Abstract
Background
Although considerable research describes the cardiovascular effects of habitual moderate and heavy alcohol consumption, the immediate risks following alcohol intake have not been well characterized. Based on its physiological effects, alcohol may have markedly different effects on immediate and long-term risk.
Methods and Results
We searched CINAHL, Embase, and PubMed from inception to March 12 2015, supplemented with manual screening for observational studies assessing the association between alcohol intake and cardiovascular events in the following hours and days.
We calculated pooled relative risks (RRs) and 95% confidence intervals (CIs) for the association between alcohol intake and myocardial infarction (MI), ischemic stroke (IS) and hemorrhagic stroke (HS) using DerSimonian and Laird random-effects models to model any alcohol intake or dose-response relationships of alcohol intake and cardiovascular events. Among 1056 citations and 37 full-text articles reviewed, 23 studies (29457 participants) were included. Moderate alcohol consumption was associated with an immediately higher cardiovascular risk that was attenuated after 24 hours, and even protective for MI and HS (≈2–4 drinks: RR=30% lower risk), and protective against IS within one week (≈6 drinks: 19% lower risk). In contrast, heavy alcohol drinking was associated with higher cardiovascular risk in the following day (≈6–9 drinks: RR=1.3–2.3) and week (≈19–30 drinks: RR=2.25–6.2).
Conclusions
There appears to be a consistent finding of an immediately higher cardiovascular risk following any alcohol consumption but by 24 hours, only heavy alcohol intake conferred continued risk.
Keywords: dose-response meta-analysis, alcohol, cardiovascular disease, epidemiology
Introduction
It is well-recognized that moderate alcohol intake has long-term cardiovascular benefits but even protective exposures can lead to acutely increased risk. Alcohol has biphasic and complex physiological effects that result in both higher and lower cardiovascular risk depending on the amount consumed, drinking frequency and the outcome under study.1, 2 For instance, moderate and high alcohol intake is associated with increased heart rate,3 electromechanical delay4 and impaired fibrinolysis5 within hours of intake but there are long-term improvements in blood pressure6 and coagulation.7 In addition, the risk of cardiovascular events triggered by alcohol may be modified by usual drinking patterns.1 There has been no comprehensive study to investigate the acute cardiovascular risk following alcohol intake. Therefore, we conducted a systematic review and dose-response meta-analysis of the evidence on the risk of myocardial infarction (MI), ischemic stroke (IS) and hemorrhagic stroke (HS) in the hours and days after alcohol intake. The primary hypothesis defined before initiation of the literature review was that compared to no alcohol consumption, moderate alcohol consumption is associated with an immediately higher risk of cardiovascular events that becomes protective after 24 hours, whereas heavy alcohol drinking is associated with higher cardiovascular risk both immediately and in the following days.
Methods
We performed a systematic review, meta-analysis and dose-response meta-analysis in accordance with the Meta-Analysis of Observational Studies in Epidemiology8 protocol throughout the design, implementation, analysis and reporting for this study.
Data Sources and Searches
One person (EM) performed a literature search of the CINAHL, Embase, and PubMed databases from January 1966 through March 2015 using free-text words and Medical Subject Headings terms without language restrictions. We also reviewed reference lists of retrieved articles.
Study Selection
Using a standardized form, two readers (EM, HSC) independently and in duplicate reviewed the list of identified articles and extracted data from selected articles with disagreements adjudicated by consensus. We selected studies with abstracts suggesting they were relevant. Studies were eligible for review if: (1) the design was a cohort, case-control, self-controlled case series or case-crossover study; (2) the investigators reported relative risks (RRs) and 95% confidence intervals (CIs) for the association between alcohol intake and MI, IS or HS (3) the investigators retrospectively evaluated alcohol intake directly from the participant or by proxy for the 1 week period before event onset. We excluded studies that evaluated the impact of laboratory-administered alcohol on myocardial ischemia, arrhythmia, atrial fibrillation, or intermediate outcomes such as blood pressure or cardiovascular reactivity.
Data Extraction and Quality Assessment
For each study, we recorded the following details: first author, year of publication, study location, hazard period, referent period or sample, number of cases and non-cases at each level of alcohol intake, amount of alcohol consumed prior to event onset, RRs and corresponding 95% CIs and covariates included in statistical models. When analyses of the same population were reported more than once, we included the largest study for the appropriate analysis. In case-control studies, cases and non-cases were interviewed about recent alcohol consumption, and potential confounding by between-person differences were addressed with matching and/or statistical adjustment. In case-crossover studies, each case was interviewed about recent alcohol intake and that same individual’s alcohol intake at other times. By comparing the same individual at different times, confounding by fixed characteristics is eliminated. When case-crossover studies reported estimates using either a referent of usual frequency of alcohol intake over several months or a referent of intake at the same time on the prior day, we included the estimates based on usual frequency. When studies reported estimates from several models, we included the estimates from the model with the greatest control for potential confounding. We also recorded information on whether the study was restricted to incident events, whether both fatal and nonfatal events were included and whether the study was restricted to current drinkers.
We qualitatively assessed study quality by recording the timing between onset of the cardiovascular event and ascertainment of alcohol intake, whether alcohol intake was assessed with an interview or questionnaire and whether proxy respondents provided information on alcohol intake.
Data Synthesis and Analysis
Details of the meta-analysis methods are provided in the Online Appendix and are summarized briefly here.
Meta-Analysis of Any Alcohol Intake
For each outcome and hazard period, we included one RR and corresponding 95%CI per study reporting the change in cardiovascular risk immediately following any alcohol intake compared to no alcohol intake. For studies that did not report an overall RR, we first pooled the RRs across sex and/or levels of alcohol consumption by using a random-effects model. We used DerSimonian and Laird9 random-effects models to pool the RRs across studies for each outcome and each hazard period.
Dose-Response Meta-Analysis
To examine the impact of the amount of alcohol consumed prior to event onset, we conducted a dose-response meta-analysis for each outcome and the risk in the day and week following intake. For each study, we assigned the median or mean grams of alcohol intake for each exposure level to the corresponding RR. To examine potential nonlinear relationships between alcohol intake and cardiovascular risk, we performed 2-stage random-effects dose–response meta-analyses.10 We estimated the predicted relative risk comparing specific levels of alcohol intake compared to no alcohol intake based on the linear or model or spline transformation, as appropriate.
