Abstract
Subchondral fracture of the femoral head is an uncommon and underdiagnosed affection. The abrupt or gradual onset of groin pain with functional disability on weight-bearing that improves with a resting period should alert the orthopedic surgeon to the possibility of this diagnosis. The differential diagnosis from osteonecrosis of the femoral head can be provided by assessing the different patterns of bone edema on MRI studies of the hip, thus avoiding unnecessary invasive operations on the hip.
Keywords: Osteonecrosis/diagnosis; Femur head/abnormalities; Magnetic resonance imaging/methods; Fractures, spontaneous/diagnosis; Hip fractures/radiography
INTRODUCTION
With so many names found in the literature to describe pain syndromes of the hip, one can predict that none of them is adequate or that they are all synonymous.
It is still unclear whether subchondral fracture, transient osteoporosis, transitory demineralization, transient osteolysis, algodystrophy of the hip, and bone marrow edema syndrome are different disorders, and many of these names predate the advent of MRI.
Transient osteoporosis was first described in 1959 in pregnant women, gradual improvement within a few months after delivery has been reported(1), and has since been described in other joints and in middle-aged men with incapacitating pain that fully improved in six to 12 months with load relief(2).
Some authors have suggested that transient osteoporosis is a form of reflex sympathetic dystrophy of the hip(2). Others believe that transient osteoporosis and the subchondral fracture are different spectra of the same disease; a fracture line is observed in the subchondral fracture(3). Subchondral fractures may be associated with the appearance of transient bone marrow edema syndrome/transient osteoporosis3, 4, 5, 6.
In contrast, avascular necrosis of the femoral head and subchondral fracture have some similar features, but its evolution and treatment are completely different, making its correct diagnosis essential.
Osteonecrosis of the femoral head has an uncertain pathophysiology, coursing with early medullary congestion and edema(7). It leads to incapacitation in proportion to pain, worsening progressively with load and even at rest(8). Ten percent are idiopathic and 80% are mainly caused by excessive use of alcohol and the use of steroids. The peak incidence is between the third and fifth decades of life, with no gender predilection. Approximately 50% of cases affect both hips(8).
Transient osteoporosis is an uncommon and self-limiting entity, ranging from six to 36 months2, 8, 9, 10, 11. Its etiology is unknown, with the only known risk factor being pregnancy(8). It courses with disabling pain with no history of trauma, worsening with walking and mobilization of the affected hip8, 9. It affects three times as many middle-aged men than women and pregnant women in the third trimester. Three temporal phases can be distinguished in its pathogenesis: the initial (lasting approximately one month), the plateau (lasting one to two months) and the regression (lasting about four months)(8).
DIAGNOSIS
The clinical picture of acute or insidious pain, especially in the groin, but also in the buttock or the anterior thigh(9), which worsens with walking and improves with the load relief in the absence of predisposing factors for osteonecrosis of the femoral head or antecedent trauma in patients of middle age, should indicate the possibility of the diagnosis of subchondral fracture of the femoral head.
Radiography in the early stage of osteonecrosis of the femoral head, transient osteoporosis, and subchondral fracture does not register changes, requiring magnetic resonance imaging analyzed by an experienced radiologist.
The diagnosis of osteonecrosis of the femoral head is made by MRI7, 12 and the area of osteonecrosis is characterized by a crescent format, with a geographic aspect, in the anterosuperior subchondral region of the femoral head. It is surrounded by a reactive interface with low external signal (sclerosis) and high internal signal on T2-weighted sequences(13). This area of hyperintensity represents hyperemia and granulation tissue at the interface between viable and devitalized bone (Figure 1), the standard double line sign that is definitive diagnosis of osteonecrosis(14) (Figure 2).
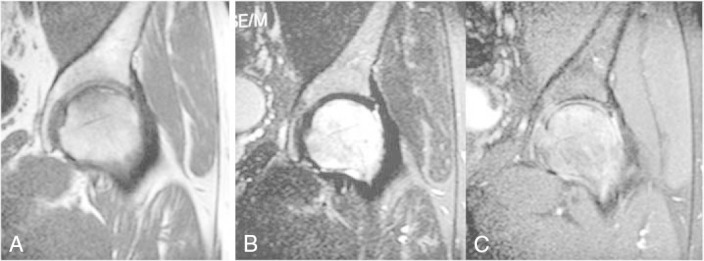
Figure 1.
