Abstract
Describe the results of proximal humeral fractures surgically treated with the Philos locking plate system. Method: Between March 2003 and October 2004 we prospectively reviewed 24 of 26 patients with proximal humerus fractures treated with a Philos plate. The mean follow-up time was 12 months and the mean age of patients was 57 years. Six patients had four-part proximal humerus fractures, 11 patients had three-part proximal humerus fractures, and nine patients had two-part proximal humerus fractures. Clinical evaluation was performed using the University of California at Los Angeles (UCLA) criteria. Results: The mean UCLA score was 30 points (17-34). All fractures showed union. Three patients showed fracture union at varus position. The mean UCLA score for these patients was 27 points. Conclusion: Osteosynthesis with Philos plate provides a stable fixation method with good functional outcome.
Keywords: Humeral fractures; Fracture fixation, Internal; Cohort studies; Prospective studies
INTRODUCTION
The incidence of fractures of the proximal humerus accounts for 4-5% of all fractures(1). They are most common in the elderly; in the young, they are generally related to high-energy trauma(2).
Most of these fractures are stable and with minimum deviation, and closed treatment is possible. However, in 15 to 20% of cases, surgical intervention is necessary. Whenever possible, the osteosynthesis is the option employed, since the functional results of hemiarthroplasty are not sufficiently satisfactory in most cases(2). The aim of osteosynthesis is to promote stability allowing for early mobilization, and obtaining good positioning of the fractured fragments(2).
The choice of the type of reduction or synthesis material to be used depends on the pattern of fracture, bone quality, age, and activity level of the patient2, 3.
The use of the plate and screw fixation method as an option is widespread among orthopedists. However, any method is subject to complications such as loosening of the fasteners, especially in older patients(3).
Therefore, the fixed-angle locked plate was developed to allow for more stable fixation, especially in poor quality bone. The Philos (Proximal Humeral Internal Locking System) plate is an example of this new generation of implant plates with a locking system; it is considered a fixed-angle implant, whose design was based on the anatomy of the proximal humerus(4).
The objective of this study was to describe the technique of using a fixed-angle plate with Philos locking screws and evaluate the results in 26 patients with traumatic injuries of the proximal humerus who underwent osteosynthesis using this type of implant.
METHODS
Between March 2003 and October 2004 a prospective cohort study was conducted in which 26 patients, 14 females and 12 males, were treated surgically by the Shoulder and Elbow Group of the National Institute of Traumatology and Orthopedics (INTO-RJ), due to fracture of the proximal humerus. Fixed-angle plate with Philos locking screws was used as the fixation method for the proximal humerus. All cases of fractures of the proximal humerus treated with indication for osteosynthesis during that period were included.
In the preoperative period, a form was completed identifying the age, gender, trauma mechanism, presence of associated injuries, and the fracture classification according to Neer and the AO (Arbeitsgemeinschaft fúr Osteosynthesefrägen). The average age of patients was 57 years (24-85 years). The mechanism of fracture was a fall in 17 patients, car accident in five, and four different causes for the others. In patients younger than 50 years (11), the automobile accident was the most common cause of fracture. According to the Neer classification, nine fractures were classified into two parts, 11 in three parts, two of which were associated with anterior dislocation (Figure 1), and six in four parts, four of the valgus impacted type (Table 1). Among the associated lesions, there was a case of pelvic bone fracture, a case of distal radius fracture, and one case of fracture of the cheekbone. Once the criteria for surgical indication were met, osteosynthesis was performed using the fixed-angle plate with Philos locking screws (Figure 2). Patients were followed on an outpatient basis with clinical and radiographic examination (Figure 3).
Figure 1.
