Supplemental Digital Content is available in the text
Abstract
18F-fluorodeoxyglucose positron emission tomography—an established modality for evaluating malignancies—exhibits increased uptake under inflammatory conditions.
A 21-year-old man came to our hospital with persistent pain in his right lower quadrant of abdomen for more than 1 month, but had no diarrhea, fever, chills, weight loss, or other constitutional symptoms. Colonoscopy analysis showed no organic diseases in his colorectum. Ultrasound results revealed multiple enlarged lymph nodes in the bilateral neck, axilla, and groin. Positron emission tomography analysis was performed and showed intense 18F-fluorodeoxyglucose accumulation in the bilateral neck, supraclavicular, pulmonary hilar, mediastinum, gastric paracardial, and mesenterium lymph node. These findings were considered typical for lymphoma. To confirm the diagnosis, we obtained a diagnostic biopsy in the left supraclavicular lymph node. The diagnosis of tuberculosis was confirmed in the final pathology.
This uncommon case underscores the necessity of considering lymph node tuberculosis as a possible differential diagnosis in lymphoma.
INTRODUCTION
Tuberculosis (TB) remains a common infectious disease of a significant medical burden, especially in developing countries.1,2 TB mainly affects the pulmonary system, but also involves extrapulmonary sites, including lymph nodes. On clinic, TB involving lymph node, but without pulmonary involvement, may present with fever, weight loss, pain, or without any symptoms, similar to lymphoma. Moreover, differentiating between systemic lymph node TB and lymphoma is difficult because both diseases can lead to hypermetabolic lesions on 18F-fluorodeoxyglucose positron emission tomography (18F-FDG PET/CT) analysis.3,4 This article reported a case of systemic lymph node TB mimicking lymphoma on 18F-FDG PET/CT and presented several differential diagnosis criteria.
CASE REPORT
A 21-year-old man presented to our hospital with pain in his right lower quadrant of abdomen that persisted for more than 1 month, but without fever and diarrhea. Ultrasound assessment showed multiple enlarged lymph nodes in the bilateral neck, axilla, and groin, without prompting appendicitis or aberrantly occupying lesions in his abdomen. Colonoscopy analysis showed no organic disease in his colorectum. The PET/CT scan (injection of 5.19 mCi 18F-FDG) showed systemic multiple lymph node with intense FDG accumulation on coronal (Figure 1A) and sagittal planes (Figure 1B), Supplementary Figures 1 and 2.
FIGURE 1.
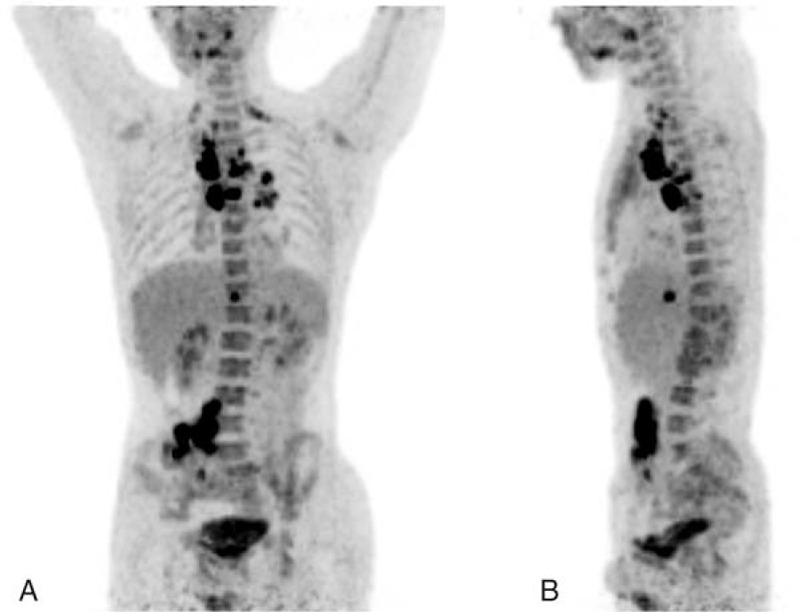
18F-FDG PET/CT scan showed systemic multiple lymph node with intense FDG accumulation on coronal (A) and sagittal planes (B). 18F-FDG PET/CT = 18F-fluorodeoxyglucose positron emission tomography.
