Abstract
Objective: The purpose of this study is to evaluate the short-term follow-up results of arthroscopic treatment of femoroacetabular impingement. Our hypothesis is that arthroscopic treatment results are favorable. Methods: Between August 2003 and August 2007, 28 hips had femoroacetabular impingement treated by hip arthroscopy. The mean age was 34 years, with mean follow-up period of 27 months. Clinical results were graded with the modified Harris hip score, which was measured pre- and postoperatively. Patients had also their internal rotation analyzed. These parameters were calculated by using Wilcoxon's t test for analysis of nonparametric paired samples performed. Results: The mean preoperative Harris Hip Score was 54.2, improving to 94.8 postoperatively (p<0,001). The mean increase was 37.5 points. We had 4 good results (15%) and 24 excellent results (85%). Preoperatively, the patients had a mean internal rotation of 17°, and, postoperatively, 36°. The average internal rotation increase was 19° (p<0,001). Conclusions: The arthroscopic treatment of femoroacetabular impingement presents satisfactory results.
Keywords: Osteoarthritis, hip/diagnosis; Osteoarthritis, hip/etiology Osteoarthritis, hip/therapy; Osteoarthritis, hip/pathology; Arthroscopy
INTRODUCTION
Several factors may coexist in the etiology of hip osteoarthritis, among them, genetic, morphological, and biochemical abnormalities. Although the pathophysiological mechanism of the degenerative process affecting the dysplastic hip is well understood, many “idiopathic” forms of arthritis deserve further clarification, since they remain the most common cause of osteoarthritis of the hip. Based on over 40 years of observations(1), it is believed that all idiopathic osteoarthritis are secondary to previously underestimated or unrecognized subtle acetabular and femoral changes. There is increasing evidence that femoroacetabular impingement (FAI) plays an important role in the mechanical etiology of the development of hip osteoarthritis(2).
Femoroacetabular impingement is capable of destroying the hip joint once it causes articular mechanical changes that generate a vicious cycle of organic action and reaction. The literature on the topic is unanimous in this assertion3, 4, 5, 6, 7, 8, 9.
Unlike the knee, where the changes in the cartilage and ligaments are the most common cause of arthritis, in the hip, bone dysmorphism such as dysplasia and FAI leads to injury of the chondrolabral complex and subsequent joint degeneration. The orthopedic surgeon must recognize these changes.
The discussion of osteoarthritis in young patients was until recently limited to the indication of osteotomy, arthrodesis, or arthroplasty, in other words, action after joint destruction. With the favorable results of open surgery in the short-term10, 11, 12, arthroscopic treatment has emerged as a promising new option.
The purpose of this study is to assess the short-term results of the arthroscopic treatment of femoroacetabular impingement. Our hypothesis is that the results of arthroscopic treatment are favorable.
Figure 1.
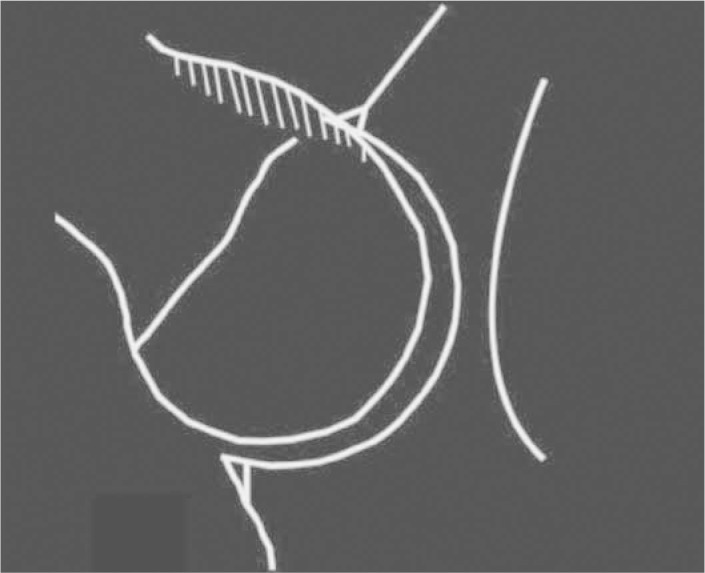
Depiction of the cam-type impingement.
