Abstract
Vitamin C was first suggested to have cancer-fighting properties in the 1930s and has been the subject of controversy ever since. Despite repeated reports of selective cancer cell toxicity induced by high-dose vitamin C treatment in vitro and in mouse models, the mechanism of action has remained elusive.
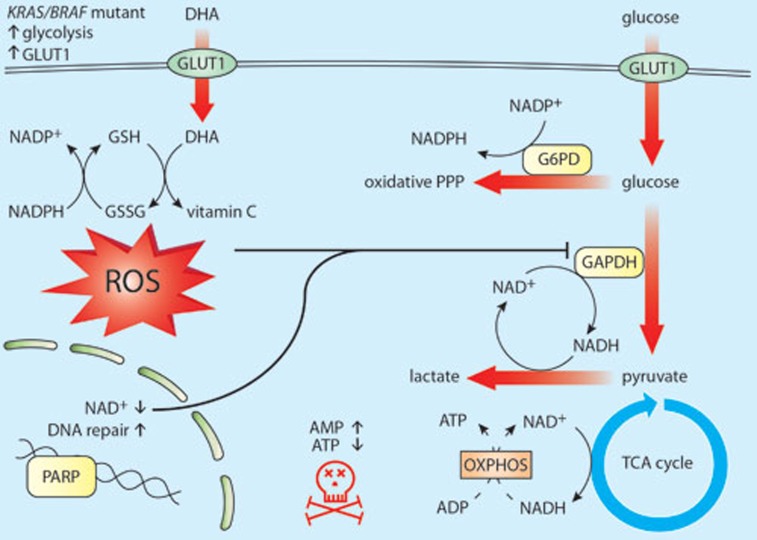
Yun et al.1 have recently shed light on what was until now the elusive mechanism by which vitamin C (aka ascorbate) induces toxicity in selected oncogene-driven cancers. They reported that in cells with mutations of KRAS or BRAF, death is not caused by vitamin C itself, but rather by its oxidized form dehydroascorbate (DHA). Whereas vitamin C enters cells through sodium cotransporters, DHA competes with glucose for uptake through glucose transporters (particularly GLUT1 and GLUT4) and then is reduced back to vitamin C in cells2 (Figure 1). It was previously observed that while melanoma cell lines take up DHA at much higher rates than vitamin C, normal melanocytes do not, demonstrating that transformation-driven upregulation of GLUTs leads to increased uptake of DHA3. More recently, using Magnetic Resonance Spectroscopy Imaging, it was demonstrated that hyperpolarized 13C-labeled DHA is rapidly taken up by cancer cells and converted to vitamin C, illustrating the tumors' reducing state4. Yun et al.1 now show that the reduction of DHA back to vitamin C is at the crux of the vitamin C-induced cell death observed in these cancer cells.
Figure 1.
Mechanistic overview of proposed vitamin C toxicity in CRCs driven by KRAS and BRAF mutations. KRAS and BRAF mutations induce metabolic reprogramming by upregulating GLUT1, glucose uptake, and glycolytic flux. Upon vitamin C treatment and its extracellular oxidation, DHA (the oxidized form of vitamin C) is taken up through GLUT1 and is reduced back to vitamin C in the cells, depleting GSH and NADPH. Consequently, an increase in ROS leads to GAPDH oxidation, and with it, to a decrease in glycolytic flux. In parallel, ROS-mediated oxidative DNA damage induces PARP activation and subsequently, NAD+ levels fall and cause additional inhibition of GAPDH and glycolysis, resulting in energy crisis and cell death.
Mutations in KRAS or BRAF are found in approximately half of the cases of colorectal cancer (CRC) and their expression correlates with an increase in GLUT1 expression, glucose uptake and reliance on glycolysis. Yun et al.1 observed that vitamin C is oxidized to DHA in tissue culture media and that KRAS or BRAF mutated CRC cell lines take up more DHA compared to their wild-type counterparts. More importantly, they found that DHA induces death in the mutant lines, but not in wild-type counterparts overexpressing GLUT1, suggesting that additional oncogenic reprogramming is necessary for DHA-induced toxicity. The authors then profiled metabolic changes after treatment with vitamin C. In cells with KRAS or BRAF mutations, they found an accumulation of the glycolytic intermediates upstream of glyceraldehyde 3-phosphate dehydrogenase (GAPDH) whereas those downstream of GAPDH were depleted. This indicated a decrease in GAPDH activity and a concomitant diversion of glucose into the oxidative phase of the pentose phosphate pathway (PPP), a metabolic shift that, upon oxidative stress, helps restore NADPH levels and cellular reducing potential (Figure 1). Indeed, Yun and co-workers found that the intracellular reduction of DHA back to vitamin C depleted the cellular stores of reduced glutathione (GSH, the major antioxidant in cells), leading to an increase in reactive oxygen species (ROS). Furthermore, they found that, upon exposure to DHA, GAPDH itself was oxidized (on Cys152), and consequently inhibited. Inhibition of GAPDH caused energy stress in the highly glycolytic mutant cell lines, leading to cell death. In mice harboring tumor xenografts with either KRAS or BRAF mutations, treatment with high doses of vitamin C reduced tumor size. Treatment also reduced the number and size of polyps in an Apc-driven transgenic mouse model of intestinal cancer, but again, only in tumors expressing mutant Kras. Moreover, in addition to showing the direct inhibition of GAPDH by oxidation, the authors demonstrated that its activity is further hindered by DHA-induced NAD+ depletion, since GAPDH activity relies on the availability of NAD+ as a co-substrate. The major NAD+ consumer, the DNA repairing enzyme poly ADP-ribose polymerase (PARP) was then investigated. It was found that the increase in ROS after high-dose vitamin C treatment also induced DNA damage and PARP activation in KRAS or BRAF transformed cells. Providing the cells with a PARP inhibitor or an NAD+ precursor partially rescued their viability. Thus, ROS cause the inhibition of GAPDH activity in cells on two fronts: first, via inducing its direct oxidation and second, by causing NAD+ depletion (Figure 1). Yun et al.1 thus demonstrated an intricate mechanism by which oncogenic reprogramming, which causes glycolysis addiction, induces a metabolic vulnerability which can be exploited with high doses of DHA that elevate intracellular ROS as it is converted back to vitamin C.
