Abstract
Chronic disease has increased in the past several decades, and environmental pollutants have been implicated. The magnitude and variety of diseases may indicate the malfunctioning of some basic mechanisms underlying human health. Environmental pollutants demonstrate a capability to complex iron through electronegative functional groups containing oxygen, nitrogen, or sulfur. Cellular exposure to the chemical or its metabolite may cause a loss of requisite functional iron from intracellular sites. The cell is compelled to acquire further iron critical to its survival by activation of iron-responsive proteins and increasing iron import. Iron homeostasis in the exposed cells is altered due to a new equilibrium being established between iron-requiring cells and the inappropriate chelator (the pollutant or its catabolite). Following exposure to environmental pollutants, the perturbation of functional iron homeostasis may be the mechanism leading to adverse biological effects. Understanding the mechanism may lead to intervention methods for this major public health concern.
Keywords: environmental pollution, iron, ferritin, transferrin receptor
Introduction
Levels of chronic disease have increased over the past several decades; some have done so dramatically. Environmental pollutants, including herbicides and byproducts from industrial chemical processes, have been implicated as possibly being responsible for some portion of this increase. To provide a few examples: exposures to environmental pollutants have been linked to diabetes, cancer, and cardiovascular, neurodegenerative, respiratory, renal, autoimmune, and other diseases;1 polychlorinated biphenyls impact immune suppression, cardiovascular disease, liver disease, diabetes, and changes in thyroid and reproductive function;2 chlorophenols and related compounds, which include chlorophenoxy herbicides and dioxins, are associated with genotoxicity and carcinogenicity;3 and several ecologic studies show that chlorophenoxy herbicide use in Minnesota, Montana, North Dakota, and South Dakota influences human mortality rates due to cancer, acute myocardial infarction, diabetes, and renal disease, as well as rates of birth anomalies.4–8
The large number of diverse diseases associated with exposure to environmental pollutants suggests perturbation of a basic biological pathway underlying the mechanism. However, current methodological approaches have not fully explored these associations for several reasons. Conducting research involving such environmental exposures is difficult because these exposures (1) are often ill defined, (2) occur at low doses, and (3) may involve multiple chemicals. Therefore, linking specific environmental exposures to effects by use of the traditional toxicological model, which is based on exposure to a single agent at different doses, is rather challenging. It has been suggested that a series of transdisciplinary, mutually complementary studies at different levels (ecosystem, population, individual, and molecular) can address these problems.9 A single study based on one of these levels cannot fully define the exposure–effect link. In addition, simultaneous or multiple exposures over time may cause subjects to become increasingly susceptible. This acquired susceptibility due to cumulative exposures needs to be accounted for in studies attempting to link environmental exposures and effects.10 Results from a recent study on environmental perchlorate exposure identified a pattern of biomarker associations that linked perturbation of iron homeostasis with adverse biological activity.11 Additional investigation suggests that other environmental exposures have this same capability.12 In the current paper, we examine further evidence that perturbation of iron homeostasis may be a widespread mechanistic pathway for adverse biological effects following exposure to environmental pollutants (Fig. 1). We selected several environmental pollutants based on their human exposure levels, in order to examine if current knowledge justifies this concept.
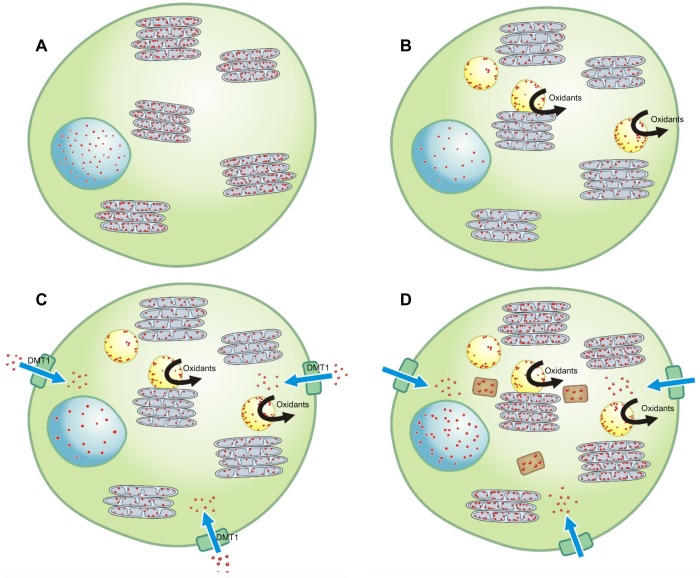
Figure 1.
Normally, a homeostasis of iron (designated by the small red dots) exists in a cell with the metal present at a concentration sufficient to meet structural and metabolic requirements; this includes the nucleus and mitochondria (designated by the blue circular and gray ovoid structures, respectively) (A). Introduction of an environmental chemical (designated by the yellow spherical structures) disrupts iron homeostasis as it, or a catabolic product, complexes the available iron, causing a functional deficiency of the metal in the cell (B). In response to a reduction in intracellular iron, the cell generates superoxide as a ferrireductant and upregulates importers (eg, DMT1) in an attempt to reacquire requisite metal (C). In addition, the complex of the environmental chemical with the iron may support electron transport, and oxidant generation may directly result from the reactions of this product with the available reductant and hydrogen peroxide (C). Oxidative stress activates cell signaling and transcription factors and will provoke a release of mediators initiating inflammation, fibrosis, and apoptosis (C). If the cell is effective in altering its iron homeostasis by increasing iron delivery, some portion of the metal will be stored in the protein ferritin (designated by the brown rectangular structures) (D). The result is an adequate level of metal available to the cell, including the environmental chemical, for continued survival and function.
Iron Homeostasis
Iron is an essential micronutrient required for virtually every aspect of normal cell function. The ability of this metal to interact with O2, reflecting a favorable oxidation–reduction potential, and its abundance in nature have led to its evolutionary selection for a wide range of biological functions. However, these properties of iron which prove so useful for catalysis also make it a threat to life via generation of reactive oxygen species. While living systems must have iron to survive, iron-catalyzed generation of superoxide (O2−), hydrogen peroxide (H2O2), and hydroxyl radical (·OH) presents a potential for oxidative stress. Such reactivity mandates that iron acquisition and distribution be tightly regulated. Consequently, living systems have evolved strategies to regulate the procurement of adequate iron for cellular function and homeostasis without major damage to biological macromolecules.
Cellular iron homeostasis is maintained by a coordinated expression of proteins involved in the import, export, storage, and utilization of this metal.13 Posttranscriptional control mediated by iron-regulatory proteins (IRPs) is essential.14–17 The IRP binds to cis-acting mRNA motifs termed iron-responsive elements (IREs) to regulate the expression of proteins involved in iron homeostasis. This includes stabilizing the mRNA of the divalent metal transport 1 importer (DMT1) and transferrin receptor 1 (TfR1) to promote translation and increase their expression while suppressing the synthesis of the storage protein ferritin.18–20 IRP1, the cytosolic counterpart of mitochondrial aconitase, is a bifunctional protein that, through [4Fe-4S] cluster assembly/disassembly, shifts from the aconitase to the IRP1 form in response to the intracellular iron concentrations.21 Accordingly, iron levels regulate RNA-binding capacity of IRP.
Perturbation of Iron Homeostasis by Environmental Pollutants
Environmental pollutants demonstrate a capability to complex iron, especially if their chemical structure includes a double bond and/or electronegative functional groups containing an oxygen, nitrogen, or sulfur atom, capable of sharing electrons. Complexes of iron sharing at least two binding sites with the ligand are termed chelates. The attribute of iron complexation by environmental pollutants may reflect their original purpose, such as disruption of normal iron homeostasis (eg, the effectiveness of a pesticide can be explained by its capability to complex iron and diminish its availability to pests). Complex formation results from a reaction between available cellular iron and either the chemical itself or a metabolic product. Many of these compounds, employed in the environment to restrict the growth or presence of specific pests, are phenolic compounds, while others are metabolized to phenols via cytochrome P450 following ingestion and inhalation. Phenolic compounds demonstrate a significant capability for iron chelation.22,23 In mammals, for example, dioxins are metabolized by cytochrome P450 to hydroxyphenol, which will complex intracellular sources of iron.24 Accordingly, exposure to either the environmental pollutant or a catabolic product, followed by iron complexation, can cause an immediate loss of functional iron from normal intracellular sites. Iron is critical to the function of cells. This is especially true for mitochondria as this organelle is central to the metabolism of cellular iron.25 Exposure to the pollutant or its catabolite, followed by its appropriation of iron, will challenge mitochondrial function. The cell is compelled to acquire further metal critical to its survival. IRPs are activated and changes in iron import are the result (eg, altered expression of DMT1 and TfR1 follows exposure to these pollutants). Therefore, while the immediate outcome of the exposure to an environmental pollutant or a catabolic product is a cellular deficiency of functional iron, iron homeostasis will be altered in response, resulting in increased import and accumulation of iron. A new equilibrium will be established between the cell sites requiring iron (eg, mitochondria) and the inappropriate chelator (ie, the environmental pollutant or its catabolite) in order to allow for continued survival. At the level of the cell and the tissue, these changes in iron homeostasis can be supported by alternations in either RNA or protein activity of IRP, DMT1, ferritin, and transferrin receptor. In a human being, this new equilibrium can be reflected by elevated concentrations of ferritin and lower transferrin-bound iron levels in the blood.