Figure 2.
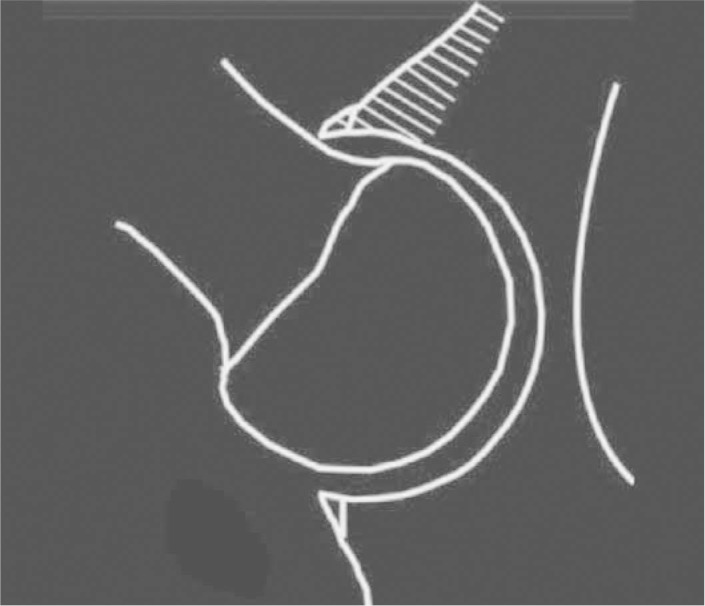
Depiction of the pincer-type impingement.
METHODS
Patients undergoing treatment of femoroacetabular impingement with a minimum follow-up period of one year were selected at the Hip Surgery Group, Department of Orthopedics and Traumatology, School of Medical Sciences, Santa Casa de Sāo Paulo. Between August 2003 and August 2007, 36 hips were arthroscopically treated for femoroacetabular impingement. The average follow-up period was 27 months (12 to 60 months). All patients were reevaluated. Eight patients who already had osteoarthritis at the initial examination (Tönnis et al. classification(13) grades 2 and 3) were excluded, and the remaining total of 28 patients were analyzed.
The patients' ages ranged from 21 to 55 years (mean of 34 years). There was male predominance in 19 cases (67%). Fifteen patients (53%) engaged in regular physical activity, 13 (86%) as amateurs and two as professionals (14%). The duration of preoperative complaints ranged from six to 96 months (mean of 26.3 months). On physical examination, all patients had pain upon 90° of flexion and internal rotation of the hip.
Regarding clinical improvement, patients were evaluated pre- and postoperatively using the Harris Hip Score (HHS) modified by Byrd(14). Results were stratified into poor (HHS < 70 points), fair (HHS 70-79), good (HHS 80-89), and excellent (HHS 90-100).
Patients were evaluated pre- and postoperatively with regard to internal rotation of the affected hip. Measurement was performed in the supine position with 90° of flexion and maximum internal hip rotation.
All patients were operated and evaluated by the same surgeon (GCP).
The values obtained in the above indices were statistically analyzed using the Wilcoxon method for the evaluation of nonparametric variables.
All patients were assessed through radiographs (AP pelvis, cross-table, Lequesne false profile) and magnetic resonance imaging or magnetic resonance arthrography when necessary. When arthro-MRI was performed, marcaine was injected intra-articularly as an adjuvant in confirming the intra-articular etiology of the pain. Computed tomography was performed as needed and was useful for mapping the acetabular rim and the femoral head-neck junction. It is important to emphasize the technical precision required to perform X-rays, since positioning errors can affect the interpretation of the acetabular version and thus mask or distort pincer-type lesions.
