Abstract
To evaluate the functional evolution of knees after repair of longitudinal meniscal rupture with absorbable arrow implant. Methods: Between June 1997 and February 2001, 23 patients with a mean age of 26.3 years were evaluated. The mean follow-up time was 72.87 months (45-96). We performed 19 medial and 4 lateral meniscal repairs. The patients were pre and postoperatively evaluated regarding joint function according to the Lysholm scale, and, postoperatively, according to IKDC. Results: For better understanding, the 23 treated cases were divided into three groups. Twenty one had ACL injuries, eleven of whom were submitted to ligament reconstruction (Group I). All these 11 cases were regarded as satisfactory. The remaining 10 cases of the 21 with ACL lesion were not submitted to ligament reconstruction (Group II). Of these, 5 evolved satisfactorily, not requiring ligament reconstruction. The remaining five evolved with complaint of ligament instability, being all submitted to reconstruction. Four of these had an integral meniscus and one presented a failure of the medial meniscus. The remaining two cases who did not present ACL injury (Group III), one patient evolved satisfactorily and one developed a failure of the lateral meniscus. According to the Lysholm scale, preoperative mean score was 57.53 and the postoperative mean score was 86.95, evidencing a statistically significant improvement (Wilcoxon p < 0.01). The non-parametric ANOVA was employed for ordinal data with repeated measurements to assess pre- and postoperative measurements, considering Groups I and II. We assessed knee stabilization and found no statistically significant difference between Groups I and II (p = 0.648). Even if there were differences between the two groups, both had the same behavior. On postoperative assessment with IKDC, 4 patients were grade A, 13 were grade B, and 6 were grade C. Two C results were caused by a meniscal rupture. Conclusion: Of the 23 patients, only two presented known failures of the sutured meniscus. According to the Lysholm scale, there was a significant improvement in the treated patients. The ACL repair caused no bias on the results.
Keywords: Arthroscopy, Meniscal repair, Implants
INTRODUCTION
Several authors1, 2, 3 have examined the use of absorbable implants for the repair of longitudinal meniscal injuries. With implants, such repair is carried out without manipulating wires and knots, avoiding an additional incision, which makes the procedure completely arthroscopic, easier, and faster. This is the differential in relation to procedures without an implant. The first available implant for arthroscopic use was the arrow. It is in the form of a “T”, the major axis of which fixates the meniscus injury and the minor axis of which compresses it (Figure 1).
Figure 1.
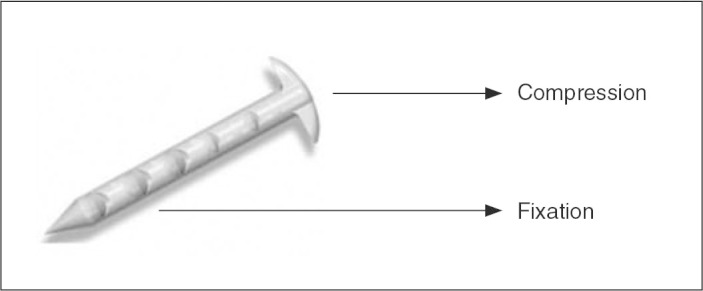
Arrow
Motivated by these advantages, we started using the arrow in 1997 in the repair of longitudinal meniscal injuries. The repair occurred in lesions observed during the reconstruction of the anterior cruciate ligament (ACL), but also in those presenting an intact ACL. Based on studies by Steenbrugge et al.(4), Hanks et al.(5), and Koukoulias and Papastergiou(6), who consider that instability does not contraindicate repair of the meniscus, there were situations where the repair of the meniscus was performed on patients with ACL injury, but refractory in carrying out ligament repair.
We reevaluated the cases submitted to meniscus repair performed exclusively with this type of implant, the arrow, and developed a retrospective study analyzing the functional evolution of patients in the medium-term. We also compared the group of patients with reconstructed ACL with the group with ACLs that remained untreated, to observe the influence of stability in the results.
METHODS
We reviewed the medical records and reevaluated all patients who had vertical meniscus lesions located in the vascularized area and repaired exclusively with absorbable arrow implants. Between June 1997 and February 2001, 26 patients with this type of lesion underwent surgery and 23 were reassessed.
Inclusion criteria
Longitudinal meniscal lesion, located between 3mm and 5mm distal to the synovial meniscal junction in a vascularized area with a length of 2cm to 4cm. All lesions were unstable on palpation. The lesions that were stable or with a length of less than 2cm were considered to be potentially healing and were not treated. No damage was greater than 60% of the circumference of the meniscus.