Selected transaxial PET/CT slices of the bilateral neck lymph node (Figure 2A), supraclavicular lymph node (Figure 2B), mediastinal lymph nodes (Figure 2C), pulmonary hilar lymph node (Figure 2D), paracardial lymph nodes (Figure 2E), and mesenteric lymph nodes (Figure 2F) showed intense FDG accumulation. The SUVmax values (maximum standardized uptake value) were 9.7 and 8.7 in the mediastinal lymph nodes (Figure 2C) and mesenteric lymph nodes (Figure 2F), respectively. Almost all of the lymph nodes indicated uniform intense FDG accumulation, lacking the characteristic diffuse accumulation. These PET/CT findings suggested possible malignancy. The medical history of the patient was unremarkable, and the patient had never been diagnosed with pulmonary TB. Moreover, there was no calcification or necrosis in the hypermetabolic lymph nodes and no obvious pulmonary abnormalities on CT scans. Furthermore, PET/CT images did not present any obvious features, such as caseous necrosis, which indicates lymph node TB. Based on the medical history and imaging findings of the patient, lymphoma was first considered. To confirm the diagnosis, we obtained a diagnostic biopsy in the left supraclavicular lymph node. Histopathological examination showed central caseous necrosis surrounded by granulomatous inflammation (Figure 3). The final pathological diagnosis was lymph node TB. The patient received a series of treatments for TB and demonstrated satisfactory clinical recovery during the follow-up.
FIGURE 2.
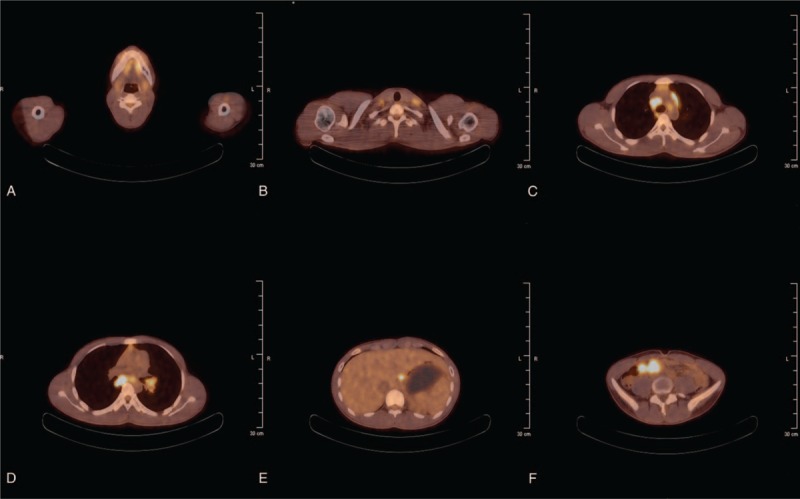
Selected transaxial 18F-FDG PET/CT slices of the bilateral neck lymph node (A), supraclavicular lymph node (B), mediastinal lymph node (C), pulmonary hilar lymph node (D), paracardial lymph node (E), and mesenteric lymph node (F) that showed intense FDG accumulation. The SUVmax values are 9.7 and 8.7 in the mediastinal lymph nodes (C) and mesenteric lymph nodes (F). 18F-FDG PET/CT = 18F-fluorodeoxyglucose positron emission tomography.
FIGURE 3.
