Abstract
Type III secretion systems (T3SSs) are specialized secretion apparatus involved in the virulence of many Gram-negative pathogens, enabling the injection of bacterial type III effectors into host cells. The T3SS-dependent injection of effectors requires the insertion into host cell membranes of a pore-forming “translocon,” whose effects on cell responses remain ill-defined. As opposed to pore-forming toxins that damage host cell plasma membranes and induce cell survival mechanisms, T3SS-dependent pore formation is transient, being regulated by cell membrane repair mechanisms or bacterial effectors. Here, we review host cell responses to pore formation induced by T3SSs associated with the loss of plasma membrane integrity and regulation of innate immunity. We will particularly focus on recent advances in mechanisms controlling pore formation and the activity of the T3SS linked to type III effectors or bacterial proteases. The implications of the regulation of the T3SS translocon activity during the infectious process will be discussed.
Keywords: SPATE, pore formation, T3SS, membrane repair, cell death
Introduction
Through secreted proteins, bacterial pathogens have the capacity to induce the formation of pores into eukaryotic host cell membranes. Pore-forming toxins (PFTs) can exert direct cytotoxic effect by irreversibly damaging the plasma membrane, or, at sub-lethal concentrations, can induce cell signaling involved in cytoskeletal reorganization, or in a variety of defense and innate immune responses (1–6). Alternatively, secreted bacterial proteins, such as AB toxins or type III secretion system (T3SS) translocon components, can form transient pores at the plasma membranes to promote the delivery of bacterial virulence factors into the host cytosol. Although host cell responses to various AB toxins have been largely described (7–9), relatively little is known about signaling linked to pore formation mediated by T3SS translocon components.
The T3SS can be viewed as a molecular syringe that upon cell contact, allows the delivery of bacterial effectors directly from the bacterial cytoplasm to the host cytosol [for review, see Ref. (10, 11)]. This system is widely spread among Gram-negative bacterial pathogens and shows conserved structural and functional features. Much of our knowledge has been inferred from extensive studies on the Shigella, Salmonella, or Yersinia T3SSs, and specific characteristics have been reported for other T3SSs, such as those from enteropathogenic (EPEC) and enterohemorrhagic (EHEC) Escherichia coli.
As for AB toxins, T3SS-mediated injection of bacterial effectors through eukaryotic cell plasma membranes requires the formation of a “translocation” pore, which occurs upon contact of T3SS with host cell membrane. Cell contact triggers the secretion of translocators proteins through the T3SS: two hydrophobic translocators proteins insert in the host cell membrane to form the so-called translocon, whereas one hydrophilic translocator protein is thought to connect the membrane-inserted translocon and the T3SS needle [for review, see Ref. (12); Table 1]. Here, we will review the responses elicited by host cells, linked to the pore-forming activity of the T3SS, and discuss their role during bacterial pathogenesis.
Table 1.
Translocators components in various T3SSs [for review, see Ref. (12)].
| Hydrophilic protein | Hydrophobic protein with 2 TM domain | Hydrophobic protein with 1 TM domain | |
|---|---|---|---|
| EPEC/EHEC | EspA | EspB | EspD |
| Yersinia | LcrV | YopD | YopB |
| Salmonella | SipD | SipC | SipB |
| Shigella | IpaD | IpaC | IpaB |
| Pseudomonas | PcrV | PopD | PopB |
T3 Translocon and Pore Activity
Upon cell contact, two hydrophobic proteins forming the translocon and containing trans-membrane domains insert into the host cell plasma membrane. Membrane insertion is associated with conformational changes, leading to oligomerization occurring through coiled-coil domain interactions, required for pore formation [Table 1; (12–16)]. Interestingly, coiled-coil domain of translocator proteins share homology with PFT, suggesting common origins and oligomerization mechanisms (17). Although the hydrophilic protein does not integrate in membranes, it is absolutely required for pore activity, possibly by acting as an assembly platform for proper oligomerization of the translocon components (12). The hydrophilic protein is also presumed to provide a molecular link between the translocon and the T3SS needle, through which type III effectors are channeled to get access to the cell cytosol. It is generally admitted that during type III effector translocation into host cells, the translocon is connected to the needle, forming a sealed conduct that does not allow exchange with the extracellular medium. This view is supported by cryo-EM studies showing a continuum between the T3SS and host cell membranes during bacterial infection (18, 19). However, the Yersinia type III effector YopH secreted in the extracellular media was shown to translocate into host cells by hijacking translocon components, suggesting that an alternate AB5-like toxin translocation mechanism could also occur for type III effectors (20). Presumably, only translocons detached from T3SS are expected to form pores opened to the extracellular medium. While such considerations remain speculative, and such disconnection may occur following the translocation of injected type III effectors. Studies using artificial membranes have illustrated the pore-forming activity of purified translocon components (21). Although there are numerous evidence demonstrating pore-activity linked to T3SS, structures corresponding to pore-forming translocons are yet to be visualized during bacterial infection (13, 22–25).
Red blood cells (RBCs), which lack internal organelles, are unable to reseal membrane injuries and have been used to demonstrate T3SS-mediated pore formation (26). Release of hemoglobin by RBCs provides a metric for membrane damage linked to pore formation, which, in combination with solute size-dependent osmoprotection experiments, allows to estimate the size of membrane pores. Such experiments indicate that the T3SS induces the formation of pores within host cell membranes with an estimated size ranging from 1.2 to 5 nm, depending on the studies and bacterial systems (27–29). This diameter size is comparable to with that estimated for the inner diameter of the T3SS needle, consistent with a continuum between the needle and the membrane-inserted translocon during the injection of type III effectors. The analysis of the effects of mutations in translocator proteins shows a lack of correlation between T3SS-dependent RBCs’ hemolysis and translocation of type III effectors in epithelial cells (30–34). This suggests that T3SS-dependent pore formation measured by the RBC’s hemolysis assay does not implicate the same requirements as pore formation during translocation of effectors in epithelial cells. These issues are a matter of current debates. Other methods, including the use of fluorescent dyes, have been developed to demonstrate T3SS-dependent pore activity (25, 35).
