Abstract
Independent researchers reported an alarming decline in life expectancy after 1990 among US non-Hispanic whites with less than a high school education. However, US educational attainment rose dramatically over the twentieth century; thus, focusing on changes in mortality rates of those not completing high school means looking at a different, shrinking, and increasingly vulnerable segment of the population in each year. We analyzed US data to examine the robustness of earlier findings to categorizing education in terms of relative rank in the overall distribution of each birth cohort, instead of by credentials such as high school graduation. Estimating trends in mortality for the bottom quartile, we found little evidence that survival probabilities declined dramatically. We conclude that widely publicized estimates of worsening mortality rates among whites with low socioeconomic position are highly sensitive to how educational attainment is classified. However, whites with low socioeconomic position, especially women, are not sharing in improving life expectancy, and disparities between US blacks and whites are entrenched. Findings underscore the urgency of an agenda to equitably disseminate new medical technologies and to deepen knowledge of social determinants of health and how it can be applied to promote the objective of achieving population health equity.
Despite a charge to public health policy makers and practitioners over the past twenty-five years to eliminate social disparities in health,[1] socioeconomic differentials in life expectancy have risen in recent decades, whether socioeconomic position is measured by education[2] or by earnings.[3]
Epidemiological, medical, and technological advances in the prevention, management, and treatment of life-threatening conditions have contributed to the overall increase in longevity.[4,5] In the absence of implementing health and social policies that include an equity component, higher-income and better-educated individuals appear to have disproportionately gained from such advances. Looking at changes during the 1990s, Ellen Meara and colleagues found that while all groups experienced some gains in life expectancy the gains among those with higher educational attainment were outpacing the gains among those with less education.[6] Even if all demographic groups reap some gains from technological advances, uneven access to them could explain the growth in socioeconomic inequality in life expectancy.
Some predicted that increasing obesity rates and prevalence of chronic diseases such as diabetes that disproportionately affect the less well-educated foreshadow a future drop in life expectancy in the United States and other developed countries.[7,8] More dramatically, some researchers concluded that among non-Hispanic whites, hereafter referred to as “whites,” with low educational attainment life expectancy is already declining.[9–12] Jennifer Montez and colleagues studied the education-mortality gradient by race, sex, and age between 1986 and 2006, finding that socioeconomic inequality in life expectancy steepened among white women and black women over the study period, and, at least for white women, it steepened as a function of both decreasing mortality risk among the higher educated and increasing mortality risk among those who did not complete high school.[9] Jay Olshansky and colleagues reported that between 1990 and 2008 the life expectancy of twenty-five-year-old US whites with less than a high school education fell by 3.4 years for men and 5.3 years for women.[10]
While possible, substantial drops in life expectancy are largely unprecedented in developed countries outside of periods of large-scale wars or fundamental political upheaval, such as the collapse of the Soviet Union.[13] Thus, these findings, if taken at face value, would be cause for alarm. One might not be surprised that these findings were highly publicized, garnering high-profile press attention.[14]
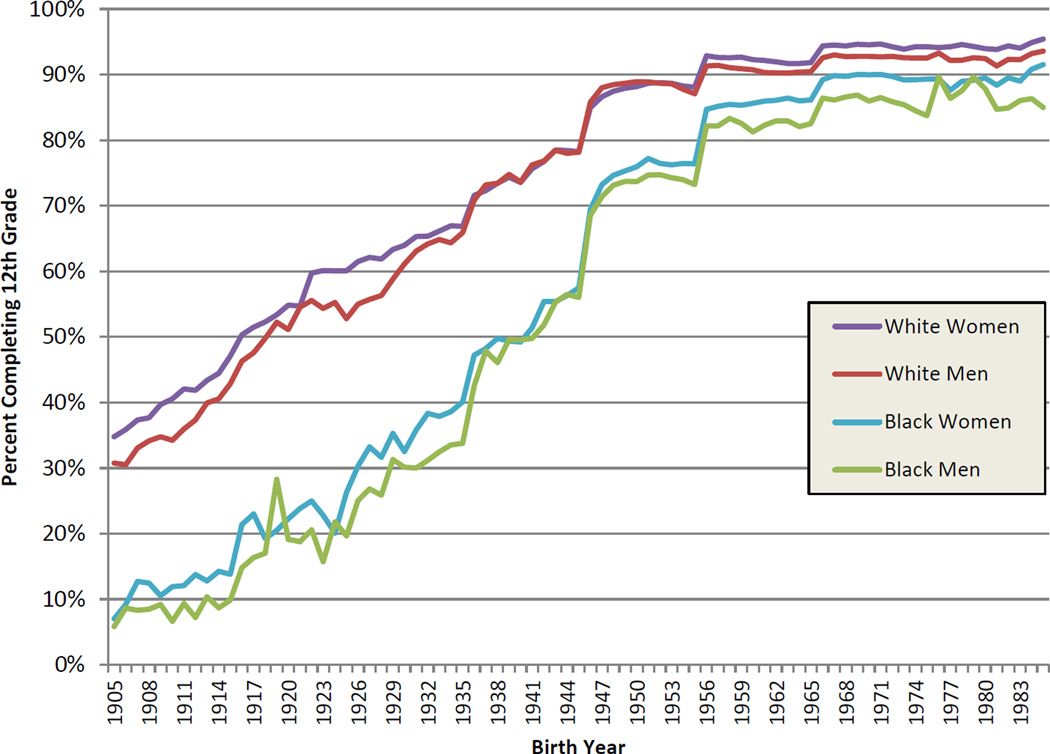
However, as discussed in a published exchange following the Olshansky and colleagues analysis,[15,16] some question the inference that proliferated in press accounts,[14] that lifespan has substantially decreased for disadvantaged whites. In particular, according to census data, the fraction of people reaching age twenty-five who had completed the twelfth grade changed dramatically over the twentieth century (Exhibit 1).[17]
Exhibit 1.