The response of the cell to environmental chemicals with elevation in the expression of proteins involved in iron import, storage, and export does not appear to be consistent with the model of reciprocal effects mediated via the IRE.26 However, the response of normal cells, tissues, and living systems to either an absolute iron deficiency or a true overload is unlikely to be relevant in the response to an exposure to an inappropriate chelator such as an environmental chemical. When an inappropriate chelator in a cell complexes endogenous iron and initiates the loss of metal from the host, either the cells will increase iron import or apoptosis will occur. As total iron in the cells is increased due to import, and some form of intracellular equilibrium must be maintained, storage of iron in ferritin will also be elevated. This is not a static response but one which will continue for as long as the inappropriate chelator (ie, the environmental chemical) persists in the cell.27–30
An example of these effects has been observed in association with exposure to 2,3,7,8-tetrachlorodibenzo-p-dioxin (2,3,7,8-TCDD).31 As a result of the central role of IRPs in the control of iron metabolism, their modulation by 2,3,7,8-TCDD leads to changes in their expression profile such as alterations of cellular levels of transferrin receptor and ferritin. Elevations in intracellular iron following dioxin exposures can be observed in mammalian cells.32 Animals treated with a single dose of 2,3,7,8-TCDD showed an increase of 41%–67% in iron absorption, reflecting immediate alterations in the metabolism of this metal.33 The major effect of the dioxin was demonstrated to be on the transfer of iron from the mucosa into the bloodstream rather than on the uptake of iron from the gut lumen. Elevated liver iron content was shown in animals treated with 2,3,7,8-TCDD, which further supports the capability of this chemical to disrupt iron homeostasis and affect iron accumulation.34 The catabolism of some herbicides to phenolic compounds is comparable with the catabolism of other aromatic hydrocarbons with regard to their capacity to complex iron, and accordingly disrupts iron homeostasis. Benzene is metabolized by cytochrome P450 to catechol, hydroquinone, 1,2,4-benzenetriol, and p-benzoquinone;35,36 these compounds are recognized to have the capability to complex iron.37 Naphthoquinones are similarly metabolized by cytochrome P450 to phenolic compounds and demonstrate an iron-chelating ability.38 Finally, benzo(a)pyrene is hydroxylated to phenols, which are predicted to affect iron homeostasis.39,40
A related aromatic compound (and a phenol as well) is doxorubicin, an antineoplastic medication (an anthracycline antitumor antibiotic). Exposure to doxorubicin disrupts iron homeostasis and increases heart iron concentrations.41 At the cellular level, exposure to this compound increases iron import by affecting the transferrin receptor42 and elevating ferritin levels,43 comparable with aromatic hydrocarbons used as herbicides. Effects of this anthracycline on cell iron homeostasis can be reversed through a provision of excess metal.44 Clofibrate (2-[4-chlorophenoxy]-2-methylpropionic acid ethyl ester) is another related aromatic hydrocarbon that was previously employed as a lipid-lowering agent. Clofibrate is not a phenolic compound but does have an oxygen-containing functional group (phenoxy) with a capacity to interact with cytochrome P450 and to complex iron. Similar to environmental pollutants, clofibrate exposure alters iron homeostasis through a differential regulation of IRPs.45 Exposure to clofibrate reduces hepatic iron efflux, thereby increasing cell iron concentrations in the liver. A clinical trial initiated in the mid-1960s, showed that subjects treated with clofibrate had a 25% reduction of nonfatal myocardial infarction. However, overall mortality was significantly increased based on diverse causes of death, which included cancer.46 The structure of clofibrate is related to that of the herbicides 2,4-dichlorophenoxyacetic acid (2,4-D) and 4-chloro-2-methylphenoxyacetic acid, which similarly have been associated with elevations in cancer incidence.47 Some environmental pollutants without either phenol groups or modification by cytochromes can form complexes with iron. The herbicide glyphosate (N-(phosphonomethyl) glycine) forms complexes with iron in the soil, resulting in decreased iron concentrations in leaves and seeds and inhibition of ferric reductase activity in the treated plant.48,49 It has been suggested that glyphosate-treated crops may have decreased nutritional levels. In human beings, glyphosate chelates iron and other metals and is thought to be associated with disease.50 The environmental pollutant perchlorate has been observed to be associated with reduced serum iron in human beings. Complexation of iron by perchlorate may be the likely mechanism.11
Subjects are exposed to many environmental chemicals identified in blood and urine, which may have the capability to complex cellular iron. However, their strength to complex iron, which may be based on their chemical structure, is often unknown and will have to be determined by laboratory studies. Some chemicals may be strong iron chelators, eg, dioxin and perchlorate, while others may be weak chelators. However, they all may contribute to perturbation of iron homeostasis resulting in decreased serum iron levels. We propose that a subject’s serum iron level may be a representative biomarker for cumulative exposure to environmental iron-chelating chemicals.
Regarding the fate of the inappropriate iron chelates, further investigation is required. Complexation of the cell cation by the compound will alter its properties of solubility, thus making prediction of its export from the cell difficult. In addition, it is unclear that such complexation is permanent. A dynamic exchange of iron and other cations is anticipated between the chelator and host.
Oxidative Stress after Exposure to Environmental Pollutants
Pathophysiological effects, including inflammation, fibrosis, and cancer, following exposures to xenobiotic agents, have been associated with oxidant damage to macromolecules such as lipids, proteins, and DNA.51 Oxidative stress is a commonly described mechanistic feature of the toxicity of environmental pollutants.52 Exposure to 2,4-D initiates oxidative stress in rat erythrocytes.53 Similarly, proteins (eg, glutathione) and their enzyme activities (eg, glutathione reductase, and superoxide dismutase) involved in oxidant generation and antioxidant function in red blood cells can be impacted by exposures to 2,4,5-trichlorophenoxyacetic acid (2,4,5-T) and its metabolite 2,4,5-trichlorophenol (2,4,5-TCP).54 In an animal model involving subacute exposure to 2,4-D, tissue malondialdehyde levels, antioxidant enzyme (ie, catalase and superoxide dismutase) activities, and serum uric acid concentrations all reflected increased oxidative stress.55 In another animal model, polychlorinated biphenyl exposure increased the levels of superoxide dismutase and heme oxygenase and concentrations of oxidatively modified lipids and proteins, reflecting an oxidative challenge and resulting in oxidant-mediated injury.56
Oxidative stress is frequently associated with disruption of iron homeostasis. A relationship between oxidant generation and disruption of iron homeostasis following exposures to environmental pollutants can result through two potential pathways. First, the environmental pollutant or a catabolic product can be postulated to complex with iron and function as a Fenton’s reagent catalyzing electron exchange and oxidant production.57 Excess iron associated with the exposure is subsequently toxic because the complexed ferrous iron reacts with the available hydrogen peroxides and lipid peroxides to generate hydroxyl and lipid radicals, respectively. These radicals, in turn, damage membrane lipids, proteins, and nucleic acids. Second, in response to diminished levels of essential intracellular iron following complexation of the metal by environmental pollutants or a catabolic product, the cell can generate superoxide as a ferrireductant in an effort to reacquire the metal. Cellular oxidant generation, specifically superoxide, is known to follow exposure to iron deficiency.58–60 This production of oxygen-based radicals functions in the remedial response to iron loss following complexation of the metal. Superoxide, produced by the living system, tissue, cell, and organelle in response to iron deficit, assists in the import of this requisite metal by chemically reducing ferric iron to ferrous iron. This ferrireduction is an essential, and frequently limiting, reaction in such iron import and can be achieved in many cell types using superoxide.61–64
Host Response to Disruption in Iron Homeostasis after Exposure to Environmental Pollutants
The response of a living system to complexation of iron by inappropriate chelators, such as that proposed for environmental pollutants, can include a systemic decrease in the available functional metal. Teleologically, microbial utilization of host iron was the challenge that probably accounts for the development of this response. The host reacts with an exploitation of its own metal by isolating the iron into the reticuloendothelial system, where it is considered less accessible to an inappropriate chelator, such as a microbe or a xenobiotic agent. This response is recognized as a component of the acute-phase reaction. If the exposure is prolonged, an anemia of chronic disease can result. Comparable to microbes and other xenobiotic agents, the complexation of host iron by environmental pollutants is proposed to initiate an attempt by the exposed individual to sequester its metal. The decreased iron level will reflect both the chelating capacity of the environmental chemical and the host’s acute-phase response to that chemical. Accordingly, exposures to environmental pollutants impact indices of the acute-phase response, serum iron, and indices of red blood cell production. Such an acute-phase response has been documented following occupational exposure to environmental pollutants (ie, dieldrin and pentachlorophenol).65,66 Similarly, the acute-phase reaction includes a loss of functional iron. With continued exposures, this can lead to anemia. Herbicide exposures have been associated with decrements in red blood cell counts, hemoglobin, and hematocrit values, which are predicted to result following significant and prolonged contact.67,68
Exposures to environmental pollutants and human health
Exposures to environmental pollutants have been associated with diseases that are predicted to disclose a relationship with disrupted iron homeostasis. A few examples are briefly discussed here to support this viewpoint.