Mechanism of T3SS-Dependent Pore Formation
The observations that (i) translocated effectors do not leak into the extracellular medium after injection into cells and (ii) only a minority of cells infected with T3SS-expressing bacteria show dye incorporation assay or K+ efflux, point to the inefficient capacity of the T3SS to mediate the formation of pore in nucleated cells (36–38). It was generally thought that as opposed to RBCs, membrane repair in nucleated cells was responsible for this relatively low pore-forming activity. As developed further, it is now clear that bacteria also control pore formation to avoid/or counteract detection by host cells.
In a very recent study, Sheahan and Isberg have identified host cell factors required for Yersinia T3SS-associated pore activity. Insertion and assembly of the translocon into the host cell membrane is a more complex process than originally thought, as numerous cytoskeletal and membrane trafficking proteins have been involved (39). This study confirms the key role played by actin and the small Rho GTPase in pore formation (40–42). Unexpectedly, Sheahan and Isberg also identified CCR5, a plasma membrane receptor, as playing a major role in T3-pore formation. CCR5 was recently identified to be a receptor for some PFT, emphasizing the functional homology the between T3 translocon and PFT (43).
Host Cell Responses to Pore Formation in Plasma Membranes
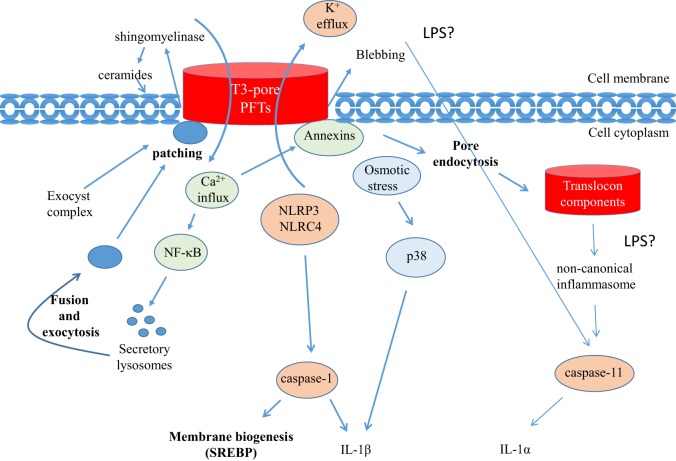
In response to membrane injuries, cells trigger repair mechanisms involving the detection and removal of damaged plasma membranes. Membrane injuries, such as those induced by PFTs, immediately trigger an osmotic stress response, as well as a Ca2+ influx and a K+ efflux that are sensed by host cells (4, 44–46). These responses activate MAP kinase signaling, inflammasomes, and NF-κB activation, which in turn lead to the elicitation of inflammatory and innate immune responses (Figure 1). Such signaling also activates membrane repair mechanisms: K+ efflux triggers NLRP3 activation, leading to the recruitment of Caspase-1 (IL-1-converting enzyme) (47). Caspase-1 has a dual effect; it cleaves pro-IL-1β to generate mature IL-1β and stimulates the sterol regulatory element-binding proteins (SREBPs) to promote membrane biogenesis (48). Fast-acting cortical membrane repair involving exocytic and endocytic processes are also well described (49, 50). Ca2+ influx triggered by pore formation is sensed by synaptotagmin, a Ca2+ sensor present at the surface of lysosomes. Intracellular Ca2+ increase determines the synaptotagmin-dependent fusion of specialized lysosomes, named secretory lysosomes, in large vesicles. These vesicles fuse with wounded membranes, a process that contributes to the patching of pores at the plasma membranes (26, 49, 50). Fusion of secretory lysosomes with wounded plasma membranes also leads to the release of lysosomal enzymes, such as sphingomyelinases, into the medium. Sphingomyelinases hydrolyze sphingomyelin to form ceramides that induce membrane curvature. This curvature is thought to initiate endocytosis of damage membranes that are subsequently targeted to intracellular degradation. Endocytosis has been proposed as an active repair mechanism of membrane damaged by PFTs (44). Ca2+ influx also leads to the binding of cytoplasmic annexins to the plasma membrane, resulting in the connection of the membrane to actin network. Annexin A5 was also shown to form a network limiting diffusion at the site of membrane injury (51). Ca2+ influx has also been associated with the annexin-dependent blebbing of the plasma membrane leading to the shedding of vesicles containing pores mediated by PFT in the extracellular milieu (52–54).
Figure 1.
Membrane repair and inflammasome activation mediated by T3 translocons and PFTs. Membrane injuries by PFTs or T3 translocon (T3-T) trigger an osmotic stress response, Ca2+ influx, and K+ efflux that are sensed by host cells. These responses activate innate immune responses and membrane repair mechanisms. K+ efflux, or possibly osmotic stress, associated with PFTs leads to the activation of the p38 MAPK and IL-1β secretion. In response to T3-pore formation, inflammasome and caspase-1 activation are also observed in association with K+ influx into the translocon component (T3-TC) containing vacuole. Following endocytosis, T3 translocon components can activate caspase-11 through the activation of the non-canonical inflammasome. Membrane repair mechanisms linked to Ca2+ influx, lysosomal exocytosis and annexin recruitment are observed. New membrane recruitment to the site of infection by the exocyst complex could also contribute to patch T3-pores.