For the analyses of any intake and the dose-response analyses, we evaluated heterogeneity across studies with the Cochrane Q χ2 test11 and we calculated the I2 statistic to quantify the proportion of between-study heterogeneity attributable to variability in the association rather than sampling variation.12
Statistical analyses were conducted with 2-tailed α set at ≤0.05 for statistical significance. We used Stata (version 13.0, StataCorp, College Station, TX, USA) packages to conduct the meta-analyses of any alcohol intake (metan), dose-response analyses (glst), and evaluation of potential publication bias (metabias) and information bias (metainf).
Results
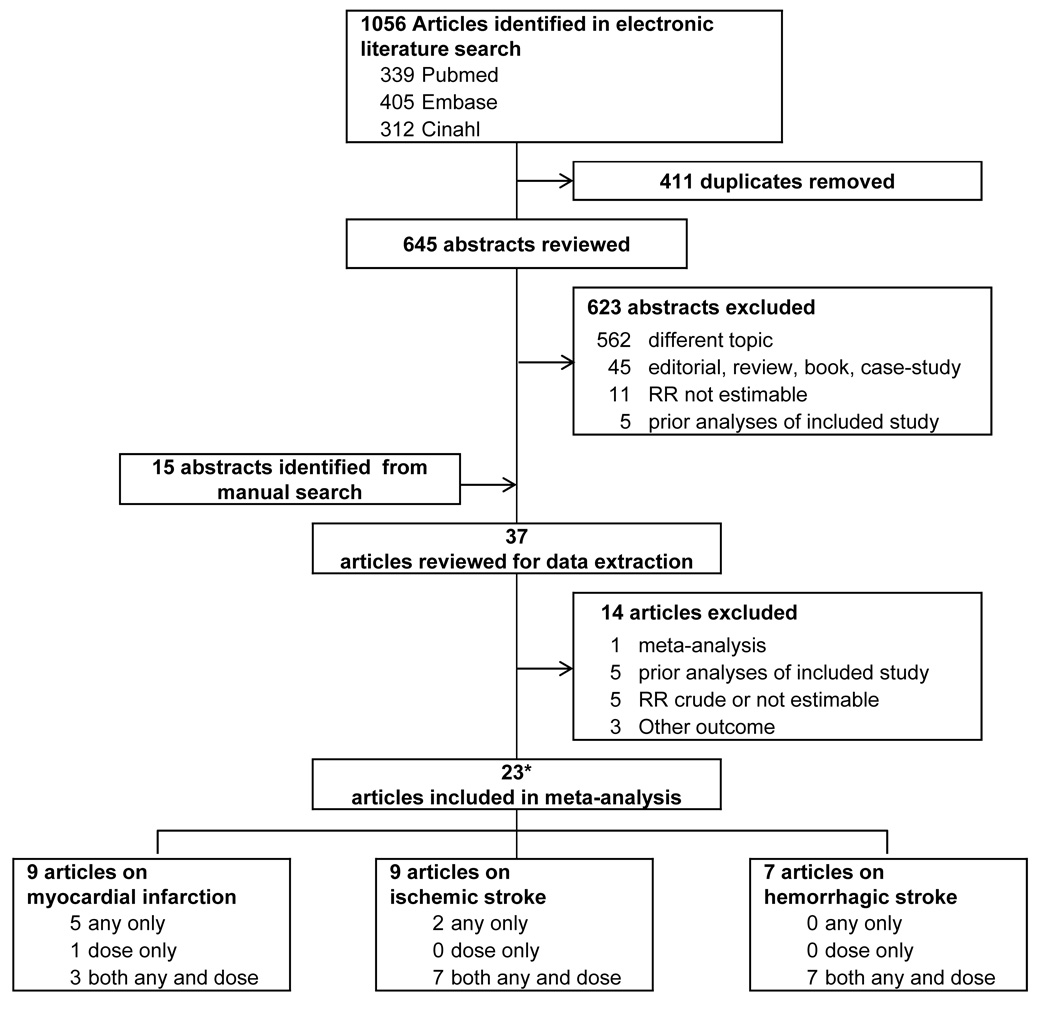
The literature search identified 1056 publications. We excluded 411 duplicates, and 623 articles were excluded after review of the title or abstract. An additional 15 articles were identified from manual searches and review of bibliographies of relevant studies. After reviewing the articles, another 14 papers were excluded, resulting in a meta-analysis of 23 articles (Figure 1). The eTable summarizes the characteristics of the eligible studies. The meta-analysis included 16 case-control and 7 case-crossover studies published in 1987–2015. Combined, there were 29457 participants including 17966 cases of MI, 2599 cases of IS and 1262 cases of HS. Eleven studies were conducted in Europe, one in Russia, four in the United States, two in New Zealand, four in Australia, and one study included participants from 52 countries worldwide. Two studies included men only, one included women only, and the remaining twenty studies enrolled men and women but only six presented sex-specific estimates, with one reporting an infinite RR for women so we included the estimate combining all participants. Fourteen studies were restricted to incident events. Alcohol consumption was assessed with a questionnaire in three studies and with interviews in all others. In ten studies, the estimated median alcohol consumption in the highest category was >4 drinks per day for men and women combined or for men but not women.
Figure 1.
Selection of studies published in 1966–2015 with information on any recent alcohol intake or a specific dose of recent alcohol intake included in a meta-analysis of alcohol consumption and risk of cardiovascular events. *One study included data on myocardial infarction and hemorrhagic stroke and one study included data on ischemic stroke and hemorrhagic stroke.