Percent Of Adults Completing Twelfth Grade, By Race, Sex, And Birth Year, 1905–85
Source/Notes: SOURCE Authors’ tabulations based on census data. NOTES “Whites” refers to non-Hispanic whites.
Indeed, if we examine distributions of the age at death for white women in 1990, half of all deaths occurred among women born between 1903 and 1921, cohorts in which high school graduation rates averaged 45 percent. By 2008 half of all deaths occurred among white women born between 1919 and 1937, cohorts in which graduation rates averaged 63 percent. Trends in age at death and graduation rates among white men show similar patterns. The difference in composition of the population with less than a high school education in 1990 compared to 2008 (who constituted the bottom 55 percent of the population in 1990 but the bottom 37 percent in 2008) suggests it may be misleading to interpret study results as if these were equivalent groups.
Recent simulations by Jennifer Dowd and Amar Hamoudi drive home this point:[18] If one simulates period life tables under plausible assumptions, including an increase in educational attainment over successive cohorts, one can reproduce the patterns observed by Olshansky and colleagues and Montez and colleagues even when all groups in the simulated data were experiencing increases in life expectancy.
We complemented these simulations empirically. Using the same data as used by Olshansky and colleagues, we categorized men’s and women’s educational attainment by relative rank within their birth cohorts. We found more modest evidence than earlier investigators that white women in the bottom quartile of the educational distribution faced shorter life expectancies in 2010 than they did in 1990. We found no evidence of any decline for white men or for black men or black women. However, population groups of low socioeconomic position, especially women, are not sharing equally, if at all, in improving mortality conditions.
Study Data And Methods
Following Olshansky and colleagues,[10] we analyzed data from the Multiple Cause-of-Death public use files, which contain individual-level information on decedents in the United States, including cause(s) of death, age, sex, race, ethnicity, educational attainment, and marital status.[10] To estimate the population at risk of death using the same covariates, we used data for US residents collected by the Census Bureau.[19] See the online Appendix for details on these calculations.[20]
First, we used the same analytic approach as Olshansky and colleagues to ensure that we could replicate their findings. Then, we categorized education in terms of relative ranks in the overall distribution for each cohort, instead of by credentials or number of years of education. Using census data, we estimated the twenty-fifth percentile of educational attainment for each birth cohort by race and sex (Appendix Exhibit 1).[20] Using these cut-points, we then used education as reported on the death certificate to calculate trends in mortality rates between 1990 and 2010 for those in the bottom quartile of the education distribution of their respective birth cohorts.
Study Results
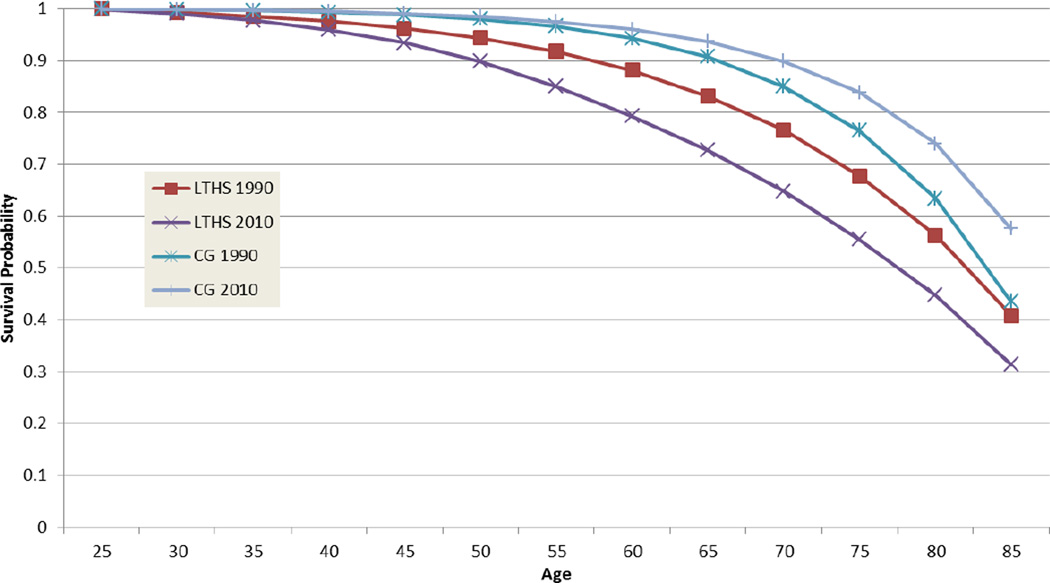
When we used the approach to classifying educational disadvantage of earlier researchers,[10,11] like them, we found dramatically declining survival probabilities among whites with less than a high school education. We found that if the age-specific rates of mortality observed in 1990 held throughout her life, a twenty-five-year-old white woman with less than a high school education had a 40.9 percent chance of surviving to age eighty-five (Exhibit 2). Under the rates observed in 2010, the same woman had only a 31.4 percent chance of surviving to age eighty-five. A twenty-five-year-old white man with less than a high school education had a 17.6 percent chance of surviving to age eighty-five based on 1990 observed rates. Under the rates observed in 2010, the same man had a 16.7 percent chance of surviving to age eighty-five (Exhibit 3). Also consistent with past research, we found that black women and black men did not show the same patterns (Appendix Exhibits 3 and 4).[20] While among those with less than a high school education, blacks gained in longevity between 1990 and 2010 relative to whites; blacks with higher levels of education made no relative gains. Combined with the lower rates of educational achievement among blacks relative to whites, the persistence of the gap at higher levels of education has meant that, on average, black life expectancy remained lower than white throughout the period.