The portals used followed descriptions by Philippon and Schenker(15). Generally, two portals were sufficient: the anterior and the anterior paratrochanteric. Alternative portals were used as needed. Seventy degree optics were used in all cases. First, the central compartment was operated, diagnosing and treating changes in the articular cartilage, labral lesions, or round ligament lesions. The acetabular labrum was debrided or repaired, depending on the appearance of the labral tissue, the location of the lesion or the presence of pincer-type impingement, and preserved whenever possible. Outerbridge classification IV full-thickness chondral lesions were treated as follows: if associated with pincer-type impingement, the acetabular rim underwent osteoplasty, which usually only resulted in macroscopic cartilage with a healthy appearance, without the need for microfracture. If the full-thickness chondral defect remained after osteochondroplasty or if the edge osteochondroplasty was not indicated, microfractures were performed. In cases where there was total lesion of the round ligament, the round ligament was debrided. Afterwards, the peripheral compartment was operated, releasing traction, and allowing for the passage of optics into the peripheral region of the femoral head-neck junction. Once the region of the cam-type impingement was defined by local morphological changes or dynamic examination of the joint, osteochondroplasty was performed. The procedure was considered finished when the test with 90° flexion, adduction, and internal hip rotation of 30° was performed and rubbing of the neck against the acetabular rim was no longer seen.
Figure 3.
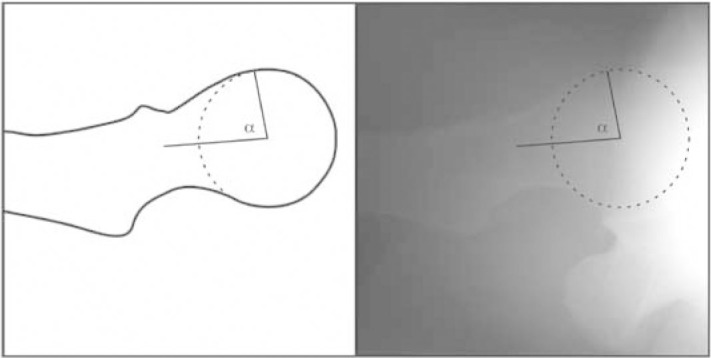
Cross-table X-ray of the right hip: decreased head-neck offset with an 82° a angle.
Figure 4.
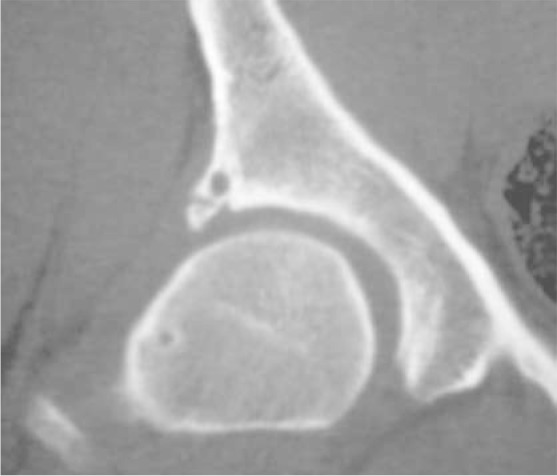
Coronal CT scan of the right hip where a perilabial cyst, calcification of the base of the acetabular labrum, and an impingement cyst on the femoral neck are observed.
Figure 5.

Anteroposterior radiograph of the left hip, in which acetabular retroversion is visible, with a crossing sign and the ischial spine visible in the pelvic cavity. AW: anterior wall, PW: posterior wall.
RESULTS
The average preoperative Harris Hip Score was 58.1 (SD = 13.5, ranging from 22 to 84.7). The average postoperative HHS was 96.9 (SD = 4.35, ranging from 66 to 100). The average increase in the HHS pre- to post-surgery was 38.7 points.
The pre- and postoperative HHS values were analyzed (SPSS version 10.0, SPSS, Chicago, IL, USA). The Wilcoxon test was used to analyze the nonparametric variables. We found a statistically significant difference between the pre- and postoperative HHS values (P < 0.001).
Stratifying the HHS results, we had four good (15%) and 24 excellent (85%) results. There was one case of transient paresthesia of the penile region, which resolved in three weeks. After modification of the perineal post(16), there were no further complications regarding the postoperative changes of the pudendal nerve.