Prenatal and neonatal effects
Pregnancy is a state of high iron demand. However, it is estimated that only 20% of reproductive-aged women worldwide have an iron reserve that is optimal for the development of the fetus.69 Exposure of the mother to environmental pollutants that have the capability to perturb iron homeostasis and diminish available concentrations may adversely affect the development of the fetus. An example of such a pollutant is perchlorate. It was shown in a previous study that increasing urinary perchlorate concentrations were associated with decreasing serum iron concentrations among pregnant women.11 Decreased availability of iron resulting from a reaction of the environmental pollutant with maternal iron pools may preferentially influence the levels in the fetus as a result of its exceptional need and the delicate balance of the metal in the developing life. Iron is needed for cell growth and cell cycle progression.70 Low iron concentrations block cellular proliferation by impinging on pathways that control cell division.71 Iron chelation can arrest cell cycle progression in late G1, before the G1/S border. Accordingly, an increased incidence of birth defects can potentially be associated with exposures to environmental pollutants.69,72,73 It has been observed that children who were iron deficient at birth have lower cognitive skills.74
Endocrine disease
Iron homeostasis influences endocrine function. For example, iron deficiency impairs thyroid hormone synthesis, possibly by reducing the activity of heme-dependent thyroid peroxidase,75 and is a common finding in patients with decreased thyroid activity.76 Iron treatment can provoke both an increase of T4 and a decline of TSH.75 Deficiency of the metal following exposures to environmental pollutants is predicted to influence thyroid function with hypothyroidism resulting. Such an impact has been described with decrements in indices of thyroid function following exposures to environmental pollutants, including perchlorate.77,78
Infections
A connection exists between infection and disruption of iron homeostasis following exposures to different xenobiotic agents.79 The same relationship is proposed following exposures to environmental pollutants. The regulation of iron metabolism is affected by exposure to either the chemical or its metabolite, complexing the metal and thereby decreasing available functional iron concentrations. However, total iron concentrations increase with the exposed cells and tissues upregulating iron importers in order to compete for the metal and allow cell survival. The increased total iron in the exposed cells and tissues will be reflected by elevated ferritin levels in the host. There is an absolute dependency of all life on iron availability. With very few exceptions (eg, lactobacilli which substitute manganese for iron), microbes require host iron in order to proliferate.80 The pathogen’s survival and virulence are directly related to its success in competing for the available iron in the host. Therefore, exposures to environmental pollutants will elevate the risk for infection by increasing total iron levels in cells, tissues, and living systems.81,82
Metabolic syndrome
This group of characteristics includes obesity, insulin resistance, hyperglycemia, and dyslipidemia, which are risk factors for several diseases such as cardiovascular disease, diabetes type 2, immune disorders, and liver diseases. Exposures to multiple environmental chemicals are suspected to contribute to this disorder according to the Parma consensus statement.83 It is proposed that perturbation of iron homeostasis, as a result of exposure to environmental chemicals, contributes to this metabolic disruption. Supporting the concept is a seven-year followup study showing that markers of iron metabolism are associated with insulin resistance in adipose tissue, liver, and muscle, which may affect impaired glucose metabolism and type 2 diabetes.84 A rat study on chronic, low-dose exposure to the widely used herbicide atrazine (2-chloro-4-ethylkamine-6-isopropylamino-S-triazine) showed that this herbicide induced abdominal obesity and insulin resistance due to impaired mitochondrial function.85 This herbicide has several nitrogen atoms and double bonds in its chemical structure and, therefore, may have the capability to form iron complexes.
Chronic diseases
Associations between exposures to environmental pollutants and increased incidence of chronic disease have been suggested.86–91 A disruption of iron homeostasis is proposed to participate in the pathogenesis of numerous chronic diseases including diabetes, cancer, and cardiovascular, cerebrovascular, and neurodegenerative diseases. Diabetes and cardiovascular disease may have been preceded by the metabolic syndrome. Changes in the concentrations of functional iron are recognized as a determinant in the pathogenesis as they are related to both oxidative stress and injury. Therefore, it is feasible that increases in the incidence and prevalence of these chronic diseases following exposures to environmental pollutants are associated with altered iron availability. Some examples are discussed.
An association between a disruption in iron homeostasis and peripheral insulin resistance has been demonstrated in epidemiological investigations. Among middle-aged men, those with higher levels of serum ferritin had higher insulin and glucose levels.92 Serum ferritin concentrations were an independent predictor of increased serum insulin levels among adults.93 Women with impaired glucose tolerance or gestational diabetes had higher serum ferritin values relative to women with normal glucose tolerance.94–98 Diabetes has been shown to be associated with a disruption of normal iron metabolism. Individuals with type 2 diabetes had higher levels of serum ferritin and nontransferrin-bound iron relative to healthy controls.99 Men with high iron stores were 2.4 times more likely to develop type 2 diabetes compared with men with lower stores.100 A potential benefit of iron depletion on insulin sensitivity and/or type 2 diabetes has been demonstrated with frequent blood donors having better insulin sensitivity and lower ferritin levels compared with nondonors.101,102 An increased number of lifetime blood donations was associated with decreased prevalence of type 2 diabetes in men.103,104 Iron chelation therapy with intravenous deferoxamine significantly improved metabolic control with a reduction in blood glucose and glycosylated hemoglobin levels among type 2 diabetics.105 Accordingly, a disruption in iron homeostasis with an accumulation in total metal following exposure to an environmental pollutant can potentially impact both insulin resistance and diabetes.
A disruption in iron homeostasis can also participate in cardiovascular disease. In women, the risk of heart disease increases following either natural or surgical menopause, which is associated with elevations in serum ferritin concentrations.106 Among men, there is an increase in the risk of coronary heart disease with elevated iron stores. Men with high body iron stores had a two- to threefold increased risk of myocardial infarction compared with men with low body iron stores.107 Among randomly selected men with no symptomatic coronary artery disease at entry, the adjusted risk of acute myocardial infarction with serum ferritin >200 ng/mL was 2.2-fold higher than in those with lower serum ferritin with the odds ratio increasing by 0.2 for each 100 ng/mL increase in serum ferritin.108 Mechanistically, evidence for a participation of iron in atherosclerosis was suggested by the ability of the metal to oxidize low-density lipoprotein (LDL) and damage endothelial cells, by the observation of ferritin induction with the progression of atherosclerotic lesions, by the inhibition of endothelial cell damage and oxidation of LDL by chelators, and by the prevention of endothelial cell dysfunction and vascular smooth muscle proliferation by chelators.109–112 Altering iron metabolism with phlebotomy, systemic iron chelation treatment, or dietary iron restriction reduces atherosclerotic lesion size and/or increases plaque stability.113–115 Changes in iron stores during a five-year follow-up period modified the risk of atherosclerosis with the lowering of iron stores being beneficial and the further accumulation of iron increasing cardiovascular risk.116 Furthermore, studies on the effect of blood donation on the reduction of cardiovascular events support the postulate that iron stores can be associated with coronary artery disease.117,118 Therefore, increases in heart disease following exposure to environmental pollutants could result from host iron complexation and impact of total available metal.