Characterizing Signals Linked to Membrane Insertion and Pore Activity of the T3 Translocon
Identifying signals that specifically associated with the T3SS translocon is challenging because it is also required for the translocation of type III effectors, many of which being reported to regulate innate immune responses. Furthermore, various microbial structures, including structural components of the T3SA, act as pathogen-associated molecular patterns (PAMPs) and are sensed by host cells to induce innate immune responses that are not directly associated with translocon insertion into host membranes (55, 56). To identify translocon-specific signals, studies have reported the use of bacterial mutants lacking all type III effectors (effectorless strain) and/or using cells lacking the two main TLR adaptor proteins (MyD88−/− and Trif−/−) and hence, deficient for TLR signaling downstream of PAMPs. Such studies showed that the insertion of translocon components into the host plasma membrane activates an innate immune response that differs depending on the cell type (42). Insertion of the Yersinia translocon is associated with NLRP3 and NLRC4 activation with downstream signaling events leading to caspase-1 activation and IL-1β production (57, 58). The T3SS-dependent activation of NLRC4 has also been observed for Shigella, Salmonella, and Pseudomonas (59, 60). For Salmonella and Pseudomonas, such NLRC4 activation was shown to depend on T3SS-dependent pore formation and K+ efflux (37). Activation of the non-canonical caspase-11 (caspase 4 in humans) inflammasome has also been described to be dependent on the T3SS, although recent evidences indicate that bacterial LPS could account for caspase-11 activation (61–64).
The cytosolic presence of translocators, rather than pore formation, has also been described to activate the inflammasome (65). The detection of translocator components in the cytosol has been attributed to the cytoplasmic tail of one of translocators following its insertion in the plasma membrane, or, alternatively, to the endocytosis of the pore-forming translocon complex. In both cases, cytosolic access of T3 translocon components leads to canonical NLRP3 and non-canonical caspase-11 activation, similar to what has been described for cytosolic PAMPs (62, 65). Consistent with a role for translocon endocytosis, Senerovic et al. have described that the purified translocator component IpaB oligomerizes in membrane and forms ion channels promoting K+ influx upon internalization within endosomes, responsible for macrophages cell death. In this case, translocon-dependent K+ influx into vacuoles may affect endolysosomal membranes’ integrity, leading to caspase-1 activation downstream of the NLRC4 inflammasome (66).
Perhaps most indicative of T3SS-dependent pore-forming activity, membrane repair mechanisms are also activated upon bacterial infection. In response to Ca2+ influx linked to T3SS-dependent pores, synaptotagmin-dependent lysosomal exocytosis has been reported in Salmonella and Yersinia infected cells (39, 67). During infection, Salmonella and EPEC also trigger the recruitment and activation of the Ca2+-sensors annexins at the site of bacterial attachment (68–73).
Bacterial Mechanisms of Avoiding Cell Death Linked to T3SS-Mediated Pore Formation
Invasive bacteria, such as Salmonella or Shigella, promote their uptake in vacuole, resulting in a process leading to the removal of membrane-inserted translocons from the plasma membrane. This “self-removal” of membrane-inserted translocons may represent an additional factor contributing to the difficulty in detecting pore formation in epithelial cells infected by these bacteria. To minimize plasma membrane damages linked to T3 translocons, bacteria that multiply extracellularly have developed multiple strategies against inflammatory cell death. Injected type III effectors may downregulate cell death and inflammatory signals, by interfering with initiator or effector caspases and NLRC4 inflammasome activation (74). The role of these type III effectors has been recently reviewed elsewhere (57, 58, 75–77). Here, we will mostly discuss the bacterial regulation of T3SS-dependent pore formation.
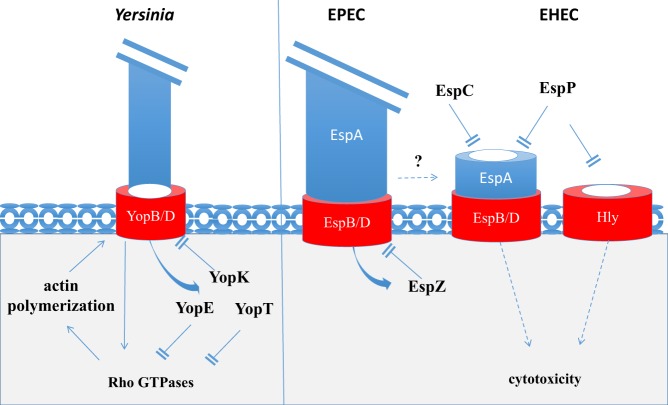
In Yersinia, at least three different type III effectors, such as YopK, YopE, and YopT, regulate T3SS-dependent pore formation and effector injection into host cells. The translocon component YopB activates both pro-inflammatory response and the small Rho GTPase, Ras (42, 78). YopB/D translocon insertion, in cooperation with invasin-beta1 integrin signaling, activates multiple Rho GTPases leading to actin polymerization, a step absolutely required for the Yersinia T3SS-dependent pore formation in the plasma membrane. The role of actin polymerization in the formation of the Yersinia T3SS-dependent pore is not clear but might reflect the importance to affix plasma membrane while translocon is inserted, or the translocon disconnection from the T3SA following effector injection in host cells. Among injected effectors, YopE and YopT display pore inhibition activity through the downregulation of several Rho GTPases (RhoA, RhoG, Rac1, and CDC42), linked to a GAP and protease activity toward these GTPases, respectively. Inhibition of Rho GTPase activity associated with actin depolymerization not only prevents pore formation but also reduces effector translocation. YopK also negatively regulates injection of type III effectors and cytotoxicity. As opposed to YopE and YopT regulating the T3SS activity through their action of Rho GTPases, YopK binds to the translocon and may directly clot it or induce conformational changes leading to translocation blockage (76). Although sharing little primary sequence homology with YopK, the EPEC/EHEC type III effector EspZ displays a similar activity (Figure 2). EspZ was shown to interact with the EPEC-translocon component EspD and prevents cell death by preventing the translocation of T3SS effectors into infected cells (79).