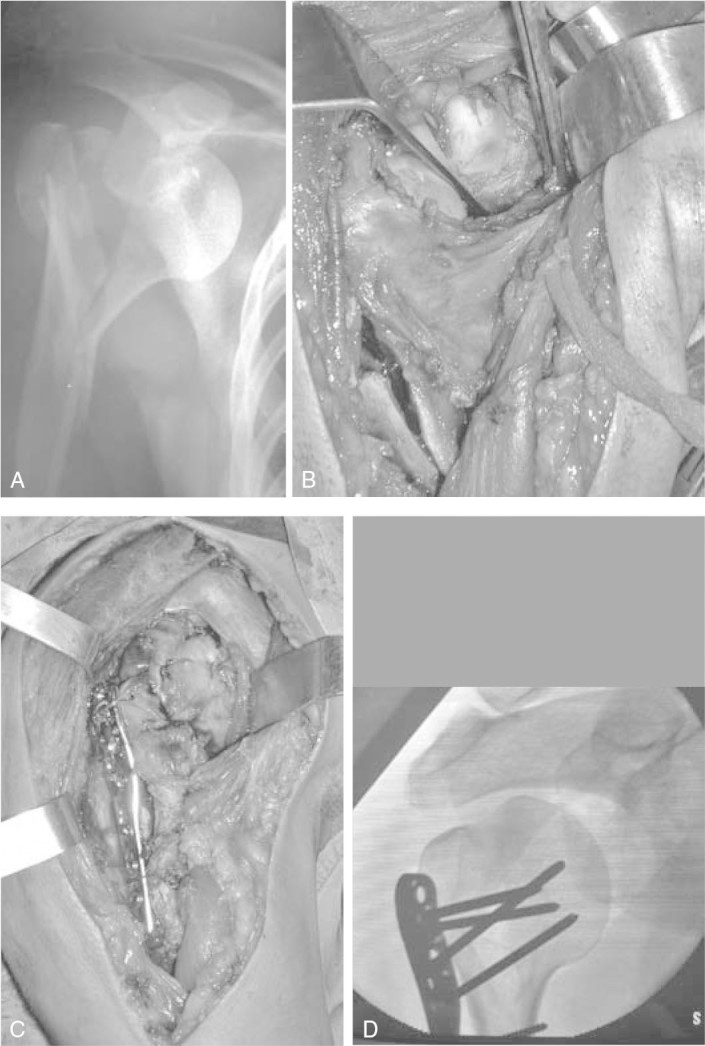
A) Radiograph showing fracture into three parts with anterior dislocation. (B and C) Intraoperative appearance of the fracture and dislocation after reduction and osteosynthesis with a Philos plate. D) Intraoperative fluoroscopic image.
Table 1.
Patients.
| Pat | Gender | Age | Classification (Neer) | Classification (AO) | Post deviation | AF | ER | IR | Post UCLA |
|---|---|---|---|---|---|---|---|---|---|
| 1 | M | 56 | 3 | B2 | NO | 110 | 40 | T8 | 29 |
| 2 | F | 85 | 2 | A3 | VARUS | 90 | 30 | T10 | 26 |
| 3 | F | 59 | 4 (imp valgus) | C1 | NO | 135 | 35 | T11 | 31 |
| 4 | M | 46 | 3 | B1 | VARUS | 150 | 30 | T10 | 29 |
| 5 | M | 50 | 4 (imp valgus) | C2 | NO | 170 | 50 | T8 | 35 |
| 6 | F | 78 | 4 (imp valgus) | C2 | NO | 100 | 30 | T12 | 26 |
| 7 | M | 51 | 3 | B2 | NO | 120 | 30 | T10 | 29 |
| 8 | F | 80 | 2 | A3 | VARUS | 90 | 25 | L1 | 26 |
| 9 | F | 41 | 3 | B1 | NO | 170 | 50 | T8 | 33 |
| 10 | F | 74 | 2 | A3 | NO | 140 | 40 | T9 | 33 |
| 11 | M | 61 | 4 (imp valgus) | C2 | NO | 160 | 40 | T10 | 33 |
| 12 | F | 67 | 3 | B2 | NO | 130 | 40 | T12 | 30 |
| 13 | F | 34 | 4 | C2 | NO | 160 | 50 | T8 | 34 |
| 14 | M | 38 | 3 | B3 | NO | 150 | 45 | T9 | 31 |
| 15 | M | 43 | 2 | A3 | NO | 170 | 50 | T5 | 28 |
| 16 | F | 82 | 2 | A2 | NO | 150 | 45 | T10 | 34 |
| 17 | F | 51 | 3 | B1 | NO | 140 | 30 | T8 | 25 |
| 18 | M | 39 | 2 | A3 | NO | 150 | 45 | T6 | 30 |
| 19 | F | 61 | 3 | B1 | NO | 120 | 25 | T9 | 30 |
| 20 | M | 38 | 2 | B3 | NO | 60 | 50 | T11 | 17 |
| 21 | F | 44 | 3 | B1 | NO | 140 | 50 | T9 | 30 |
| 22 | M | 41 | 4 | C2 | NO | 130 | 30 | T9 | 30 |
| 23 | F | 74 | 2 | A3 | NO | 140 | 50 | T8 | 34 |
| 24 | M | 24 | 3 | B2 | NO | 180 | 60 | T8 | 34 |
Legend: Pat = patient; M = male, F = female; Imp valgus = Impacted valgus; Post deviation = postoperative deviation; AF = anterior flexion, ER = external rotation, IR = Internal rotation; Post UCLA = postoperative UCLA score. Source: National Institute of Traumatology and Orthopedics (INTO).
