Abstract
To assess the outcomes of the surgical treatment of extensive rotator cuff injuries through arthroscopy. Methods: Between June 1998 and October 2006, 61 patients with extensive rotator cuff injuries and submitted to surgical arthroscopy technique by the Shoulder and Elbow Group of the Department of Orthopaedics and Traumatology, Santa Casa de Misericórdia Medical School were reassessed. The study included all patients with at least two tendons affected or with retraction at least on two tendons up to the glenoidal cavity edge and with at least 12 months of follow-up. Results: According to UCLA's evaluation criteria, 54 (89%) patients showed excellent or good outcomes; no fair outcome in none of the patients; and seven (11%) poor outcomes. A satisfaction rate of 92% was reported. Postoperative joint motion went from a mean lifting value of 93° to 141°, the mean lateral rotation went from 32° to 48° and the mean medial rotation went from L1 to T10. These differences were regarded as statistically significant. Conclusion: The arthroscopic repair of extensive rotator cuff injuries leads to satisfactory outcomes for most of the patients, with a high satisfaction degree.
Keywords: Rotator cuff, Arthroscopy/method, Evaluation studies
INTRODUCTION
The term “extensive lesions of the rotator cuff” (ELRC) has been widely used to identify large lesions whose repair is particularly difficult, and so the prognosis is uncertain. Hawkins et al. define as extensive the lesions exceeding five centimeters in length(1). Due to the variation in the size of patients and measurement techniques, Gerber et al. believe that it is appropriate to define the size in terms of the number of tendons involved in the lesion, classifying as extensive those involving at least two tendons(2).
ELRC evolve especially in young patients with high functional disability, loss of lifting strength and chronic pain; medical treatment does not usually lead to good results(3).
Open repair of rotator cuff injuries can lead to complications widely discussed in literature, such as damage to the deltoid muscle, arthrofibrosis, and residual pain(4), which are difficult to correct in the postoperative period. The hybrid technique using arthroscopic acromioplasty and suture of the injury by mini-incision is another treatment option, though it is not without complications5, 6. Arthroscopy has been settled upon as the option for the treatment of these lesions because it combines maximum visualization of the joint with minimal tissue damage(4). Patients undergoing arthroscopic suture of rotator cuff injuries have less pain in the postoperative period and a faster return of function and to activities of daily living7, 8.
Repairing ELRC can be technically challenging due to the retraction of the tendon stumps, bursal fibrosis, muscular atrophy, and fatty degeneration of the muscles(9). Due to these characteristics, extensive lesions are eventually called “irreparable”, which does not always reflect reality.
Treatment options for these extensive lesions of the rotator cuff are: conservative treatment, joint debridement with tenotomy of the long head tendon of the biceps brachii, reconstruction with homograft, transfer of the shoulder girdle muscles, partial or even complete rotator cuff repair attempts whenever possible, and reverse shoulder arthroplasty in exceptional cases10, 11, 12, 13, 14. When proper mobilization techniques are employed, the vast majority of these injuries can be completely or partially repaired9, 11, 15, 16.
The objective of this study is to evaluate the results of arthroscopic surgical treatment of “extensive lesions” of the rotator cuff.
METHODS
From June 1998 to October 2006, 71 patients with extensive lesions of the rotator cuff underwent arthroscopic surgery; from this total, 61 were reassessed by the Shoulder and Elbow Group, Department of Orthopedics and Traumatology, School of Medical Sciences, Santa Casa de São Paulo, “Fernandinho Simonsen Pavilion”. Inclusion criteria in this study were patients with rotator cuff injuries involving more than two tendons or retraction of at least two of the tendon stumps to the top edge of the glenoid cavity, identified by preoperative magnetic resonance imaging or during the arthroscopic procedure. Exclusion criteria were patients undergoing arthroscopic surgery for lesions that affected only one tendon or if retraction of the tendons did not reach the level of the glenoid, or those who had less than 12 months of postoperative follow-up (Table 1).