Figure 2.
Bacterial effectors regulating T3-pore formation. Upon cell contact and T3SS activation, the Yersinia YopB/D translocon components activate Rho GTPases leading to the polymerization of actin and T3-pore formation. The injected T3 effectors, such as YopK, YopE, and YopT, downregulate T3-pore formation and effector translocation. YopK directly acts on the T3 translocon. YopE and YopT inhibit RhoGTPases. EspZ shares an activity related to that of YopK by binding to the EPEC T3 translocon, inhibiting T3-pore formation and effector injection. EspC downregulates T3 pore by degrading the translocator components EspA/D, an activity shared by the EHEC EspP. EspP also downregulate the Hly PFT inserted in plasma membranes.
Proteolytic Degradation of T3-Pores by a Bacterial Serine Protease Autotransporter of Enterobacteriaceae
More recently, our group has reported a novel mechanism controlling T3SS-mediated pore formation and cytotoxicity induced by EPEC and EHEC (38). In addition to the T3SS, EPEC secretes other bacterial toxins involved in virulence. Among these, EspC, a protease belonging to the serine protease autotransporter of enterobacteriaceae (SPATE) family (80, 81), was shown to degrade the T3SS translocon components following contact with epithelial cells, thus downregulating T3SS-dependent pore formation and cytotoxicity. In EPEC, the hydrophilic translocator component EspA polymerizes into a filament connecting the T3SS needle to the translocon that is composed of the EspB and EspD hydrophobic proteins. EspC appears to preferentially target EspA associated with EspD. Since EspC does not prevent type III effector injection, it may recognize a specific conformation of EspA/D corresponding to a T3SS “by-product” with potential cytotoxic activity. Interestingly, EspP, the EspC hortologue in EHEC has been involved in the proteolytic degradation of the E. coli hemolysin Hly, a pore-forming cytolysin (82). The cleavage of Hly by EspP occurs in the region of the hydrophobic domain and lead to the inactivation of its pore-forming activity.
Epithelial Cell Death Linked to T3SS-Pores
Depending on the cell type and the extent of pore formation, membrane lesions can lead to apoptotic or necrotic cell death. It has been suggested that pores detected in epithelial cells infected with effectorless Yersinia or an EPEC espC mutant result from unsealed translocons similar to those found in membranes of erythrocytes. With the exception of T3SS-dependent cell death induced by Yersinia, which appears to implicate distinct pathways, T3SS-dependent cytotoxicity appears to be caspase independent (38, 79, 83, 84). Epithelial cells dying from T3SS-dependent unregulated pore formation show nuclear shrinkage without signs of nuclear fragmentation, consistent with non-apoptotic cell death (38, 79, 83, 84). The precise mechanism implicated in this T3SS-dependent death is unknown. In unrelated studies, however, nuclear shrinkage and caspase-independent cell death have been linked to the activation of phospholipase A2 (PLA2) (85). Interestingly, PLA2 activation associated with K+ efflux and/or Ca2+ influx triggers IL-1 β secretion (86, 87), as observed for T3SS-dependent pore formation. Nuclear shrinkage may correspond to a common response to membrane insults induced by PFTs and T3SS-dependent unregulated pore formation (88, 89).
Concluding Remarks and Perspectives
As reviewed here, T3SS-expressing bacteria have developed a diversity of mechanisms to downregulate the formation of pores linked to the activity of T3SS translocon, reflecting the importance of this process in the pathophysiology of bacterial infections. In the absence of such translocon regulatory processes, a variety of inflammatory and death processes can be induced, depending on the bacterial pathogen. Although the insertion of T3SS-translocons during type III effector injection may induce a common canonical response associated with the activation of the NLRC4 inflammasome and eventually, necrotic cell death, these responses may be subsequently further tuned by other bacterial effectors. Deciphering how these signals integrate during the course of the bacterial infectious process represents a challenge needed to be addressed in future studies. Understanding how the T3SS pore formation and injection of effector is regulated could also lead to the development of innovative therapeutic molecules, widening the spectrum of currently studied T3SS inhibitor (90, 91).
Author Contributions
JG wrote the manuscript, and GN edited the manuscript.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Funding
The work was supported in part by grants from the Labex Memolife and the Idex (ANR-10-IDEX-0001-02 PSL).
