain control is unsatisfactory under conventional care, or when patients are experiencing significant side effects induced by analgesic medications. Regarding alleviation of cancer-related fatigue, 1 previous meta-analysis17 demonstrated statistical significant improvement with acupuncture and patient education when compared with conventional care. However, whether the effect was attributable to acupuncture or patient education could not be well delineated. Fatigue is a well acknowledged undertreated symptom in cancer patients due to lack of effective options in conventional medicine.47 Our results suggest the practice of acupressure alone or in combination with essential oil can be an alternative or adjuvant treatment for cancer-related fatigue.
Risk of bias among the included RCTs should be carefully assessed. The majority of them did not provide information on how allocation concealment and blinding were ensured, results in high risk of ascertainment bias. On the other hand, bias could be further reduced if the outcomes were assessed by blinded29 investigators.29 Unfortunately, the majority of included RCTs did not specify whether the investigators analyzing outcomes were blinded except for 1 trial on fatigue and insomnia.30 These reflected poor adherence of the Consolidated Standards of Reporting Trials reporting requirements48 among these RCTs.30
Another limitation of the reviewed evidence is that, due to small number of included studies for each outcome, we are unable to evaluate the presence or absence of publication bias. The majority of the included studies were conducted in Chinese populations either from Mainland China or Taiwan. Evidence users should consider potential heterogeneity among different ethnicities and settings when adopting acupuncture and related therapies for their own practice.
Based on limitations of the included RCTs, several recommendations are made for further research. First, with the emergence of integrative medicine, acupuncture and related therapies are usually used as an adjuvant therapy on top of conventional care in real clinical settings. Hence, comparing acupuncture alone with standard care or sham acupuncture alone may only generate results with limited external validity. Conducting pragmatic trials that compare acupuncture plus standard care versus standard care alone may provide results that can directly inform clinical practice.46 Second, future RCTs should use validated instruments for measuring outcomes. Amendments of instruments were not uncommon among included trials and this practice should be discouraged. For example, although all the 8 RCTs that reported data on pain used VAS or NRS, 5 of them summarized their results as dichotomous data according to self-developed rules. This reduces the interpretability of their results, and reporting bias of the outcomes is highly suspected. Third, future trials should evaluate the effect of acupuncture and related therapies in managing other important symptoms, including limb edema of which we did not locate any RCTs. Lastly, future RCTs should report adverse effect comprehensively so as to facilitate the safety assessment.
In conclusion, our meta-analyses demonstrated that acupuncture and related therapies showed a significant analgesic effect in terms of reducing pain score, providing quicker analgesic effect, and longer analgesic duration in cancer patients when compared with conventional medicine alone. However, these results are not in line with the rest of the evidence body in the area.49 Acupuncture and related therapies can be considered as an adjunct, instead of a replacement to, conventional pain management protocol for cancer palliative care patients.
Acupressure or acupressure plus essential oil showed efficacy in improving fatigue in lung cancer patients. The combined use of acupuncture and related therapies with conventional medications or Chinese herbal medicine can improve quality of life among cancer patients. The effectiveness of acupuncture and related therapies in treating anorexia, constipation, paresthesia and dysesthesia, insomnia, and limb edema in cancer patients is unclear. As a relatively safe modality, acupuncture could be considered as an adjuvant options for the management of pain, fatigue, and improving quality of life in cancer patients. On the other hand, safety of acupoint injection and moxibustion would require further investigation. Future research should pay attention on: choosing appropriate control interventions that reflect real clinical practice; using validated outcome measurement instrument without unwarranted amendments; blinding the outcome assessors to reduce potential bias; and reporting the RCTs in accordance to the Consolidated Standards of Reporting Trials statement.48
Supplementary Material
Footnotes
Abbreviations: CI = confidence interval, CIPN = chemotherapy-induced peripheral neuropathy, NRS = numerical rating scale, PSQI = Pittsburgh Sleep Quality Index, RCT = randomized controlled trial, RR = relative risk, SR = systematic review, TFRS = Tang Fatigue Rating Scale, VAS = visual analog scale.
CHL, XW, HC, and RL contributed equally to the article.
This systematic review was funded by Hospital Authority of Hong Kong (Reference number: 8110016609).