Exclusion criteria
Exclusion criteria were multiple lesions of the meniscus with deformities of the body located in the avascular area with capsulomeniscal detachment or those the joint fragment reduction of which required tension, were injured or irregular. Lesions repaired by the arrow but associated with another kind of fixation with sutures were also eliminated.
The implant
The arrow was used as the absorbable implant. It has a T-shaped body with a 1.1-mm diameter and a head 4 mm in length. The major axis has length of 10 mm, 13 mm, and 16 mm. It is indented on both sides, forming a right angle to the implant head. It consists of poly-L-lactic acid (PLA), the resorption of which takes 30 to 60 months. After September 2000, it began to be composed of a polymer with 96% PLA and 4% poly-DL-lactic acid. The latter composition was not used in this study.
Classification of individuals
For a better understanding of the study, we divided patients into three groups according to the integrity or repair of the ACL:
Group I (meniscal injury and ACL repair). This group includes patients with mechanical knee pain and that in the physical examination showed tenderness in the joint interline with Appley and McMurray signs, with complaints of frontal instability of the joint with an anterior drawer sign larger than 6 mm, compared with the contralateral knee evaluated by Rolimeter (Aircast). When submitted to arthroscopy, if a longitudinal meniscal lesion was observed, it would be repaired; if ACL injury was confirmed, the ACL would be rebuilt. The patients were aware of the ligament reconstruction technique and the possibility of meniscus repair. Group II (meniscal injury in an unstable knee). These patients showed signs of meniscal injury, with no complaints of instability, and using the Rolimeter (Aircast), showed an anterior drawer sign less than 6 mm compared with the contralateral knee. They were alerted to the instability and possible need for ligament reconstruction. Certain patients, for various reasons, did not agree to ligament reconstruction, but only to repair the meniscus. During arthroscopy, if ACL injury was observed to be associated with the longitudinal meniscal lesion, it would be repaired without repairing the ligament injury, making these individuals the focus of the study. Group III (meniscal injury in a stable knee). Patients with mechanical pain and tenderness in the joint interline with Appley and McMurray signs present and a stable knee. Patients underwent arthroscopy, but longitudinal meniscal injury would be treated with an arrow. All patients were aware of the possibility of repair.
SURGICAL TECHNIQUES
The patients underwent arthroscopy of the knee with use of a pneumatic tourniquet and a leg holder. We used the anterolateral and anteromedial portals. All patients underwent arthroscopic evaluation, observing the integrity or damage to the menisci, cartilage, and ligaments. The meniscus lesion, once detected, was prepared by scraping its edges with a shaver. Bleeding was stimulated by drilling the parietal portion of the meniscus to the perimeniscal synovial tissue using an epidural needle. The reduction of the lesion was performed by aligning the edges without traction.
The transverse dimension of the likely extent of penetration of the implant in the articular portion to the meniscocapsular junction of the parietal edge of the meniscus was measured by determining the dimensions of the arrow. The lesion was fixed by a cannulated guide and the implants applied. The number of implants varied according to the visual impression of stabilization.
The patients with a symptomatic ACL injury who were willing to undergo ligament reconstruction underwent the procedure with patellar tendon or semitendinosus and gracilis tendon, according to preoperative planning.
Patients with partial or total ACL injury that did not agree to ligament reconstruction, but had this type of meniscal injury, had it repaired without the ligament procedure.
The patients were not immobilized, allowing for active movement between 0° and 90°. Walking was permitted with crutches without weight-bearing. After four days of surgery, isometric quadriceps exercises were started depending on the sensation of pain of each individual. After 40 days, treatment by physical therapy started with progressive increase of the load while walking.
Evaluation criteria
All were evaluated preoperatively and postoperatively using the Lysholm scale(7) and the results were statistically compared using the Wilcoxon test. For comparison between groups (I and II) and time (pre- and postoperative), a nonparametric ANOVA with ordinal repeated measures was performed. All were evaluated postoperatively by the (IKDC)(8). Symptomatic patients complaining of persistent pain, swelling and instability were evaluated by magnetic resonance imaging (MRI). Patients requiring a second arthroscopic procedure underwent joint reevaluation, considering the integrity of the meniscus and possible cartilaginous injuries. We conclude that asymptomatic patients should show some degree of healing.
RESULTS
Of the 23 patients evaluated, 20 were male, including 16 with the right knee affected. The average age of patients was 26 years (12-40). The interval between injury and surgery was approximately 15 months (1-72) and the mean follow-up period was 73 months (45-96). In the diagnostic arthroscopy evaluation of these patients, 18 had normal cartilage and five had patellofemoral and femorotibial fibrillation without bone exposure.