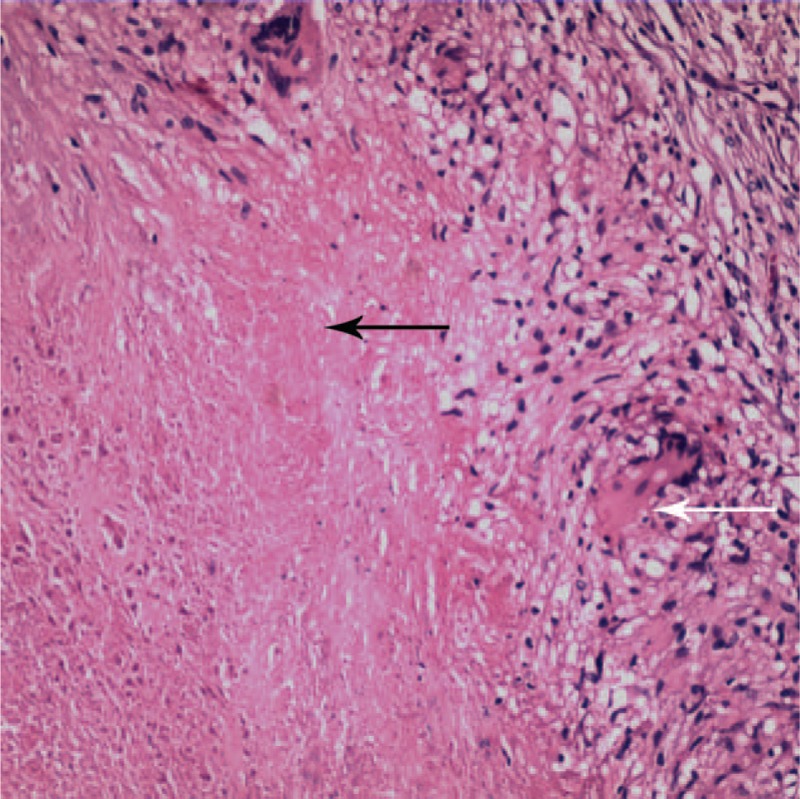
Histopathological examination of the left supraclavicular lymph node showed caseous necrosis (black arrow) and multinucleated giant cells (white arrow). The final diagnosis was lymph node tuberculosis.
A written informed consent for the case report was obtained from the patient. The consent procedure was approved by the Ethics Committee of the First Affiliated Hospital of Wenzhou Medical University.
DISCUSSION
The global epidemic of TB remains a major health problem worldwide. In 2013, an estimated 9 million people developed TB, with 1.5 million deaths associated with this disease.1,2 The main form of this disease is pulmonary TB, which enables the transmission of the infection to susceptible hosts. A study in the Australian state showed that lymph nodes are the second most common site of infection after lungs, and a common infection site in 25% of all TB cases and 51% of TB cases with extrapulmonary involvement.5 China suffers from a large burden associated with TB, with huge health and economic losses; the number of patients with TB is the second highest worldwide, and around 250 000 patients die of TB every year.6
Tuberculosis caused by Mycobacterium tuberculosis involves any body system, and leads to coughing, fever, weight loss, abdominal pain, and other nontypical symptoms. Although an increasing number of studies focused on the transmission, diagnosis, and treatment of TB, issues on how to effectively decrease the incidence of and eventually eradicate TB remain debatable.
Positron emission tomography is a diagnostic technology for tumor detection, staging, therapeutic monitoring, and follow-up evaluation for the treatment and management of various malignant tumors.7,8 However, the use of 18F-FDG PET/CT imaging in tumor diagnosis is limited by the fact that FDG is absorbed not only by tumor cells but also by macrophages, granulation, and inflammatory tissues.9
On clinic, TB occurring in lymph nodes usually manifests no typical symptoms. Hence, the diagnosis of lymph node TB is difficult, especially in the absence of pulmonary manifestations and medical history of TB. Furthermore, lymphoma also has no typical symptoms and may manifest with enlarged lymph nodes, fever, drenching sweats, weight loss, itching, and feeling of tiredness. The enlarged lymph nodes are usually painless. Therefore, differentiating between systemic lymph node TB and lymphoma is difficult. Chen et al10 reported a similar case in which TB mimics lymphoma on 18F-FDG PET/CT evaluation; in this case, the accurate diagnosis was confirmed by sputum culture. This case exhibited typical symptom of TB, such as afternoon chills, fever, and weight loss; by contrast, the present case manifested persistent pain in his abdomen only. Therefore, our case demonstrated more subtle symptoms. To our knowledge, we sum up the following 4 differential diagnosis criteria:
Caseous necrosis is an important characteristic of TB; hence, the central part of lymph node has no obvious FDG uptake, whereas lymphoma shows uniform intense FDG accumulation. This different FDG uptake in PET/CT imaging is a significant diagnostic characteristic to identify lymph node TB.