Exhibit 2.
Survival Curves For White Women With Less Than A High School Education Compared To White Female College Graduates, 1990 And 2010
Source/Notes: SOURCE Authors’ tabulations based on National Vital Statistics System Multiple Cause-of-Death data and census data. NOTES LTHS is less than high school. CG is college graduate. “Whites” refers to non-Hispanic whites.
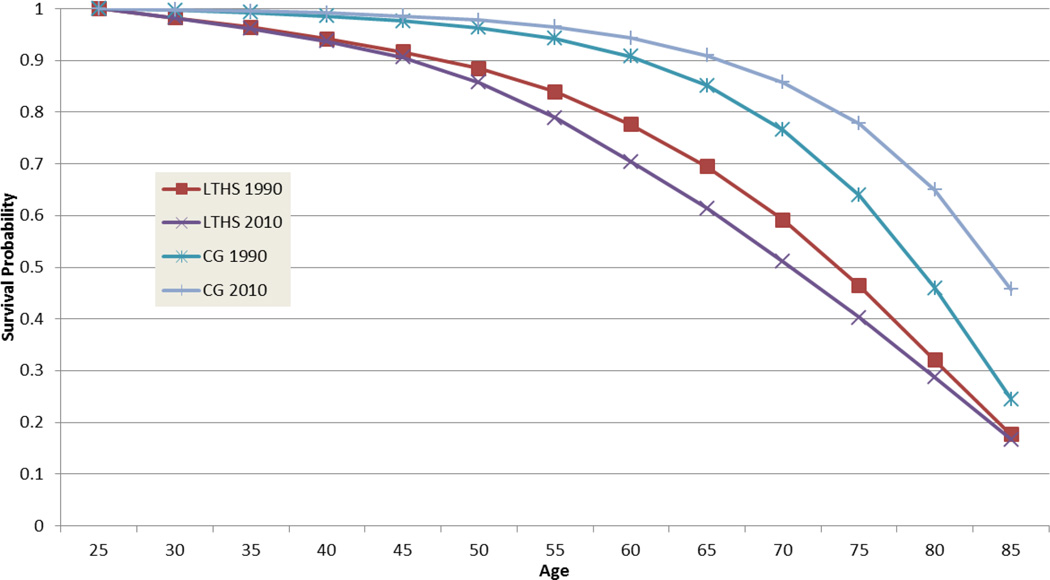
Exhibit 3.
Survival Curves For White Men With Less Than A High School Education Compared To White Male College Graduates, 1990 And 2010
Source/Notes: SOURCE Authors’ tabulations based on National Vital Statistics System Multiple Cause-of-Death data and census data. NOTES LTHS is less than high school. CG is college graduate. “Whites” refers to non-Hispanic whites.