Figure 2.

A) Radiograph showing fracture of the shoulder in four parts with a valgus deviation. B) Good consolidation after fracture reduction and osteosynthesis.
Figure 3.
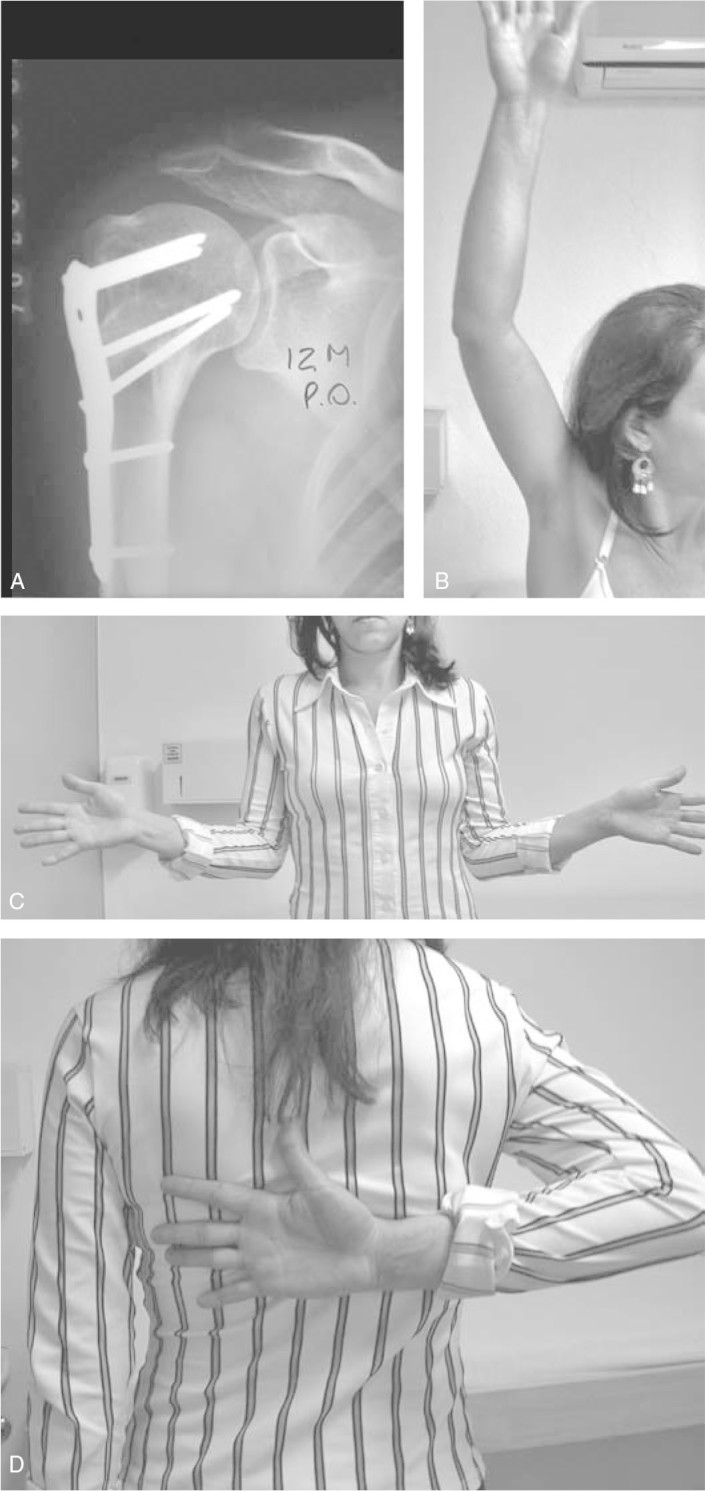
A) Radiograph of postoperative fracture treated surgically with Philos plate. B, C and D) Functional outcome after one year of surgery.