We repaired 19 medial and four lateral menisci. On average, 4.17 implants (two to eight) were used in the medial meniscus procedures and an average of four implants (three to five) were used in the lateral meniscus.
Eleven patients had an anterior drawer sign with displacement greater than 5 mm preoperatively and underwent ligament reconstruction as planned and are considered to be in group I (meniscal injury and ACL repair).
Ten patients had an anterior drawer smaller than 6 mm, no complaints of instability, and ACL injury was found in the arthroscopic examination. Meniscal repair was performed without ligament reconstruction, creating group II (meniscal injury in an unstable knee).
Two patients had a meniscus injury with an intact ACL and were classified as group III (meniscal injury in a stable knee).
Of the 23 patients, 21 had ACL injuries. Clinical improvement occurred in all patients in group I (meniscal injury and ACL repair).
In the ten patients in group II (meniscal injury in an unstable knee) with an untreated ACL injury, five evolved asymptomatically and did not ask for ligament reconstruction. The other five evolved with significant complaints of instability and in all cases ligament reconstruction was performed. In arthroscopic examination, four of the treated menisci were intact, confirming the MRI findings. One patient had a rupture of the medial meniscus and underwent partial meniscectomy. In the five patients who required further intervention, we considered only the last degree by the IKDC and Lysholm scales prior to the new procedure. These patients were excluded postoperatively and were not considered as group I.
The two patients in group III (meniscal injury in a stable knee) with initially no ACL injury progressed satisfactorily, but one patient ruptured the lateral meniscus after 56 months of follow-up (Figure 2).
Figure 2.
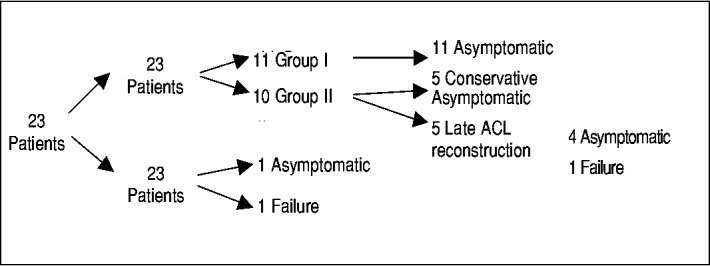
Study of patients undergoing arrow repair of longitudinal rupture of the meniscus. Group I: patients with meniscal injury and ACL reconstruction. Group II: patients with meniscal injury in an unstable knee. Group III: patients with meniscal injury in a stable knee.
Of the 23 operated cases, only two failed to repair, accounting for 8.7% of cases (Figure 1). This failure occurred in one patient in group II and one patient in group III.
Lysholm Scale
For this evaluation, the preoperative average was 55.43 points (36-74) with a standard deviation of ± 13.71; 15 patients had poor and eight had fair results. Postoperatively, the average was 86.3 points (6-100) with a standard deviation of ± 12.7; nine had excellent results, seven had good results, five were fair, and two were weak. Comparing the pre- and postoperative scores, there was a statistically significant improvement (Wilcoxon, p < 0.01) (Table 1 and Chart 1).
Table 1.
Preoperative and postoperative assessment using the Lysholm scale.
| Individual | Preoperative | Postoperative | ACL |
|---|---|---|---|
| I | 68 | 86 | Group I |
| II | 55 | 71 | Group I |
| III | 44 | 85 | Group II |
| IV | 55 | 60 | Group I |
| V | 68 | 85 | Group II |
| VI | 55 | 100 | Group I |
| VII | 36 | 91 | Group II |
| VIII | 68 | 95 | Group I |
| IX | 55 | 86 | Group II |
| X | 43 | 91 | Group I |
| XI | 59 | 95 | Group I |
| XII | 59 | 100 | Group I |
| XIII | 74 | 95 | Group I |
| XIV | 68 | 81 | Group III |
| XV | 74 | 95 | Group II |
| XVI | 51 | 68 | Group III |
| XVII | 42 | 100 | Group II |
| XVIII | 38 | 100 | Group II |
| XIX | 65 | 91 | Group I |
| XX | 74 | 64 | Group II |
| XXI | 61 | 66 | Group II |
| XXII | 29 | 80 | Group I |
| XXIII | 34 | 100 | Group II |
| MEAN | 55.43 | 86.3 |
Individual = Patient operated. Preoperative = Lysholm scale results for each individual in the preoperative period. Postoperative = Lysholm scale results for each individual in the postoperative period. State of ACL found in the immediate postoperative period. Group I: patients with meniscal injury and ACL reconstruction. Group II: patients with meniscal injury in an unstable knee. Group III: patients with meniscal injury in a stable knee. Mean: arithmetic mean between pre-and postoperative. Source: Hospital São Joaquim.