References
- 1.Freche B, Reig N, van der Goot FG. The role of the inflammasome in cellular responses to toxins and bacterial effectors. Semin Immunopathol (2007) 29:249–60. 10.1007/s00281-007-0085-0 [DOI] [PubMed] [Google Scholar]
- 2.Gonzalez MR, Bischofberger M, Pernot L, van der Goot FG, Freche B. Bacterial pore-forming toxins: the (w)hole story? Cell Mol Life Sci (2008) 65:493–507. 10.1007/s00018-007-7434-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Garcia-Saez AJ, Buschhorn SB, Keller H, Anderluh G, Simons K, Schwille P. Oligomerization and pore formation by equinatoxin II inhibit endocytosis and lead to plasma membrane reorganization. J Biol Chem (2011) 286:37768–77. 10.1074/jbc.M111.281592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Los FC, Randis TM, Aroian RV, Ratner AJ. Role of pore-forming toxins in bacterial infectious diseases. Microbiol Mol Biol Rev (2013) 77:173–207. 10.1128/MMBR.00052-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wiles TJ, Mulvey MA. The RTX pore-forming toxin alpha-hemolysin of uropathogenic Escherichia coli: progress and perspectives. Future Microbiol (2013) 8:73–84. 10.2217/fmb.12.131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Diabate M, Munro P, Garcia E, Jacquel A, Michel G, Obba S, et al. Escherichia coli alpha-hemolysin counteracts the anti-virulence innate immune response triggered by the Rho GTPase activating toxin CNF1 during bacteremia. PLoS Pathog (2015) 11:e1004732. 10.1371/journal.ppat.1004732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Beddoe T, Paton AW, Le Nours J, Rossjohn J, Paton JC. Structure, biological functions and applications of the AB5 toxins. Trends Biochem Sci (2010) 35:411–8. 10.1016/j.tibs.2010.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Odumosu O, Nicholas D, Yano H, Langridge W. AB toxins: a paradigm switch from deadly to desirable. Toxins (Basel) (2010) 2:1612–45. 10.3390/toxins2071612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lemichez E, Barbieri JT. General aspects and recent advances on bacterial protein toxins. Cold Spring Harb Perspect Med (2013) 3:a013573. 10.1101/cshperspect.a013573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cornelis GR. The type III secretion injectisome. Nat Rev Microbiol (2006) 4:811–25. 10.1038/nrmicro1526 [DOI] [PubMed] [Google Scholar]
- 11.Puhar A, Sansonetti PJ. Type III secretion system. Curr Biol (2014) 24:R784–91. 10.1016/j.cub.2014.07.016 [DOI] [PubMed] [Google Scholar]
- 12.Mattei PJ, Faudry E, Job V, Izore T, Attree I, Dessen A. Membrane targeting and pore formation by the type III secretion system translocon. FEBS J (2011) 278:414–26. 10.1111/j.1742-4658.2010.07974.x [DOI] [PubMed] [Google Scholar]
- 13.Schoehn G, Di Guilmi AM, Lemaire D, Attree I, Weissenhorn W, Dessen A. Oligomerization of type III secretion proteins PopB and PopD precedes pore formation in Pseudomonas. EMBO J (2003) 22:4957–67. 10.1093/emboj/cdg499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dickenson NE, Choudhari SP, Adam PR, Kramer RM, Joshi SB, Middaugh CR, et al. Oligomeric states of the Shigella translocator protein IpaB provide structural insights into formation of the type III secretion translocon. Protein Sci (2013) 22:614–27. 10.1002/pro.2245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Myeni SK, Wang L, Zhou D. SipB-SipC complex is essential for translocon formation. PLoS One (2013) 8:e60499. 10.1371/journal.pone.0060499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Adam PR, Dickenson NE, Greenwood JC, II, Picking WL, Picking WD. Influence of oligomerization state on the structural properties of invasion plasmid antigen B from Shigella flexneri in the presence and absence of phospholipid membranes. Proteins (2014) 82:3013–22. 10.1002/prot.24662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Barta ML, Dickenson NE, Patil M, Keightley A, Wyckoff GJ, Picking WD, et al. The structures of coiled-coil domains from type III secretion system translocators reveal homology to pore-forming toxins. J Mol Biol (2012) 417:395–405. 10.1016/j.jmb.2012.01.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hu B, Morado DR, Margolin W, Rohde JR, Arizmendi O, Picking WL, et al. Visualization of the type III secretion sorting platform of Shigella flexneri. Proc Natl Acad Sci U S A (2015) 112:1047–52. 10.1073/pnas.1411610112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nans A, Kudryashev M, Saibil HR, Hayward RD. Structure of a bacterial type III secretion system in contact with a host membrane in situ. Nat Commun (2015) 6:10114. 10.1038/ncomms10114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Edgren T, Forsberg A, Rosqvist R, Wolf-Watz H. Type III secretion in Yersinia: injectisome or not? PLoS Pathog (2012) 8:e1002669. 10.1371/journal.ppat.1002669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wager B, Faudry E, Wills T, Attree I, Delcour AH. Current fluctuation analysis of the PopB and PopD translocon components of the Pseudomonas aeruginosa type III secretion system. Biophys J (2013) 104:1445–55. 10.1016/j.bpj.2013.02.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ide T, Laarmann S, Greune L, Schillers H, Oberleithner H, Schmidt MA. Characterization of translocation pores inserted into plasma membranes by type III-secreted Esp proteins of enteropathogenic Escherichia coli. Cell Microbiol (2001) 3:669–79. 10.1046/j.1462-5822.2001.00146.x [DOI] [PubMed] [Google Scholar]
- 23.Veenendaal AK, Hodgkinson JL, Schwarzer L, Stabat D, Zenk SF, Blocker AJ. The type III secretion system needle tip complex mediates host cell sensing and translocon insertion. Mol Microbiol (2007) 63:1719–30. 10.1111/j.1365-2958.2007.05620.x [DOI] [PubMed] [Google Scholar]