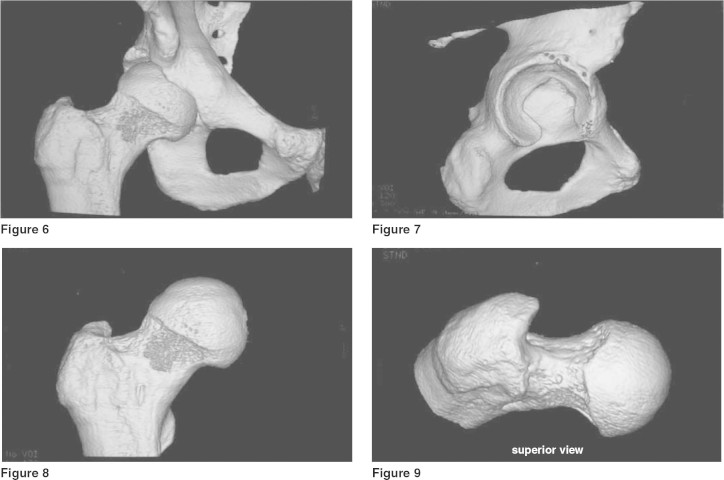
Figures 6, 7, 8 and 9.
Computed tomography reconstruction in three dimensions, where we see the result of the femoral and acetabular osteochondroplasty. Figure 7 – Observe the holes at the sites for the placement of the anchors for labral reattachment.
Regarding the treatment of labral lesions, 20 hips underwent debridement and eight labra were repaired with anchors. Since this was a consecutive series of patients, it is noteworthy that the labra were repaired/reinserted in most of the recent cases.
All patients showed an internal rotation limitation of the affected hip preoperatively with an average internal rotation of 17° (SD = 16.9, ranging from -15° to 45°). The patients showed increased internal rotation mobility of the operated hip, with an average internal rotation of 36° (SD = 11.6, ranging from 0° to 50°). The average increase in internal rotation was 19°, ranging from 0 to 40°.
The Wilcoxon test was performed to analyze the nonparametric variables. We found a statistically significant difference between preoperative and postoperative values of internal hip rotation (P < 0.001).
There were no cases of aseptic necrosis of the hip, heterotopic ossification, neck fracture, or infection.
DISCUSSION
Based on the clinical experience of more than 700 surgical hip dislocations(4), Ganz et al. argue that femoroacetabular impingement leads to the development of precocious osteoarthritis in non-dysplastic hips(5). The concept is based more on the movement than on the axial loading of the hip. The impingement may result from morphological abnormalities affecting the acetabulum and the proximal femur or may occur in patients subjecting the hip to an extreme and supraphysiological range of motion. Depending on the underlying cause, the femoroacetabular impingement results in injury to the labrum and the acetabular cartilage.
Clinical, radiographic, and intraoperative parameters may be used to confirm the diagnosis2, 5, 6, 7, 8, 17. Surgical treatment of femoroacetabular impingement is based on improving the range of motion, alleviating the impingement of the femur against the acetabular rim and its consequences. It is believed that early surgical intervention, besides relieving the symptoms, can slow the progression of the degenerative process.
Figure 10.
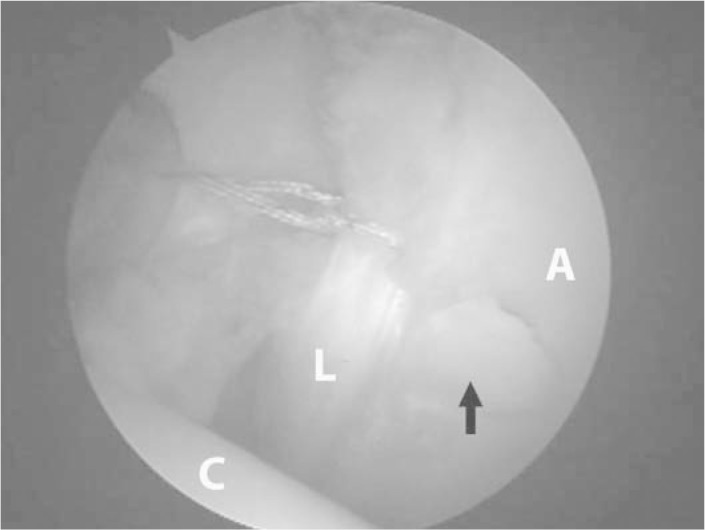
Labral reattachment after osteochondroplasty of acetabular overcoverage. A chondral lesion is observed in the “watershed” area (arrow). H: femoral head, L: acetabular labrum, A: acetabular cartilage. (Image courtesy of Dr. Giancarlo Polesello).