Twenty-seven of the patients were male (44%) and 34 were female (56%). The average age was 64 years and four months, ranging from 45 to 82 years. The duration of pain preoperatively ranged from one week to 192 months, with an average of 30 months and 10 days. The dominant side was affected in 51 (84%) cases. Among the lesions, 42 (69%) were due to trauma or physical stress on the shoulder. Of the affected patients, 25 (41%) were playing sports that used the upper limb.
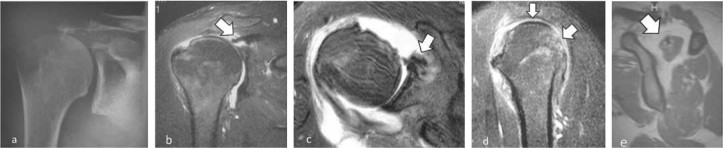
The preoperative joint mobility was assessed by the parameters described by Hawkins and Bokos(17). Elevation ranged from 0° to 160° with an average of 92°, lateral rotation ranged from 0° to 90°, averaging 32°; and the medial rotation evaluated according to the vertebral level reached by the patient with her/his thumb ranged from the ipsilateral greater trochanter to T7, with an average of L1. Not all patients underwent magnetic resonance imaging in the preoperative period, especially the first patients in the series. All patients underwent surgery in the beach chair position under general anesthesia in combination with a brachial plexus block. All patients underwent intra-articular inspection in which the associated lesions were seen. Where injury to the tendon of the long head of biceps was observed, tenotomy was performed, followed by tenodesis, prior to cuff repair. After intra-articular inspection, subacromial inspection was performed, and the lesions were classified according to the inclusion criteria. After the debridement of soft tissue, tendon mobilization and preparation of the bone bed of the greater tubercle, the suture was made with the use of anchors, tendon to tendon stitches, or a combination of these techniques. Tenodesis of the long head tendon of the biceps, acromioplasty, and resection of the distal clavicle were associated procedures that were considered as required (Figures 1 and 2).
Figure 1.
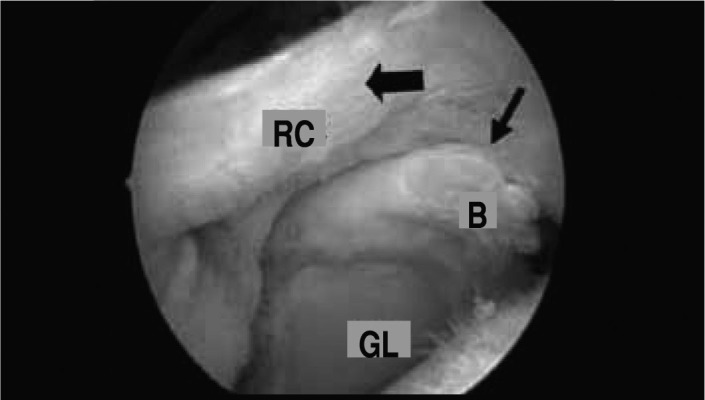
Intraoperative arthroscopic surgical image for the repair of extensive lesion to the rotator cuff (RC) with vision through the lateral portal: large arrow – edge of the RC lesion at the height of the edge of the glenoid cavity (GL); thin arrow – origin of the long head tendon of the biceps (B) submitted to tenotomy.
Figure 2.
Intraoperative surgical image for the repair of extensive lesion to the rotator cuff (RC) in the greater tubercle (GT) via arthroscopy through the posterior portal showing the stitches made in the suture of the lesion (arrow). Repairs carried out with 3 anchors and 6 stitches. (A = acromion)
Of the patients, 39 (64%) had lesions that totally or partially affected the insertion of the subscapularis muscle tendon. Acromioplasty was performed in 52 (85%) patients and resection of the distal end of the clavicle was performed in 18 (29%). Tenodesis of the long head tendon of the brachial biceps muscle was performed in 20 (32%) patients. In 13 (21%) patients, tenodesis was performed at the suture of the rotator cuff injury, and a biotenodesis interference screw (Arthrex®) was used in seven (11%). Eight (13%) patients underwent only the tenotomy of the long head tendon of the brachial biceps muscle, since it was probably already attached to the intertubercular groove; in eight patients (13%), this tendon was absent during joint inspection.