- 24.Montagner C, Arquint C, Cornelis GR. Translocators YopB and YopD from Yersinia enterocolitica form a multimeric integral membrane complex in eukaryotic cell membranes. J Bacteriol (2011) 193:6923–8. 10.1128/JB.05555-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chatterjee A, Caballero-Franco C, Bakker D, Totten S, Jardim A. Pore-forming activity of the Escherichia coli type III secretion system protein EspD. J Biol Chem (2015) 290:25579–94. 10.1074/jbc.M115.648204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McNeil PL, Kirchhausen T. An emergency response team for membrane repair. Nat Rev Mol Cell Biol (2005) 6:499–505. 10.1038/nrm1665 [DOI] [PubMed] [Google Scholar]
- 27.Blocker A, Gounon P, Larquet E, Niebuhr K, Cabiaux V, Parsot C, et al. The tripartite type III secretion of Shigella flexneri inserts IpaB and IpaC into host membranes. J Cell Biol (1999) 147:683–93. 10.1083/jcb.147.3.683 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Buttner D, Bonas U. Port of entry – the type III secretion translocon. Trends Microbiol (2002) 10:186–92. 10.1016/S0966-842X(02)02331-4 [DOI] [PubMed] [Google Scholar]
- 29.Mueller CA, Broz P, Cornelis GR. The type III secretion system tip complex and translocon. Mol Microbiol (2008) 68:1085–95. 10.1111/j.1365-2958.2008.06237.x [DOI] [PubMed] [Google Scholar]
- 30.Barzu S, Benjelloun-Touimi Z, Phalipon A, Sansonetti P, Parsot C. Functional analysis of the Shigella flexneri IpaC invasin by insertional mutagenesis. Infect Immun (1997) 65:1599–605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Olsson J, Edqvist PJ, Broms JE, Forsberg A, Wolf-Watz H, Francis MS. The YopD translocator of Yersinia pseudotuberculosis is a multifunctional protein comprised of discrete domains. J Bacteriol (2004) 186:4110–23. 10.1128/JB.186.13.4110-4123.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Picking WL, Nishioka H, Hearn PD, Baxter MA, Harrington AT, Blocker A, et al. IpaD of Shigella flexneri is independently required for regulation of Ipa protein secretion and efficient insertion of IpaB and IpaC into host membranes. Infect Immun (2005) 73:1432–40. 10.1128/IAI.73.3.1432-1440.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Luo W, Donnenberg MS. Analysis of the function of enteropathogenic Escherichia coli EspB by random mutagenesis. Infect Immun (2006) 74:810–20. 10.1128/IAI.74.2.810-820.2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Roehrich AD, Martinez-Argudo I, Johnson S, Blocker AJ, Veenendaal AK. The extreme C terminus of Shigella flexneri IpaB is required for regulation of type III secretion, needle tip composition, and binding. Infect Immun (2010) 78:1682–91. 10.1128/IAI.00645-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Faudry E, Perdu C, Attree I. Pore formation by T3SS translocators: liposome leakage assay. Methods Mol Biol (2013) 966:173–85. 10.1007/978-1-62703-245-2_11 [DOI] [PubMed] [Google Scholar]
- 36.Viboud GI, Bliska JB. A bacterial type III secretion system inhibits actin polymerization to prevent pore formation in host cell membranes. EMBO J (2001) 20:5373–82. 10.1093/emboj/20.19.5373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Arlehamn CS, Petrilli V, Gross O, Tschopp J, Evans TJ. The role of potassium in inflammasome activation by bacteria. J Biol Chem (2010) 285:10508–18. 10.1074/jbc.M109.067298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Guignot J, Segura A, Tran Van Nhieu G. The serine protease EspC from enteropathogenic Escherichia coli regulates pore formation and cytotoxicity mediated by the type III secretion system. PLoS Pathog (2015) 11:e1005013. 10.1371/journal.ppat.1005013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sheahan KL, Isberg RR. Identification of mammalian proteins that collaborate with type III secretion system function: involvement of a chemokine receptor in supporting translocon activity. MBio (2015) 6:e2023–2014. 10.1128/mBio.02023-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mounier J, Popoff MR, Enninga J, Frame MC, Sansonetti PJ, Van Nhieu GT. The IpaC carboxyterminal effector domain mediates Src-dependent actin polymerization during Shigella invasion of epithelial cells. PLoS Pathog (2009) 5:e1000271. 10.1371/journal.ppat.1000271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Verove J, Bernarde C, Bohn YS, Boulay F, Rabiet MJ, Attree I, et al. Injection of Pseudomonas aeruginosa exo toxins into host cells can be modulated by host factors at the level of translocon assembly and/or activity. PLoS One (2012) 7:e30488. 10.1371/journal.pone.0030488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bliska JB, Wang X, Viboud GI, Brodsky IE. Modulation of innate immune responses by Yersinia type III secretion system translocators and effectors. Cell Microbiol (2013) 15:1622–31. 10.1111/cmi.12164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.DuMont AL, Torres VJ. Cell targeting by the Staphylococcus aureus pore-forming toxins: it’s not just about lipids. Trends Microbiol (2014) 22:21–7. 10.1016/j.tim.2013.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Andrews NW, Almeida PE, Corrotte M. Damage control: cellular mechanisms of plasma membrane repair. Trends Cell Biol (2014) 24:734–42. 10.1016/j.tcb.2014.07.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Draeger A, Schoenauer R, Atanassoff AP, Wolfmeier H, Babiychuk EB. Dealing with damage: plasma membrane repair mechanisms. Biochimie (2014) 107(Pt A):66–72. 10.1016/j.biochi.2014.08.008 [DOI] [PubMed] [Google Scholar]
- 46.Babiychuk EB, Draeger A. Defying death: cellular survival strategies following plasmalemmal injury by bacterial toxins. Semin Cell Dev Biol (2015) 45:39–47. 10.1016/j.semcdb.2015.10.016 [DOI] [PubMed] [Google Scholar]
