Abstract
Heart failure (HF) is a growing healthcare burden and one of the leading causes of hospitalizations and readmission. Preventing readmissions for HF patients is an increasing priority for clinicians, researchers, and various stakeholders. The following review will discuss the interventions found to reduce readmissions for patients and improve hospital performance on the 30-day readmission process measure. While evidence-based therapies for HF management have proliferated, the consistent implementation of these therapies and development of new strategies to more effectively prevent readmissions remain areas for continued improvement.
Keywords: Heart failure, Readmission, Prevention, Process measures
Approximately 5.7 million American adults are living with heart failure (HF) and the projections are that the prevalence of HF will increase 46% from 2012 to 2030 with greater than 8 million adults living with the chronic condition. HF is one of the leading primary diagnoses for hospitalization with an estimated 1 million patients discharged in 2010. The total cost of HF for 2012 was $30.7 billion. According to Medicare, from 2009 to 2012 the median risk-standardized 30 day readmission rate for HF was 23.0%.1 Readmissions receive particular attention from researchers and policy makers as they are perceived as a correctable source of poor quality of care and excessive medical spending. The Affordable Care Act instituted a financial penalty for excessive readmissions for hospitals that is capped at 3% of a hospital’s total Medicare payments for 2015 and beyond. Previously Medicare’s diagnosis-related group payment system lacked a financial disincentive to reduce readmissions.2 The Centers for Medicare and Medicaid Services’ (CMS) Hospital Readmission Reduction Program currently only assesses risk-adjusted 30-day readmission rates for HF, acute myocardial infractions, pneumonia, chronic obstructive pulmonary disease, and elective total knee and hip arthroplasty.3