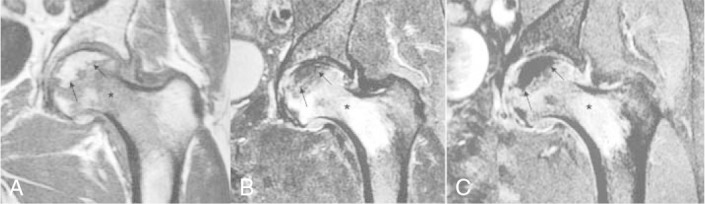
Osteonecrosis (arrow) characterized by crescentshaped area in a coronal T1 (a). T2 sequence with fat saturation (b) is surrounded by a double line sign (central hyperintense and peripheral hypointense signal). In the post-contrast T1 phase with fat saturation (c), the area of necrosis shows no enhancement, persisting with very low signal. The bone marrow edema (*) is characterized by an intermediate signal on T1, and hyperintense on the T2 and on the post-contrast phase.
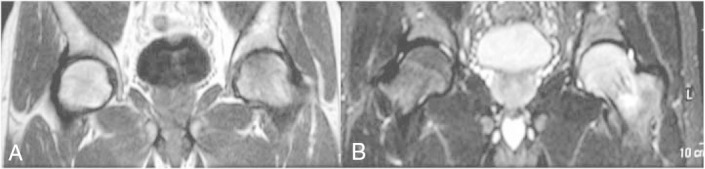
Figure 2.
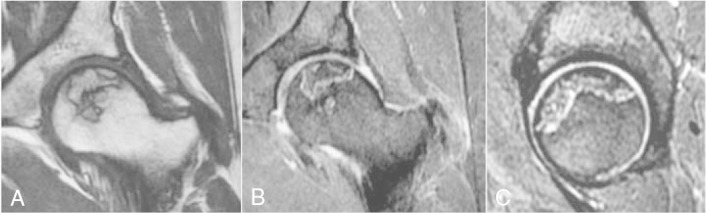
Osteonecrosis in a chronic phase (*), characterized by a serpiginous subchondral area across the upper portion of the femoral head. It presents a sclerotic coronal T1 halo (a), the double line sign on T2 with fat saturation in the coronal (b) and sagittal (c) images – a central hyperintense signal (white arrow) and peripheral hypointense signal (black arrow). There are no signs of bone marrow edema or collapse.
The area of necrosis initially shows high T1 signal intensity, but the signal can then be replaced by liquid or sclerosis(15). The most important factor in the prognosis of osteonecrosis is the estimated percentage of compromised load surface(16) (Figure 3).
Figure 3.
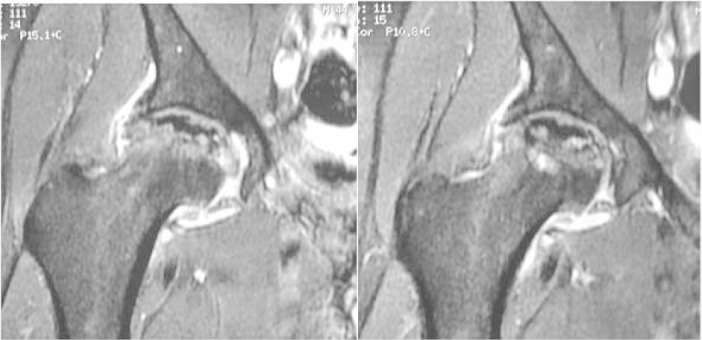
Osteonecrosis with collapse and secondary osteoarthritis. Coronal post-contrast T1 with fat saturation. The area of necrosis (*) has a very low signal, because it does not show enhancement. There is loss of sphericity (white arrows), extensive marginal osteophytic formation both in the acetabulum and femoral head, associated with joint and synovial effusion (black arrow).