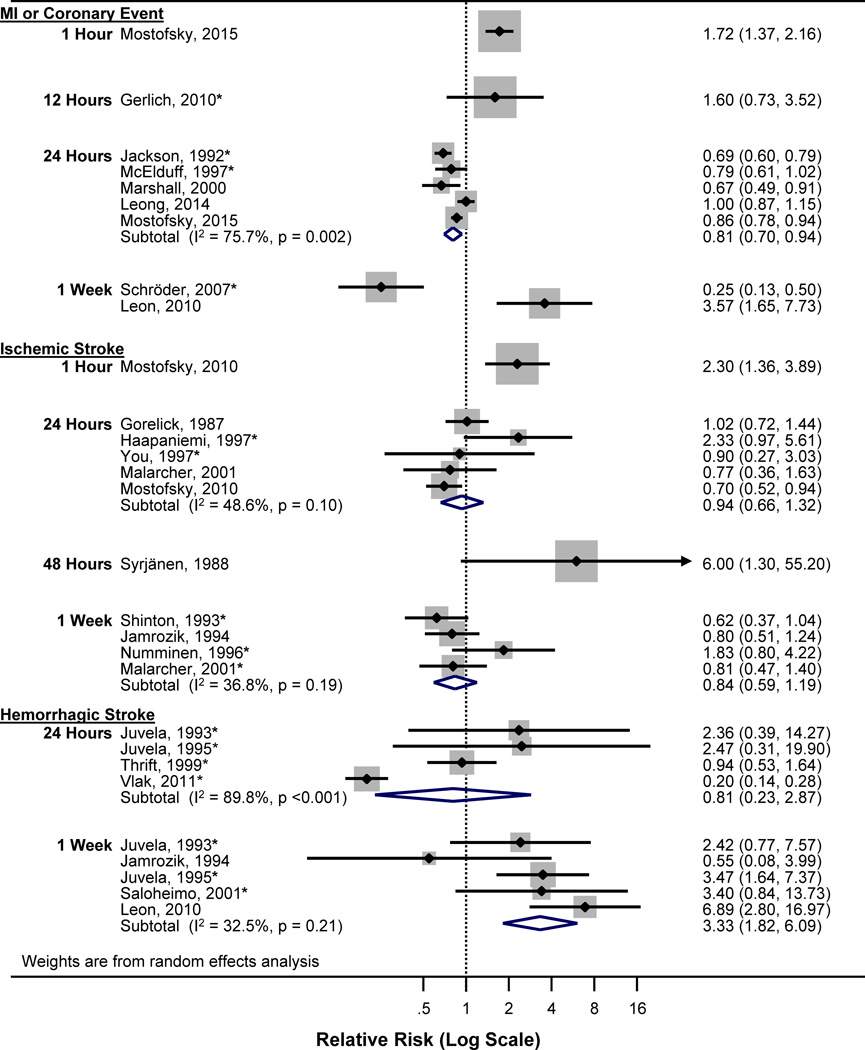
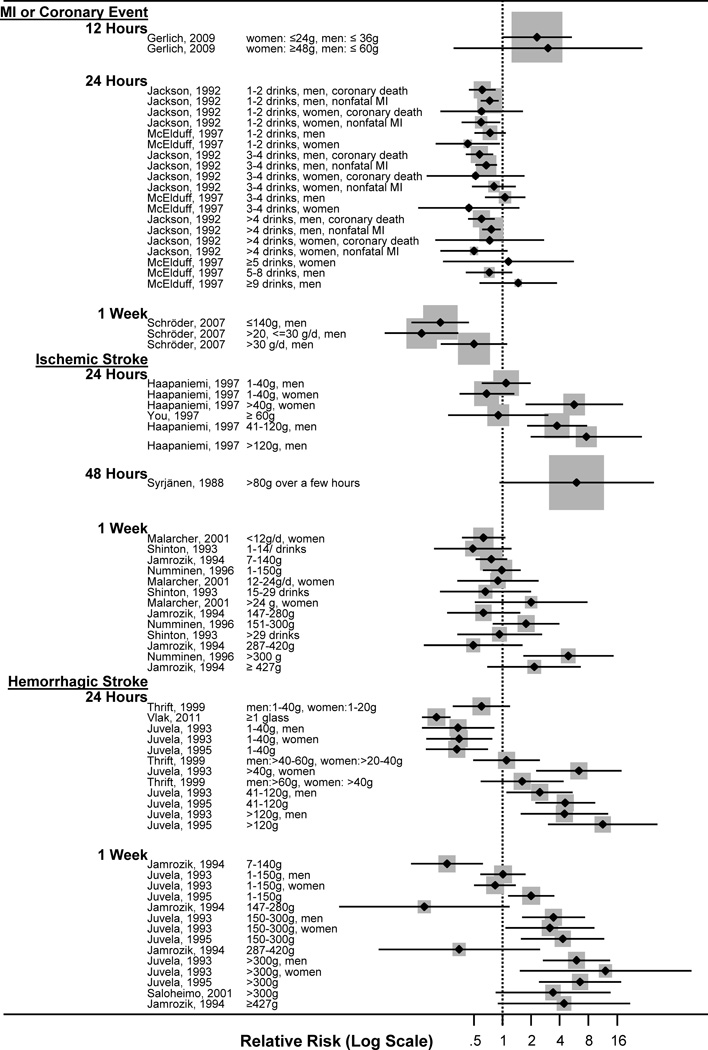
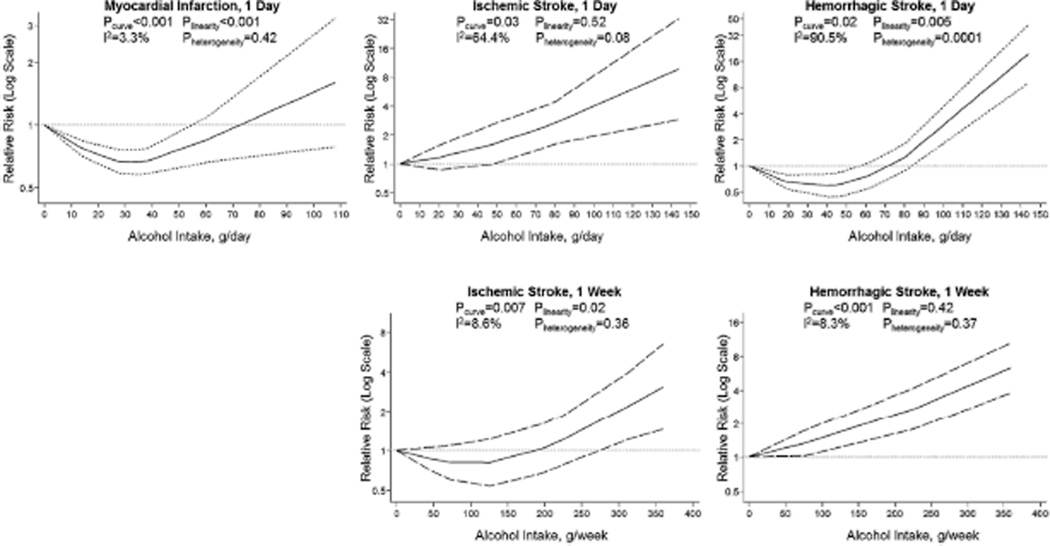
Figure 2 presents a forest plot of RRs and 95% CIs and heterogeneity statistics for analyses of any alcohol intake, Figure 3 presents a forest plot of dose-specific data with RRs and 95%CIs in Supplementary Figure 1, and Figure 4 presents splines, heterogeneity statistics and p-values for the dose-response analyses.