While 30-day HF readmission rates are an increasing focus of quality improvement, inpatient interventions for effectively preventing or reducing readmissions are not agreed upon. Furthermore, the 30-day period for readmissions is likely an arbitrary period of observation and a multitude of factors external to the quality of inpatient care influence readmission risk. Nevertheless, the goal for health systems should be to reduce all avoidable admissions whether index hospitalization or repeat admission. The following review article will highlight research on the strategies to prevent HF readmissions.
The burden of heart failure hospitalizations
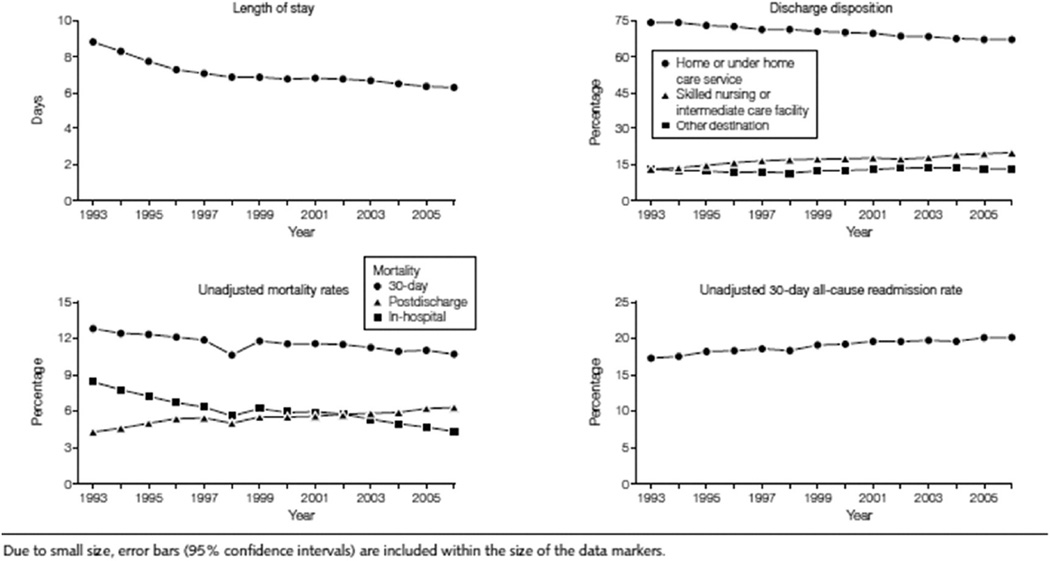
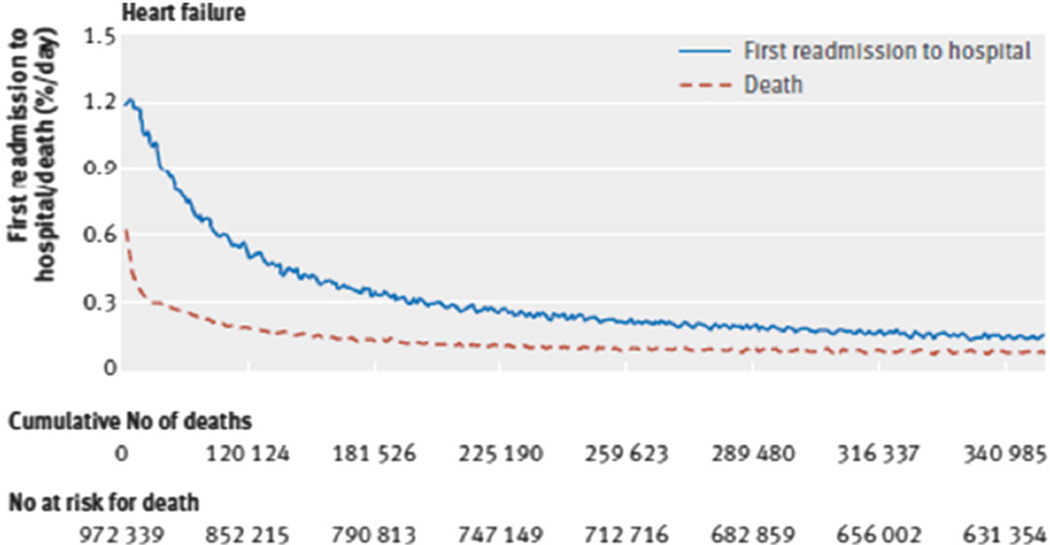
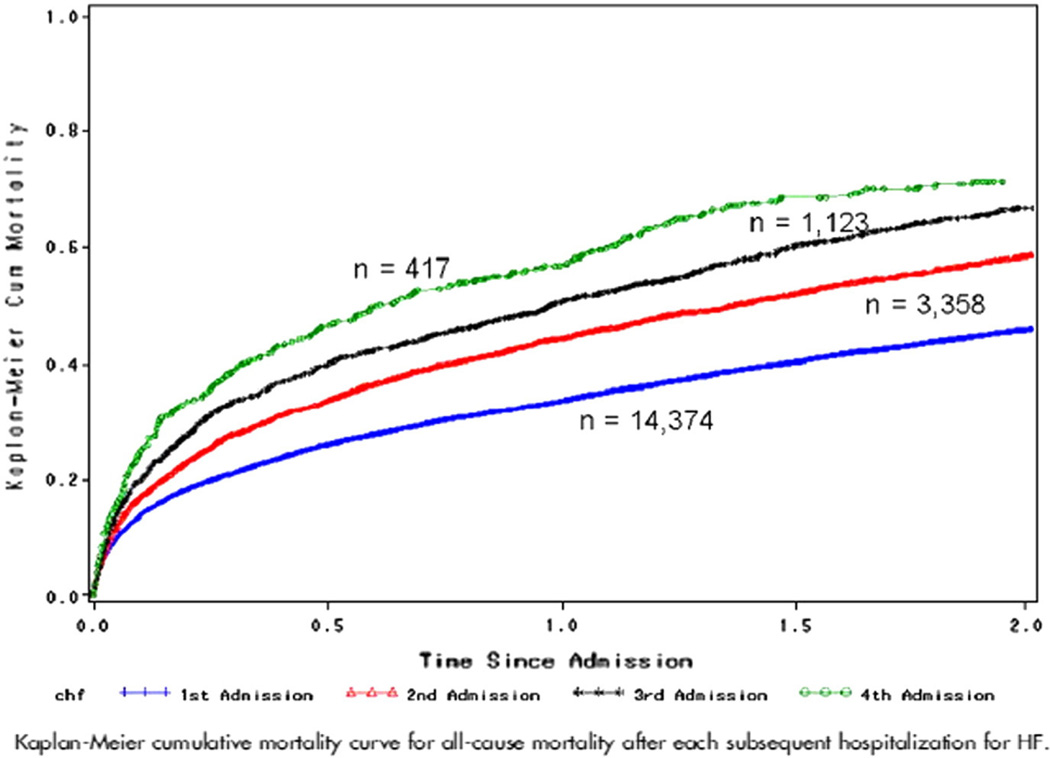
HF management has evolved considerably over recent decades with improvements in medical therapies and interventions that enable living with the condition for longer. Recent trends observe a reduction in length of stay as well as in-hospital and 30-daymortality, whereas 30-day readmission rates and discharges to skilled nursing facilities have increased (Fig 1).4 Among Medicare patients hospitalized for HF from 2008 to 2010, 67.4% experienced a readmission and 35.8% died within one year of the index hospitalization. The daily risk of readmission was highest on day 3 after discharge. Not until 38 days after hospitalization did the daily readmission risk decrease by 50% (Fig 2).5 Although the risk for readmission declines over time, patients with an index HF hospitalization have a significantly elevated risk of readmission for at least one year. An index HF admission is a significant marker of morbidity and mortality that extends beyond 30 days that should indicate to both inpatient and outpatient medical providers the severity of illness and importance of close evaluation and management (Fig 3).