Despite numerous clinical studies, the anti-cancer property of vitamin C has remained controversial. Potential translation of the mechanism presented by Yun et al.1 to therapeutic application raises concerns regarding toxicities of high-dose vitamin C treatment. Though the authors do not report side effects in their mice (treated daily with 4-8 g/kg body weight IP), the upper dose equates to over half a kilogram for the average person. High-dose oral supplementation of vitamin C is associated with increased kidney stone incidence, and clinical studies demonstrated significant renal, cardiac, and metabolic toxicity upon vitamin C administration. Still, overall reports of toxicity are variable, poorly graded, and therefore inconclusive5,6. Affinity studies of DHA for GLUT1 may help establish a lower effective dose, though unwanted side effects in tissues that highly express GLUT1 need to be considered. The brain obtains vitamin C by uptake of DHA through GLUT1 at the blood-brain barrier and its subsequent reduction7. Erythrocytes express high levels of GLUT1 and are crucial for ascorbate recycling, keeping DHA levels low8. Importantly, erythrocytes rely solely on glycolysis for energy production. Thus, high DHA levels may induce brain toxicity and haemolysis via mechanisms similar to those described by Yun et al.1.
Though vitamin C oxidizes rapidly in tissue culture media, it acts mainly as an antioxidant in vivo. It remains unclear how and where circulating vitamin C is oxidized in vivo, an issue not addressed by Yun et al.1. Oxidation of vitamin C to DHA by tumor stroma has been suggested9, complicating the ability to predict tumor responsiveness to the treatment. As such, without being able to control the extent of vitamin C oxidation to DHA, effectiveness and toxicity of vitamin C treatment cannot be predicted.
Finally, the authors report that, following DHA uptake, NAD+ depletion by PARP activation contributes to the inhibition of glycolysis (and potentially to the stimulation of oxidative PPP flux). The observation that PARP inhibition partly rescues vitamin C-treated cells may suggest that the toxic effect of DHA uptake is not caused by ROS alone, since restoring NAD+ levels and glycolysis with the PARP inhibitor may actually decrease PPP flux and NADPH production, and aggravate the redox stress. It remains to be demonstrated that PARP inhibition indeed restores NAD+ levels in vitamin C-treated cells, and how this affects the balance between energy and redox metabolism. This also raises the question whether PARP activity in BRCA1/2-deficient tumors produces a similar metabolic phenotype via NAD+ depletion and whether the use of a PARP inhibitor (e.g., olaparib) to treat these tumors10 might restore NAD+ levels and counterbalance GAPDH inhibition by other oxidative agents.
In summary, Yun et al.1 show that, in glycolysis-addicted KRAS and BRAF driven cancer cells, high-dose vitamin C treatment induces cell death via the uptake and reduction of its oxidized form DHA back to vitamin C. DHA reduction, through scavenging GSH, induces oxidative stress, leading to GAPDH inactivation, inhibition of glycolysis and the subsequent energy crisis and cell death. This study further elucidates the mechanism by which ROS can induce cell death, and neatly shows how vitamin C, an antioxidant, can work as a double edged sword. However, further work is necessary to determine whether there is a therapeutic potential for vitamin C in cancer patients.
References
- Yun J, Mullarky E, Lu C, et al. Science 2015; 350:1391–1396. [DOI] [PMC free article] [PubMed]
- Vera JC, Rivas CI, Fischbarg J, et al. Nature 1993; 364:79–82. [DOI] [PubMed]
- Spielholz C, Golde DW, Houghton AN, et al. Cancer Res 1997; 37:2529–2537. [PubMed]
- Bohndiek SE, Kettunen MI, Hu DE, et al. J Am Chem Soc 2011; 133:11795–11801. [DOI] [PMC free article] [PubMed]
- Thomas LD, Elinder CG, Tiselius HG, et al. JAMA Intern Med 2013; 173:386–388. [DOI] [PubMed]
- Jacobs C, Hutton B, Ng T, et al. Oncologist 2015; 20:210–223. [DOI] [PMC free article] [PubMed]
- Agus DB, Gambhir SS, Pardridge WM, et al. J Clin Invest 1997; 100:2842–2848. [DOI] [PMC free article] [PubMed]
- May JM. Front Biosci 1998; 3:d1–d10. [DOI] [PubMed]
- Agus DB, Vera JC, Golde DW. Cancer Res 1999; 59:4555–4558. [PubMed]
- O'Connor MJ. Mol Cell 2015; 60:547–560. [DOI] [PubMed]