Chart 1.
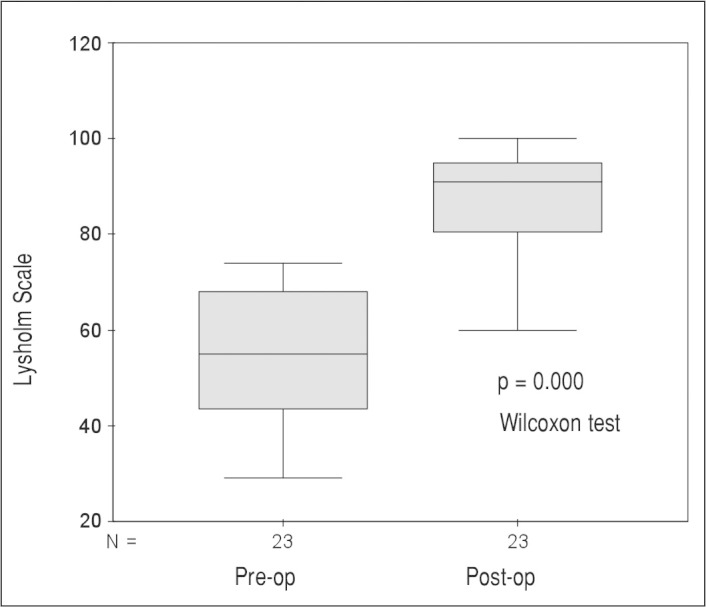
Comparative study of all patients pre -and ostoperatively using the Lysholm scale.
We used the nonparametric ANOVA for ordinal data with repeated measures to assess the pre- and postoperative measurements of groups I and II. This approach allows for testing the hypothesis of a lack of effect of factors among individuals (groups I and II) and intraindividually (pre- and post-operative), and the interaction of these factors (Table 2).
Table 2.
Preoperative and postoperative evaluation by Lysholm scale in patients undergoing ACL reconstruction and with injured ACL.
| Test statistic | g.l. | p-value | |
|---|---|---|---|
| Between individuals (group) | 0.209 | 1 | 0.648 |
| Intraindividual (time) | 45.532 | 1 | < 0.001 |
| Interaction | 0.034 | 1 | 0.854 |
Test statistic: nonparametric ANOVA for ordinal data with repeated measures. p-value: p value. Between individuals (group): Comparison of group I and group II. Intraindividual (time): Comparison between preoperative and postoperative results.
Source: Hospital São Joaquim
We evaluated the stabilization of the knee and did not detect a statistically significant difference between groups I and II (p = 0.648). Even if there were differences between the two groups, both had the same behavior (Chart 2). No interaction effect was found, but there was a difference between the preoperative and postoperative periods.
Chart 2.
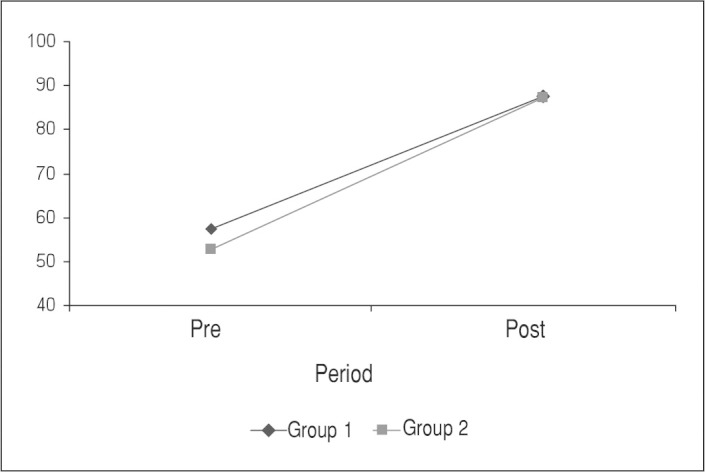
Comparative study of patients in groups I and II preoperatively and postoperatively by Lysholm scale scores.
The postoperative evaluation showed that four of these patients complained of claudication, two in group II (meniscal injury in an unstable knee) and two in group III (meniscal injury in a stable knee). Claudication was related to instability in two of the patients, but meniscus repair had failed in the other two.
All patients were capable of walking without crutches or canes.
Six complained of some degree of joint stiffness, four in group I (meniscal injury and ACL repair), two from group II (meniscal injury in an unstable knee).
Regarding stability, it was observed that three belonged to group I (meniscal injury and ACL repair), six belonged to group II (meniscal injury in an unstable knee) and one belonged to group III (meniscal injury in a stable knee).