Fig 1.
Secular trends for length of stay, discharge disposition, and unadjusted mortality and 30-day all-cause readmission rates in Medicare fee-for-service patients hospitalized for heart failure between 1993 and 2006.4
Fig 2.
Risks (hazard ratios) of first readmission to hospital and death for one year after hospitalization for heart failure (Medicare 2008–2010).5
Fig 3.
Kaplan–Meier cumulative mortality curve for all-cause mortality after each subsequent hospitalization for HF.53
The primary mechanism of acute HF decompensation is congestion and typically not a decrease in cardiac output. Subclinical congestion may precede clinical congestion by days to weeks.6 However, only 17%–35% of readmissions are attributed to a HF re-exacerbation and 53%–62% of readmissions are secondary to non-cardiovascular causes. Among readmitted Medicare patients with HF, the five most common primary diagnoses — HF, renal disorders, pneumonia, arrhythmias, and sepsis—account for 56% of the readmissions with no other diagnoses accounting for more than 5%.7,8 The diversity of readmission triggers highlights the importance of comprehensive care to prevent complications from secondary conditions and patient specific risk factors. Furthermore, the degree to which readmissions are avoidable is unclear. A meta-analysis of the literature estimates that only 23.1% of hospital 30-day readmissions may be avoidable. The estimates from the 16 primary studies included in the meta-analysis ranged from 5% to 79% for the proportion of readmissions deemed avoidable.9 The assessment of “avoidability” is not a standardized measure and researchers employ differing criteria mostly through chart review that may over or underestimate true rates. Nevertheless, the current evidence suggests only a quarter of 30-day readmissions may be preventable.
Risk models and variations in hospital performance
Predicting readmissions is important to both identify patients at-risk for readmissions, as well as risk adjust hospitals for comparison. A systematic review of 30 studies and 26 models unfortunately found that prediction models generally had poor discrimination with c-statistics ranging from 0.55 to 0.65 for models using administrative data alone, while other models used smaller populations that require further validation.10 Residual congestion at discharge has been noted in approximately 10%–15% of patients enrolled in randomized control trials and is associated with an increased risk for rehospitalization and mortality.11,12 Poor performance on the Mini-Cog exam was recently found to be both prevalent in a quarter of HF patients and doubled the risk of death or readmission during a mean follow-up of 6 months.13 Evaluation of health literacy, functional and cognitive status along with traditional markers of HF severity would strengthen models, but further validation is required.
CMS risk-adjusted hospital HF readmission rates vary considerably ranging from 17.0% to 28.2% with a median of 21.9% in the most recent CMS report. From 2010 to 2013, CMS observed a 1.5% decrease in the median readmission rate.14 Studies have revealed hospital characteristics outside of the current CMS risk-adjustment model that are associated with higher and lower readmission rates. One study found that hospitals with lower HF admission rates have higher rates of HF emergency department visits and subsequent increased risk for hospitalization after emergency department visits.15 A few studies have noted differences in HF care based on the overall hospital volume of admissions. Hospitals with a higher volume of HF admissions had better mortality and lower readmission rates suggesting better quality of care.16 While another study found that the all-cause hospital admission rate was associated with a greater risk for HF readmission. The analysis estimated that the hospital referral region explained 16% of the variation in readmissions compared to 2.6% for case mix (adjustments included age, sex, self-reported ethnicity, and Elixhauser comorbidities).17 These findings suggest that hospital case mix adjustments inadequately account for the healthcare needs of regional populations and that perhaps access to quality ambulatory care before and after hospital admission may better alleviate readmission risks.
Hospitals in resource-poor communities secondary to financial and clinical restraints have higher 30-day readmission rates. Having more exhaustive cardiac services and higher nurse staffing ratios are associated with lower readmission rates after controlling for other hospital factors.18 Furthermore, adding socioeconomic status removes to two to three times the expected hospital readmission variation and may make readmission models more useful.19,20 Hospitals in lower socioeconomic regions are disadvantaged by the current 30-day readmission performance measures and the CMS adjustments do not account for this bias.