Suturing of the lesion was performed by means of anchors in all patients, the number used ranged from one to five, averaging three. The number of stitches ranged from four to 12, with an average of seven. In 50 cases, tendon to tendon stitches were also made to approximate the edges of the lesion prior to suturing to the bone, with an average of two tendon to tendon stitches, ranging from one to four stitches. In two cases it was impossible to complete suturing of the tendon to the bone, and the “suspension bridge” principle was then used for the partial repair(11).
The average postoperative period of immobilization with a functional sling was seven weeks, ranging from four to 12 weeks.
In the postoperative period, patients were clinically reevaluated using the method of the University of California at Los Angeles (UCLA) and joint mobility was evaluated by the parameters described by Hawkins and Bokos(17).
Statistical analysis was performed using the Wilcoxon signed rank test to evaluate the possible differences between two moments of observation for the variables of interest, and Spearman correlation analysis to study the level of relationship between pairs of variables. We adopted a significance level of 5% (0.05) for the statistical tests.
RESULTS
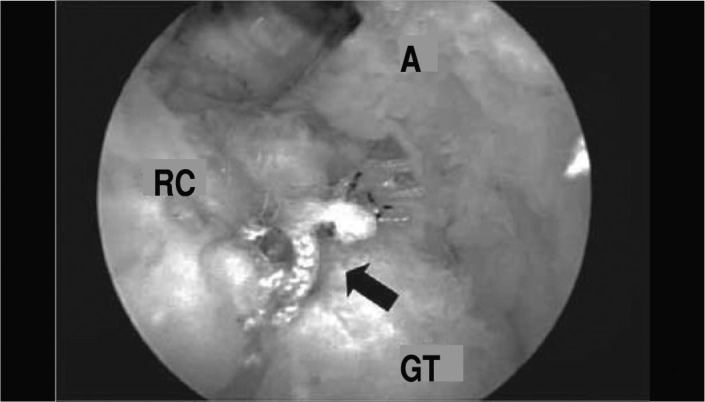
When evaluating the results of the 61 operated patients, we obtained an average score (UCLA) of 31.2 (six to 35 points). Sixty-seven percent of cases were considered excellent and 22% were considered good. In 11% of cases, with UCLA scores from six to 20, the result was considered poor and in no case was it considered fair (Figures 3 and 4).
Figure 3.

Patient (case 60) in the postoperative period 23 months after repair of extensive rotator cuff lesion of the right shoulder, with good results: a – active elevation, b – active lateral rotation.
Figure 4.
Preoperative imaging studies of patient (case 60) with extensive rotator cuff lesion (RC): a – anteroposterior radiograph shows the rise of the humeral head, b – resonance imaging (MRI) in the coronal T2 slice shows retraction of the supraspinatus tendon to the edge of the glenoid cavity (arrow) and the rise of the humeral head; c – axial T2 MRI, injury to the subscapularis tendon (arrow), d – sagittal T2 MRI, RC lesion including the supraspinatus and infra-spinal tendons (arrows), e – sagittal T1 MRI, fatty degeneration greater than 50% of the supraspinatus muscle (arrow).
The average range of motion in the postoperative evaluation was 141° of elevation, ranging from 45° to 160°, an external rotation of 48°, from 0° to 80°, and a medial rotation of T10, from L5 to T5. The mean follow-up period was around 36 weeks, ranging from 12 to 108 months.
Age, presence of trauma or stress, and associated acromioplasty did not show statistically significant correlation with the outcome. Patients with lesions of the subscapularis had greater gain in medial rotation (one level) compared to those with an intact subscapularis, but this difference was not statistically significant.
Complications were observed in nine patients (15%), such as tendon suture dehiscence, found in five cases, rotator cuff arthropathy in two cases, and adhesive capsulitis in two others.