As a summary measure of these results, we derived life expectancies from the estimated survival curves. The number of expected years lived between ages twenty-five and eighty-five rose for most groups but fell by 2.2 and 3.9 years for white men and white women with less than a high school education, respectively[21,22] (Appendix Exhibit 5).[20]
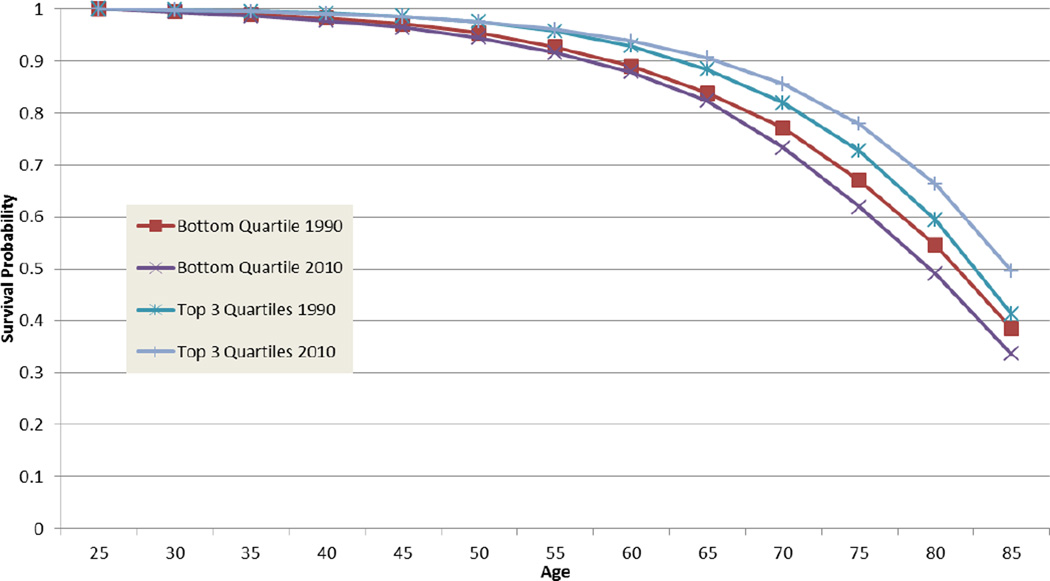
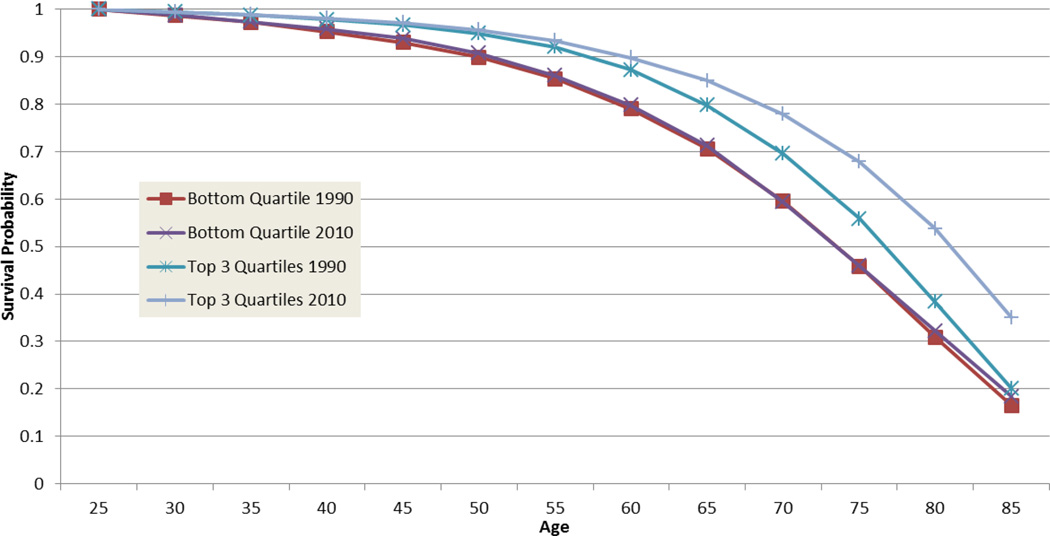
However, when we considered mortality rates by quartile rank in educational attainment, a different picture emerged. Appendix Exhibit 1 shows the thresholds that define the bottom quartile as derived from census data on educational attainment collected for each birth cohort when they were ages 25–35.[20] We found that white women in the bottom quartile had no appreciable change in survival rates through the age of sixty-five but showed some drop in survival rates at older ages (Exhibit 4). In contrast, women in the top three quartiles saw an increase in survival probability for every age. For white men, the lowest quartile showed small increases in survival through middle age, although the 1990 and 2010 survival curves lie more or less on top of each other, suggesting stagnation (Exhibit 5). In contrast, the top three quartiles saw increased survival probabilities between 1990 and 2010.
Exhibit 4.
Survival Curves For White Women By Quartile Rank In Educational Attainment, 1990 And 2010
Source/Notes: SOURCE Authors’ tabulations based on National Vital Statistics System Multiple Cause-of-Death data and census data. NOTES “Whites” refers to non-Hispanic whites.
Exhibit 5.
Survival Curves For White Men By Quartile Rank In Educational Attainment, 1990 And 2010
Source/Notes: SOURCE Authors’ tabulations based on National Vital Statistics System Multiple Cause-of-Death data and census data. NOTES “Whites” refers to non-Hispanic whites.
To summarize the shifts in the survival curves in a single statistic, we calculated life expectancy (Appendix Exhibit 7).[20] While life expectancy gains between 1990 and 2010 are apparent for white men and black men and black women in all education quartiles, our estimates do suggest that white women in the bottom quartile experience a modest decline (1.2 years, compared to a decline of 3.9 years based on the less than a high school education measure). White men in the bottom quartile experience a 0.4 years increase compared to a decline of 2.2 years based on the less than a high school education measure. Whites in the top 75 percent of the educational distribution experience gains of 1.2 years for women and 2.8 years for men. Consistent with other literature,[3] we see clear evidence of increasing inequality in survival probabilities between those in the bottom and those in the top of the educational distribution.