Figure 2.
Forest plot of relative risks (RRs) and 95% confidence intervals (CIs) for the association between any alcohol consumption relative to no drinking. Squares indicate study-specific RR estimates, with the size of the square reflecting the proportion of the DerSimonian and Laird weights under study; horizontal lines indicate the 95% CI; diamonds indicate the pooled RRs with their 95% CI from a random-effects model. The dotted line indicates the value for no association. *Also included in dose-response meta-analysis.
Figure 3.
Forest plot of relative risks (RRs) and 95% confidence intervals (CIs) for the association between alcohol consumption and cardiovascular events in the following day and week by amount of alcohol intake. Squares indicate study-specific RR estimates, with the size of the square reflecting the proportion of the DerSimonian and Laird weights under study; horizontal lines indicate the 95% CI. The dotted line indicates the value for no association.
Figure 4.
Relative risk (solid line) and 95% confidence interval (dashed lines) for the association between grams of alcohol and risk of cardiovascular events within 24 hours. Alcohol consumption was modelled with restricted cubic splines in a random-effects dose–response model. The lowest value of zero (non-drinkers) was used to estimate all relative risks. The vertical axis is on a log scale. The dotted line indicates the value for no association.
Myocardial Infarction
One study13 reported a higher risk of sudden cardiac death within 2 hours after alcohol consumption (RR=3.00, 95%CI 1.61–5.68), but we did not include this estimate in our analyses since the cause of death may have been due to cardiomyopathy or arrhythmias. Five case-crossover14–18 and four case-control studies19–22 evaluated the association between alcohol intake and the immediate risk of MI or major coronary event.20 There was a higher MI risk in the hour after alcohol intake compared to other times and a modestly lower risk after 24 hours. Two studies assessed MI risk within one week among men, with one21 reporting a lower MI risk (RR=0.25, 95%CI 0.13–0.50) after approximately 18 grams of alcohol in the past week and the other22 reporting higher risk of death from ischemic heart disease or MI after heavy alcohol intoxication for ≥2 days when the person is withdrawn from normal social life (RR=3.57, 95%CI 1.65–7.73).
When accounting for the amount of alcohol consumed in the 24 hours prior to MI onset, there was a U-shaped association (pcurve<0.001) between alcohol intake and MI risk, with the greatest benefit following approximately 28 grams of alcohol (≈2 drinks) in one day (RR=0.67) and a higher risk following approximately 108 grams (≈9 drinks) in one day (RR=1.59). Within a week following alcohol consumption, there was a lower risk of MI with moderate alcohol intake but a higher risk following heavy alcohol consumption.
There was no indication of small-study effects for studies of MI risk in the day (Egger's p=0.18) and week (Egger's p=0.86) following alcohol consumption. Results were similar in sensitivity analyses excluding one estimate at a time.
Ischemic Stroke
One case-crossover23 and eight case-control studies24–31 examined the association between alcohol intake and the immediate risk of IS. One study27 with RRs by level of alcohol intake could not be included in the dose-response meta-analysis because information on the sample size at each level of consumption was not reported. There was evidence of a higher IS risk within an hour of any alcohol intake, and a suggestion of protective benefits thereafter, though the results were inconsistent.
In the dose-response analysis, there was a higher IS risk with higher alcohol intake in the preceding day, though this linear association was only based on two studies with dose information. There was a U-shaped association (pcurve=0.007) for risk in the following week. Compared to no alcohol consumption, there was a 19% lower risk of IS in the week following approximately 75 grams of alcohol (≈6 drinks/week) but a 2.25-fold higher IS risk in the week following 225 grams (≈19 drinks) that continues to climb with higher amounts of alcohol consumption. The dose-response association was apparent for both men and for women. There was no indication of publication bias (Egger's p=0.39). In sensitivity analyses excluding one study at a time, the RR for IS within 1 day was lower (RR=0.82, 95%CI 0.66–1.01) when we removed one study’s results29 and higher (RR=1.08, 95%CI 0.74–1.60) when we removed the estimate from another study,18 but a similar sensitivity analysis had no impact on the RR for IS risk within a week.
In sensitivity analyses, we included estimates from case-control studies that did not account for confounders.24, 32, 33 The estimated risk in 24 hours was similar to the preliminary analysis. Five studies26, 32, 34–36 enrolled cases with either IS or HS but after restricting the analyses to studies that accounted for potential confounders and at least some exposed cases and controls, only one study26 with a combined endpoint was included- since the study was comprised of 81 cases of IS and only 9 cases of HS, the RR was included in the analysis of IS risk; results were similar when this estimate was excluded.
Hemorrhagic Stroke
One case-crossover37 and six case-control studies22, 27, 38–41 examined the immediate risk of HS following alcohol intake, with most studies reporting a higher risk within a day or a week after any consumption.
In the dose-response meta-analysis, there was a U-shaped association (pcurve=0.02) between alcohol consumption and HS risk after 24 hours. Compared to no intake, consumption of 48 grams (≈4 drinks) was associated with a 38% lower HS risk whereas drinking 81 grams (≈7 drinks) was associated with a 1.26-fold higher HS risk in the following day. This association was apparent for both men and women. There was a linear association for HS risk within a week of alcohol consumption, with no evidence of protective benefits.
There was no indication of publication bias for studies of HS risk in the day (Egger's p=0.25) and week (Egger's p=0.19) following any alcohol intake. Results were similar in sensitivity analyses excluding one estimate at a time.
Discussion
In this systematic review and meta-analysis, moderate alcohol consumption was associated with an immediately higher risk of cardiovascular events, but after 24 hours, there was a lower risk of MI and HS and after one week, there was a lower risk of IS, consistent with prior research showing cardiovascular benefits of habitual intake. Heavy alcohol drinking was associated with higher cardiovascular risk in the following hours and days.