DISCUSSION
The treatment of extensive lesions is controversial, especially regarding the technique to be used. Treatment options vary greatly, from non-surgical, open debridement associated with subacromial decompression, arthroscopic debridement with or without subacromial decompression, partial rotator cuff repair, open repair, repair by the mini-incision technique, arthroscopic repair, biceps tenotomy, and combined techniques7, 10, 11, 12, 13, 15, 18, 19, 20, besides more recently being able to use the reverse prosthesis(14).
The size of the ELRC is not the only factor to be considered in choosing the method of treatment. The mobility and the quality of tendons and their corresponding muscle bellies are important factors for assessing the possibility of repair of these lesions(3).
Bigliani et al.(9) obtained 85% good and excellent results in the open surgical treatment of extensive lesions of the rotator cuff and stressed the importance of the integrity of the deltoid muscle for the rehabilitation program. In contrast, Bennett(10) observed a rate of 95% satisfactory results with arthroscopic treatment of ELRC in a prospective study with two to four years of follow-up and found no statistically significant difference between lesions with or without the involvement of the subscapularis tendon.
In 2001, Burkhart(18) highlighted the advantage of visualization of the lesion by arthroscopy and recognition of its format in employing closing techniques, usually by the convergence of margins with or without associated tendon-bone repair, achieving 92% good and excellent results. Similarly, Jones and Savoie(12) had 88% good and excellent results in a prospective study of 60 patients, with ratings of satisfaction in 98% of cases.
More recently, other authors have published studies using arthroscopic release of the rotator interval for better mobilization of retracted tissues and found satisfactory results in preliminary studies9, 21.
Our results were excellent or good in most cases, reaching around 89% (54 shoulders), a value similar to our results in previous studies with open operation and mini-incision. In active movement, there was a 52° average increase in anterior elevation and 16° in lateral rotation. As for internal rotation, there was an average increase of four vertebral levels in the joint motion. The increase in these three directions of range of motion was statistically significant.
It was not possible to perform closure of the entire lesion in two patients, who were treated with the partial repair advocated by Burkhart(11) and still yielded satisfactory results (cases 47 and 55). Another patient (case 3) had suture dehiscence with three years of postoperative follow-up after a traumatic episode of anterior dislocation of the shoulder, but chose not to re-operate and evolved favorably with a UCLA score of 34.
We found poor results in seven patients (11%). Two of these (cases 24 and 43) evolved with suture dehiscence. One patient (case 27) did not follow medical guidelines, removing the immobilization before the recommended time. Another patient (case 44), a carrier of hepatitis C and with a depressive psychological profile, developed adhesive capsulitis, and poor results persist even after treatment with serial anesthesia of the suprascapular nerve. Evidently, and according to Boileau et al.(22), we know that the rate of open or arthroscopic suture dehiscence of the rotator cuff is greater than evidenced by us. This is primarily due to the lack of postoperative MRI images for all of our patients, due to either economic limitations or the patient's refusal to perform the exam. Only those patients who developed unsatisfactorily underwent such examination (Figure 5).
Figure 5.
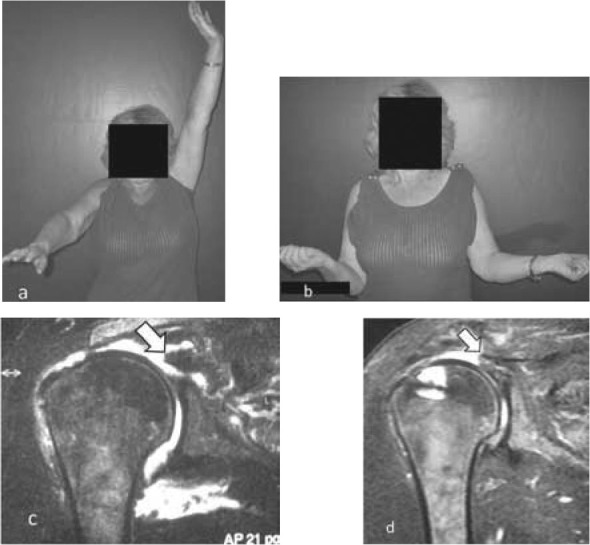
Patient (case 43) 57 months into the postoperative period (PO) for arthroscopic repair of extensive rotator cuff injury with poor outcome: a – active elevation, b – active lateral rotation, c – preoperative MRI: retraction of the lesion to the edge of the glenoid cavity is observed (arrow), d – PO MRI: re-rupture of the rotator cuff (arrow).