In transient osteoporosis, MRI is the examination of choice for early diagnosis8, 11, 12, showing hypointense signal on T1 and hyperintense signal on T2 in the head and neck of the femur and, occasionally, the acetabulum9, 10, 12, 17 (Figures 4, 5, and 6). Unlike osteonecrosis, there is no bone erosion or subchondral collapse (Figure 7).
Figure 4.
MAF, male. Subchondral fracture (black arrow) in the anterior-superior portion of the left femoral head. It is characterized by a linear trace with low serpiginous signal parallel to the articular surface in the coronal T1 (a), T2 with fat saturation in the coronal (b) and sagittal (c) images. Extensive bone marrow edema (*) and joint effusion (white arrow).
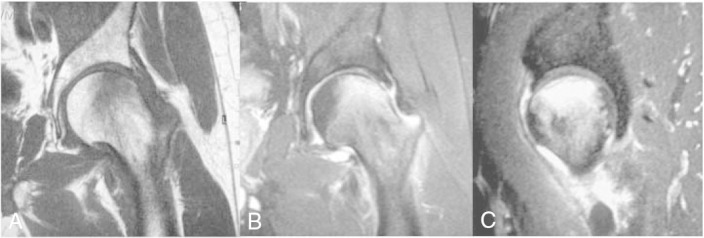
Figure 5.
MJC, male, April 2007. Subchondral fracture (arrow) in the superior left femoral head, associated with bone marrow edema (*). Coronal T1 (a), T2 with fat saturation (b) and post-contrast T1 with fat saturation (c).
Figure 6.
MJC, male, March 2007. Fine subchondral fracture line (arrow) best seen on a coronal T1-weighted image (a). Extensive bone marrow edema (*) in the femoral head extending to the intertrochanteric region characterized by hyperintensity on T2 with fat saturation (b). There are no signs of collapse.
Figure 7.

ARL, male, October 2007. Front (a) and lateral (b) radiographic study. Radiography of control with no signs of collapse or osteonecrosis. Joint space preserved.
The subchondral fracture is characterized by a subchondral, linear or slightly serpiginous thin trace of low signal intensity on all sequences paralleling the articular surface(18). It is associated with bone marrow edema extending to the femoral neck.
TREATMENT
Several treatments are possible in cases of osteonecrosis, from the conservative with medication for symptoms and load relief to decompression, proximal femur osteotomy, autogenous bone graft or allograft, vascularized fibular grafting with microsurgical technique and arthroplasty. The most commonly used treatment for the early stages of osteonecrosis is the decompression of the femoral head, which aims to reduce the intraosseous pressure and normalize the blood flow, leading to pain relief(4).
It has been reported that conservative treatment of transient osteoporosis, consisting of anti-inflammatory medication and load relief, allows for the resolution of the clinical and radiological picture2, 19.
From January 2006 to December 2007 seven consecutive patients with a diagnosis of subchondral fracture of the femoral head were evaluated, treated by the Hip Surgery Group, at Santa Casa de Misericórdia, ≪rnandinho Simonsen Pavilion≫, São Paulo, with ages ranging from 37 to 60 years (mean 50 years). The main symptom was pain in the groin, present from two to 16 weeks (average of eight weeks) before the first consultation. We analyzed six male patients (86%) and one female patient (14%), five of which were the left hip (71.4%) and two were the right (28.6%). None of the patients reported severe traumatic antecedents.
All were evaluated clinically and had front pelvis and lateral hip joint radiographs taken of the affected hip, as well as magnetic resonance imaging (MRI) of the hip in the pre- and post-treatment periods. The control MRI of the affected hip was performed every four weeks to observe the improvement of medullary edema.
The complete absence of pain in the affected hip was considered a criterion for clinical improvement, as a criterion for load relief of the affected hip, with the overall improvement of medullary edema demonstrated by MRI.