Immediately following alcohol intake, there are both harmful and protective physiologic responses.7 Within 1–3 hours, a single dose of alcohol increases heart rate,3 interarterial electromechanical delay4 and plasminogen activator inhibitor levels,5 but by 12–24 hours, an alcohol dose consistent with two alcoholic beverages causes transient improvements in flow-mediated vasodilatation, endothelial function,7 and fibrinolytic factors.5
Within weeks of regular intake, there are improvements in inflammatory markers, lipid profile, and adipokines and insulin sensitivity.7 Habitual moderate alcohol consumption (1–2 drinks per day) is associated with improvements in HDL cholesterol, heart rate variability,42 endothelial function, insulin sensitivity, coagulation and fibrinolytic cascades7 and a lower risk of cardiovascular disease and IS and HS.43 However, heavy drinking (3–4 or more drinks per day) is associated with a higher risk of hypertension,6 diabetes, cardiovascular disease, IS and HS, and mortality after MI.43–45 Usual drinking habits may modify the acute physiologic response to alcohol. Therefore, the 2015 Dietary Guidelines Advisory Committee recommended that, If alcohol is consumed, it should be consumed in moderation—up to one drink per day for women and two drinks per day for men.46 The results of this meta-analysis show that there may also be an immediate risk of cardiovascular events even if moderate habitual consumption yields cardioprotective benefits.
Our dose-response analysis suggests that after 24 hours, moderate drinkers may experience a lower risk of a cardiovascular event compared to other times, whereas heavy drinking is associated with a higher risk even after 24 hours. This is supported by prior work showing that the health effects of alcohol intake depend on both the amount and the pattern of consumption. Heavy episodic drinking, defined as 4 or more alcoholic beverages within 1–2 hours, has harmful effects, even if individuals who binge only drink one or two days per week, resulting in the same average alcohol intake per week that is known to yield cardioprotective benefits. Among men, drinking a small amount of alcohol regularly (e.g., 1–2 drinks/day, 4 days/week) lowers cardiovascular risk more than drinking the same total weekly amount but on fewer days per week.1 Therefore, it is possible that over time, individuals who frequently drink small amounts of alcohol may experience a temporarily heightened risk, but this may be offset in part by the subsequent protective benefits in the hours after consumption, whereas consuming large amounts of alcohol at once may result in both a sharply higher immediate risk and repeated bouts cause a higher long-term risk. The results of studies examining a one-week risk period are unclear because most studies did not provide information on the pattern of drinking in the week prior to the event; it is possible that some people only drank early in the prior week, some only drank immediately before the event and some drank alcohol on several occasions in the prior week. However, one case-control study31 reported that among women who drank alcohol in the past week, those who drank in the past 24 hours had a lower risk of stroke than never drinkers, and the risk was even lower for women who did not drink in the past 24 hours. This supports our hypothesis that there may be protective benefits in the 24 hours after moderate alcohol intake, and perhaps the benefits are even greater in the following days.
The immediate impact of alcohol consumption may be influenced by usual alcohol intake. One study18 noted that the higher MI risk in the hour following alcohol consumption was not apparent for daily drinkers. This may be due to alcohol tolerance whereby habitual intake leads to up-regulation of enzymes that metabolize alcohol, resulting in a lower physiological response to each drink.47 Although case-crossover studies are restricted to current drinkers by design since only cases reporting alcohol in the past year contribute information, only two case-control studies10,11 conducted analyses restricted to current drinkers and six studies19, 20, 28, 29, 31, 39 adjusted for usual intake. In the remaining studies, some of the former drinkers may have stopped drinking alcohol because of illness, prior alcohol abuse or prescription medications that cannot be taken with alcohol which would overestimate the health benefits of alcohol intake.48 It is possible that some people abstained from alcohol in response to prodromal symptoms before clinical onset of the cardiovascular event, resulting in an underestimate of recent intake and a biased estimate. However, the results were similar in studies18, 23 that used symptom onset rather than hospital admission time to define event onset and when they conducted sensitivity analyses restricted to cases with no preclinical symptoms. In one study,49 the results were weaker but still evident after accounting for prodromal symptoms.
Habitual moderate alcohol consumption is associated with lower risk of heart disease in both sexes, but the amount of alcohol associated with cardiovascular benefits is lower among women than among men. Only some of the studies reported results separately for men and for women, so we could not statistically evaluate whether sex modifies the magnitude or timing of heightened acute risk, but higher cardiovascular risk following higher levels of alcohol intake was apparent for both men and women. There were no studies that examined whether the immediate risk following alcohol intake was modified by medical history, but in studies of habitual alcohol consumption, the benefits of moderate intake were similar for people with existing cardiovascular disease or diabetes and those in the general population.45
Prior studies have reported racial/ethnic differences in the magnitude of the association between habitual alcohol consumption and risk of cardiovascular events17, 50 which may involve ethnic variations in the prevalence of genetic polymorphisms related to alcohol metabolism,51 cultural differences in past drinking, current drinking patterns and associations between drinking patterns and other health risk factors and health problems.52 Future studies are needed to evaluate whether there is any racial/ethnic variation in the acute effects of alcohol intake on cardiovascular risk, and whether genetic differences may play a role.
Only five studies18, 23, 31, 37, 40 examined the association by drink type, so we could not evaluate whether the risk differs for wine, beer or liquor consumption. In case-crossover studies of alcohol types and the acute risk of MI18 and IS,23 there was a suggestion that the acutely elevated risk in the hour after alcohol consumption was stronger for liquor than for beer or wine, and the protective association by 24 hours was apparent for beer and wine but not for liquor. Other studies have reported that within 24 hours of intake, individuals drinking wine were protected from intracerebral hemorrhage (ICH) and there was also a lower risk of ICH for those who recently consumed liquor, but there was little association between either beer or fortified beverages and ICH,40 whereas another study reported similar risk of ICH by beverage type for the risk of ICH.37 However, none of the studies simultaneously evaluated beverage type and drinking patterns. Furthermore, previous studies have shown that all alcohol types have similar effects on high density lipoprotein cholesterol and other biological markers of cardiovascular risk. Therefore, differences in the magnitude of the association between different alcohol types and cardiovascular outcomes are more likely to result from differences in lifestyle and the frequency and amount of alcohol intake rather than from different physiologic effects of a specific beverage type.1, 7, 31
Some studies did not report enough details to be included in our dose–response meta-analysis, and none of the studies provided information on heavy episodic drinking, defined as four drinks for women and five drinks for men consumed within about two hours.53 However, our results suggest that moderate alcohol consumption is associated with an immediately higher risk of cardiovascular events that is attenuated by 24 hours whereas heavy alcohol drinking remains harmful.