Optimizing medical therapy to improve outcomes and reduce hospitalizations
Despite the challenges in identifying factors that predict readmission, a strong foundation exists for the use of evidence-based medical therapies to improve outcomes and reduce the hospitalization burden for HF patients.21 Therapies that reduce hospitalizations should be expected to reduce readmissions as well. Increasingly, hospitalization and readmissions are reported as primary or secondary outcomes of randomized clinical trials. One of the earliest trials from the Digitalis Investigators Group found a 6% absolute risk reduction in hospitalization for digoxin over an average follow-up of 37 months.22 Although the beta-blockers were not approved for HF at the time, more recent observational data suggest that digoxin may still be effective in reducing readmissions.23
As one of the cornerstones of HF therapy for patients with reduced ejection fraction, evidence-based beta-blockers are effective in reducing both mortality and readmissions.24,25 Of the performance measures recommended by the American College of Cardiology and the American Heart Association, only beta-blockers and angiotensin-converting enzyme (ACE) inhibitor or angiotensin receptor blocker (ARB) were significantly associated with reductions in mortality and readmissions.26 The novel developmental drug LCZ696 which combines an ARB with a neutral endopeptidase decreased both all-cause mortality and hospitalization when compared to an ACE inhibitor among HF patients with significant benefits observed within 30 days of randomization and market approval is pending.27
Aldosterone inhibitors such as spironolactone and eplerenone have both been shown in randomized clinical trials to reduce death and hospitalizations, with benefits seen within 30 days of initiation of therapy.28,29 Recent observational data from discharge confirm that the addition of an aldosterone inhibitor reduces HF readmissions.30 With regard to diuretic therapy, torsemide has higher bioavailability with less variability when compared to furosemide. Small trials suggest that inpatients discharged on torsemide have a lower risk for readmission in comparison to furosemide.31
Device therapies such as implantable cardioverter defibrillators (ICD) are indicated for the prevention of sudden cardiac death. Cardiac resynchronization therapy (CRT) reduces symptoms and improves left ventricular function and cardiac dyssynchrony. In the Cardiac Resynchronization – Heart Failure trial, patients with New York Heart Association (NYHA) class III or IV HF and systolic dysfunction had a 15% absolute risk reduction in HF readmissions at a mean follow-up of 29.4 months.32 When compared to ICD therapy alone, CRT therapy is associated with a lower risk of death and all-cause readmission.33
The potential for new technologies to monitor congestion and prevent readmissions is a developing field. A large randomized trial of telemonitoring for recently hospitalized HF patients utilized daily, toll-free calls to an automated system assessing general health and HF symptoms. Deviations in symptoms triggered flags for medical providers. The telephone based monitoring program did not improve outcomes or reduce readmissions.34 Impedance monitoring is a commonly included feature on many ICD and CRT devices. A randomized trial that provided impedance monitoring data to physicians and audible alerts to patients resulted in higher admission rates.35 The increased monitoring led to excessive admissions despite encouraging medical providers to evaluate symptoms and make treatment adjustments where appropriate. The Food and Drug Administration recently approved the CardioMEMS device (St. Jude Medical, Inc., St. Paul, MN), an implantable pulmonary artery sensor that wirelessly transmits pulmonary artery pressure measurements. The device was found to reduce HF hospitalizations by 37% at mean 15 months among patients previously hospitalized for HF compared to standard care, and a post hoc analysis of patients aged 65 years or older suggested a 58% reduction in 30-day readmissions with the pulmonary artery monitoring system.36 Both the fidelity of data and response to information determine the success of home monitoring technologies.
Health system strategies to reduce readmissions
Identifying health system strategies proven to reduce preventable hospitalization would be valuable to patients, medical providers, and healthcare administrators. A systemic review of interventions (such as patient education, discharge planning, medication reconciliation, scheduling follow-up before discharge, communication with outpatient providers, and follow-up telephone calls) implemented to reduce readmissions found that no single intervention alone was associated with lower 30-day readmission risk. Generally, more comprehensive interventions reported greater success.37 A survey of hospital practices and their association with lower 30-day HF readmission rates found certain strategies such as partnering with community physicians and health systems reduced readmission rates, while other strategies such as informing outpatient providers of discharge or providing a treatment plan to families increased the risk for readmission.38 Overall, this type of observational data makes determining the causative effects of strategies difficult and further research is warranted.
Nevertheless, there are indications that the quality of inpatient care is lacking and that transitions in care from inpatient to outpatient should be improved. The majority of patients at discharge are unaware of the changes made to their medications and nearly a quarter of medication changes are suspected provider errors secondary to inadequate medication reconciliation.39 Higher quality discharge summaries and timely transmission are associated with a lower risk of readmission for HF patients.40 Reducing medical errors and improving communication during transitions in care require continued attention.
Inpatient interventions peri-discharge have been shown to improve clinical outcomes and reduce HF readmissions. An early trial of a nurse-directed multidisciplinary intervention providing comprehensive education to the patient and family, medication review, and intensive follow-up reduced readmissions by 56.2% and also improved quality of life scores.41 Another small randomized trial found formal education and support using nurse teaching soon after discharge and intermittent monitoring for one year had a 39% relative risk reduction for readmissions.42 Similarly, an intervention targeting outpatient and inpatient HF patient in minority communities featuring bilingual nurses to counsel patients on diet, medication adherence, and self-management of symptoms at an initial visit and regularly scheduled follow-up phone calls found a 16.2% relative risk reduction of hospitalizations at one year.43 A meta-analysis of interventions for older HF patients found that comprehensive discharge planning with post-discharge support reduces HF readmissions and improved outcomes without increasing costs.44 Publication bias remains a concern especially for smaller studies using peri-discharge interventions. Overall, more support and careful outpatient monitoring have shown readmissions may be prevented.