Discussion
Between 1990 and 2010, white women of low socioeconomic position older than age sixty-five experienced a modest decrease in life expectancy. Yet we find little evidence to support the conclusion that any segment of the white or black population suffered a dramatic drop in life expectancy. The fact that we analyzed the same data sets as Olshansky and colleagues and were able to replicate their findings before considering our alternative hypothesis supports the interpretation that their highly publicized conclusion of dramatically decreasing life expectancy for some groups was misleading, likely an artifact of an increasingly disadvantaged or adversely selected group of people with less than a high school education between 1990 and 2010. Focusing on mortality rates of those with less than a high school education over a twenty-year period means looking at a different, shrinking, and increasingly vulnerable segment of the population in each year.
Consistent with earlier studies,[9,10] we found that black and white men and women of all ages at the low end of the education distribution have lost significant ground in life expectancy in relative terms. As with recent findings on disparity in economic outcomes,[23] mortality also appears to be trending toward greater inequality.
The robustness of our findings is supported by other recent analyses using different methods and data.[24,25] The data that both Olshansky and colleagues and we used involved matching vital statistics and census data aggregated by age, sex, race, and educational attainment. As we elaborate in the Appendix,[20] such matching can lead to an underestimation of death rates for those with less than a high school education at any single point in time. However, we know of no reason or evidence to suggest that magnitude of this bias has changed over time.
Other researchers have used individually matched survey and administrative data.[24,25] This method avoids the potential mismatch problems of aggregate data and allows for more consistent measurement of education over time and across geographic areas; however, sample sizes are much smaller than available in the Multiple Cause-of-Death files we used and the surveys analyzed exclude the institutionalized population, unlike our data. The fact that researchers using different data sets have obtained similar findings suggests that these findings are not simply artifacts of the data being used but reflect actual changes in mortality.
While the large drops in life expectancy that were observed for those with less than a high school education seem implausible short of cataclysmic social circumstances, the more modest drops and stagnation we observed are robust and disturbing. While some have suggested that changes in obesity and smoking behavior might play an important role,[26] we suspect that the contribution of individual health behavior to population health disparities may be overstated. The evidence on the impact of changes in obesity on mortality is, at best, mixed.[26] Researchers who have directly examined the role of smoking estimated that the differential decline in smoking behavior among women of higher socioeconomic position can account for only a small portion of the growing gap between the higher and lower groups.[6,27] However, it seems less likely that smoking behavior can account for rising mortality rates among the less well-educated. Our tabulations using the 1991 and 2010 National Health Interview Survey showed little change in the fraction of less well-educated white women who report having ever smoked.
If the impact of individual behavioral risks on population health disparities have been overstated, the role of social determinants of health inequity have been oversimplified.[28] Real wages have eroded for the working and middle classes over recent decades, with income, wealth, and educational inequalities growing to unprecedented levels. There is robust evidence that access to material and educational resources enhances health.[29] Questions of material resources and academic achievement are only a part of the story as other social research demonstrates that residential and work environments for low-income populations are rife with exposure to health harmful and environmental stressors.[30] Growing mixed methods and interdisciplinary research emphasizes how social disadvantage may trigger the repeated activation of physiological stress processes with resultant impacts on population health and mortality.[30,31] Repeated or chronic exposure to stress hormones causes wear and tear on body systems (allostatic load) and increases susceptibility to infectious disease; early onset of chronic diseases such as hypertension, diabetes, morbid obesity, and metabolic syndrome; as well as mood disorders, functional limitations, accelerated aging, and excess death.[30,32–34] Evidence of such population weathering has been well-documented in the United States for blacks compared to whites, on average, and among the poorest urban and poorest rural whites compared to white national averages.[30,31,34]
Policy Implications
The robust evidence that life expectancy has not been rising for segments of the US population of low socioeconomic position, and that the presence of gaps in life expectancy between the low socioeconomic group and higher socioeconomic groups have widened, should inform social as well as health policy approaches and priorities. Thus, for example, increasing the normal retirement age is a frequently discussed reform to the Social Security system, and some argue for increasing the age of Medicare eligibility to relieve financial pressure on the system. Our findings emphasize that basing this type of policy decision on the increased life expectancy for the US population overall is an inequitable way to consider reforms to such policies and is likely to have regressive impacts.
More globally, with the governmental release of each decennial Healthy People national public health objectives, the goal of eliminating health disparities continues to be reaffirmed. As noted in the most recent Healthy People 2020: “During the past 2 decades, one of Healthy People’s overarching goals has focused on disparities. In Healthy People 2000, it was to reduce health disparities among Americans. In Healthy People 2010, it was to eliminate, not just reduce, health disparities. In Healthy People 2020, that goal was expanded even further: to achieve health equity, eliminate disparities, and improve the health of all groups.”[1]
Studies that have consistently found that health inequity has persisted and even grown confirm the failure to meet these important objectives and raise the question: What should be done differently?