We evaluated the influence of the timing and amount of alcohol on cardiovascular risk, but we could not address sources of bias in the original studies. However, although residual and unmeasured confounding cannot be ruled out, most of the case-control studies accounted for many confounders and the self-matching in case-crossover studies eliminates confounding by slowly varying characteristics. All of the included studies obtained information on alcohol intake after the cardiovascular event occurred, and alcohol intake may have been differentially misreported for cases and controls or in the case-crossover studies, for recent intake compared to usual intake. If recent alcohol intake impacted the cases’ ability or willingness to participate in the study, selection bias may have led to incorrect estimates, but many studies used proxy respondents when the case could not provide information. Finally, we did not identify any unpublished studies and we cannot exclude the possibility that publication bias may have affected our results, but we found no evidence of such bias. There was no evidence of small study effects but tests for funnel plot asymmetry are not recommended when there are fewer than ten studies. For some of the analyses, we observed between-study heterogeneity and the results were slightly but not meaningfully altered when removing a single study, though the magnitude of the change was also impacted by the amount of alcohol. Although it may be tempting to infer that the heterogeneity in the magnitude of the association between different cardiovascular events is due to different biological mechanisms linking alcohol and the outcome of interest, it may also be at least partially due to differences in the baseline risk and drinking patterns of the populations under study. Despite these limitations, this study is the first attempt to understand comprehensively the interplay between dose and timing of alcohol intake and the immediate risks and benefits on both MI and stroke.
In summary, our results suggest that alcohol intake is associated with an immediately higher risk of cardiovascular events, but after 24 hours, there is a lower risk of MI and HS and within one week, there is a lower risk of IS whereas heavy drinking continues to confer higher risk even after 24 hours.
Supplementary Material
Clinical Perspectives.
There is consistent evidence that habitual moderate consumption is associated with a lower risk of coronary heart disease whereas heavy alcohol consumption may be harmful. However, the acute risks following alcohol intake have not been well characterized. Based on its physiological effects, alcohol may have markedly different effects on immediate and long-term risk. Therefore, we conducted a systematic review and meta-analysis of observational studies that evaluated the association between alcohol intake and myocardial infarction, ischemic stroke, and hemorrhagic stroke in the following hours and days. Based on data from 23 full-text articles (29457 participants), moderate alcohol consumption was associated with an immediately higher cardiovascular risk that was attenuated after 24 hours, and even protective for myocardial infarction and hemorrhagic stroke, and protective against ischemic stroke within one week. In contrast, heavy alcohol drinking was associated with higher cardiovascular risk in the following day and week.
Acknowledgments
Funding Sources: Elizabeth Mostofsky received support from the a National Institutes of Health grant (L30-HL115623-02) and a KL2/Catalyst Medical Research Investigator Training award (an appointed KL2 award) from Harvard Catalyst/The Harvard Clinical and Translational Science Center (National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health Award KL2 TR001100). The content is solely the responsibility of the authors and does not necessarily represent the official views of the European Research Council, Harvard Catalyst, Harvard University and its affiliated academic healthcare centers, or the National Institutes of Health. Harpreet Chahal received support from by the Frederick Banting and Charles Best Canada Graduate Scholarship and the Michael Smith Foreign Study Supplement from the Canadian Institutes of Health Research. Role of the Funder/Sponsor: No funding organization had any role in the design and conduct of the study; collection; management, analysis and interpretation of the data; and preparation of the manuscript.
Footnotes
Disclosures: None.
References
- 1.Mukamal KJ, Conigrave KM, Mittleman MA, Camargo CA, Jr, Stampfer MJ, Willett WC, Rimm EB. Roles of drinking pattern and type of alcohol consumed in coronary heart disease in men. N Engl J Med. 2003;348:109–118. doi: 10.1056/NEJMoa022095. [DOI] [PubMed] [Google Scholar]
- 2.Whitfield JB, Heath AC, Madden PA, Pergadia ML, Montgomery GW, Martin NG. Metabolic and biochemical effects of low-to-moderate alcohol consumption. Alcohol Clin Exp Res. 2013;37:575–586. doi: 10.1111/acer.12015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Spaak J, Merlocco AC, Soleas GJ, Tomlinson G, Morris BL, Picton P, Notarius CF, Chan CT, Floras JS. Dose-related effects of red wine and alcohol on hemodynamics, sympathetic nerve activity, and arterial diameter. Am J Physiol Heart Circ Physiol. 2008;294:H605–H612. doi: 10.1152/ajpheart.01162.2007. [DOI] [PubMed] [Google Scholar]
- 4.Sengul C, Cevik C, Ozveren O, Sunbul A, Oduncu V, Akgun T, Can MM, Semiz E, Dindar I. Acute alcohol consumption is associated with increased interatrial electromechanical delay in healthy men. Cardiol J. 2011;18:682–686. doi: 10.5603/cj.2011.0033. [DOI] [PubMed] [Google Scholar]