Other hospital characteristics have been associated with lower readmission risks. Hospitals with higher nurse staffing ratios have a 41% lower odds of receiving Medicare penalties for excessive readmissions while controlling for case-mix and hospital characteritiscs.45 Hospitals with a greater proportion of patients receiving follow-up care within 7 days of discharge have a lower risk of 30-daymortality and readmission controlling for patient and hospital factors.46
Perspective on HF readmission reduction efforts
Increasing efforts have been focused on reducing 30-day readmissions as they are perceived as a modifiable event after hospitalization, risk standardized readmission rates are publicly reported, and hospitals face substantial financial penalties from CMS. Prediction models to date are poor at risk stratifying patients as well as explaining variation in performance between hospitals. Nevertheless, HF management has evolved to provide a number of medical and device treatments that improve outcomes and reduce hospitalizations. Although 30-day readmission rates for HF, acute myocardial infarctions, and pneumonia are a quality and performance metrics with financial implications to health systems, they do not correlate with mortality.47 Whether the 30-day HF readmission is an appropriate marker of inpatient care is debatable.
Researchers and critics have argued that the 30-day readmission measure does not adjust for medical complexity, disability, and socioeconomic status. Hospitals in lower socioeconomic areas are disadvantaged and are at increased risk for Medicare penalities.48–50 An estimated 58% of the national variation in hospital readmission rates may be explained by the county socioeconomic factors.51 Financially penalizing hospitals most at need is a perverse disincentive that may exacerbate the ability of health systems to improve the quality of care delivered.
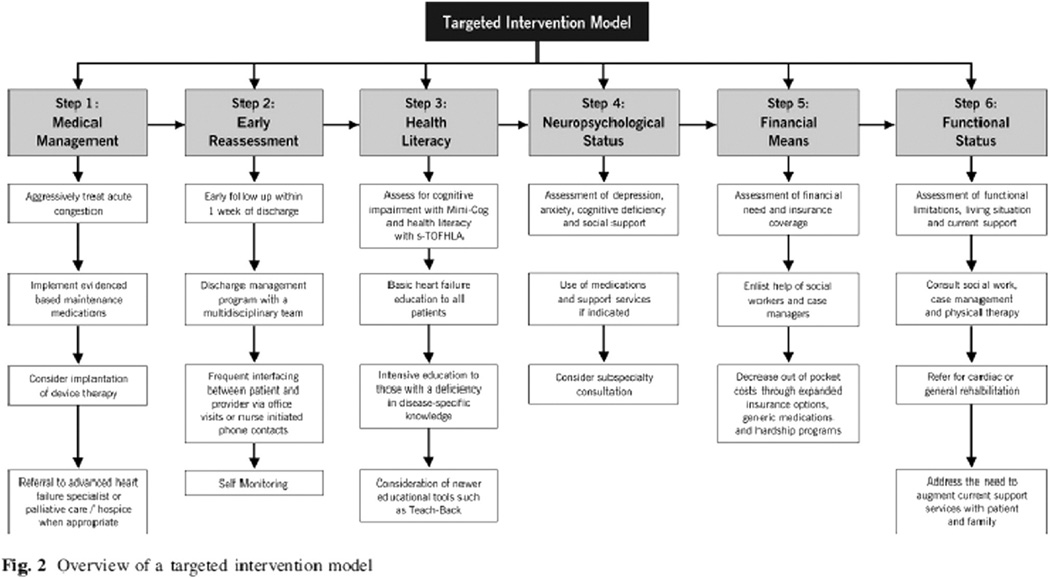
Most HF patients are readmitted for non-cardiovascular conditions. The importance of a complete medical evaluation should be emphasized as HF is one of many comorbidities that may increase the risk of future hospitalizations. A targeted intervention model described by Sperry et al. outlines the domains that should be considered during each HF hospitalization with guidance toward interventions to ameliorate risks (Fig 4).52 A HF hospitalization should not only assess the acute medical issues but also evaluate the outpatient challenges HF patients face.
Fig 4.
Targeted intervention model.52
Conclusions
A number of medical therapies are known to improve outcomes and reduce the risk of readmissions for HF patients. These therapies are often underutilized in appropriate selected patients. Strategies that provide increased support at discharge, improved communication, and early and close outpatient follow-up are associated with lower readmission risk. For select HF patients, enhanced monitoring with a wireless pulmonary artery monitoring system has proved effective and is now clinically available. Whether the 30-day readmission rate is an appropriate quality metric for inpatient care is debatable and the evidence suggests that external factors such as a patient and community socioeconomic status contribute significantly to the observed variations in the performance metric. Health system strategies to improve patient outcomes and reduce the hospitalization burden for HF require further research.