Thirteen patients complained of pain, which was most salient in a patient from group III (meniscal injury in a stable knee) with a torn meniscus. Twelve patients reported pain on exertion, four in group I (meniscal injury and ACL repair) and eight in group II (meniscal injury in an unstable knee); one patient in the latter group had a new injury.
Four patients reported edema, two in group I (meniscal injury and ACL repair) and two in group II (meniscal injury in an unstable knee).
Nine reported a minor restriction when climbing stairs, four in group I (meniscal injury and ACL repair), three in group II (meniscal injury in an unstable knee) and two in group III (meniscal injury in a stable knee).
IKDC
Postoperative IKDC evaluation resulted in four patients with an A score, 13 with a B score, and six with a C score. Of these, 12 reported no changes related to activity, and consequently, with the knee injury. Two patients were classified as B in the radiological exam, but none progressed to osteoarthritis according to the radiological criteria (Table 3).
Table 3.
Results of the postoperative IKDC.
| Individual | IKDC | ACL status |
|---|---|---|
| I | B | Group I |
| II | C | Group I |
| III | A | Group II |
| IV | C | Group I |
| V | B | Group II |
| VI | B | Group I |
| VII | B | Group II |
| VIII | B | Group I |
| IX | C | Group II |
| X | B | Group I |
| XI | B | Group I |
| XII | B | Group I |
| XIII | B | Group I |
| XIV | B | Group III |
| XV | B | Group II |
| XVI | C | Group III |
| XVII | A | Group II |
| XVIII | A | Group II |
| XIX | B | Group I |
| XX | C | Group II |
| XXI | C | Group II |
| XXII | A | Group I |
| XXIII | A | Group II |
Individual refers to each patient. IKDC scores: A – Normal, B – Almost normal, C – Abnormal, D – Severely abnormal. ACL – Status of the ACL (anterior cruciate ligament). Group I: patients with meniscal injury and ACL reconstruction. Group II: patients with meniscal injury in an unstable knee. Group III: patients with meniscal injury in a stable knee.
Source: Hospital São Joaquim
One patient in group I (meniscal injury and ACL repair) and four in group II (meniscal injury in an unstable knee) were considered normal. Eight patients in group I (meniscal injury and ACL repair), three in group II (meniscal injury in an unstable knee), and one in group III (meniscal injury in a stable knee) had knees that were considered almost normal.
Two patients in group I (meniscal injury and ACL repair), three in group II (meniscal injury in an unstable knee) and group III (meniscal injury in a stable knee) had knees that were considered abnormal.
We reassessed the six patients classified as C. Two had meniscal injury. One patient in group III (meniscal injury in a stable knee) showed lateral injury and one patient in group II (meniscal injury in an unstable knee) showed medial injury.
Two patients in group II (meniscal injury in an unstable knee) developed significant instability, however, the repair of the meniscus remained intact, which was confirmed by arthroscopic evaluation.
Two patients in group I (meniscal injury and ACL repair) were classified as C. One reported pain on compression of the medial scar and paresis of the medial aspect of the leg. The patient underwent MRI and the meniscal repair appeared intact, this patient did not report mechanical pain. Another patient presented anterior knee pain during patellar compression when kneeling but no mechanical pain; control MRI showed an intact meniscus; the pain was associated with patellar fracture, which occurred during the surgical procedure.
Of the eight patients complaining of knee that were assessed by MRI, only two showed meniscal injury.
There were no neurovascular complications, signs of synovitis, subcutaneous granuloma, or foreign body granuloma. In patients that were reevaluated arthroscopically, there were no chondral injuries or fragments of intra-articular implant. However, some complications may not have been detected in this study, especially in the asymptomatic group, because there was no MRI control or arthroscopic control.
DISCUSSION
The results of this study indicate that there was functional improvement in patients who underwent meniscus repair with the arrow and only two known failures of consolidation.
In choosing an absorbable implant, it is necessary to consider the stabilization of the fragments and if the repaired meniscus and the implant can withstand the same loads supported by wire sutures. Comparative studies indicate that the initial mechanical strength of sutures of the meniscus with wires is superior to the implants. According to Song and Lee(9), the resistance of the vertical PDS suture is 114N compared to 38N of the arrow, but stressed that when two arrows are applied at a distance of 6 mm, this resistance increases to 57N.