The time between the onset of pain and the diagnosis of subchondral fracture ranged from two to 16 weeks (average of eight weeks). In all cases, treatment was performed with load relief on the hip with axillary crutches and non-standard symptomatic medication for 24 to 30 weeks (mean 27.3 weeks). Follow-up ranged from 13 to 20 months (mean 15.5 months). Pain resolved gradually over a period ranging from nine to 10 months (mean 9.7 months) from the time of clinical onset. No patient underwent decompression. The resolution of bone marrow edema was observed in the control MRI performed every four weeks.
This study evaluated only seven patients. However, the cases were consecutive, and that is a rare entity. More importantly, in all cases we performed the differential diagnosis and used conservative treatment. Moreover, its true incidence may be higher, because of the misdiagnosis of osteonecrosis as subchondral fracture in many cases, both by the radiologist and orthopedic surgeon.
The role of the radiologist is as important as that of an orthopedist in the differentiation of these diseases. Very often, we observe the radiologist naming the condition as avascular osteonecrosis. After the diagnosis of osteonecrosis, it is important to define the extent of necrosis, if there is collapse of the femoral head and secondary osteoarthritis, whereas if it is defined as subchondral fracture, immediate load relief is the most important.
The diagnostic confusion causes errors indicating decompression. Often, cases of subchondral fracture are treated as if they were osteonecrosis, improving without collapse or deformity(5), and are erroneously counted as osteonecroses with good evolution, leading many orthopedic surgeons to believe that decompression is a salvaging technique. Until it is diagnosed and load relief implemented in these hips, the patients do not improve.
Correct diagnosis of subchondral fracture of the femoral head, which improves slowly, though spontaneously, avoids invasive measures in the affected hip. The misdiagnosis of osteonecrosis of the femoral head can be avoided by recognizing the differences and characteristics of subchondral fractures of the femoral head on MRI.
Footnotes
Acknowledgement: To Denise Tokechi Amaral, Medimagem Radiologist of the Hospital Beneficência Portuguesa de São Paulo
Study conducted at the Hip Surgery Group, Department of Orthopedics and Traumatology, School of Medical Sciences, Santa Casa de Misericórdia de São Paulo, “Simonsen Fernandinho Pavilion” (DOT-FCMSCSP). Director Prof. Dr. Osmar Avanzi.
We declare no conflict of interest this article.
REFERENCES
- 1.Curtiss PH, Jr, Kincaid WE. Transitory demineralization of the hip in pregnancy. A report of three cases. J Bone Joint Surg Am. 1959;41:1327–1333. [PubMed] [Google Scholar]
- 2.Froberg PK, Braunstein EM, Buckwalter KA. Osteonecrosis, transient osteoporosis, and transient bone marrow edema: current concepts. Radiol Clin North Am. 1996;34(2):273–291. [PubMed] [Google Scholar]
- 3.Kim JW, Yoo JJ, Min BW, Hong SH, Kim HJ. Subchondral fracture of the femoral head in healthy adults. Clin Orthop Relat Res. 2007;(464):196–204. doi: 10.1097/BLO.0b013e3181577212. [DOI] [PubMed] [Google Scholar]
- 4.Mitchell DG, Joseph PM, Fallon M, Hickey W, Kressel HY, Rao VM. Chemical shift MR imaging of the femoral head: an in vitro study of normal hips and hips with avascular necrosis. AJR Am J Roentgenol. 1987;148(6):1159–1164. doi: 10.2214/ajr.148.6.1159. [DOI] [PubMed] [Google Scholar]