Acknowledgments
B. Ziaeian is supported by the NIH Cardiovascular Scientist Training Program (T32 HL007895).
Gregg C. Fonarow: Research: NIH, AHRQ; Consulting: Amgen, Bayer, Baxter, Janssen, Medtronic, Novartis.
Abbreviations and Acronyms
- ACE
angiotensin-converting enzyme
- ARB
angiotensin receptor blocker
- CMS
Centers for Medicare and Medicaid Services
- CRT
cardiac resynchronization therapy
- HF
heart failure
- ICD
implantable cardioverter defibrillator
- NYHA
New York Heart Association
Footnotes
Statement of conflict of interest
Boback Ziaeian: None.
REFERENCES
- 1.Go AS, et al. Heart disease and stroke statistics—2015 update: a report from the American Heart Association. Circulation. 2014;129:29–323. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 2.Berenson RA, Paulus RA, Kalman NS. Medicare’s readmissions-reduction program—a positive alternative. N Engl J Med. 2012;366:1364–1366. doi: 10.1056/NEJMp1201268. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Medicare & Medicaid Services. Readmissions Reduction Program. at, http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program.html2015.
- 4.Bueno H, et al. Trends in length of stay and short-term outcomes among Medicare patients hospitalized for heart failure, 1993–2006. JAMA. 2010;303:2141–2147. doi: 10.1001/jama.2010.748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dharmarajan K, et al. Trajectories of risk after hospitalization for heart failure, acute myocardial infarction, or pneumonia: retrospective cohort study. BMJ. 2015;350:h411–h411. doi: 10.1136/bmj.h411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gheorghiade M, Vaduganathan M, Fonarow GC, Bonow RO. Rehospitalization for heart failure: problems and perspectives. J AmColl Cardiol. 2013;61:391–403. doi: 10.1016/j.jacc.2012.09.038. [DOI] [PubMed] [Google Scholar]
- 7.Dunlay SM, et al. Hospitalizations after heart failure diagnosis. a community perspective. J Am Coll Cardiol. 2009;54:1695–1702. doi: 10.1016/j.jacc.2009.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dharmarajan K, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013 doi: 10.1001/jama.2012.216476. http://dx.doi.org/10.1001/jama.2012.216476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Van Walraven C, Jennings A, Forster AJ. A meta-analysis of hospital 30-day avoidable readmission rates. J Eval Clin Pract. 2012;18:1211–1218. doi: 10.1111/j.1365-2753.2011.01773.x. [DOI] [PubMed] [Google Scholar]
- 10.Kansagara D, et al. Risk prediction models for hospital readmission: a systematic review. JAMA. 2011;306:1688–1698. doi: 10.1001/jama.2011.1515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gattis WA, O’Connor CM, Gallup DS, Hasselblad V, Gheorghiade M. Predischarge initiation of carvedilol in patients hospitalized for decompensated heart failure: results of the initiation management predischarge: process for assessment of carvedilol therapy in heart failure (IMPACT-HF) trial. J Am Coll Cardiol. 2004;43:1534–1541. doi: 10.1016/j.jacc.2003.12.040. [DOI] [PubMed] [Google Scholar]
- 12.Ambrosy AP, et al. Clinical course and predictive value of congestion during hospitalization in patients admitted for worsening signs and symptoms of heart failure with reduced ejection fraction: findings from the EVEREST trial. Eur Heart J. 2013;34:835–843. doi: 10.1093/eurheartj/ehs444. [DOI] [PubMed] [Google Scholar]
- 13.Patel A, et al. Mini-Cog performance: novel marker of post discharge risk among patients hospitalized for heart failure. Circ Heart Fail. 2015;8:8–16. doi: 10.1161/CIRCHEARTFAILURE.114.001438. [DOI] [PubMed] [Google Scholar]
- 14.Schwartz J, et al. Medicare Hospital Quality Chartbook Performance Report on Outcome Measures: September 2014. at, http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/OutcomeMeasures.html2014.