Evidence also supports the participation of iron in cerebrovascular disease. Experimental iron overload induced by using an iron-rich diet causes larger infarct volumes after permanent middle cerebral arterial occlusion in rats.119 These results indicate that the severity of tissue injury with cerebrovascular occlusion can be proportional to total iron. Asymptomatic carotid atherosclerosis, assessed by duplex sonography, shows a strong correlation with iron stores in men and women.120 Higher serum ferritin concentrations can be associated with an increased risk of ischemic stroke.121 Increased ferritin concentrations, in both blood and cerebrospinal fluid, have been related to poor outcome in stroke patients.122 Increased serum ferritin concentrations before treatment also predict prognosis in patients with a higher risk of hemorrhagic transformation and brain edema.123 Treatment with an iron-deficient diet reduces neuronal necrosis and improves neurological status in animal models of global and focal cerebral ischemia.124 Following exposure to environmental pollutants, an accumulation in total iron concentration combined with a decrease of functional iron could account for the observed changes in cerebrovascular disease.
Perturbed iron homeostasis has been observed in neurodegenerative diseases, including Alzheimer’s disease, Parkinson’s disease, and amyotrophic lateral sclerosis (ALS).125 In Alzheimer’s disease, increased levels of iron and ferritin have been noted pathologically in the cerebral cortex.126 Among those individuals suffering from Parkinson’s disease, iron accumulates at the sites of neuronal death.127 Among ALS patients, elevations in serum ferritin and transferrin saturation levels have been shown.128 It is feasible that altered iron homeostasis following exposure to environmental pollutants could contribute to the observed accumulations of this metal in neurodegenerative disease.
Regarding cancer, cohort studies have found that indices of iron metabolism are associated with an increased risk of cancer incidence and cancer mortality. Among persons with increased transferrin saturation, a daily intake of dietary iron of >18 mg is associated with an increased risk of cancer.129 A causal relationship is suggested by studies showing that blood donation (to reduce total body iron stores) is associated with lower cancer risk130,131 and that blood transfusion adversely affects cancer outcome.132 A randomized trial of subjects undergoing phlebotomy showed a significant reduction in overall cancer incidence with iron reduction.133 An association of iron intake with colorectal cancer risk has been observed among a cohort of the National Health and Nutrition Examination Survey I.134 The association between elevations in biologically available iron and increased cancer may result from the antiapoptotic effect of the metal.71 Experimental study findings support a role of iron in chemically induced carcinogenesis and demonstrate that iron may initiate and promote carcinogenesis through the production of oxidative stress, facilitation of tumor cell growth, and modification of the immune system. Excessive accumulation of iron in hepatocytes causes hepatocellular injury, which leads to the development of hepatoma.135 A low iron diet resulted in a decrease in skin tumor incidence (both papillomas and carcinomas) and the number of tumors per mouse, as well as the conversion of papillomas to carcinomas.136 Comparable to diabetes, coronary artery disease, cerebrovascular disease, neurodegenerative disease, and cancer may be associated with a disruption in iron homeostasis initiated by the exposure to an environmental pollutant.
Conclusion
Based on previous investigations, various diseases have been shown to be associated with exposure to environmental pollutants. Multiple exposures over time may have cumulative effects and lead to increased susceptibility to disease. Mechanistically, we propose that this occurs through an impact of such pollutants on iron homeostasis. The disruption of iron homeostasis results from the initial interaction with environmental pollutants, ie, complexation of the metal by the chemical or its metabolic products with subsequent reductions in host cell and tissue levels of functional iron, and likely represents the most basic mechanism underlying the biological effects following such exposure. If the concept described in this investigation is confirmed, iron chelation may be the molecular-initiating event of the adverse outcome pathway of many environmental chemicals. Determination of their chelating capability will be of interest with regard to their association with adverse health effects.
Acknowledgments
The authors acknowledge the valuable comments by Michael Madden, Joachim Pleil, and the reviewers for Environmental Health Insights.
Footnotes
ACADEMIC EDITOR: Timothy Kelley, Editor in Chief
PEER REVIEW: Five peer reviewers contributed to the peer review report. Reviewers’ reports totaled 1403 words, excluding any confidential comments to the academic editor.
FUNDING: Authors disclose no external funding sources.
COMPETING INTERESTS: Authors disclose no potential conflicts of interest.
Paper subject to independent expert single-blind peer review. All editorial decisions made by independent academic editor. Upon submission manuscript was subject to anti-plagiarism scanning. Prior to publication all authors have given signed confirmation of agreement to article publication and compliance with all applicable ethical and legal requirements, including the accuracy of author and contributor information, disclosure of competing interests and funding sources, compliance with ethical requirements relating to human and animal study participants, and compliance with any copyright requirements of third parties. This journal is a member of the Committee on Publication Ethics (COPE).
Disclaimer
The research described in this article has been reviewed in accordance with the U.S. Environmental Protection Agency policy and approved for publication. Approval does not signify that the contents necessarily reflect the views and policies of the agency.
Author Contributions
Conceived the concepts: DMS, AJG. Analyzed the data: DMS, AJG. Wrote the first draft of the manuscript: DMS, AJG. Contributed to the writing of the manuscript: DMS, AJG. Agree with manuscript results and conclusions: DMS, AJG. Jointly developed the structure and arguments for the paper: DMS, AJG. Made critical revisions and approved final version: DMS, AJG. Both authors reviewed and approved of the final manuscript.
REFERENCES
- 1.Mostafalou S, Abdollahi M. Pesticides and human chronic diseases: evidences, mechanisms, and perspectives. Toxicol Appl Pharmacol. 2013;268:157–77. doi: 10.1016/j.taap.2013.01.025. [DOI] [PubMed] [Google Scholar]
- 2.Carpenter DO. Polychlorinated biphenyls (PCBs): routes of exposure and effects on human health. Rev Environ Health. 2006;21:1–23. doi: 10.1515/reveh.2006.21.1.1. [DOI] [PubMed] [Google Scholar]
- 3.Igbinosa EO, Odjadjare EE, Chigor VN, et al. Toxicological profile of chlorophenols and their derivatives in the environment: the public health perspective. Scientific World Journal. 2013;2013:460215. doi: 10.1155/2013/460215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Garry VF, Kelly JT, Sprafka JM, Edwards S, Griffith J. Survey of health and use characterization of pesticide appliers in Minnesota. Arch Environ Health. 1994;49:337–43. doi: 10.1080/00039896.1994.9954984. [DOI] [PubMed] [Google Scholar]