Studies of trends in causes of mortality disparities suggest that failure to adequately address excessive rates of complex and chronic disease among reproductive and working-age adults in high-poverty locales limited the extent to which progress has been made in reducing excess mortality.[34] Population differences in the early onset of chronic disease seen in the low socioeconomic group result from the qualitatively different life experiences, exposure to stressors, and unequal access to coping resources. Standard approaches to promoting population health have placed heavy emphasis on improving clinical treatments and individual health behavior change interventions. The United States’ poor track record implies these standard approaches alone have proved insufficient to the task.
Increasing attention to policies to promote healthy physical environments that also facilitate healthy behavior--for example, ensuring access to grocery stores and safe exercise spaces in all neighborhoods--is a positive enhancement to the healthy lifestyles agenda.[35–37] So, too, expanding the accessibility of health insurance through the Affordable Care Act is a positive step. However, if the nation is committed to health equity, additional steps to better align the policy agenda with professed national public health goals are indicated.
First, in the realm of health services, studies point to dwindling in number and underresourced safety-net hospitals that are ill-equipped to deal with complex health issues as one important contributor to health inequity.[38] Health service delivery must address the twenty-first-century complex and chronic disease mix, generally,[39] and population- and geography-specific disease mixes, in particular.[34] Prioritizing ways to ensure well-matched health services are accessible to the poor where they live is essential.
Second, studies point to growing inequality in gains to life expectancy being a function of differential access to advances in epidemiological knowledge and technological innovation.[4,5,30] To the extent that the allocation of new biomedical technologies favors those with the deepest pockets and most generous health benefits, health disparities are likely to become entrenched and continue to grow.[5] An explicit equity agenda needs to be developed and applied to the dissemination of new medical technologies, pharmaceutical treatments, and developments in precision medicine.
Third, although the growing and well-funded scientific initiatives to improve precision medicine may, as some commentators recently stated, “ultimately make critical contributions to a narrow set of conditions that are primarily genetically determined,”[40(p501)] the growing consensus is that they will not address population health disparities.[41] Yet, as vast resources are being applied to these endeavors, National Institutes of Health funding for public and population health projects has plummeted.[40] Socially grounded, mixed methods, and community-based participatory research can provide windows into the stressors that loom large in specific low socioeconomic populations but are otherwise unfamiliar to many policy makers.[30] Consistent with forwarding a health equity agenda, a better balance of research funding between precision medicine and population health research should be achieved.
Conclusion
Robust evidence refutes a dramatic decline in life expectancy for any race-sex group in the United States in recent decades. While no cataclysmic events of the magnitude one might expect to see an alarming decline have occurred, the more modest evidence of a decline for white women of low socioeconomic status and the entrenchment or even growth of other race-sex socioeconomic inequalities in longevity appear to signal chronic and insidious processes. We recommend drawing on a broader set of evidenced-based remedies than only individual behavior change or universal health insurance, to develop and implement a successful health equity policy agenda.[42]
Supplementary Material
Acknowledgments
This work was supported by the Social Security Administration (SSA) and through the Retirement Research Consortium. This research was also supported in part by a National Institutes of Health training grant to the Population Studies Center at the University of Michigan (Grant No. T32 HD007339). The findings and conclusions expressed are solely those of the authors and do not represent the views of the SSA, any agency of the federal government, the University of Michigan, Mathematica Policy Research, or the Urban Institute. A previous version of this article was presented at the sixteenth annual Retirement Research Consortium Meeting, August 7–8, 2014, in Washington, D.C. The authors thank Kyle Caswell for advice and assistance using historical census data, and Stephen Goss, chief actuary at the SSA, anonymous reviewers, and other meeting participants for helpful comments.
Biographies
John Bound is a professor in the Department of Economics at the University of Michigan, in Ann Arbor.
Arline T. Geronimus is a professor in the School of Public Health at the University of Michigan.
Javier M. Rodriguez is a health researcher at Mathematica Policy Research, in Ann Arbor.
Timothy A. Waidmann (twaidmann@urban.org) is a senior fellow in the Health Policy Center at the Urban Institute, in Washington, D.C.
Contributor Information
John Bound, Department of Economics at the University of Michigan, in Ann Arbor.
Arline T. Geronimus, School of Public Health at the University of Michigan.
Javier M. Rodriguez, Mathematica Policy Research in Ann Arbor.
Timothy A. Waidmann, Email: twaidmann@urban.org, Health Policy Center at the Urban Institute, in Washington, D.C.