- 15.Bhatia RS, et al. Outcomes in patients with heart failure treated in hospitals with varying admission rates: population-based cohort study. BMJ Qual Saf. 2014;23:981–988. doi: 10.1136/bmjqs-2014-002816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Joynt KE, Orav EJ, Jha AK. The association between hospital volume and processes, outcomes, and costs of care for congestive heart failure. Ann Intern Med. 2011 doi: 10.1059/0003-4819-154-2-201101180-00008. http://dx.doi.org/10.7326/0003-4819-154-2-201101180-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Epstein AM, Jha AK, Orav EJ. The relationship between hospital admission rates and rehospitalizations. N Engl J Med. 2011;365:2287–2295. doi: 10.1056/NEJMsa1101942. [DOI] [PubMed] [Google Scholar]
- 18.Joynt KE, Jha AK. Who has higher readmission rates for heart failure, and why? Implications for efforts to improve care using financial incentives. Circ Cardiovasc Qual Outcomes. 2011;4:53–59. doi: 10.1161/CIRCOUTCOMES.110.950964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nagasako EM, Reidhead M, Waterman B, Dunagan WC. Adding socioeconomic data to hospital readmissions calculations may produce more useful results. Health Aff (Millwood) 2014;33(786–91) doi: 10.1377/hlthaff.2013.1148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kind AJH, et al. Neighborhood socioeconomic disadvantage and 30-day rehospitalization: a retrospective cohort study. Ann Intern Med. 2014;161:765–774. doi: 10.7326/M13-2946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vaduganathan M, Fonarow GC, Gheorghiade M. Drug therapy to reduce early readmission risk in heart failure: ready for prime time? JACC Heart Fail. 2013;1:361–364. doi: 10.1016/j.jchf.2013.04.010. [DOI] [PubMed] [Google Scholar]
- 22.The Digitalis Intervention Group. The effect of digoxin on mortality and morbidity in patients with heart failure. N Engl J Med. 1997;336:525–533. doi: 10.1056/NEJM199702203360801. [DOI] [PubMed] [Google Scholar]
- 23.Ahmed A, et al. Digoxin use and lower 30-day all-cause readmission for Medicare beneficiaries hospitalized for heart failure. Am J Med. 2014;127:61–70. doi: 10.1016/j.amjmed.2013.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Packer M, et al. The effect of carvedilol on morbidity and mortality in patients with chronic heart failure. U.S. Carvedilol Heart Failure Study Group. N Engl J Med. 1996;334:1349–1355. doi: 10.1056/NEJM199605233342101. [DOI] [PubMed] [Google Scholar]
- 25.Hernandez AF, et al. Clinical effectiveness of beta-blockers in heart failure. Findings from the OPTIMIZE-HF (Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients With Heart Failure) Registry. J Am Coll Cardiol. 2009;53:184–192. doi: 10.1016/j.jacc.2008.09.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fonarow GC, et al. Association between performance measures and clinical outcomes for patients hospitalized with heart failure. JAMA. 2007;297:61–70. doi: 10.1001/jama.297.1.61. [DOI] [PubMed] [Google Scholar]
- 27.McMurray John JV, et al. Angiotensin–neprilysin inhibition versus enalapril in heart failure. N Engl J Med. 2014 doi: 10.1056/NEJMoa1409077. http://dx.doi.org/10.1056/NEJMoa1409077. 140830040023009. [DOI] [PubMed] [Google Scholar]
- 28.Pitt B, et al. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. Randomized Aldactone Evaluation Study Investigators. N Engl JMed. 1999;341:709–717. doi: 10.1056/NEJM199909023411001. [DOI] [PubMed] [Google Scholar]
- 29.Zannad F, et al. Eplerenone in patients with systolic heart failure and mild symptoms. N Engl J Med. 2011;364:11–21. doi: 10.1056/NEJMoa1009492. [DOI] [PubMed] [Google Scholar]
- 30.Hernandez AF, et al. Associations between aldosterone antagonist therapy and risks of mortality and readmission among patients with heart failure and reduced ejection fraction. JAMA. 2012;308:2097–2107. doi: 10.1001/jama.2012.14795. [DOI] [PubMed] [Google Scholar]
- 31.Murray MD, et al. Open-label randomized trial of torsemide compared with furosemide therapy for patients with heart failure. Am J Med. 2001;111:513–520. doi: 10.1016/s0002-9343(01)00903-2. [DOI] [PubMed] [Google Scholar]
- 32.Cleland JGF, et al. The effect of cardiac resynchronization on morbidity and mortality in heart failure. N Engl J Med. 2005;352:1539–1549. doi: 10.1056/NEJMoa050496. [DOI] [PubMed] [Google Scholar]
- 33.Masoudi FA, et al. Comparative effectiveness of cardiac resynchronization therapy with an implantable cardioverter-defibrillator versus defibrillator therapy alone: a cohort study. Ann Intern Med. 2014;160:603–611. doi: 10.7326/M13-1879. [DOI] [PubMed] [Google Scholar]