- 5.Schreinemachers DM, Creason JP, Garry VF. Cancer mortality in agricultural regions of Minnesota. Environ Health Perspect. 1999;107:205–11. doi: 10.1289/ehp.99107205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schreinemachers DM. Cancer mortality in four northern wheat-producing states. Environ Health Perspect. 2000;108:873–81. doi: 10.1289/ehp.00108873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schreinemachers DM. Birth malformations and other adverse perinatal outcomes in four U.S. Wheat-producing states. Environ Health Perspect. 2003;111:1259–64. doi: 10.1289/ehp.5830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schreinemachers DM. Mortality from ischemic heart disease and diabetes mellitus (type 2) in four U.S. wheat-producing states: a hypothesis-generating study. Environ Health Perspect. 2006;114:186–93. doi: 10.1289/ehp.8352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pekkanen J, Pearce N. Environmental epidemiology: challenges and opportunities. Environ Health Perspect. 2001;109:1–5. doi: 10.1289/ehp.011091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vineis P, Khan AE, Vlaanderen J, Vermeulen R. The impact of new research technologies on our understanding of environmental causes of disease: the concept of clinical vulnerability. Environ Health. 2009;8:54. doi: 10.1186/1476-069X-8-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schreinemachers DM, Ghio AJ, Sobus JR, Williams MA. Perchlorate exposure is associated with oxidative stress and indicators of serum iron homeostasis among NHANES 2005–2008 subjects. Biomark Insights. 2015;10:9–19. doi: 10.4137/BMI.S20089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Guo W, Zhang J, Li W, Xu M, Liu S. Disruption of iron homeostasis and resultant health effects upon exposure to various environmental pollutants: a critical review. J Environ Sci. 2015;34:155–64. doi: 10.1016/j.jes.2015.04.004. [DOI] [PubMed] [Google Scholar]
- 13.Hentze MW, Muckenthaler MU, Andrews NC. Balancing acts: molecular control of mammalian iron metabolism. Cell. 2004;117:285–97. doi: 10.1016/s0092-8674(04)00343-5. [DOI] [PubMed] [Google Scholar]
- 14.Pantopoulos K. Iron metabolism and the IRE/IRP regulatory system: an update. Ann N Y Acad Sci. 2004;1012:1–13. doi: 10.1196/annals.1306.001. [DOI] [PubMed] [Google Scholar]
- 15.Rouault TA. The role of iron regulatory proteins in mammalian iron homeostasis and disease. Nat Chem Biol. 2006;2:406–14. doi: 10.1038/nchembio807. [DOI] [PubMed] [Google Scholar]
- 16.Muckenthaler MU, Galy B, Hentze MW. Systemic iron homeostasis and the iron-responsive element/iron-regulatory protein (IRE/IRP) regulatory network. Annu Rev Nutr. 2008;28:197–213. doi: 10.1146/annurev.nutr.28.061807.155521. [DOI] [PubMed] [Google Scholar]
- 17.Wallander ML, Leibold EA, Eisenstein RS. Molecular control of vertebrate iron homeostasis by iron regulatory proteins. Biochim Biophys Acta. 2006;1763:668–89. doi: 10.1016/j.bbamcr.2006.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fishman JB, Rubin JB, Handrahan JV, Connor JR, Fine RE. Receptor mediated transcytosis of transferrin across the blood-brain barrier. J Neurosci Res. 1987;18:299–304. doi: 10.1002/jnr.490180206. [DOI] [PubMed] [Google Scholar]
- 19.Mims MP, Prchal JT. Divalent metal transporter 1. Hematology. 2005;10:339–45. doi: 10.1080/10245330500093419. [DOI] [PubMed] [Google Scholar]
- 20.Aziz N, Munro HN. Iron regulates ferritin mRNA translation through a segment of its 5′ untranslated region. Proc Natl Acad Sci U S A. 1987;84:8478–82. doi: 10.1073/pnas.84.23.8478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kennedy MC, Mende-Mueller L, Blondin GA, Beinert H. Purification and characterization of cytosolic aconitase from beef liver and its relationship to the iron-responsive element binding protein. Proc Natl Acad Sci U S A. 1992;89:11730–4. doi: 10.1073/pnas.89.24.11730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Perron NR, Brumaghim JL. A review of the antioxidant mechanisms of polyphenol compounds related to iron binding. Cell Biochem Biophys. 2009;53:75–100. doi: 10.1007/s12013-009-9043-x. [DOI] [PubMed] [Google Scholar]
- 23.Chobot V, Hadacek F. Iron and its complexation by phenolic cellular metabolites. From oxidative stress to chemical weapons. Plant Signal Behav. 2010;5:4–8. doi: 10.4161/psb.5.1.10197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sakaki T, Yamamoto K, Ikushiro S. Possibility of application of cytochrome P450 to bioremediation of dioxins. Biotechnol Appl Biochem. 2013;60:65–70. doi: 10.1002/bab.1067. [DOI] [PubMed] [Google Scholar]
- 25.Richardson DR, Lane DJ, Becker EM, et al. Mitochondrial iron trafficking and the integration of iron metabolism between the mitochondrion and cytosol. Proc Natl Acad Sci U S A. 2010;107:10775–82. doi: 10.1073/pnas.0912925107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cairo G, Recalcati S, Pietrangelo A, Minotti G. The iron regulatory proteins: targets and modulators of free radical reactions and oxidative damage. Free Radic Biol Med. 2002;32:1237–43. doi: 10.1016/s0891-5849(02)00825-0. [DOI] [PubMed] [Google Scholar]
- 27.Basaraba RJ, Bielefeldt-Ohmann H, Eschelbach EK, et al. Increased expression of host iron-binding proteins precedes iron accumulation and calcification of primary lung lesions in experimental tuberculosis in the guinea pig. Tuberculosis (Edinb) 2008;88:69–79. doi: 10.1016/j.tube.2007.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ghio AJ, Tong H, Soukup JM, et al. Sequestration of mitochondrial iron by silica particle initiates a biological effect. Am J Physiol Lung Cell Mol Physiol. 2013;305:L712–24. doi: 10.1152/ajplung.00099.2013. [DOI] [PubMed] [Google Scholar]
- 29.Zhang HY, Wang ND, Song N, et al. 6-Hydroxydopamine promotes iron traffic in primary cultured astrocytes. Biometals. 2013;26:705–14. doi: 10.1007/s10534-013-9647-x. [DOI] [PubMed] [Google Scholar]
- 30.Michael S, Petrocine SV, Qian J, et al. Iron and iron-responsive proteins in the cardiomyopathy of Friedreich’s ataxia. Cerebellum. 2006;5:257–67. doi: 10.1080/14734220600913246. [DOI] [PubMed] [Google Scholar]
- 31.Santamaria R, Fiorito F, Irace C, et al. 2,3,7,8-Tetrachlorodibenzo-p-dioxin impairs iron homeostasis by modulating iron-related proteins expression and increasing the labile iron pool in mammalian cells. Biochim Biophys Acta. 2011;1813:704–12. doi: 10.1016/j.bbamcr.2011.02.003. [DOI] [PubMed] [Google Scholar]
- 32.Fiorito F, Irace C, Di Pascale A, et al. 2,3,7,8-Tetrachlorodibenzo-p-dioxin promotes BHV-1 infection in mammalian cells by interfering with iron homeostasis regulation. PLoS One. 2013;8:e58845. doi: 10.1371/journal.pone.0058845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Manis J, Kim G. Stimulation of iron absorption by polychlorinated aromatic hydrocarbons. Am J Physiol. 1979;236:E763–8. doi: 10.1152/ajpendo.1979.236.6.E763. [DOI] [PubMed] [Google Scholar]
- 34.Wahba ZZ, al-Bayati ZA, Stohs SJ. Effect of 2,3,7,8-tetrachlorodibenzo-p-dioxin on the hepatic distribution of iron, copper, zinc, and magnesium in rats. J Biochem Toxicol. 1988;3:121–9. doi: 10.1002/jbt.2570030206. [DOI] [PubMed] [Google Scholar]
- 35.Kolachana P, Subrahmanyam VV, Meyer KB, Zhang L, Smith MT. Benzene and its phenolic metabolites produce oxidative DNA damage in HL60 cells in vitro and in the bone marrow in vivo. Cancer Res. 1993;53:1023–6. [PubMed] [Google Scholar]
- 36.Gillis B, Gavin IM, Arbieva Z, King ST, Jayaraman S, Prabhakar BS. Identification of human cell responses to benzene and benzene metabolites. Genomics. 2007;90:324–33. doi: 10.1016/j.ygeno.2007.05.003. [DOI] [PubMed] [Google Scholar]
- 37.Ahmad S, Rao GS. Complexation of 1,2,4-benzenetriol with inorganic and ferritin-released iron in vitro. Biochem Biophys Res Commun. 1999;259:169–71. doi: 10.1006/bbrc.1999.0741. [DOI] [PubMed] [Google Scholar]