In their study, Barber and Herbert(10) found that the resistance of Mersilene 2.0 is 113N and that of the arrow is 34N. Becker et al.(11) found the resistance of Ethibond to be 62.0N versus the arrow, with 24.7N. These mechanistic studies were conducted on animals and cadavers, indicating greater resistance of the wires at the time of application in a particular area of the meniscus, but do not consider the whole repaired meniscus or resistance during and after the healing period. Arnoczky and Lavagnino(12) compared PDS sutures with PLA implants and observed that initially there is greater resistance with the wire, but that after six weeks, the implant maintained its tension and the wire showed signs of loosening. The fixation of the fragments provided by the arrow was enough to allow for clinical improvement in our study. In the eight symptomatic patients who underwent MRI, two had a meniscal injury, but arthroscopic evaluation of the integrity of the meniscus was performed only in the five patients in which there was ACL reconstruction at a second time.
The use of the arrow allowed for repair of the meniscus by arthroscopy exclusively without the use of a fixation knot, which seemed to us to be an important evolution. Before absorbable implants, repair of the meniscus by arthroscopy was performed exclusively with different types of wires and the suture was passed from within the joint out and from outside in. The repair of the meniscus from the inside out requires an additional incision up to the capsule on the posteromedial or lateral aspect of the knee to protect the neurovascular structures in the passage of the needle with the wires; knot fixation is extra-articular. Cannon and Vittori(13) evaluated this procedure in combination with ACL reconstruction when necessary and found 82% asymptomatic patients. In cases where there were no ACL injuries, only 48% remained asymptomatic. Rubman et al.(14) performed meniscal suture in vascularized areas with 42 months of follow-up and obtained 80% favorable results.
Another surgical technique to repair the meniscus is made by passing the suture from the outside in and distinguishes itself by reaching all areas, particularly the anterior horn. Morgan et al.(15) evaluated it by applying the extra-articular knot and found 96% of cases to be asymptomatic and 3% failures. Reassessing the asymptomatic group, they found 84% healing (65% complete and 19% incomplete healing). Reigel et al.(16) also assessed the repair of the meniscus by completely arthroscopic suture and totally intra-articular knot, noting that all remained asymptomatic. Using this technique, Abdelkafy et al.(17) re-examined 52 of the 93 patients operated by this procedure, and in 12 years of follow-up found a Lysholm score of 87.29; 36 had an IKDC classification of A, and so concluded that it is a safe procedure with good results. This process produces satisfactory results but also uses an additional incision, exposing the vascular nervous structures to risks, as well as requiring several intra- or extra-articular knots, which are not necessary with implants.
Some studies have compared arrows to sutures. Albrecht-Olsen et al.(1) compared the horizontal suture with the arrow and evaluated the arthroscopic repair after three to four months. Healing was observed in 91% of cases by arrow and 75% by suture. Steenbrugge et al.(4) and Húrel et al.(2) compared the suture from the inside out with the arrow, realizing that the use of the implant procedure required less surgical time, which is technically easier, with less neurovascular risk, especially while manipulating the posterior horn.
Controversy exists regarding the use of the arrow. Petsche et al.(3) evaluated patients undergoing meniscorrhaphy with the arrow and observed statistically significant improvement in the Lysholm and Tegner scales. There were two cases of new rupture in a patient who had an ACL injury, the first with the ligament untreated and the other that underwent ACL reconstruction. On the other hand, Kurzweil et al.(19) found failure in 20% by arrow meniscorrhaphy associated with ligamentoplasty, and in isolated meniscal injuries, 42%, considering this type of fixation to be a poor choice.
Our study has limitations because it is retrospective, with a limited sample without arthroscopic reevaluation of the treated patients. The certainty of healing or meniscus injury was only possible in six patients who underwent arthroscopic reevaluation. By the clinical criteria, we believe that patients with satisfactory functional results showed some degree of healing of the meniscus, however, we believe that there was undetected failure in the healing of the meniscus, since these individuals have not been reevaluated by MRI or by new diagnostic arthroscopy.
Perhaps some of the injuries we treated would have healed without any kind of fixation, particularly in the group that underwent ACL reconstruction. Weiss et al.(20) found that longitudinal lesions that tend to occur in the vascular portion of the periphery of the meniscus have great potential for cure and should not be treated, besides some abnormality. On the other hand, Talley and Grana(21) believe that stable longitudinal lesions of the meniscus have great potential for not healing caused by the spread of the injury, and should therefore be repaired. Pierre et al.(22) studied untreated meniscal injuries in patients undergoing ACL reconstruction and concluded that injuries of the medial meniscus larger than 10 mm should be treated. Yagishita et al.(23) observed that despite the healing potential of these meniscal injuries found during ACL reconstruction, the longer lesions must be repaired. In our study, all viable lesions larger than 20 mm were repaired and those that were smaller were excluded from the analysis.