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Andersson S, Lundeberg T. Acupuncture: from empiricism to science: Functional background to acupuncture effects in pain and disease pain and disease. Med Hypotheses 1995; 45:271–281. [DOI] [PubMed] [Google Scholar]
- 2.Han JS, Terenius L. Neurochemical basis of acupuncture analgesia. Annu Rev Pharmacol Toxicol 1982; 22:193–220. [DOI] [PubMed] [Google Scholar]
- 3.Cho ZH, Chung SC, Jones JP, et al. New findings of the correlation between acupoints and corresponding brain cortices using functional MRI. Proc Natl Acad Sci 19981998; 95:2670–2673. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 4.Langevin HM, Yandow JA. Relationship of acupuncture points and meridians to connective tissue planes. Anat Rec 2002; 269:257–265. [DOI] [PubMed] [Google Scholar]
- 5.Yamashita H, Tsukayama H, Tanno Y, et al. Adverse events in acupuncture and moxibustion treatment: a six-year survey at a national clinic in Japan. J Altern Complement Med 1999; 5:229–236. [DOI] [PubMed] [Google Scholar]
- 6.MacPherson H, Thomas K, Walters S, et al. The York acupuncture safety study: prospective survey of 34 000 treatments by traditional acupuncturists. Br Med J 2001; 323:486–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.White A, Hayhoe S, Hart A, et al. Adverse events following acupuncture: prospective survey of 32 000 consultations with doctors and physiotherapists. Br Med J 2001; 323:485–486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Crawford J, Cella D, Cleeland CS, et al. Relationship between changes in hemoglobin level and quality of life during chemotherapy in anemic cancer patients receiving epoetin alfa therapy. Cancer 2002; 95:888–895. [DOI] [PubMed] [Google Scholar]
- 9.Del Fabbro E, Hui D, Nooruddin ZI, et al. Associations among hypogonadism, C-reactive protein, symptom burden, and survival in male cancer patients with cachexia: a preliminary report. J Pain Symptom Manage 2010; 39:1016–1024. [DOI] [PubMed] [Google Scholar]
- 10.Dev R, Hui D, Del Fabbro E, et al. Association between hypogonadism, symptom burden, and survival in male patients with advanced cancer. Cancer 2014; 120:1586–1593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Walsh D, Nelson K. Autonomic nervous system dysfunction in advanced cancer. Support Care Cancer 2002; 10:523–528. [DOI] [PubMed] [Google Scholar]
- 12.Lee BN, Dantzer R, Langley KE, et al. A cytokine-based neuroimmunologic mechanism of cancer-related symptoms. Neuroimmunomodulation 2004; 11:279–292. [DOI] [PubMed] [Google Scholar]
- 13.Ahlberg K, Ekman T, Gaston-Johansson F. Assessment and management of cancer related fatigue in adults. Lancet 2003; 362:640–650. [DOI] [PubMed] [Google Scholar]
- 14.Kurita GP, Sjøgren P, Ekholm O, et al. Prevalence and predictors of cognitive dysfunction in opioid- treated patients with cancer: a multinational study. J Clin Oncol 2011; 29:1297–1303. [DOI] [PubMed] [Google Scholar]
- 15.Johnstone PA, Polston GR, Niemtzow RC, et al. Integration of acupuncture into the oncology clinicy. Palliat Med 2002; 16:235–239. [DOI] [PubMed] [Google Scholar]
- 16.NCDP A. NIH Consensus Conference. Acupuncture. J Am Med Assoc 1998; 280:1518–1524. [PubMed] [Google Scholar]
- 17.Zeng Y, Luo T, Finnegan-John J, et al. Meta-analysis of randomized controlled trials of acupuncture for cancer-related fatigue. Integr Cancer Ther 2013; 13:193–200. [DOI] [PubMed] [Google Scholar]
- 18.Towler P, Molassiotis A, Brearley SG. What is the evidence for the use of acupuncture as an intervention for symptom management in cancer supportive and palliative care: an integrative overview of reviews. Support Care Cancer 2013; 21:2913–2923. [DOI] [PubMed] [Google Scholar]
- 19.Lee H, Schmidt K, Ernst E. Acupuncture for the relief of cancer-related pain: a systematic review. Eur J Pain 2005; 9:437–444. [DOI] [PubMed] [Google Scholar]
- 20.Bardia A, Barton DL, Prokop LJ, et al. Efficacy of complementary and alternative medicine therapies in relieving cancer pain: a systematic review. J Clin Oncol 2006; 24:5457–5464. [DOI] [PubMed] [Google Scholar]
- 21.O’Regan D, Filshie J. Acupuncture and cancer. Auton Neurosci 2010; 157:96–100. [DOI] [PubMed] [Google Scholar]
- 22.Chao L-F, Zhang A, Liu H-E, et al. The efficacy of acupoint stimulation for the management of therapy-related adverse events in patients with breast cancer: a systematic review. Breast Cancer Res Treat 2009; 118:255–267. [DOI] [PubMed] [Google Scholar]
- 23.Melamed E, Ziv I, Djaldetti R. Management of motor complications in advanced Parkinson's disease. Mov Disord 2007; 22:S379–S384. [DOI] [PubMed] [Google Scholar]