- 38.Lebedev AV, Ivanova MV, Levitsky DO. Iron chelators and free radical scavengers in naturally occurring polyhydroxylated 1,4-naphthoquinones. Hemoglobin. 2008;32:165–79. doi: 10.1080/03630260701700017. [DOI] [PubMed] [Google Scholar]
- 39.Melikian AA, Sun P, Prokopczyk B, et al. Identification of benzo[a]pyrene metabolites in cervical mucus and DNA adducts in cervical tissues in humans by gas chromatography-mass spectrometry. Cancer Lett. 1999;146:127–34. doi: 10.1016/s0304-3835(99)00203-7. [DOI] [PubMed] [Google Scholar]
- 40.Honey S, O’Keefe P, Drahushuk AT, Olson JR, Kumar S, Sikka HC. Metabolism of benzo(a)pyrene by duck liver microsomes. Comp Biochem Physiol C Toxicol Pharmacol. 2000;126:285–92. doi: 10.1016/s0742-8413(00)00121-3. [DOI] [PubMed] [Google Scholar]
- 41.Cascales A, Sánchez-Vega B, Navarro N, et al. Clinical and genetic determinants of anthracycline-induced cardiac iron accumulation. Int J Cardiol. 2012;154:282–6. doi: 10.1016/j.ijcard.2010.09.046. [DOI] [PubMed] [Google Scholar]
- 42.Kotamraju S, Chitambar CR, Kalivendi SV, Joseph J, Kalyanaraman B. Transferrin receptor-dependent iron uptake is responsible for doxorubicin-mediated apoptosis in endothelial cells: role of oxidant-induced iron signaling in apoptosis. J Biol Chem. 2002;277:17179–87. doi: 10.1074/jbc.M111604200. [DOI] [PubMed] [Google Scholar]
- 43.Kwok JC, Richardson DR. Anthracyclines induce accumulation of iron in ferritin in myocardial and neoplastic cells: inhibition of the ferritin iron mobilization pathway. Mol Pharmacol. 2003;63:849–61. doi: 10.1124/mol.63.4.849. [DOI] [PubMed] [Google Scholar]
- 44.Xu X, Sutak R, Richardson DR. Iron chelation by clinically relevant anthracyclines: alteration in expression of iron-regulated genes and atypical changes in intracellular iron distribution and trafficking. Mol Pharmacol. 2008;73:833–44. doi: 10.1124/mol.107.041335. [DOI] [PubMed] [Google Scholar]
- 45.Huang HL, Shaw NS. Role of hypolipidemic drug clofibrate in altering iron regulatory proteins IRP1 and IRP2 activities and hepatic iron metabolism in rats fed a low-iron diet. Toxicol Appl Pharmacol. 2002;180:118–28. doi: 10.1006/taap.2002.9378. [DOI] [PubMed] [Google Scholar]
- 46.Committee of Principal Investigators W.H.O. cooperative trial on primary prevention of ischaemic heart disease using clofibrate to lower serum cholesterol: mortality follow-up. Lancet. 1980;2:379–85. [PubMed] [Google Scholar]
- 47.Axelson O, Tagesson C, Hardell L. The clofibrate problem: a different viewpoint. Lancet. 1980;2:1081–2. [PubMed] [Google Scholar]
- 48.Bellaloui N, Reddy KN, Zablotowicz RM, Abbas HK, Abel CA. Effects of glyphosate application on seed iron and root ferric (III) reductase in soybean cultivars. J Agric Food Chem. 2009;57:9569–74. doi: 10.1021/jf902175y. [DOI] [PubMed] [Google Scholar]
- 49.Sheals J, Granström M, Sjöberg S, Persson P. Coadsorption of Cu (II) and glyphosate at the water-goethite (alpha-FeOOH) interface: molecular structures from FTIR and EXAFS measurements. J Colloid Interface Sci. 2003;262:38–47. doi: 10.1016/S0021-9797(03)00207-8. [DOI] [PubMed] [Google Scholar]
- 50.Samsel A, Seneff S. Glyphosate, pathways to modern diseases II: celiac sprue and gluten intolerance. Interdiscip Toxicol. 2013;6:159–84. doi: 10.2478/intox-2013-0026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kelly KA, Havrilla CM, Brady TC, Abramo KH, Levin ED. Oxidative stress in toxicology: established mammalian and emerging piscine model systems. Environ Health Perspect. 1998;106:375–84. doi: 10.1289/ehp.98106375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Poljšak B, Fink R. The protective role of antioxidants in the defense against ROS/RNS-mediated environmental pollution. Oxid Med Cell Longev. 2014;2014:671539. doi: 10.1155/2014/671539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Tayeb W, Nakbi A, Chargui I, Imed C, Miled A, Chargui I. Subacute effects of 2,4-dichlorophenoxyacetic herbicide on antioxidant defense system and lipid peroxidation in rat erythrocytes. Pestic Biochem Physiol. 2011;99:256–64. [Google Scholar]
- 54.Bukowska B. 2,4,5-T and 2,4,5-TCP induce oxidative damage in human erythrocytes: the role of glutathione. Cell Biol Int. 2004;28:557–63. doi: 10.1016/j.cellbi.2004.04.013. [DOI] [PubMed] [Google Scholar]
- 55.Tayeb W, Nakbi A, Trabelsi M, Miled A, Hammami M. Biochemical and histological evaluation of kidney damage after sub-acute exposure to 2,4-dichlorophenoxyacetic herbicide in rats: involvement of oxidative stress. Toxicol Mech Methods. 2012;22:696–704. doi: 10.3109/15376516.2012.717650. [DOI] [PubMed] [Google Scholar]
- 56.Lee DW, Notter SA, Thiruchelvam M, et al. Subchronic polychlorinated biphenyl (Aroclor 1254) exposure produces oxidative damage and neuronal death of ventral midbrain dopaminergic systems. Toxicol Sci. 2012;125:496–508. doi: 10.1093/toxsci/kfr313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kell DB. Iron behaving badly: inappropriate iron chelation as a major contributor to the aetiology of vascular and other progressive inflammatory and degenerative diseases. BMC Med Genomics. 2009;2:2. doi: 10.1186/1755-8794-2-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Callens C, Coulon S, Naudin J, et al. Targeting iron homeostasis induces cellular differentiation and synergizes with differentiating agents in acute myeloid leukemia. J Exp Med. 2010;207:731–50. doi: 10.1084/jem.20091488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Chaston TB, Watts RN, Yuan J, Richardson DR. Potent antitumor activity of novel iron chelators derived from di-2-pyridylketone isonicotinoyl hydrazone involves fenton-derived free radical generation. Clin Cancer Res. 2004;10:7365–74. doi: 10.1158/1078-0432.CCR-04-0865. [DOI] [PubMed] [Google Scholar]
- 60.Dendorfer A, Heidbreder M, Hellwig-Burgel T, Jöhren O, Qadri F, Dominiak P. Deferoxamine induces prolonged cardiac preconditioning via accumulation of oxygen radicals. Free Radic Biol Med. 2005;38:117–24. doi: 10.1016/j.freeradbiomed.2004.10.015. [DOI] [PubMed] [Google Scholar]
- 61.Cakmak I, van de Wetering DA, Marschner H, Bienfait HF. Involvement of superoxide radical in extracellular ferric reduction by iron-deficient bean roots. Plant Physiol. 1987;85:310–4. doi: 10.1104/pp.85.1.310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Rose AL, Salmon TP, Lukondeh T, Neilan BA, Waite TD. Use of superoxide as an electron shuttle for iron acquisition by the marine cyanobacterium Lyngbya majuscula. Environ Sci Technol. 2005;39:3708–15. doi: 10.1021/es048766c. [DOI] [PubMed] [Google Scholar]
- 63.Srinivasan C, Liba A, Imlay JA, Valentine JS, Gralla EB. Yeast lacking super-oxide dismutase(s) show elevated levels of “free iron” as measured by whole cell electron paramagnetic resonance. J Biol Chem. 2000;275:29187–92. doi: 10.1074/jbc.M004239200. [DOI] [PubMed] [Google Scholar]
- 64.Ghio AJ, Nozik-Grayck E, Turi J, et al. Superoxide-dependent iron uptake: a new role for anion pesticide exposure. Life Sci. 1976;19:1645–51. [Google Scholar]
- 65.Takahashi W, Reichert ER, Fung GC, Hokama Y. Acute phase proteins and pesticide exposure. Life Sci. 1976;19:1645–51. doi: 10.1016/0024-3205(76)90069-2. [DOI] [PubMed] [Google Scholar]
- 66.Patil JA, Patil AJ, Sontakke AV, Govindwar SP. Occupational pesticides exposure of sprayers of grape gardens in western Maharashtra (India): effects on liver and kidney function. J Basic Clin Physiol Pharmacol. 2009;20:335–55. doi: 10.1515/jbcpp.2009.20.4.335. [DOI] [PubMed] [Google Scholar]
- 67.Pereira L, Fernandes MN, Martinez CB. Hematological and biochemical alterations in the fish Prochilodus lineatus caused by the herbicide clomazone. Environ Toxicol Pharmacol. 2013;36:1–8. doi: 10.1016/j.etap.2013.02.019. [DOI] [PubMed] [Google Scholar]