- 34.Chaudhry SI, et al. Telemonitoring in patients with heart failure. N Engl J Med. 2010;363:2301–2309. doi: 10.1056/NEJMoa1010029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Van Veldhuisen DJ, et al. Intrathoracic impedance monitoring, audible patient alerts, and outcome in patients with heart failure. Circulation. 2011;124:1719–1726. doi: 10.1161/CIRCULATIONAHA.111.043042. [DOI] [PubMed] [Google Scholar]
- 36.Abraham WT, et al. Wireless pulmonary artery haemodynamic monitoring in chronic heart failure: a randomised controlled trial. Lancet. 2011;377:658–666. doi: 10.1016/S0140-6736(11)60101-3. [DOI] [PubMed] [Google Scholar]
- 37.Hansen LO, Young RS, Hinami K, Leung A, Williams MV. Interventions to reduce 30-day rehospitalization: a systematic review. Ann Intern Med. 2011 doi: 10.7326/0003-4819-155-8-201110180-00008. http://dx.doi.org/10.7326/0003-4819-155-8-201110180-00008. [DOI] [PubMed] [Google Scholar]
- 38.Bradley EH, et al. Hospital strategies associated with 30-day readmission rates for patients with heart failure. Circ Cardiovasc Qual Outcomes. 2013;6:444–450. doi: 10.1161/CIRCOUTCOMES.111.000101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ziaeian B, Araujo KLB, Van Ness PH, Horwitz LI. Medication reconciliation accuracy and patient understanding of intended medication changes on hospital discharge. J Gen Intern Med. 2012;27:1513–1520. doi: 10.1007/s11606-012-2168-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Salim Al-Damluji M, et al. Association of discharge summary quality with readmission risk for patients hospitalized with heart failure exacerbation. Circ Cardiovasc Qual Outcomes. 2015;8:109–111. doi: 10.1161/CIRCOUTCOMES.114.001476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rich MW, et al. A multidisciplinary intervention to prevent the readmission of elderly patients with congestive heart failure. N Engl J Med. 1995;333:1190–1195. doi: 10.1056/NEJM199511023331806. [DOI] [PubMed] [Google Scholar]
- 42.Krumholz HM, et al. Randomized trial of an education and support intervention to prevent readmission of patients with heart failure. J Am Coll Cardiol. 2002;39:83–89. doi: 10.1016/s0735-1097(01)01699-0. [DOI] [PubMed] [Google Scholar]
- 43.Sisk JE, et al. Effects of nurse management on the quality of heart failure care in minority communities: a randomized trial. Ann Intern Med. 2006;145:273–283. doi: 10.7326/0003-4819-145-4-200608150-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Phillips CO, et al. Comprehensive discharge planning with postdischarge support for older patients with congestive heart failure: a meta-analysis. JAMA. 2004;291:1358–1367. doi: 10.1001/jama.291.11.1358. [DOI] [PubMed] [Google Scholar]
- 45.McHugh MD, Berez J, Small DS. Hospitals with higher nurse staffing had lower odds of readmissions penalties than hospitals with lower staffing. Health Aff. 2013;32:1740–1747. doi: 10.1377/hlthaff.2013.0613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hernandez AF, et al. Relationship between early physician follow-up and 30-day readmission among Medicare beneficiaries hospitalized for heart failure. JAMA. 2010;303:1716–1722. doi: 10.1001/jama.2010.533. [DOI] [PubMed] [Google Scholar]
- 47.Krumholz HM, et al. Relationship between hospital readmission and mortality rates for patients hospitalized with acute myocardial infarction, heart failure, or pneumonia. JAMA. 2013;309:587–593. doi: 10.1001/jama.2013.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bhalla R, Kalkut G. Could medicare readmission policy exacerbate health care system inequity? Ann Intern Med. 2010;152:114–117. doi: 10.7326/0003-4819-152-2-201001190-00185. [DOI] [PubMed] [Google Scholar]
- 49.Joynt KE, Jha AK. A path forward on Medicare readmissions. N Engl J Med. 2013;368:1175–1177. doi: 10.1056/NEJMp1300122. [DOI] [PubMed] [Google Scholar]
- 50.Hu J, Gonsahn MD, Nerenz DR. Socioeconomic status and readmissions: evidence from an urban teaching hospital. Health Aff (Millwood) 2014;33:778–785. doi: 10.1377/hlthaff.2013.0816. [DOI] [PubMed] [Google Scholar]
- 51.Herrin J, et al. Community factors and hospital readmission rates. Health Serv Res. 2014:1–20. doi: 10.1111/1475-6773.12177. http://dx.doi.org/10.1111/1475-6773.12177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sperry BW, Ruiz G, Najjar SS. Hospital readmission in heart failure, a novel analysis of a longstanding problem. Heart Fail Rev. 2014 doi: 10.1007/s10741-014-9459-2. http://dx.doi.org/10.1007/s10741-014-9459-2. [DOI] [PubMed] [Google Scholar]
- 53.Setoguchi S, Stevenson LW, Schneeweiss S. Repeated hospitalizations predict mortality in the community population with heart failure. Am Heart J. 2007;154:260–266. doi: 10.1016/j.ahj.2007.01.041. [DOI] [PubMed] [Google Scholar]