In addition to the four patients mentioned above, we found two more unsatisfactory results in cases 6 and 37, which evolved with arthropathy post rotator cuff injury. Reverse arthroplasty was indicated in both, but was performed in only one case.
We obtained pain relief in 87% of cases, with satisfaction ratings of approximately 92%, demonstrating the effectiveness of arthroscopic surgery for extensive lesions of the rotator cuff.
As for postoperative immobilization, patients were usually given a functional sling (in abduction and neutral rotation of the shoulder) for about six to eight weeks, doing passive exercises for the brachial biceps. One patient removed the sling after only four weeks and ended up having a very poor surgical outcome. Another case was a patient who developed adhesive capsulitis, and because of pain, was unable to remove the sling and remained immobilized for 12 weeks.
CONCLUSION
The arthroscopic treatment of extensive lesions of the rotator cuff leads to 89% excellent and good results and provides an increased range of shoulder movement.
Footnotes
Study conducted at the Department of Orthopedics and Traumatology, School of Medical Sciences, Santa Casa de São Paulo, “Fernandinho Simonsen Pavilion”.
We declare no conflict of interesti this article.
REFERENCES
- 1.Hawkins RJ, Misamore GW, Hobeika PE. Surgery for full thickness rotator-cuff tears. J Bone Joint Surg Am. 1985;67(9):1349–1355. [PubMed] [Google Scholar]
- 2.Gerber C, Fuchs B, Hodler J. The results of repair of massive tears of rotator cuff. J Bone Joint Surg Am. 2000;82(4):505–515. doi: 10.2106/00004623-200004000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Checchia SL, Doneux Santos P, Miyazaki NA, Fregoneze M, Silva LA, Mussi Filho S, Faria AC, Ribeiro Junior GFF. Tratamiento cirúrgico das lesões extensas do manguito rotador pela via de acesso deltopeitoral. Rev Bras Ortop. 2003;38(5):252–260. [Google Scholar]
- 4.Checchia SL, Doneux Santos P, Miyazaki AN, Fregoneze M, Silva LA, Ishi M, Braga SR, Nascimento LG. Avaliação dos resultados obtidos na reparação artroscópica das lesões do manguito rotador. Rev Bras Ortop. 2005;40(5):229–238. [Google Scholar]
- 5.Miyazaki AN, Doneux Santos P, Saito RY Kussakawa D, Checchia SL. Acromioplastia por via artroscópica e reparo das lesões do manguito rotador por “miniincisão”. Rev Bras Ortop. 1999;34(7):415–420. [Google Scholar]
- 6.Bittar ES. Arthroscopic management of massive rotator cuff tears. Arthroscopy. 2002;18(9 Suppl 2):104–106. doi: 10.1053/jars.2002.36512. [DOI] [PubMed] [Google Scholar]
- 7.Galatz LM, Ball CM, Teefey SA, Middleton WD, Yamaguchi K. The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am. 2004;86(2):219–224. doi: 10.2106/00004623-200402000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Rokito AS, Cuomo F, Gallagher MA, Zuckerman JD. Long-term functional outcome of repair of large and massive chronic tears of the rotator cuff. J Bone Joint Surg Am. 1999;81(7):991–997. doi: 10.2106/00004623-199907000-00012. [DOI] [PubMed] [Google Scholar]
- 9.Bigliani LU, Cordasco FA, Mcilveen SJ, Musso ES. Operative treatment of failed repair of massive rotator cuff. J Bone Joint Surg Am. 1992;74(10):1505–1515. [PubMed] [Google Scholar]