We assessed the range of motion of the shoulder, fracture healing, patient satisfaction, and the presence of complications related to the surgical technique or implant. Clinical evaluation was performed using the system of points defined by the University of California at Los Angeles (UCLA)(5).
SURGICAL TECHNIQUE
All surgeries were performed under general anesthesia and with a scalene block for postoperative analgesia. Prophylactic antibiotic therapy (cephalosporin) was initiated with the anesthetic induction, lasting for 24 hours after the surgery. Patients were positioned supine, in the beach chair position, on a table made specifically for shoulder surgery, which allowed for radiographs in the three planes essential for the procedure, these being: anteroposterior, axillary, and lateral profiles of the shoulder. The image intensifier was placed at the head of the operating table so that the arc could rotate freely.
Deltopectoral approach was used. Since plate positioning determines the position of the screws on the head of the humerus, whenever possible, we positioned the implant so that the screws were located mainly in the central, inferior, and posterior regions of the humeral head. On average, five screws were placed in the humeral head (three to six screws). In the immediate postoperative period, the upper limb was kept in the sling, starting mobilization after the first outpatient visit between the fifth and seventh days.
RESULTS
Of the 26 patients enrolled, 24 returned for evaluation with a mean follow-up period of 12 months (ranging from eight to 24 months). All fractures consolidated with clinical and radiographic evidence.
The time between fracture and osteosynthesis averaged 14.4 days (ranging from two to 50 days). Seven patients had an interval of more than 21 days between injury and surgery.
The functional outcome assessed by the UCLA protocol had a mean score of 30 points, ranging from 17 to 35. The patients had active anterior flexion, which ranged from 60° to 180° (mean 135°), lateral rotation from 25° to 60° (mean 41°) and medial rotation of T8 to L1 (mean T9).
Three patients (11%) had consolidation with varus angulation (Figure 4), the UCLA functional score of these patients averaged 27 points. When these three patients were evaluated in isolation, their mean active anterior flexion was 110°, their mean lateral rotation was 28°, and internal rotation averaged T11. There were no complications such as avascular necrosis, nerve damage, or infection. The patient who presented pelvic bone fractures evolved with deep vein thrombosis of lower limb, which was treated with medication.
Figure 4.