The 2 diseases also differ in terms of the location of lymph nodes. In lymph node TB, most lymph nodes with intense accumulation are clustered in the liver portal area, pulmonary hilar area, and neck area. By contrast, lymph nodes with intense accumulation suffering from lymphoma are more widely distributed.
Lymph node TB usually has no obvious liver or splenic space-occupying lesions, whereas lymphoma manifests as hepatosplenomegaly or occupied lesions in liver or spleen.
Caseous necrosis in TB frequently leads to calcification and manifests as hyperdense mass in the lymph node by CT scan. Conversely, lymphoma rarely presents calcification.
In conclusion, lymph node TB easily mimicks lymphoma. In the PET/CT imaging, both diseases present intense accumulation of FDG; hence, simply measuring SUVmax is inadequate to differentiate them. This uncommon case underscores the necessity of considering lymph node TB as a possible differential diagnosis in systemic enlarged lymph nodes.
Supplementary Material
Footnotes
Abbreviations: 18F-FDG PET = 18F-fluorodeoxyglucose positron emission tomography, SUVmax = maximum standardized uptake value, MTB = Mycobacterium tuberculosis, TB = tuberculosis.
QW and EC have contributed equally to the writing of this article.
Authors’ contributions: QW and XZ designed the study. EC collected data. YC and XZ prepared figures. QW, QL, YC, and XZ reviewed the results, interpreted data, and wrote the manuscript. All authors saw and approved the final version of the paper.
Funding: This work was supported by a grant from the National High Technology Research and Development Program of 863 project of China (NO. 2012AA02A210) and Scientific Research Incubator Project of The First Affiliated Hospital of Wenzhou Medical University (NO. FHY2014018).
Conflicts of interest: The authors have nothing to disclose.
REFERENCES
- 1.Zumla A, George A, Sharma V, et al. The WHO 2014 global tuberculosis report: further to go. Lancet Global Health 2015; 3:e10–e12. [DOI] [PubMed] [Google Scholar]
- 2.Zumla A, Raviglione M, Hafner R, et al. Tuberculosis. N Engl J Med 2013; 368:745–755. [DOI] [PubMed] [Google Scholar]
- 3.Audebert F, Schneidewind A, Hartmann P, et al. Lymph node tuberculosis as primary manifestation of Hodgkin's disease. Medizinische Klinik 2006; 101:500–504. [DOI] [PubMed] [Google Scholar]
- 4.Ouedraogo M, Ouedraogo SM, Cisse R, et al. Active tuberculosis in a patient with Hodgkin's disease. A case report. Revue de pneumologie clinique 2000; 56:33–35. [PubMed] [Google Scholar]
- 5.Lowbridge C, Christensen A, McAnulty JM. EpiReview: tuberculosis in NSW, 2009–2011. N South Wales Public Health Bull 2013; 24:3–9. [DOI] [PubMed] [Google Scholar]
- 6.Zheng YL, Zhang LP, Zhang XL, et al. Forecast model analysis for the morbidity of tuberculosis in Xinjiang, China. PloS One 2015; 10:e0116832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aoki J, Watanabe H, Shinozaki T, et al. FDG-PET for preoperative differential diagnosis between benign and malignant soft tissue masses. Skelet Radiol 2003; 32:133–138. [DOI] [PubMed] [Google Scholar]
- 8.Schulte M, Brecht-Krauss D, Heymer B, et al. Fluorodeoxyglucose positron emission tomography of soft tissue tumours: is a non-invasive determination of biological activity possible? Eur J Nucl Med 1999; 26:599–605. [DOI] [PubMed] [Google Scholar]
- 9.Schulte M, Brecht-Krauss D, Heymer B, et al. Grading of tumors and tumor-like lesions of bone: evaluation by FDG PET. J Nucl Med 2000; 41:1695–1701. [PubMed] [Google Scholar]
- 10.Chen YK, Shen YY, Kao CH. Abnormal FDG PET imaging in tuberculosis appearing like lymphoma. Clin Nucl Med 2004; 29:124. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