- 5.Mitchell DG, Rao VM, Dalinka MK, Spritzer CE, Alavi A, Steinberg ME. Femoral head avascular necrosis: correlation of MR imaging, radiographic stanging, radionuclide imaging, and clinical findings. Radiology. 1987;162(3):709–715. doi: 10.1148/radiology.162.3.3809484. [DOI] [PubMed] [Google Scholar]
- 6.Lieberman JR, Berry DJ, Mont MA, Aaron RK, Callaghan JJ, Rajadhyaksha AD. Osteonecrosis of the hip: management in the 21st century. Instr Course Lect. 2003;52:337–355. [PubMed] [Google Scholar]
- 7.Davies M, Cassar-Pullicino VN, Darby AJ. Subchondral insufficiency fractures of the femoral head. Eur Radiol. 2004;14(2):201–207. doi: 10.1007/s00330-003-1998-1. [DOI] [PubMed] [Google Scholar]
- 8.Yamamoto T, Bullough PG. Subchondral insufficiency fracture of the femoral head. A differential diagnosis in acute onset of coxarthrosis in the elderly. Arthritis Rheum. 1999;42(12):2719–2723. doi: 10.1002/1529-0131(199912)42:12<2719::AID-ANR31>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- 9.Yamamoto T, Schneider R, Bullough PG. Subchondral insufficiency fracture of the femoral head: histopathologic correlation with MRI. Skeletal Radiol. 2001;30(5):247–254. doi: 10.1007/s002560100348. [DOI] [PubMed] [Google Scholar]
- 10.Hayes CW, Conway WF, Daniel WW. MR imaging of bone marrow edema pattern: transient osteoporosis, transient bone marrow edema syndrome, or osteonecrosis. Radiographics. 1993;13(5):1001–1011. doi: 10.1148/radiographics.13.5.8210586. [DOI] [PubMed] [Google Scholar]
- 11.Bloem JL. Transient osteoporosis of the hip: MR imaging. Radiology. 1988;167(3):753–755. doi: 10.1148/radiology.167.3.3363135. [DOI] [PubMed] [Google Scholar]
- 12.Turner DA, Templeton AC, Selzer PM, Rosenberg AG, Petasnick JP. Femoral capital osteonecrosis: MR finding of diffuse marrow abnormalities without focal lesions. Radiology. 1989;171(1):135–140. doi: 10.1148/radiology.171.1.2928517. [DOI] [PubMed] [Google Scholar]
- 13.Hofmann S, Engel A, Neuhold A, Leder K, Kramer J, Plenk H., Jr Bone-marrow oedema syndrome and transient osteoporosis of the hip. An MRI-controlled study of treatment by core decompression. J Bone Joint Surg Br. 1993;75(2):210–216. doi: 10.1302/0301-620X.75B2.8444939. [DOI] [PubMed] [Google Scholar]
- 14.Guerra JJ, Steinberg ME. Distinguishing transient osteoporosis from avascular necrosis of the hip. J Bone Joint Surg Am. 1995;77(4):616–624. doi: 10.2106/00004623-199504000-00017. [DOI] [PubMed] [Google Scholar]
- 15.Rafii M, Mitnick H, Klug J, Firooznia H. Insufficiency fracture of the femoral head: MR imaging in three patients. AJR Am J Roentgenol. 1997;168(1):159–163. doi: 10.2214/ajr.168.1.8976940. [DOI] [PubMed] [Google Scholar]
- 16.Lafforgue P, Dahan E, Chagnaud C, Schiano A, Kasbarian M, Acquaviva PC. Early-stage avascular necrosis of the femoral head: MR imaging for prognosis in 31 cases with at least 2 years of follow-up. Radiology. 1993;187(1):199–204. doi: 10.1148/radiology.187.1.8451413. [DOI] [PubMed] [Google Scholar]
- 17.Yamamoto T, Schneider R. Bullough PG. Subchondral insufficiency fracture of the femoral head: histopathologic correlation with MRI. Skeletal Radiol. 2001;30(5):247–254. doi: 10.1007/s002560100348. [DOI] [PubMed] [Google Scholar]
- 18.Takatori Y, Kokubo T, Ninomiya S, Nakamura S, Morimoto S, Kusaba I. Avascular necrosis of the femoral head. Natural history and magnetic resonance imaging. J Bone Joint Surg Br. 1993;75(2):217–218. doi: 10.1302/0301-620X.75B2.8444940. [DOI] [PubMed] [Google Scholar]
- 19.Wilson AJ, Murphy WA, Hardy DC, Totty WG. Transient osteoporosis: transient bone marrow edema? Radiology. 1988;167(3):757–760. doi: 10.1148/radiology.167.3.3363136. [DOI] [PubMed] [Google Scholar]