- 5.Hendriks HF, Veenstra J, Velthuis-te Wierik EJ, Schaafsma G, Kluft C. Effect of moderate dose of alcohol with evening meal on fibrinolytic factors. BMJ. 1994;308:1003–1006. doi: 10.1136/bmj.308.6935.1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Briasoulis A, Agarwal V, Messerli FH. Alcohol consumption and the risk of hypertension in men and women: a systematic review and meta-analysis. J Clin Hypertens (Greenwich) 2012;14:792–798. doi: 10.1111/jch.12008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brien SE, Ronksley PE, Turner BJ, Mukamal KJ, Ghali WA. Effect of alcohol consumption on biological markers associated with risk of coronary heart disease: systematic review and meta-analysis of interventional studies. BMJ. 2011;342:d636. doi: 10.1136/bmj.d636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283:2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 9.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 10.Orsini N, Bellocco R, Greenland S. Generalized least squares for trend estimation of summarized dose-response data. Stata J. 2006;6:40–57. [Google Scholar]
- 11.Cochran W. The combination of estimates from different experiments. Biometrics. 1954;10:101–129. [Google Scholar]
- 12.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Šelb Šemerl J, Šelb K. Coffee and alcohol consumption as triggering factors for sudden cardiac death: case-crossover study. Croat Med J. 2004;45:775–780. [PubMed] [Google Scholar]
- 14.Marshall RJ, Wouters S, Jackson RT. A case-crossover analysis of a case-control study of alcohol consumption and coronary events: the effects of exposure definition and the use of control data. J Epidemiol Biostat. 2000;5:367–373. [PubMed] [Google Scholar]
- 15.Gerlich MG, Kramer A, Gmel G, Maggiorini M, Luscher TF, Rickli H, Kleger GR, Rehm J. Patterns of alcohol consumption and acute myocardial infarction: a case-crossover analysis. Eur Addict Res. 2009;15:143–149. doi: 10.1159/000213641. [DOI] [PubMed] [Google Scholar]
- 16.Gerlich MG, Rehm J. Recall bias in case-crossover designs studying the potential influence of alcohol consumption. J Stud Alcohol Drugs. 2010;71:619. doi: 10.15288/jsad.2010.71.619. author reply 620–1. [DOI] [PubMed] [Google Scholar]
- 17.Leong DP, Smyth A, Teo KK, McKee M, Rangarajan S, Pais P, Liu L, Anand SS, Yusuf S. Patterns of Alcohol Consumption and Myocardial Infarction Risk: Observations From 52 Countries in the INTERHEART Case-Control Study. Circulation. 2014;130:390–398. doi: 10.1161/CIRCULATIONAHA.113.007627. [DOI] [PubMed] [Google Scholar]
- 18.Mostofsky E, van der Bom JG, Mukamal KJ, Maclure M, Tofler GH, Muller JE, Mittleman MA. Risk of myocardial infarction immediately after alcohol consumption. Epidemiology. 2015;26:143–150. doi: 10.1097/EDE.0000000000000227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jackson R, Scragg R, Beaglehole R. Does recent alcohol consumption reduce the risk of acute myocardial infarction and coronary death in regular drinkers? Am J Epidemiol. 1992;136:819–824. doi: 10.1093/aje/136.7.819. [DOI] [PubMed] [Google Scholar]
- 20.McElduff P, Dobson AJ. How much alcohol and how often? Population based case-control study of alcohol consumption and risk of a major coronary event. BMJ. 1997;314:1159–1164. doi: 10.1136/bmj.314.7088.1159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schroder H, Masabeu A, Marti MJ, Cols M, Lisbona JM, Romagosa C, Carion T, Vilert E, Marrugat J. Myocardial infarction and alcohol consumption: a population-based case-control study. Nutr Metab Cardiovasc Dis. 2007;17:609–615. doi: 10.1016/j.numecd.2006.04.010. [DOI] [PubMed] [Google Scholar]
- 22.Leon DA, Shkolnikov VM, McKee M, Kiryanov N, Andreev E. Alcohol increases circulatory disease mortality in Russia: acute and chronic effects or misattribution of cause? Int J Epidemiol. 2010;39:1279–1290. doi: 10.1093/ije/dyq102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mostofsky E, Burger MR, Schlaug G, Mukamal KJ, Rosamond WD, Mittleman MA. Alcohol and acute ischemic stroke onset: the stroke onset study. Stroke. 2010;41:1845–1849. doi: 10.1161/STROKEAHA.110.580092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gorelick PB, Rodin MB, Langenberg P, Hier DB, Costigan J, Gomez I, Spontak S. Is acute alcohol ingestion a risk factor for ischemic stroke? Results of a controlled study in middle-aged and elderly stroke patients at three urban medical centers. Stroke. 1987;18:359–364. doi: 10.1161/01.str.18.2.359. [DOI] [PubMed] [Google Scholar]
- 25.Syrjanen J, Valtonen VV, Iivanainen M, Kaste M, Huttunen JK. Preceding infection as an important risk factor for ischaemic brain infarction in young and middle aged patients. Br Med J (Clin Res Ed) 1988;296:1156–1160. doi: 10.1136/bmj.296.6630.1156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shinton R, Sagar G, Beevers G. The relation of alcohol consumption to cardiovascular risk factors and stroke. The west Birmingham stroke project. J Neurol Neurosurg Psychiatry. 1993;56:458–462. doi: 10.1136/jnnp.56.5.458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jamrozik K, Broadhurst RJ, Anderson CS, Stewart-Wynne EG. The role of lifestyle factors in the etiology of stroke. A population-based case-control study in Perth, Western Australia. Stroke. 1994;25:51–59. doi: 10.1161/01.str.25.1.51. [DOI] [PubMed] [Google Scholar]
- 28.Numminen H, Hillbom M, Juvela S. Platelets, alcohol consumption, and onset of brain infarction. J Neurol Neurosurg Psychiatry. 1996;61:376–380. doi: 10.1136/jnnp.61.4.376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Haapaniemi H, Hillbom M, Juvela S. Lifestyle-associated risk factors for acute brain infarction among persons of working age. Stroke. 1997;28:26–30. doi: 10.1161/01.str.28.1.26. [DOI] [PubMed] [Google Scholar]