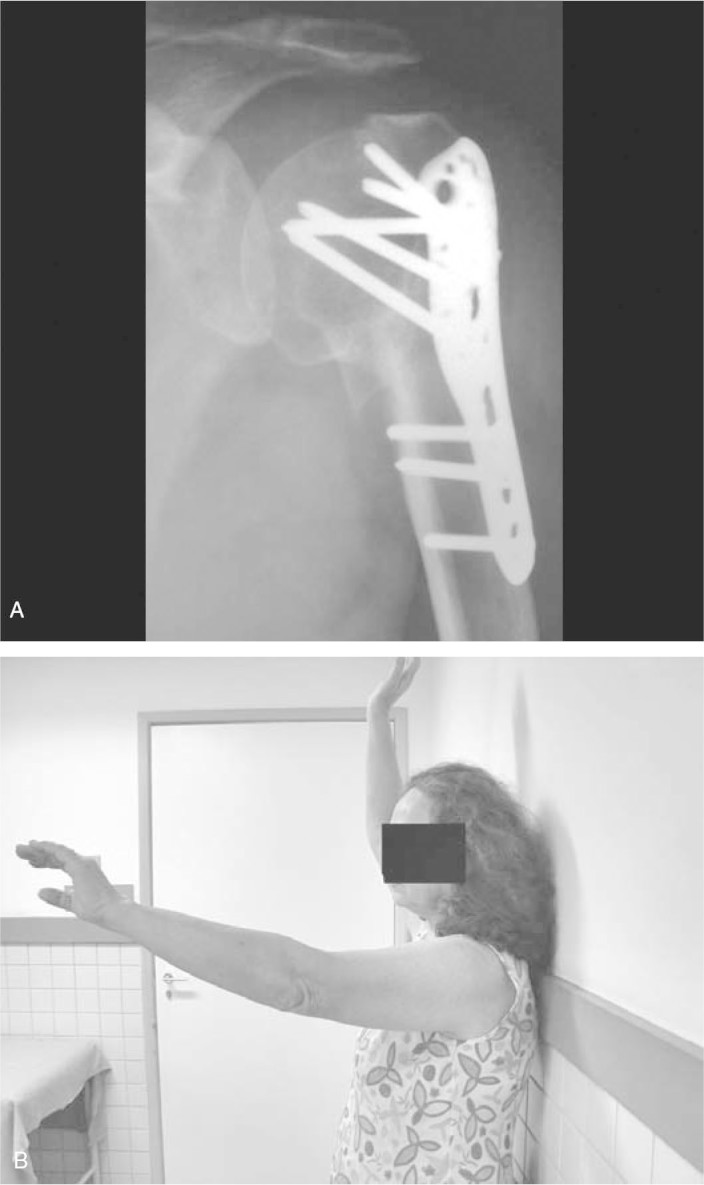
A) Radiograph of the shoulder showing a consolidated fracture with varus deviation. B) Patient showing decreased range of motion of the shoulder.
All patients reported satisfaction with the end result and 20 (83%) returned to work activities with the affected limb.
DISCUSSION
Several techniques have been described for fixation of fractures of the proximal humerus, such as the use of cerclage wire, tension band, Kirschner wire, T-plate, intramedullary nail, blade plate, and more recently the fixed-angle locked plates, each of these methods having their advantages and disadvantages6, 7.
Less invasive fixation methods such as percutaneous fixation as described by Braman and Flatow(8) are attractive though technically difficult, especially in patients with osteoporosis, in fractures with large bone comminution or significant deviation.
The primary goal of fracture fixation of the proximal humerus is to obtain a stable construction that allows for early rehabilitation. Koval et al.(9) demonstrated that in patients with minimally deviated fractures treated with closed surgery, better results were obtained in those who began rehabilitation within two weeks after the fracture.
Some authors report satisfactory results with osteosynthesis using conventional plates. Wanner et al.(10) reported good results using two one-third tubular plates. However, in osteopenic bone and in comminuted fractures, fixation with conventional plates may have a high incidence of complications, especially the release of the synthesis material(11).
Kristiansen and Christensen(11) reported satisfactory results in only nine of 20 patients (mean age 63 years) treated with a T-plate for proximal humerus fractures, with a high incidence of fixation failure.
Hintermann et al.(12) described good results in fractures fixed with a blade plate. But recently, Meier et al.(13) reported a 33% complication rate with this method, 22% of patients had protrusion of the blade plate in the shoulder joint.
Siffri et al.(14), in a biomechanical study on a cadaveric model, demonstrated greater stiffness of the locking plate under torsional forces compared with the blade plate. Edwards et al.(15) also demonstrated in cadaver studies that the biomechanical strength of the locking plate, the angling force and torsion force, in comminuted fractures of the surgical neck is higher when compared with that of the locked intramedullary nail.
Fixed-angle locked plates were developed to meet stability requirements, especially in osteopenic bone, without increasing the risk of osteonecrosis. There are few studies in the literature using Philos plates for these fractures.