- 10.Bennett WF. Arthroscopic repair of massive rotator cuff tears: A prospective cohort with 2- and 4- year follow-up. Arthroscopy. 2003;19(4):380–390. doi: 10.1053/jars.2003.50131. [DOI] [PubMed] [Google Scholar]
- 11.Burkhart SS. Arthroscopic treatment of massive rotator cuff tears. Clin Orthop Relat Res. 2001;(390):107–118. doi: 10.1097/00003086-200109000-00013. [DOI] [PubMed] [Google Scholar]
- 12.Jones CK, Savoie FH., 3rd Arthroscopic repair of large and massive rotator cuff tears. Arthroscopy. 2003;19(6):564–571. doi: 10.1016/s0749-8063(03)00169-5. [DOI] [PubMed] [Google Scholar]
- 13.Tauro JC. Arthroscopic repair of large rotator cuff tears using the interval slide technique. Arthroscopy. 2004;20(1):13–21. doi: 10.1016/j.arthro.2003.10.013. [DOI] [PubMed] [Google Scholar]
- 14.Wall B, Nové-Josserand L, O'Connor DP, Edwards TB, Walch G. Reverse total shoulder arthroplasty: a review of results according to etiology. J Bone Joint Surg Am. 2007;89(7):1476–1485. doi: 10.2106/JBJS.F.00666. [DOI] [PubMed] [Google Scholar]
- 15.Lo IK, Burkhart SS. Arthroscopic repair of massive, contracted, immobile rotator cuff tears using single and double interval slides: technique and preliminary results. Arthroscopy. 2004;20(1):22–33. doi: 10.1016/j.arthro.2003.11.013. [DOI] [PubMed] [Google Scholar]
- 16.Burkhart SS, Athanasiou KA, Wirth MA. Margin convergence: A method of reducing strain in massive rotator cuff tears. Arthroscopy. 1996;12(3):335–338. doi: 10.1016/s0749-8063(96)90070-5. [DOI] [PubMed] [Google Scholar]
- 17.Hawkins RJ, Bokos DJ. Clinical evaluation of shoulder problems. In: Rockwood CA Jr, Matsen FA 3rd, editors. The shoulder. 2nd ed. Saunders; Philadelphia: 1998. pp. 175–180. [Google Scholar]
- 18.Burkhart SS. Partial repair of massive rotator cuff tears: The evolution of a concept. Orthop Clin North Am. 1997;28(1):125–132. doi: 10.1016/s0030-5898(05)70270-4. [DOI] [PubMed] [Google Scholar]
- 19.Snyder SJ, Murray TF, Lajtai G, Mileski RM. Arthroscopic repair of medium to large full-thickness rotator cuff tears: Outcome at 2- to 6-year follow up. J Shoulder Elbow Surg. 2002;11(1):19–24. doi: 10.1067/mse.2002.120142. [DOI] [PubMed] [Google Scholar]
- 20.Boileau P, Brassart N, Watkinson DJ, Carles M, Hatzidakis AM, Krishnan SG. Arthroscopic repair of full-thickness tears of the supraspinatus: Does the tendon really heal? J Bone Joint Surg. Am. 2005;87(6):1229–1240. doi: 10.2106/JBJS.D.02035. [DOI] [PubMed] [Google Scholar]
- 21.Walch G, Edwards TB, Boulahia A, Nove-Josserand L, Neyton L, Szabo I. Arthroscopic tenotomy of the long head of the biceps in the treatment of rotator cuff tears: Clinical and radiographic results of 307 cases. J Shoulder Elbow Surg. 2005;14(3):238–246. doi: 10.1016/j.jse.2004.07.008. [DOI] [PubMed] [Google Scholar]
- 22.Boileau P, Baque F, Valerio L, Ahrens P, Chuinard C, Trojani C. Isolated arthroscopic bíceps tenotomy or tenodesis improves symptoms in patients with massive irreparable rotator cuff tears. J Bone Joint Surg Am. 2007;89(4):747–757. doi: 10.2106/JBJS.E.01097. [DOI] [PubMed] [Google Scholar]