- 47.Munoz-Planillo R, Kuffa P, Martinez-Colon G, Smith BL, Rajendiran TM, Nunez G. K(+) efflux is the common trigger of NLRP3 inflammasome activation by bacterial toxins and particulate matter. Immunity (2013) 38:1142–53. 10.1016/j.immuni.2013.05.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gurcel L, Abrami L, Girardin S, Tschopp J, van der Goot FG. Caspase-1 activation of lipid metabolic pathways in response to bacterial pore-forming toxins promotes cell survival. Cell (2006) 126:1135–45. 10.1016/j.cell.2006.07.033 [DOI] [PubMed] [Google Scholar]
- 49.Idone V, Tam C, Andrews NW. Two-way traffic on the road to plasma membrane repair. Trends Cell Biol (2008) 18:552–9. 10.1016/j.tcb.2008.09.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Idone V, Tam C, Goss JW, Toomre D, Pypaert M, Andrews NW. Repair of injured plasma membrane by rapid Ca2+-dependent endocytosis. J Cell Biol (2008) 180:905–14. 10.1083/jcb.200708010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bouter A, Carmeille R, Gounou C, Bouvet F, Degrelle SA, Evain-Brion D, et al. Review: annexin-A5 and cell membrane repair. Placenta (2015) 36(Suppl 1):S43–9. 10.1016/j.placenta.2015.01.193 [DOI] [PubMed] [Google Scholar]
- 52.Draeger A, Monastyrskaya K, Babiychuk EB. Plasma membrane repair and cellular damage control: the annexin survival kit. Biochem Pharmacol (2011) 81:703–12. 10.1016/j.bcp.2010.12.027 [DOI] [PubMed] [Google Scholar]
- 53.Cassidy SK, O’Riordan MX. More than a pore: the cellular response to cholesterol-dependent cytolysins. Toxins (Basel) (2013) 5:618–36. 10.3390/toxins5040618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Jaiswal JK, Lauritzen SP, Scheffer L, Sakaguchi M, Bunkenborg J, Simon SM, et al. S100A11 is required for efficient plasma membrane repair and survival of invasive cancer cells. Nat Commun (2014) 5:3795. 10.1038/ncomms4795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Miao EA, Mao DP, Yudkovsky N, Bonneau R, Lorang CG, Warren SE, et al. Innate immune detection of the type III secretion apparatus through the NLRC4 inflammasome. Proc Natl Acad Sci U S A (2010) 107:3076–80. 10.1073/pnas.0913087107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hwang I, Park S, Hong S, Kim EH, Yu JW. Salmonella promotes ASC oligomerization-dependent caspase-1 activation. Immune Netw (2012) 12:284–90. 10.4110/in.2012.12.6.284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Brodsky IE, Palm NW, Sadanand S, Ryndak MB, Sutterwala FS, Flavell RA, et al. A Yersinia effector protein promotes virulence by preventing inflammasome recognition of the type III secretion system. Cell Host Microbe (2010) 7:376–87. 10.1016/j.chom.2010.04.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kwuan L, Adams W, Auerbuch V. Impact of host membrane pore formation by the Yersinia pseudotuberculosis type III secretion system on the macrophage innate immune response. Infect Immun (2013) 81:905–14. 10.1128/IAI.01014-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sutterwala FS, Mijares LA, Li L, Ogura Y, Kazmierczak BI, Flavell RA. Immune recognition of Pseudomonas aeruginosa mediated by the IPAF/NLRC4 inflammasome. J Exp Med (2007) 204:3235–45. 10.1084/jem.20071239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Abdelaziz DH, Amr K, Amer AO. Nlrc4/Ipaf/CLAN/CARD12: more than a flagellin sensor. Int J Biochem Cell Biol (2011) 42:789–91. 10.1016/j.biocel.2010.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Casson CN, Copenhaver AM, Zwack EE, Nguyen HT, Strowig T, Javdan B, et al. Caspase-11 activation in response to bacterial secretion systems that access the host cytosol. PLoS Pathog (2013) 9:e1003400. 10.1371/journal.ppat.1003400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Shin S, Brodsky IE. Caspase-11: the noncanonical guardian of cytosolic sanctity. Cell Host Microbe (2013) 13:243–5. 10.1016/j.chom.2013.02.011 [DOI] [PubMed] [Google Scholar]
- 63.Rivers-Auty J, Brough D. Potassium efflux fires the canon: potassium efflux as a common trigger for canonical and noncanonical NLRP3 pathways. Eur J Immunol (2015) 45:2758–61. 10.1002/eji.201545958 [DOI] [PubMed] [Google Scholar]
- 64.Stowe I, Lee B, Kayagaki N. Caspase-11: arming the guards against bacterial infection. Immunol Rev (2015) 265:75–84. 10.1111/imr.12292 [DOI] [PubMed] [Google Scholar]
- 65.Zwack EE, Snyder AG, Wynosky-Dolfi MA, Ruthel G, Philip NH, Marketon MM, et al. Inflammasome activation in response to the Yersinia type III secretion system requires hyperinjection of translocon proteins YopB and YopD. MBio (2015) 6:e2095–2014. 10.1128/mBio.02095-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Senerovic L, Tsunoda SP, Goosmann C, Brinkmann V, Zychlinsky A, Meissner F, et al. Spontaneous formation of IpaB ion channels in host cell membranes reveals how Shigella induces pyroptosis in macrophages. Cell Death Dis (2012) 3:e384. 10.1038/cddis.2012.124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Roy D, Liston DR, Idone VJ, Di A, Nelson DJ, Pujol C, et al. A process for controlling intracellular bacterial infections induced by membrane injury. Science (2004) 304:1515–8. 10.1126/science.1098371 [DOI] [PubMed] [Google Scholar]
- 68.Zobiack N, Rescher U, Laarmann S, Michgehl S, Schmidt MA, Gerke V. Cell-surface attachment of pedestal-forming enteropathogenic E. coli induces a clustering of raft components and a recruitment of annexin 2. J Cell Sci (2002) 115:91–8. [DOI] [PubMed] [Google Scholar]
- 69.Rescher U, Ruhe D, Ludwig C, Zobiack N, Gerke V. Annexin 2 is a phosphatidylinositol (4,5)-bisphosphate binding protein recruited to actin assembly sites at cellular membranes. J Cell Sci (2004) 117:3473–80. 10.1242/jcs.01208 [DOI] [PubMed] [Google Scholar]