Notes
- 1. HealthyPeople.gov. Rockville (MD): Office of Disease Prevention and Health Promotion; [cited 2015 Oct 22]. Disparities [Internet] Available from: http://www.healthypeople.gov/2020/about/foundation-health-measures/Disparities. [Google Scholar]
- 2.Preston SH, Elo IT. Are educational differentials in adult mortality increasing in the United States? J Aging Health. 1995;7(4):476–496. doi: 10.1177/089826439500700402. [DOI] [PubMed] [Google Scholar]
- 3.Waldron H. Trends in mortality differentials and life expectancy for male Social Security-covered workers, by socioeconomic status. Soc Secur Bull. 2007;67(3):1–28. [PubMed] [Google Scholar]
- 4.Goldman DP, Lakdawalla DN. A theory of health disparities and medical technology. Contrib Econ Anal Policy. 2005;4(1):1–32. [Google Scholar]
- 5.Link BG, Phelan J. Social conditions as fundamental causes of disease. J Health Soc Behav. 1995;35(Spec No):80–94. [PubMed] [Google Scholar]
- 6.Meara ER, Richards S, Cutler DM. The gap gets bigger: changes in mortality and life expectancy, by education, 1981–2000. Health Aff (Millwood) 2008;27(2):350–360. doi: 10.1377/hlthaff.27.2.350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Olshansky SJ, Passaro DJ, Hershow RC, Layden J, Carnes BA, Brody J, et al. A potential decline in life expectancy in the United States in the 21st century. N Engl J Med. 2005;352(11):1138–1145. doi: 10.1056/NEJMsr043743. [DOI] [PubMed] [Google Scholar]
- 8.Stewart ST, Cutler DM, Rosen AB. Forecasting the effects of obesity and smoking on U.S. life expectancy. N Engl J Med. 2009;361(23):2252–2260. doi: 10.1056/NEJMsa0900459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Montez JK, Hummer RA, Hayward MD, Woo H, Rogers RG. Trends in the educational gradient of U.S. adult mortality from 1986 to 2006 by race, gender, and age group. Res Aging. 2011;33(2):145–171. doi: 10.1177/0164027510392388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Olshansky SJ, Antonucci T, Berkman L, Binstock RH, Boersch-Supan A, Cacioppo JT, et al. Differences in life expectancy due to race and educational differences are widening, and many may not catch up. Health Aff (Millwood) 2012;31(8):1803–1813. doi: 10.1377/hlthaff.2011.0746. [DOI] [PubMed] [Google Scholar]
- 11.Kindig DA, Cheng ER. Even as mortality fell in most US counties, female mortality nonetheless rose in 42.8 percent of counties from 1992 to 2006. Health Aff (Millwood) 2013;32(3):451–458. doi: 10.1377/hlthaff.2011.0892. [DOI] [PubMed] [Google Scholar]
- 12.Montez JK, Zajacova A. Trends in mortality risk by education level and cause of death among US white women from 1986 to 2006. Am J Public Health. 2013;103(3):473–479. doi: 10.2105/AJPH.2012.301128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stuckler D, Basu S. The body economic: why austerity kills. New York (NY): Basic Books; 2013. p. 240. [Google Scholar]
- 14.Tavernise S. Life spans shrink for least-educated whites in the U.S. New York Times [serial on the Internet] [cited 2015 Oct 22];2012 Sep 20; Available from: http://www.nytimes.com/2012/09/21/us/life-expectancy-for-less-educated-whites-in-us-is-shrinking.html. [Google Scholar]
- 15.Begier B, Li W, Maduro G. Life expectancy among non-high school graduates. Health Aff (Millwood) 2013;32(4):822. doi: 10.1377/hlthaff.2013.0198. [DOI] [PubMed] [Google Scholar]
- 16.Olshansky SJ. Life expectancy and education: the author replies. Health Aff (Millwood) 2013;32(4):822. doi: 10.1377/hlthaff.2013.0200. [DOI] [PubMed] [Google Scholar]
- 17.For each cohort, we used the census data file from the first appearance of the cohort after they turned age twenty-five. Thus, for cohorts born from 1905 to 1915, we used the 1940 decennial census; for cohorts born from 1916 to 1925, we used the 1950 decennial, and so forth.
- 18.Dowd JB, Hamoudi A. Is life expectancy really falling for groups of low socio-economic status? Lagged selection bias and artefactual trends in mortality. Int J Epidemiol. 2014;43(4):983–988. doi: 10.1093/ije/dyu120. [DOI] [PubMed] [Google Scholar]
- 19.Ruggles S, Genadek K, Goeken R, Grover J, Sobek M. Integrated Public Use Microdata Series: Version 6.0 (machine-readable database) [Internet] Minneapolis (MN): University of Minnesota; 2010. [cited 2015 Oct 22]. Available from: usa.ipums.org. [Google Scholar]
- 20.To access the Appendix, click on the Appendix link in the box to the right of the article online.
- 21.That we found these results when we limited the population studied to ages 25–84 suggests that the techniques that Jay Olshansky and colleagues used to address the particular complications of measuring age among the oldest old (ages eighty-five and older) (see Note 22) do not threaten the validity of their findings, another concern one might have had.