- 24.Haynes RB, McKibbon KA, Wilczynski NL, et al. Optimal search strategies for retrieving scientifically strong studies of treatment from Medline: analytical survey. Br Med J 2005; 330:1179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wong SSL, Wilczynski NL, Haynes RB. Developing optimal search strategies for detecting clinically sound treatment studies in EMBASE. J Med Libr Assoc 2006; 94:41–47. [PMC free article] [PubMed] [Google Scholar]
- 26.Higgins JPT, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. Br Med J 2011; 343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Riley RD, Higgins JPT, Deeks JJ. Interpretation of random effects meta-analyses. Br Med J 2011; 342:d549. [DOI] [PubMed] [Google Scholar]
- 28.Higgins JPT, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. Br Med J 2003; 327:557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.The Cochrane Collaboration, Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. 2011; Available at: www.cochrane-handbook.org.: Accessed March 2011. [Google Scholar]
- 30.Tang W-R, Chen W-J, Yu C-T, et al. Effects of acupressure on fatigue of lung cancer patients undergoing chemotherapy: An experimental pilot study. Complement Ther Med 2014; 22:581–591. [DOI] [PubMed] [Google Scholar]
- 31.Wang SC, Yin HB, Li WF. Acupuncture combined with point injection of Chinese angelica injection for pain of advanced stomach carcinoma. Chin J Cancer Prev Treat 2010; 17:1487–1488. [Google Scholar]
- 32.Chen WF. Clinical observation on effect of combined acupoint-injection and chemotherapy in the treatment of advanced lung cancer. Tian Jin Univ Chin Med 2005; 1–44. [Google Scholar]
- 33.Rostock M, Jaroslawski K, Guethlin C, et al. Chemotherapy-induced peripheral neuropathy in cancer patients: a four-arm randomized trial on the effectiveness of electroacupuncture. Evid Based Complement Alternat Med 2013; 2013:349653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.2006; Li PX, Jia YJ. Treatment of aneroxia in late stage tumor of digestive tract by acupuncture: a clinical observation of 27 casesJT N J Tradit Chin Med. 38:67–68. [Google Scholar]
- 35.Yang XL, Zhu YQ. Effect of injecting tramadol at Zusanli acupoint on patients suffered from digestive system cancer pain. Chin J Clin Med 2005; 4:22–23. [Google Scholar]
- 36.Liu XY. Treatment of pain in liver cancer by acupuncture and acupoints injection. Shan Xi J Chin Med 2007; 28:1125–1126. [Google Scholar]
- 37.Chen ZJ, Guo YP. Observation on the therapeutic effect of acupuncture at pain points on cancer pain. Chin Acupunct Moxibustion 2008; 28:251–253. [PubMed] [Google Scholar]
- 38.Yang FY, Peng AL. Observations on electro-auricular acupuncture combined with morphine for treatment of cancer pain. Chin Pract J Rural Doct 2011; 18:56–57. [Google Scholar]
- 39.Qin MX, Xi CY, Zhou H. Observation on effect of acupoint injection for treatment of morhine induced constipation. J Qiqihar Med Coll 2010; 31:3921. [Google Scholar]
- 40.Li B, Zhang XF, Na LY. Observation on the effect of catgut implantation at acupoint and acupuntcure for treatment of cancer pain. Mod Oncol 2011; 19:1417–1418. [Google Scholar]
- 41.Liu XF. Observation on morphine injection at Zusanli for treatment of cancer pain. J N Chin Med 2013; 45:128–129. [Google Scholar]
- 42.Pan CF, Xue HY, Shen KP, et al. Study of moxibustion for improvement in immunologic fuction and quality of life in gastric cancer patients. Shanghai J Acupunct Moxibustion 2013; 32:726–728. [Google Scholar]
- 43.Tang WR, Chen WJ, Yu CT, et al. Effects of acupressure on fatigue of lung cancer patients undergoing chemotherapy: an experimental pilot study. Complement Ther Med 2014; 22:581–591. [DOI] [PubMed] [Google Scholar]
- 44.Tang WR, Yu CY, Yeh SJ. Fatigue and its related factors in patients with chronic heart failure. J Clin Nurs 2010; 19:69–78. [DOI] [PubMed] [Google Scholar]
- 45.Wang R-C, Wang S-J, Chang Y-C, et al. Mood state and quality of sleep in cancer pain patients: a comparison to chronic daily headache. J Pain Symptom Manage 2007; 33:32–39. [DOI] [PubMed] [Google Scholar]
- 46.Paley CA, Johnson MI, Tashani OA, et al. Acupuncture for cancer pain in adults. Cochrane Database Syst Rev 2015; 10:CD007753.doi: 10.1002/14651858.CD007753.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Koornstra RHT, Peters M, Donofrio S, et al. Management of fatigue in patients with cancer: a practical overview. Cancer Treat Rev 2014; 40:791–799. [DOI] [PubMed] [Google Scholar]
- 48.Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomized trials. Ann Intern Med 2010; 152:726–732. [DOI] [PubMed] [Google Scholar]
- 49.Wu XY, Chung VCH, Hui EP, et al. Effectiveness of acupuncture and related therapies for palliative care of cancer: overview of systematic reviews. Sci Rep 2015; 5:16776. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