- 30.You RX, McNeil JJ, O'Malley HM, Davis SM, Thrift AG, Donnan GA. Risk factors for stroke due to cerebral infarction in young adults. Stroke. 1997;28:1913–1918. doi: 10.1161/01.str.28.10.1913. [DOI] [PubMed] [Google Scholar]
- 31.Malarcher AM, Giles WH, Croft JB, Wozniak MA, Wityk RJ, Stolley PD, Stern BJ, Sloan MA, Sherwin R, Price TR, Macko RF, Johnson CJ, Earley CJ, Buchholz DW, Kittner SJ. Alcohol intake, type of beverage, and the risk of cerebral infarction in young women. Stroke. 2001;32:77–83. doi: 10.1161/01.str.32.1.77. [DOI] [PubMed] [Google Scholar]
- 32.Taylor JR, Combs-Orme T. Alcohol and strokes in young adults. Am J Psychiatry. 1985;142:116–118. doi: 10.1176/ajp.142.1.116. [DOI] [PubMed] [Google Scholar]
- 33.Bråthen G, Brodtkorb E, Sand T, Helde G, Bovim G. Weekday distribution of alcohol consumption in Norway: influence on the occurrence of epileptic seizures and stroke? Eur J Neurol. 2000;7:413–421. doi: 10.1046/j.1468-1331.2000.00097.x. [DOI] [PubMed] [Google Scholar]
- 34.Taylor JR. Alcohol and strokes. N Engl J Med. 1982;306:1111. doi: 10.1056/NEJM198205063061816. [DOI] [PubMed] [Google Scholar]
- 35.Taylor JR, Combs-Orme T, Anderson D, Taylor DA, Koppenol C. Alcohol, hypertension, and stroke. Alcohol Clin Exp Res. 1984;8:283–286. doi: 10.1111/j.1530-0277.1984.tb05512.x. [DOI] [PubMed] [Google Scholar]
- 36.Gill JS, Zezulka AV, Shipley MJ, Gill SK, Beevers DG. Stroke and alcohol consumption. N Engl J Med. 1986;315:1041–1046. doi: 10.1056/NEJM198610233151701. [DOI] [PubMed] [Google Scholar]
- 37.Vlak MH, Rinkel GJ, Greebe P, van der Bom JG, Algra A. Trigger factors and their attributable risk for rupture of intracranial aneurysms: a case-crossover study. Stroke. 2011;42:1878–1882. doi: 10.1161/STROKEAHA.110.606558. [DOI] [PubMed] [Google Scholar]
- 38.Juvela S, Hillbom M, Numminen H, Koskinen P. Cigarette smoking and alcohol consumption as risk factors for aneurysmal subarachnoid hemorrhage. Stroke. 1993;24:639–646. doi: 10.1161/01.str.24.5.639. [DOI] [PubMed] [Google Scholar]
- 39.Juvela S, Hillbom M, Palomaki H. Risk factors for spontaneous intracerebral hemorrhage. Stroke. 1995;26:1558–1564. doi: 10.1161/01.str.26.9.1558. [DOI] [PubMed] [Google Scholar]
- 40.Thrift AG, Donnan GA, McNeil JJ. Heavy drinking, but not moderate or intermediate drinking, increases the risk of intracerebral hemorrhage. Epidemiology. 1999;10:307–312. [PubMed] [Google Scholar]
- 41.Saloheimo P, Juvela S, Hillbom M. Use of aspirin, epistaxis, and untreated hypertension as risk factors for primary intracerebral hemorrhage in middle-aged and elderly people. Stroke. 2001;32:399–404. doi: 10.1161/01.str.32.2.399. [DOI] [PubMed] [Google Scholar]
- 42.Janszky I, Ericson M, Blom M, Georgiades A, Magnusson JO, Alinagizadeh H, Ahnve S. Wine drinking is associated with increased heart rate variability in women with coronary heart disease. Heart. 2005;91:314–318. doi: 10.1136/hrt.2004.035105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ronksley PE, Brien SE, Turner BJ, Mukamal KJ, Ghali WA. Association of alcohol consumption with selected cardiovascular disease outcomes: a systematic review and meta-analysis. BMJ. 2011;342:d671. doi: 10.1136/bmj.d671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pai JK, Mukamal KJ, Rimm EB. Long-term alcohol consumption in relation to all-cause and cardiovascular mortality among survivors of myocardial infarction: the Health Professionals Follow-up Study. Eur Heart J. 2012;33:1598–1605. doi: 10.1093/eurheartj/ehs047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Breslow RA, Mukamal KJ. Measuring the burden--current and future research trends: results from the NIAAA Expert Panel on Alcohol and Chronic Disease Epidemiology. Alcohol Res. 2013;35:250–259. [PMC free article] [PubMed] [Google Scholar]
- 46.United States Dietary Guidelines Advisory Committee. Scientific Report of the Dietary Guidelines Advisory Committee on the dietary guidelines for Americans to the Secretary of Agriculture and the Secretary of Health and Human Services. 2015 http://permanent.access.gpo.gov/gpo51700/2015/Scientific-Report-of-the-2015-Dietary-Guidelines-Advisory-Committee.pdf.
- 47.Tabakoff B, Cornell N, Hoffman PL. Alcohol tolerance. Ann Emerg Med. 1986;15:1005–1012. doi: 10.1016/s0196-0644(86)80119-6. [DOI] [PubMed] [Google Scholar]
- 48.Shaper AG, Wannamethee G, Walker M. Alcohol and mortality in British men: explaining the U-shaped curve. Lancet. 1988;2:1267–1273. doi: 10.1016/s0140-6736(88)92890-5. [DOI] [PubMed] [Google Scholar]
- 49.Wouters S, Marshall R, Yee RL, Jackson R. Is the apparent cardioprotective effect of recent alcohol consumption due to confounding by prodromal symptoms? Am J Epidemiol. 2000;151:1189–1193. doi: 10.1093/oxfordjournals.aje.a010169. [DOI] [PubMed] [Google Scholar]
- 50.Mukamal KJ, Chen CM, Rao SR, Breslow RA. Alcohol consumption and cardiovascular mortality among U.S. adults, 1987 to 2002. J Am Coll Cardiol. 2010;55:1328–1335. doi: 10.1016/j.jacc.2009.10.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Han H, Wang H, Yin Z, Jiang H, Fang M, Han J. Association of genetic polymorphisms in ADH and ALDH2 with risk of coronary artery disease and myocardial infarction: a meta-analysis. Gene. 2013;526:134–141. doi: 10.1016/j.gene.2013.05.002. [DOI] [PubMed] [Google Scholar]
- 52.Kerr WC, Greenfield TK, Bond J, Ye Y, Rehm J. Racial and ethnic differences in all-cause mortality risk according to alcohol consumption patterns in the national alcohol surveys. Am J Epidemiol. 2011;174:769–778. doi: 10.1093/aje/kwr147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wechsler H, Dowdall GW, Davenport A, Rimm EB. A gender-specific measure of binge drinking among college students. Am J Public Health. 1995;85:982–985. doi: 10.2105/ajph.85.7.982. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.