- 22.Coale AJ, Kisker EE. Defects in data on old-age mortality in the United States: new procedures for calculating mortality schedules and life tables at the highest ages. Asian Pac Popul Forum. 1990;4(1):32. [Google Scholar]
- 23.DeNavas-Walt C, Proctor BD. Washington (DC): Census Bureau; 2014. Sep, [cited 2015 Oct 22]. Income and poverty in the United States: 2013 [Internet] Table A–2, Selected measures of household income dispersion: 1967 to 2013; (Report No.: P60-249). Available from: http://www.census.gov/content/dam/Census/library/publications/2014/demo/p60-249.pdf. [Google Scholar]
- 24.Goldring T, Lange F, Richards-Shubik S. Testing for changes in the SES-mortality gradient when the distribution of education changes too [Internet] Cambridge (MA): National Bureau of Economic Research; 2015. Feb, [cited 2015 Oct 22]. (Report No.: 20993). Available from: http://www.nber.org/papers/w20993. [DOI] [PubMed] [Google Scholar]
- 25.Hendi AS. Trends in U.S. life expectancy gradients: the role of changing educational composition. Int J Epidemiol. 2014;44(3):946–955. doi: 10.1093/ije/dyv062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Crimmins EM, Preston SH, Cohen B, editors. International differences in mortality at older ages: dimensions and sources. Washington (DC): National Academies Press; 2010. [PubMed] [Google Scholar]
- 27.Cutler DM, Lange F, Meara E, Richards-Shubik S, Ruhm CJ. Rising educational gradients in mortality: the role of behavioral risk factors. J Health Econ. 2011;30(6):1174–1187. doi: 10.1016/j.jhealeco.2011.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pearson JA. Can’t buy me whiteness: new lessons from the Titanic on race, ethnicity, and health. DuBois Rev Soc Sci Res Race. 2008;5(1):27–47. [Google Scholar]
- 29.Lynch J, Smith GD, Harper S, Hillemeier M, Ross N, Kaplan GA, et al. Is income inequality a determinant of population health? Part 1. A systematic review. Milbank Q. 2004;82(1):5–99. doi: 10.1111/j.0887-378X.2004.00302.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Geronimus AT, Pearson JA, Linnenbringer E, Schulz AJ, Reyes AG, Epel ES, et al. Race-ethnicity, poverty, urban stressors, and telomere length in a Detroit community-based sample. J Health Soc Behav. 2015;56(2):199–224. doi: 10.1177/0022146515582100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Geronimus AT, Hicken M, Keene D, Bound J. “Weathering” and age patterns of allostatic load scores among blacks and whites in the United States. Am J Public Health. 2006;96(5):826–833. doi: 10.2105/AJPH.2004.060749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Seeman TE, McEwen BS, Rowe JW, Singer BH. Allostatic load as a marker of cumulative biological risk: MacArthur studies of successful aging. Proc Natl Acad Sci USA. 2001;98(8):4770–4775. doi: 10.1073/pnas.081072698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McEwen BS. Protective and damaging effects of stress mediators. N Engl J Med. 1998;338(3):171–179. doi: 10.1056/NEJM199801153380307. [DOI] [PubMed] [Google Scholar]
- 34.Geronimus AT, Bound J, Colen CG. Excess black mortality in the United States and in selected black and white high-poverty areas, 1980–2000. Am J Public Health. 2011;101(4):720–729. doi: 10.2105/AJPH.2010.195537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zenk SN, Powell LM, Rimkus L, Isgor Z, Barker DC, Ohri-Vachaspati P, et al. Relative and absolute availability of healthier food and beverage alternatives across communities in the United States. Am J Public Health. 2014;104(11):2170–2178. doi: 10.2105/AJPH.2014.302113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Perdue WC, Stone LA, Gostin LO. The built environment and its relationship to the public’s health: the legal framework. Am J Public Health. 2003;93(9):1390–1394. doi: 10.2105/ajph.93.9.1390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sallis JF, Glanz K. Physical activity and food environments: solutions to the obesity epidemic. Milbank Q. 2009;87(1):123–154. doi: 10.1111/j.1468-0009.2009.00550.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gilman M, Adams EK, Hockenberry JM, Wilson IB, Milstein AS, Becker ER. California safety-net hospitals likely to be penalized by ACA value, readmission, and meaningful-use programs. Health Aff (Millwood) 2014;33(8):1314–1322. doi: 10.1377/hlthaff.2014.0138. [DOI] [PubMed] [Google Scholar]
- 39.Rifkin DE. A fighting chance: how acute care training is failing patients with chronic disease. Health Aff (Millwood) 2014;33(8):1481–1484. doi: 10.1377/hlthaff.2013.0461. [DOI] [PubMed] [Google Scholar]
- 40.Bayer R, Galea S. Public health in the precision-medicine era. N Engl J Med. 2015;373(6):499–501. doi: 10.1056/NEJMp1506241. [DOI] [PubMed] [Google Scholar]
- 41.Geronimus AT. Deep integration: letting the epigenome out of the bottle without losing sight of the structural origins of population health. Am J Public Health. 2013;103(Suppl 1):S56–S63. doi: 10.2105/AJPH.2013.301380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Centers for Disease Control and Prevention. Atlanta (GA): CDC; [cited 2015 Oct 22]. National Vital Statistics System: public use data file documentation: mortality multiple cause-of-death [Internet] last updated 2014 Dec 30 Available from: http://www.cdc.gov/nchs/nvss/mortality_public_use_data.htm. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.