In a recent study, Bjorkenheim et al.(16), using this plate, reported good results in 72 patients followed for at least one year. Among the complications, there were reports of two cases of nonunion, three cases of avascular necrosis, and two implant failures attributed to technical error.
Koukakis et al.(17) in a prospective study that included 20 patients with fractures in two, three and four parts of the Neer classification, treated with the same plate showed satisfactory results, reasoning that the use of this implant provides good stability in osteopenic bone, allowing for early mobilization.
More recently, Moonot et al.(18) reported results in 32 patients treated with Philos plate, but in three-and four-part fractures. There was clinical and radiographic union in 31 patients. One case progressed to avascular necrosis requiring hemiarthroplasty. The other complications reported were malunion in two patients and wrong positioning of the plate or screw in three cases.
In our study, all patients had their fractures consolidated, different from the study presented recently by Rose et al.(19), in which consolidation occurred in 75% of 16 patients treated with the locking plate system. In their series, the four patients who had progressed to pseudarthrosis had three-part fractures associated with metaphyseal comminution, and in three cases, the patients were smokers. Rose et al.(19) cite this as a risk factor for delayed union and nonunion. Varus malunion occurred in three of our patients. We attribute this complication to poor perioperative reduction prior to implant placement. It is very important to obtain anatomical reduction before placing the locking plate, since this system does not allow for improvement of the reduction after the locking screws are placed in the humeral head. Another fact that is important to consider is the placement of screws in regions with higher trabecular bone density in the humeral head, which are the central, inferior, and posterior regions(20). There are no studies in the literature on the subject of the number of screws in the humeral head. Since five screws were placed in most of our patients, we believe that this number provides good safety in regards to stability. A disadvantage of this implant is that its cost is far greater than that of conventional implants.
In our experience, osteosynthesis with this type of plate revealed no major difficulties in relation to other previously used implants and the main challenge was to obtain anatomic reduction, especially in fractures in three and four parts. The high rate of consolidation, together with patient satisfaction, makes this method a good alternative in the treatment of these fractures.
CONCLUSION
The osteosynthesis of fractures of the proximal humerus with fixed-angle plates and locking Philos screws proved to be a technique with satisfactory functional results and a low complication rate in this group of patients.
Footnotes
We declare no conflict of interest in this article.
Study conducted at the National Institute of Traumatology and Orthopedics (INTO-RJ).
REFERENCES
- 1.Habermeyer P, Schweiberer L. Fractures of the proximal humerus. Orthopade. 1989;18(3):200–207. [PubMed] [Google Scholar]
- 2.Iannotti JP, Ramsey ML, Williams GR, Jr, Warner JJ. Nonprosthetic management of proximal humeral fractures. Instr Course Lect. 2004;53:403–416. [PubMed] [Google Scholar]
- 3.Broos PL, Semon A. From unstable internal fixation to biological osteosynthesis. A historical overview of operative fracture treatment. Acta Chir Belg. 2004;104(4):396–400. [PubMed] [Google Scholar]
- 4.Smith WR, Ziran BH, Anglen JO, Stahel PF. Locking plates: Tips and tricks. J Bone Joint Surg Am. 2007;89(10):2298–2307. doi: 10.2106/00004623-200710000-00028. [DOI] [PubMed] [Google Scholar]
- 5.Amstutz HC, Sew Hoy AL, Clarke IC. UCLA anatomic total shoulder arthroplasty. Clin Orthop Relat Res. 1981;(155):7–20. [PubMed] [Google Scholar]