- 68.Hussain R, Mahmood F, Khan MZ, Muhammad F. Pathological and genotoxic effects of atrazine in male Japanese quail (Coturnix japonica) Ecotoxicology. 2011;20:1–8. doi: 10.1007/s10646-010-0515-y. [DOI] [PubMed] [Google Scholar]
- 69.Cao C, O’Brien KO. Pregnancy and iron homeostasis: an update. Nutr Rev. 2013;71:35–51. doi: 10.1111/j.1753-4887.2012.00550.x. [DOI] [PubMed] [Google Scholar]
- 70.Lederman HM, Cohen A, Lee JW, Freedman MH, Gelfand EW. Deferoxamine: a reversible S-phase inhibitor of human lymphocyte proliferation. Blood. 1984;64:748–53. [PubMed] [Google Scholar]
- 71.Hileti D, Panayiotidis P, Hoffbrand AV. Iron chelators induce apoptosis in proliferating cells. Br J Haematol. 1995;89:181–7. doi: 10.1111/j.1365-2141.1995.tb08927.x. [DOI] [PubMed] [Google Scholar]
- 72.McArdle HJ, Gambling L, Kennedy C. Iron deficiency during pregnancy: the consequences for placental function and fetal outcome. Proc Nutr Soc. 2014;73:9–15. doi: 10.1017/S0029665113003637. [DOI] [PubMed] [Google Scholar]
- 73.Collard KJ. Iron homeostasis in the neonate. Pediatrics. 2009;123:1208–16. doi: 10.1542/peds.2008-1047. [DOI] [PubMed] [Google Scholar]
- 74.Radlowski EC, Johnson RW. Perinatal iron deficiency and neurocognitive development. Front Hum Neurosci. 2014;7(article 585):1–11. doi: 10.3389/fnhum.2013.00585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Duntas LH, Papanastasiou L, Mantzou E, Koutras DA. Incidence of sideropenia and effects of iron repletion treatment in women with subclinical hypothyroidism. Exp Clin Endocrinol Diabetes. 1999;107(6):356–60. doi: 10.1055/s-0029-1212126. [DOI] [PubMed] [Google Scholar]
- 76.Zimmermann MB, Köhrle J. The impact of iron and selenium deficiencies on iodine and thyroid metabolism: biochemistry and relevance to public health. Thyroid. 2002;12:867–78. doi: 10.1089/105072502761016494. [DOI] [PubMed] [Google Scholar]
- 77.Steinmaus C, Miller MD, Smith AH. Perchlorate in drinking water during pregnancy and neonatal thyroid hormone levels in California. J Occup Environ Med. 2010;52:1217–524. doi: 10.1097/JOM.0b013e3181fd6fa7. [DOI] [PubMed] [Google Scholar]
- 78.Baccarelli A, Giacomini SM, Corbetta C, et al. Neonatal thyroid function in Seveso 25 years after maternal exposure to dioxin. PLoS Med. 2008;5:e161. doi: 10.1371/journal.pmed.0050161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Ghio AJ. Particle exposures and infections. Infection. 2014;42:459–67. doi: 10.1007/s15010-014-0592-6. [DOI] [PubMed] [Google Scholar]
- 80.Weinberg ED. Iron availability and infection. Biochim Biophys Acta. 2009;1790:600–5. doi: 10.1016/j.bbagen.2008.07.002. [DOI] [PubMed] [Google Scholar]
- 81.Repetto R, Baliga SS. Pesticides and immunosuppression: the risks to public health. Health Policy Plan. 1997;12:97–106. doi: 10.1093/heapol/12.2.97. [DOI] [PubMed] [Google Scholar]
- 82.Dallaire F, Dewailly E, Muckle G, et al. Acute infections and environmental exposure to organochlorines in Inuit infants from Nunavik. Environ Health Perspect. 2004;112:1359–65. doi: 10.1289/ehp.7255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Heindel JJ, vom Saal FS, Blumberg B, et al. Parma consensus statement on metabolic disruptors. Environ Health. 2015;14:54. doi: 10.1186/s12940-015-0042-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Wlazlo N, van Greevenbroek MMJ, Ferreira I, et al. Iron metabolism is prospectively associated with insulin resistance and glucose intolerance over a 7-year follow-up period: the CODAM study. Acta Diabetol. 2014;52:337–48. doi: 10.1007/s00592-014-0646-3. [DOI] [PubMed] [Google Scholar]
- 85.Lim S, Ahn SY, Song IC, et al. Chronic exposure to the herbicide atrazine, causes mitochondrial dysfunction and insulin resistance. PLoS One. 2009;4:e5186. doi: 10.1371/journal.pone.0005186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Park SK, Son HK, Lee SK, et al. Relationship between serum concentrations of organochlorine pesticides and metabolic syndrome among non-diabetic adults. J Prev Med Public Health. 2010;43:1–8. doi: 10.3961/jpmph.2010.43.1.1. [DOI] [PubMed] [Google Scholar]
- 87.Everett CJ, Thompson OM. Association of DDT and heptachlor epoxide in human blood with diabetic nephropathy. Rev Environ Health. 2015;30:93–7. doi: 10.1515/reveh-2015-0003. [DOI] [PubMed] [Google Scholar]
- 88.Lind L, Lind PM. Can persistent organic pollutants and plastic-associated chemicals cause cardiovascular disease? J Intern Med. 2012;271:537–53. doi: 10.1111/j.1365-2796.2012.02536.x. [DOI] [PubMed] [Google Scholar]
- 89.Charles LE, Burchfiel CM, Fekedulegn D, et al. Occupational exposure to pesticides, metals, and solvents: the impact on mortality rates in the Honolulu heart program. Work. 2010;37:205–15. doi: 10.3233/WOR-2010-1071. [DOI] [PubMed] [Google Scholar]
- 90.Baltazar MT, Dinis-Oliveira RJ, de Lourdes Bastos M, Tsatsakis AM, Duarte JA, Carvalho F. Pesticides exposure as etiological factors of Parkinson’s disease and other neurodegenerative diseases – a mechanistic approach. Toxicol Lett. 2014;230:85–103. doi: 10.1016/j.toxlet.2014.01.039. [DOI] [PubMed] [Google Scholar]
- 91.Schinasi L, Leon ME. Non-Hodgkin lymphoma and occupational exposure to agricultural pesticide chemical groups and active ingredients: a systematic review and meta-analysis. Int J Environ Res Public Health. 2014;11:4449–527. doi: 10.3390/ijerph110404449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Fernandez-Real JM, Ricart-Engel W, Arroyo E, et al. Serum ferritin as a component of the insulin resistance syndrome. Diabetes Care. 1998;21:62–8. doi: 10.2337/diacare.21.1.62. [DOI] [PubMed] [Google Scholar]
- 93.Fumeron F, Pean F, Driss F, et al. Insulin Resistance Syndrome (DESIR) Study Group Ferritin and transferrin are both predictive of the onset of hyperglycemia in men and women over 3 years: the data from an epidemiological study on the Insulin Resistance Syndrome (DESIR) study. Diabetes Care. 2006;29:2090–4. doi: 10.2337/dc06-0093. [DOI] [PubMed] [Google Scholar]
- 94.Rajpathak SN, Crandall JP, Wylie-Rosett J, Kabat GC, Rohan TE, Hu FB. The role of iron in type 2 diabetes in humans. Biochim Biophys Acta. 2009;1790:671–81. doi: 10.1016/j.bbagen.2008.04.005. [DOI] [PubMed] [Google Scholar]
- 95.Lao TT, Chan PL, Tam KF. Gestational diabetes mellitus in the last trimester – a feature of maternal iron excess? Diabet Med. 2001;18:218–23. doi: 10.1046/j.1464-5491.2001.00453.x. [DOI] [PubMed] [Google Scholar]
- 96.Lao TT, Tam KF. Maternal serum ferritin and gestational impaired glucose tolerance. Diabetes Care. 1997;20:1368–9. doi: 10.2337/diacare.20.9.1368. [DOI] [PubMed] [Google Scholar]
- 97.Chen X, Scholl TO, Stein TP. Association of elevated serum ferritin levels and the risk of gestational diabetes mellitus in pregnant women: The Camden study. Diabetes Care. 2006;29:1077–82. doi: 10.2337/diacare.2951077. [DOI] [PubMed] [Google Scholar]
- 98.Tarim E, Kilicdag E, Bagis T, Ergin T. High maternal hemoglobin and ferritin values as risk factors for gestational diabetes. Int J Gynaecol Obstet. 2004;84:259–61. doi: 10.1016/S0020-7292(03)00341-2. [DOI] [PubMed] [Google Scholar]
- 99.Lee DH, Liu DY, Jacobs DR, Jr, et al. Common presence of non-transferrin-bound iron among patients with type 2 diabetes. Diabetes Care. 2006;29:1090–5. doi: 10.2337/diacare.2951090. [DOI] [PubMed] [Google Scholar]
- 100.Salonen JT, Tuomainen TP, Nyyssonen K, Lakka HM, Punnonen K. Relation between iron stores and non-insulin dependent diabetes in men: case-control study. BMJ. 1998;317:727. doi: 10.1136/bmj.317.7160.727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Liu Q, Sun L, Tan Y, Wang G, Lin X, Cai L. Role of iron deficiency and overload in the pathogenesis of diabetes and diabetic complications. Curr Med Chem. 2009;16:113–29. doi: 10.2174/092986709787002862. [DOI] [PubMed] [Google Scholar]