- 70.Goebeler V, Ruhe D, Gerke V, Rescher U. Annexin A8 displays unique phospholipid and F-actin binding properties. FEBS Lett (2006) 580:2430–4. 10.1016/j.febslet.2006.03.076 [DOI] [PubMed] [Google Scholar]
- 71.Tobe T. Cytoskeleton-modulating effectors of enteropathogenic and enterohemorrhagic Escherichia coli: role of EspL2 in adherence and an alternative pathway for modulating cytoskeleton through annexin A2 function. FEBS J (2010) 277:2403–8. 10.1111/j.1742-4658.2010.07654.x [DOI] [PubMed] [Google Scholar]
- 72.Munera D, Martinez E, Varyukhina S, Mahajan A, Ayala-Sanmartin J, Frankel G. Recruitment and membrane interactions of host cell proteins during attachment of enteropathogenic and enterohaemorrhagic Escherichia coli. Biochem J (2012) 445:383–92. 10.1042/BJ20120533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Jolly C, Winfree S, Hansen B, Steele-Mortimer O. The annexin A2/p11 complex is required for efficient invasion of Salmonella Typhimurium in epithelial cells. Cell Microbiol (2014) 16:64–77. 10.1111/cmi.12180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Al Moussawi K, Kazmierczak BI. Distinct contributions of interleukin-1alpha (IL-1alpha) and IL-1beta to innate immune recognition of Pseudomonas aeruginosa in the lung. Infect Immun (2014) 82:4204–11. 10.1128/IAI.02218-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Shin H, Cornelis GR. Type III secretion translocation pores of Yersinia enterocolitica trigger maturation and release of pro-inflammatory IL-1beta. Cell Microbiol (2007) 9:2893–902. 10.1111/j.1462-5822.2007.01004.x [DOI] [PubMed] [Google Scholar]
- 76.Dewoody RS, Merritt PM, Marketon MM. Regulation of the Yersinia type III secretion system: traffic control. Front Cell Infect Microbiol (2013) 3:4. 10.3389/fcimb.2013.00004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Wong Fok Lung T, Pearson JS, Schuelein R, Hartland EL. The cell death response to enteropathogenic Escherichia coli infection. Cell Microbiol (2014) 16:1736–45. 10.1111/cmi.12371 [DOI] [PubMed] [Google Scholar]
- 78.Viboud GI, So SS, Ryndak MB, Bliska JB. Proinflammatory signalling stimulated by the type III translocation factor YopB is counteracted by multiple effectors in epithelial cells infected with Yersinia pseudotuberculosis. Mol Microbiol (2003) 47:1305–15. 10.1046/j.1365-2958.2003.03350.x [DOI] [PubMed] [Google Scholar]
- 79.Berger CN, Crepin VF, Baruch K, Mousnier A, Rosenshine I, Frankel G. EspZ of enteropathogenic and enterohemorrhagic Escherichia coli regulates type III secretion system protein translocation. MBio (2012) 3:e00317-12. 10.1128/mBio.00317-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Dautin N. Serine protease autotransporters of enterobacteriaceae (SPATEs): biogenesis and function. Toxins (Basel) (2010) 2:1179–206. 10.3390/toxins2061179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Ruiz-Perez F, Nataro JP. Bacterial serine proteases secreted by the autotransporter pathway: classification, specificity, and role in virulence. Cell Mol Life Sci (2014) 71:745–70. 10.1007/s00018-013-1355-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Brockmeyer J, Aldick T, Soltwisch J, Zhang W, Tarr PI, Weiss A, et al. Enterohaemorrhagic Escherichia coli haemolysin is cleaved and inactivated by serine protease EspPalpha. Environ Microbiol (2011) 13:1327–41. 10.1111/j.1462-2920.2011.02431.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Stockbauer KE, Foreman-Wykert AK, Miller JF. Bordetella type III secretion induces caspase 1-independent necrosis. Cell Microbiol (2003) 5:123–32. 10.1046/j.1462-5822.2003.00260.x [DOI] [PubMed] [Google Scholar]
- 84.Zhao Z, Zhang L, Ren C, Zhao J, Chen C, Jiang X, et al. Autophagy is induced by the type III secretion system of Vibrio alginolyticus in several mammalian cell lines. Arch Microbiol (2011) 193:53–61. 10.1007/s00203-010-0646-9 [DOI] [PubMed] [Google Scholar]
- 85.Shinzawa K, Tsujimoto Y. PLA2 activity is required for nuclear shrinkage in caspase-independent cell death. J Cell Biol (2003) 163:1219–30. 10.1083/jcb.200306159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Walev I, Klein J, Husmann M, Valeva A, Strauch S, Wirtz H, et al. Potassium regulates IL-1 beta processing via calcium-independent phospholipase A2. J Immunol (2000) 164:5120–4. 10.4049/jimmunol.164.10.5120 [DOI] [PubMed] [Google Scholar]
- 87.Andrei C, Margiocco P, Poggi A, Lotti LV, Torrisi MR, Rubartelli A. Phospholipases C and A2 control lysosome-mediated IL-1 beta secretion: implications for inflammatory processes. Proc Natl Acad Sci U S A (2004) 101:9745–50. 10.1073/pnas.0308558101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Cockeran R, Theron AJ, Steel HC, Matlola NM, Mitchell TJ, Feldman C, et al. Proinflammatory interactions of pneumolysin with human neutrophils. J Infect Dis (2001) 183:604–11. 10.1086/318536 [DOI] [PubMed] [Google Scholar]
- 89.Noor S, Goldfine H, Tucker DE, Suram S, Lenz LL, Akira S, et al. Activation of cytosolic phospholipase A2alpha in resident peritoneal macrophages by Listeria monocytogenes involves listeriolysin O and TLR2. J Biol Chem (2008) 283:4744–55. 10.1074/jbc.M709956200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Marshall NC, Finlay BB. Targeting the type III secretion system to treat bacterial infections. Expert Opin Ther Targets (2014) 18:137–52. 10.1517/14728222.2014.855199 [DOI] [PubMed] [Google Scholar]
- 91.Gu L, Zhou S, Zhu L, Liang C, Chen X. Small-molecule inhibitors of the type III secretion system. Molecules (2015) 20:17659–74. 10.3390/molecules200917659 [DOI] [PMC free article] [PubMed] [Google Scholar]