- 6.Veado MAC, Moura ALL. Fraturas em duas e tres partes do umero proximal tratadas com sutura nao absorvivel. Rev Bras Ortop. 2007;42(10):333–342. [Google Scholar]
- 7.Checchia SL, Doneux SP, Miyazaki AN, Fregonese M, Silva LA, Lobo AC. Avaliação do tratamento cirúrgico da fratura em duas partes do colo cirúrgico do úmero com placa PFS 80R. Rev Bras Ortop. 2004;39(10):555–567. [Google Scholar]
- 8.Braman JP, Flatow EL. How to transition to percutaneous pinning for proximal humerus fractures. Tech Shoulder Elbow Surg. 2005;6:171–177. [Google Scholar]
- 9.Koval KJ, Gallagher MA, Marsicano JG, Cuomo F, McShinawy A, Zuckerman JD. Functional outcome after minimally displaced fractures of the proximal part of the humerus. J Bone Joint Surg Am. 1997;79(2):203–207. doi: 10.2106/00004623-199702000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Wanner GA, Wanner-Schmid E, Romero J, Hersche O, von Smekal A, Rrentz O. Internal fixation of displaced proximal humeral fractures with two one-third tubular plates. J Trauma. 2003;54(3):536–544. doi: 10.1097/01.TA.0000052365.96538.42. [DOI] [PubMed] [Google Scholar]
- 11.Kristiansen B, Christensen SW. Plate fixation of proximal humeral fractures. Acta Orthop Scand. 1986;57(4):320–323. doi: 10.3109/17453678608994401. [DOI] [PubMed] [Google Scholar]
- 12.Hintermann B, Trouillier HH, Schafer D. Rigid internal fixation of fractures of the proximal humerus in older patients. J Bone Joint Surg Br. 2000;82(8):1107–1112. doi: 10.1302/0301-620x.82b8.10330. [DOI] [PubMed] [Google Scholar]
- 13.Meier RA, Messmer P, Regazzoni P, Rothfischer W, Gross T. Unexpected high complication rate following internal fixation of unstable proximal humerus fractures with an angled blade plate. J Orthop Trauma. 2006;20(4):253–260. doi: 10.1097/00005131-200604000-00004. [DOI] [PubMed] [Google Scholar]
- 14.Siffri PC, Peindl RD, Coley ER, Norton J, Connor PM, Kellam JF. Biomechanical analysis of blade plate versus locking plate fixation for a proximal humerus fracture: Comparison using cadaveric and synthetic humeri. J Orthop Trauma. 2006;20(8):547–554. doi: 10.1097/01.bot.0000244997.52751.58. [DOI] [PubMed] [Google Scholar]
- 15.Edwards SL, Wilson NA, Zhang L, Flores S, Merk BR. Two-part surgical neck fractures of the proximal part of the humerus. A biomechanical evaluation of two fixation techniques. J Bone Joint Surg Am. 2006;88(10):2258–2264. doi: 10.2106/JBJS.E.00757. [DOI] [PubMed] [Google Scholar]
- 16.Bjorkenheim JM, Pajarinen J, Savolainen V. Internal fixation of proximal humeral fractures with a locking compression plate. A retrospective evaluation of 72 patients followed for a minimum of 1 year. Acta Orthop Scand. 2004;75(6):741–745. doi: 10.1080/00016470410004120. [DOI] [PubMed] [Google Scholar]
- 17.Koukakis A, Apostolou CD, Taneja T, Korres DS, Amini A. Fixation of proximal humerus fractures using the PHILOS plate: early experience. Clin Orthop Relat Res. 2006;(442):115–120. doi: 10.1097/01.blo.0000194678.87258.6e. [DOI] [PubMed] [Google Scholar]
- 18.Moonot P, Ashwood N, Hamlet M. Early results for treatment of three-and four-part fractures of the proximal humerus using the PHILOS plate system. J Bone Joint Surg Br. 2007;89(9):1206–1209. doi: 10.1302/0301-620X.89B9.18528. [DOI] [PubMed] [Google Scholar]
- 19.Rose PS, Adams CR, Torchia ME, Jacofsky DJ, Haidukewych GG, Steinmann SP. Locking plate fixation for proximal humeral fractures: Initial results with a new implant. J Shoulder Elbow Surg. 2007;16(2):202–207. doi: 10.1016/j.jse.2006.06.006. [DOI] [PubMed] [Google Scholar]
- 20.Tingart MJ, Lehtinen J, Zurakowski D, Warner JJ, Apreleva M. Proximal humeral fractures: regional differences in bone mineral density of the humeral head affect the fixation strength of cancellous screws. J Shoulder Elbow Surg. 2006;15(5):620–624. doi: 10.1016/j.jse.2005.09.007. [DOI] [PubMed] [Google Scholar]