The need for immediate ACL repair in cases of meniscus repair is a controversial subject. Steenbrugge et al.(4) compared patients who underwent meniscus repair with ACL repair with the group with unstable knees. Of the 20 patients treated, 14 had satisfactory results. On the other hand, seven underwent reconstruction in a second surgical period. They concluded that even if unsatisfactory results are higher in patients with unstable knees, ACL injury does not contraindicate repair of the meniscus. Hanks et al.(5) performed 23 repairs of the meniscus in unstable knees, 12 by arthrotomy and 11 by arthroscopy, and found a new rupture in only three cases. Of these patients, six reported pain, but only one required analgesics. Eight patients reported instability and one underwent ACL reconstruction. They also found instability not to contraindicate meniscus repair. More recently, Koukoulias and Papastergiou(6) evaluated 11 medial meniscus repairs in patients with an unstable knee for ACL injury with an arrow. They found failures in three individuals. Eight remained asymptomatic during daily activities, but seven complained of swelling after sports. They concluded that ACL deficiency does not contraindicate repair of the meniscus, but that there is a need to reduce the intensity of sport activities. In our study, the repair or injury of the anterior cruciate ligament did not influence the results according to the Lysholm scale. It is relevant that in our study 10 patients with ACL injury were not immediately submitted to ligament reconstruction and although there was joint instability, five remained asymptomatic and there was some degree of healing of the meniscus. Five other patients complained of instability, and of pain to a lesser degree, and in revision surgery for ligament reconstruction, rupture of the meniscus was observed in only one patient. Even so, all showed some functional improvement.
There were not enough patients in group III (meniscal injury in a stable knee) for statistical comparison with the other groups. Two subjects had an intact ACL, one remained asymptomatic, and the other suffered a new sprain after four years with rupture of the lateral meniscus (IKDC = 6 and Lysholm = 68). It was the least significant group, but its outcome could have been influenced by the quality of the meniscus. Cannon and Vittori(13) observed that injuries of the posterior horn of the meniscus in knees without ACL injury exhibit degenerative changes, which would compromise our criteria for the integrity of the meniscus. On the other hand, Sommerlath(24) noted that despite the significant incidence of rupture on the repaired menisci in the stable knees, those which heal retain better function and show less progression to osteoarthritis compared with those that underwent immediate meniscectomy. Therefore, in this situation we repaired the menisci.
CONCLUSION
There was improvement of joint function in these patients. Of the 23 operated, only two had a known failure in the repair of the meniscus. In this group, the ACL injury did not affect the functional outcome of repair. There was a higher incidence of reinterventions in patients with ACL injury.
Footnotes
We declare no conflict of interest in this article.
Study conducted by the Arthroscopy and Orthopedic Clinic, Hospital Alemão Oswaldo Cruz.
REFERENCES
- 1.Albrecht-Olsen P, Kristensen G, Burgaard P, Joergensen U, Toerholm C. The arrow versus horizontal suture in arthroscopic meniscus repair. A prospective randomized study with arthroscopic evaluation. Knee Surg Sports Traumatol Arthrosc. 1999;7(5):268–273. doi: 10.1007/s001670050162. [DOI] [PubMed] [Google Scholar]
- 2.Húrel C, Mertens F, Verdonk R. Biofix resorbable meniscus arrow for meniscal ruptures: results of a 1-year follow-up. Knee Surg Sports Traumatol Arthrosc. 2000;8(1):46–52. doi: 10.1007/s001670050010. [DOI] [PubMed] [Google Scholar]
- 3.Petsche TS, Selesnick H, Rochman A. Arthroscopic meniscus repair with bioabsorbable arrows. Arthroscopy. 2002;18(3):246–253. doi: 10.1053/jars.2002.30615. [DOI] [PubMed] [Google Scholar]
- 4.Steenbrugge F, Verdonk R, Hurel C, Verstraete K. Arthroscopic meniscus repair: inside-out technique vs. Biofix meniscus arrow. Knee Surg Sports Traumatol Arthrosc. 2004;12(1):43–49. doi: 10.1007/s00167-003-0446-8. [DOI] [PubMed] [Google Scholar]