- 102.Swaminathan S, Fonseca VA, Alam MG, Shah SV. The role of iron in diabetes and its complications. Diabetes Care. 2007;30:1926–33. doi: 10.2337/dc06-2625. [DOI] [PubMed] [Google Scholar]
- 103.Ascherio A, Rimm EB, Giovannucci E, Willett WC, Stampfer MJ. Blood donations and risk of coronary heart disease in men. Circulation. 2001;103:52–7. doi: 10.1161/01.cir.103.1.52. [DOI] [PubMed] [Google Scholar]
- 104.Fernandez-Real JM, Lopez-Bermejo A, Ricart W. Iron stores, blood donation, and insulin sensitivity and secretion. Clin Chem. 2005;51:1201–5. doi: 10.1373/clinchem.2004.046847. [DOI] [PubMed] [Google Scholar]
- 105.Cutler P. Deferoxamine therapy in high-ferritin diabetes. Diabetes. 1989;38:1207–10. doi: 10.2337/diab.38.10.1207. [DOI] [PubMed] [Google Scholar]
- 106.Kannel WB, Hjortland MC, McNamara PM, Gordon T. Menopause and risk of cardiovascular disease: the Framingham study. Ann Intern Med. 1976;85:447–52. doi: 10.7326/0003-4819-85-4-447. [DOI] [PubMed] [Google Scholar]
- 107.Tuomainen TP, Punnonen K, Nyyssonen K, Salonen JT. Association between body iron stores and the risk of acute myocardial infarction in men. Circulation. 1998;97:1461–6. doi: 10.1161/01.cir.97.15.1461. [DOI] [PubMed] [Google Scholar]
- 108.Salonen JT, Nyyssonen K, Korpela H, Tuomilehto J, Seppänen R, Salonen R. High stored iron levels are associated with excess risk of myocardial infarction in eastern Finnish men. Circulation. 1992;86:803–11. doi: 10.1161/01.cir.86.3.803. [DOI] [PubMed] [Google Scholar]
- 109.Van Lenten BJ, Prieve J, Navab M, Hama S, Lusis AJ, Fogelman AM. Lipid-induced changes in intracellular iron homeostasis in vitro and in vivo. J Clin Invest. 1995;95:2104–10. doi: 10.1172/JCI117898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Stadler N, Lindner RA, Davies MJ. Direct detection and quantification of transition metal ions in human atherosclerotic plaques: evidence for the presence of elevated levels of iron and copper. Arterioscler Thromb Vasc Biol. 2004;24:949–54. doi: 10.1161/01.ATV.0000124892.90999.cb. [DOI] [PubMed] [Google Scholar]
- 111.de Valk B, Marx JJ. Iron, atherosclerosis, and ischemic heart disease. Arch Intern Med. 1999;159:1542–8. doi: 10.1001/archinte.159.14.1542. [DOI] [PubMed] [Google Scholar]
- 112.Asmis R, Begley JG. Oxidized LDL promotes peroxide-mediated mitochondrial dysfunction and cell death in human macrophages: a caspase-3-independent pathway. Circ Res. 2003;92:e20–9. doi: 10.1161/01.res.0000051886.43510.90. [DOI] [PubMed] [Google Scholar]
- 113.Matthews AJ, Vercellotti GM, Menchaca HJ, et al. Iron and atherosclerosis: inhibition by the iron chelator deferiprone (L1) J Surg Res. 1997;73:35–40. doi: 10.1006/jsre.1997.5180. [DOI] [PubMed] [Google Scholar]
- 114.Meyers DG. The iron hypothesis – does iron cause atherosclerosis? Clin Cardiol. 1996;19:925–9. doi: 10.1002/clc.4960191205. [DOI] [PubMed] [Google Scholar]
- 115.Sullivan JL. Iron in arterial plaque: modifiable risk factor for atherosclerosis. Biochim Biophys Acta. 2009;1790:718–23. doi: 10.1016/j.bbagen.2008.06.005. [DOI] [PubMed] [Google Scholar]
- 116.Kiechl S, Willeit J, Egger G, Poewe W, Oberhollenzer F. Body iron stores and the risk of carotid atherosclerosis: prospective results from the Bruneck study. Circulation. 1997;96:3300–7. doi: 10.1161/01.cir.96.10.3300. [DOI] [PubMed] [Google Scholar]
- 117.Meyers DG, Strickland D, Maloley PA, Seburg JK, Wilson JE, McManus BF. Possible association of a reduction in cardiovascular events with blood donation. Heart. 1997;78:188–93. doi: 10.1136/hrt.78.2.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Tuomainen TP, Salonen R, Nyyssonen K, Salonen JT. Cohort study of relation between donating blood and risk of myocardial infarction in 2682 men in eastern Finland. BMJ. 1997;314:793–4. doi: 10.1136/bmj.314.7083.793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Castellanos M, Puig N, Carbonell T, et al. Iron intake increases infarct volume after permanent middle cerebral artery occlusion in rats. Brain Res. 2002;952:1–6. doi: 10.1016/s0006-8993(02)03179-7. [DOI] [PubMed] [Google Scholar]
- 120.Kiechl S, Aichner F, Gerstenbrand F, et al. Body iron stores and presence of carotid atherosclerosis. Results from the Bruneck Study. Arterioscler Thromb. 1994;14:1625–30. doi: 10.1161/01.atv.14.10.1625. [DOI] [PubMed] [Google Scholar]
- 121.Davalos A, Fernandez-Real JM, Ricart W, et al. Iron-related damage in acute ischemic stroke. Stroke. 1994;25:1543–6. doi: 10.1161/01.str.25.8.1543. [DOI] [PubMed] [Google Scholar]
- 122.van der ADL, Grobbee DE, Roest M, Marx JJ, Voorbij HA, van der Schouw YT. Serum ferritin is a risk factor for stroke in postmenopausal women. Stroke. 2005;36:1637–41. doi: 10.1161/01.STR.0000173172.82880.72. [DOI] [PubMed] [Google Scholar]
- 123.Millan M, Sobrino T, Castellanos M, et al. Increased body iron stores are associated with poor outcome after thrombolytic treatment in acute stroke. Stroke. 2007;38:90–5. doi: 10.1161/01.STR.0000251798.25803.e0. [DOI] [PubMed] [Google Scholar]
- 124.Carbonell T, Rama R. Iron, oxidative stress and early neurological deterioration in ischemic stroke. Curr Med Chem. 2007;14:857–74. doi: 10.2174/092986707780363014. [DOI] [PubMed] [Google Scholar]
- 125.Hadzhieva M, Kirches E, Mawrin C. Review: iron metabolism and the role of iron in neurodegenerative disorders. Neuropathol Appl Neurobiol. 2014;40:240–57. doi: 10.1111/nan.12096. [DOI] [PubMed] [Google Scholar]
- 126.van Duijn S, Nabuurs RJ, van Duinen SG, Natté R. Comparison of histological techniques to visualize iron in paraffin-embedded brain tissue of patients with Alzheimer’s disease. J Histochem Cytochem. 2013;61:785–92. doi: 10.1369/0022155413501325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Mochizuki H, Yasuda T. Iron accumulation in Parkinson’s disease. J Neural Transm. 2012;119:1511–4. doi: 10.1007/s00702-012-0905-9. [DOI] [PubMed] [Google Scholar]
- 128.Veyrat-Durebex C, Corcia P, Mucha A, et al. Iron metabolism disturbance in a French cohort of ALS patients. Biomed Res Int. 2014;2014:485723. doi: 10.1155/2014/485723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Mainous AG, III, Gill JM, Everett CJ. Transferrin saturation, dietary iron intake, and risk of cancer. Ann Fam Med. 2005;3:131–7. doi: 10.1370/afm.283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Edgren G, Reilly M, Hjalgrim H, et al. Donation frequency, iron loss, and risk of cancer among blood donors. J Natl Cancer Inst. 2008;100:572–9. doi: 10.1093/jnci/djn084. [DOI] [PubMed] [Google Scholar]
- 131.Merk K, Mattsson B, Mattsson A, Holm G, Gullbring B, Björkholm M. The incidence of cancer among blood donors. Int J Epidemiol. 1990;19:505–9. doi: 10.1093/ije/19.3.505. [DOI] [PubMed] [Google Scholar]
- 132.Swede H, Hajduk AM, Sharma J, et al. Baseline serum C-reactive protein and death from colorectal cancer in the NHANES III cohort. Int J Cancer. 2014;134:1862–70. doi: 10.1002/ijc.28504. [DOI] [PubMed] [Google Scholar]
- 133.Deugnier Y. Iron and liver cancer. Alcohol. 2003;30:145–50. doi: 10.1016/s0741-8329(03)00129-0. [DOI] [PubMed] [Google Scholar]
- 134.Wurzelman JI, Silver A, Schreinemachers DM, Sandler RS, Everson RB. Iron intake and the risk of colorectal cancer. Cancer Epidemiol Biomarkers Prev. 1996;5:503–7. [PubMed] [Google Scholar]
- 135.Toyokuni S. Role of iron in carcinogenesis: cancer as a ferrotoxic disease. Cancer Sci. 2009;100:9–16. doi: 10.1111/j.1349-7006.2008.01001.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Bhasin G, Kauser H, Athar M. Low iron state is associated with reduced tumor promotion in a two-stage mouse skin carcinogenesis model. Food Chem Toxicol. 2002;40:1105–11. doi: 10.1016/s0278-6915(02)00056-x. [DOI] [PubMed] [Google Scholar]