- 5.Hanks G, Gause TM, Handal JA, Kalenak A. Meniscus repair in the anterior cruciate deficient knee. Am J Sports Med. 1990;18:606–613. doi: 10.1177/036354659001800609. [DOI] [PubMed] [Google Scholar]
- 6.Koukoulias N, Papastergiou S. Mid-term clinical results of medial meniscus repair with the meniscus arrow in the unstable knee. Knee Surgery, Sports Traumatology, Arthroscopy. 2006;15(2):138–143. doi: 10.1007/s00167-006-0162-2. [DOI] [PubMed] [Google Scholar]
- 7.Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop. 1985;198:43–49. [PubMed] [Google Scholar]
- 8.Hefti F, Muller W, Jakob RP, Staubli HU. Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sports Traumatol Arthrosc. 1993;1:226–234. doi: 10.1007/BF01560215. [DOI] [PubMed] [Google Scholar]
- 9.Song EK, Lee KB. Biomechanical test comparing the load to failure of the biodegradable meniscus arrow versus meniscal suture. Arthroscopy. 1999;15(7):726–732. doi: 10.1016/s0749-8063(99)70004-6. [DOI] [PubMed] [Google Scholar]
- 10.Barber FA, Herbert MA. Meniscal repair devices. Arthroscopy. 2000;16(6):613–618. doi: 10.1053/jars.2000.4819. [DOI] [PubMed] [Google Scholar]
- 11.Becker R, Wirz D, Wolf C, Gopfert B, Nebelung W, Friederich N. Measurement of meniscofemoral contact pressure after repair of bucket-handle tears with biodegradable implants. Arch Orthop Trauma Surg. 2005;125(4):254–260. doi: 10.1007/s00402-004-0739-5. [DOI] [PubMed] [Google Scholar]
- 12.Arnoczky SP, Lavagnino M. Tensile fixation strengths of absorbable meniscal repair devices as a function of hydrolysis time. An in vitro experimental study. Am J Sports Med. 2001;29(2):118–123. doi: 10.1177/03635465010290020201. [DOI] [PubMed] [Google Scholar]
- 13.Cannon WD, Jr, Vittori JM. The incidence of healing in arthroscopic meniscal repairs in anterior cruciate ligament-reconstructed knees versus stable knees. Am J Sports Med. 1992;20(2):176–181. doi: 10.1177/036354659202000214. [DOI] [PubMed] [Google Scholar]
- 14.Rubman MH, Noyes FR, Barber-Westin SD. Arthroscopic repair of meniscal tears that extend into the avascular zone. A review of 198 single and complex tears. Am J Sports Med. 1998;26(1):87–95. doi: 10.1177/03635465980260013301. [DOI] [PubMed] [Google Scholar]
- 15.Morgan CD, Wojtys EM, Casscells CD, Casscells SW. Arthroscopic meniscal repair evaluated by second-look arthroscopy. Am J Sports Med. 1991;19(6):632–687. doi: 10.1177/036354659101900614. [DOI] [PubMed] [Google Scholar]
- 16.Reigel CA, Mulhollan JS, Morgan CD. Arthroscopic all-inside meniscus repair. Clin Sports Med. 1996;15(3):483–489. [PubMed] [Google Scholar]
- 17.Abdelkafy A, Aigner N, Zada M, Elghoul Y, Abdelsadek H, Landsiedl F. Two to nineteen years follow-up of arthroscopic meniscal repair using the outside-in technique: a retrospective study. Arch Orthop Trauma Surg. 2007;127(4):245–252. doi: 10.1007/s00402-006-0139-0. [DOI] [PubMed] [Google Scholar]
- 19.Kurzweil PR, Tifford CD, Ignacio EM. Unsatisfactory clinical results of meniscal repair using the meniscus arrow. Arthroscopy. 2005;21(8):905. doi: 10.1016/j.arthro.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 20.Weiss CB, Lundberg M, Hamberg P, DeHaven KE, Gillquist J. Non-operative treatment of meniscal tears. J Bone Joint Surg Am. 1989;71(6):811–822. [PubMed] [Google Scholar]
- 21.Talley MC, Grana WA. Treatment of partial meniscal tears identified during anterior cruciate ligament reconstruction with limited synovial. Arthroscopy. 2000;16(1):6–10. doi: 10.1016/s0749-8063(00)90120-8. [DOI] [PubMed] [Google Scholar]
- 22.Pierre A, Hulet C, Locker B, Schiltz D, Delbarre JC, Vielpeau C. Outcome of 95 stable meniscal tears left in place after reconstruction of the anterior cruciate ligament. Rev Chir Orthop Reparatrice Appar Mot. 2001;87(7):661–668. [PubMed] [Google Scholar]
- 23.Yagishita K, Muneta T, Ogiuchi T, Sekiya I, Shinomiya K. Healing potential of meniscal tears without repair in knees with anterior cruciate ligament reconstruction. Am J Sports Med. 2004;32(8):1953–1961. doi: 10.1177/0363546504263702. [DOI] [PubMed] [Google Scholar]
- 24.Sommerlath KG. Results of meniscal repair and partial meniscectomy in stable knees. Int Orthop. 1991;15(4):347–350. doi: 10.1007/BF00186875. [DOI] [PubMed] [Google Scholar]