The recognition of femoroacetabular impingement requires careful analysis of small abnormalities of the proximal femur, as well as abnormalities in the orientation or depth of the acetabulum, which may cause movements to be difficult. Internal rotation is the most critical movement. This issue is not new. In 1911, Preiser(18) already speculated about the relationship between reduced internal rotation and the subsequent development of osteoarthritis; however, the modern concept of femoroacetabular impingement was described only a decade ago(5). Although the femoroacetabular impingement can be localized anywhere in the joint, the most common site is the anterolateral region, produced by the internal rotation of the femur in 90° of hip flexion. In the anterior impingement test, performed by maximum internal rotation and 90° of passive flexion of the hip, there is a decrease in internal hip rotation and associated pain. Hip flexion and adduction lead to conflict between the femoral neck and the acetabular rim. Associated internal rotation causes shearing forces on the acetabular labrum, similarly to the meniscus of the knee, stimulating the nerve endings. This causes acute inguinal pain in patients with a torn or degenerated labrum(6). High speed movements are more destructive than low speed impact, which makes athletes and patients who perform strenuous physical activity more susceptible to them(15).
Two distinct types of femoroacetabular impingement have been identified(5) and are often combined(7). The first is characterized by linear impingement of the acetabular rim against the femoral head-neck junction due to acetabular overcoverage, which is called pincer-type. The second type occurs with compression of the non-spherical extension of the femoral head in the acetabular cavity, called the cam-type.
Impingements with femoral causes (idiopathic, epiphysiolysis, post-traumatic retroversion of the femoral head, deformity secondary to Perthes disease, or avascular necrosis of the femoral head) are named cam-type impingements, and were described in 1968 by Carlioz et al.(3) The non-spherical segment of the head or of the head-neck junction is compressed within the acetabulum, causing abrasion from the “outside-in” or avulsion of the articular cartilage, while the labrum at first remains intact(2). Over time, the substance of the detached labrum degenerates, while the lateral rim region retains its normal texture for a long period(6), allowing for reattachment(19). The preservation of any healthy portion of the labrum is important due to the fact that the labrum functions as a joint lubricator, distributor of pressure, and shock absorber in the normal hip. Successful reattachment has been confirmed by arthro-MRI and arthroscopy. The cartilage that covers the spherical part of the head remains intact for a long period, unlike the cartilage from the non-spherical portion, which shows signs of progressive degeneration(2).
Impingement from acetabular causes (idiopathic retroversion and other types, coxa profunda, and acetabular protrusion) is called pincer-type impingement. There is evidence that idiopathic retroversion is more of a pelvic than an acetabular pathomorphological change(17). With the retroversion of the acetabulum, the ischial spine becomes visible in the pelvic cavity in most cases. The pincer-type impingement is produced by the linear collision between the femoral head-neck junction and the area of acetabular overcoverage. The fact that the labrum is squeezed and contains nerve endings may explain why this kind of impingement, often found in women, is more painful than the cam-type. With the chronic impingement of the acetabular labrum, degeneration and intrasubstance cyst formation occur. The chronic irritation mechanism can cause bone apposition in the acetabular rim that, by progressive growth, causes thinning of the labrum and increases overcoverage, worsening the impingement(2).
The femoral head remains intact for long periods and, in later stages, cartilage abrasion occurs in the posterior-inferior articular region of the head and/or the acetabulum, leading to changes called “countrecoup injuries” later resulting in posteromedial arthritis of the hip(7). Although more painful, pincer-type impingement causes smaller and slower destruction of the articular cartilage.
The pincer-type impingement is most commonly found in women between 30 and 40 years who perform activities with a large range of motion. The cam–type impingement is typically found in men between 20 and 30 years(2). Beck et al.(7) reported that most cases are mixtures of these two types.
Conservative treatment may even be tried at first, with restriction of athletic activities and the use of NSAIDs. Physical therapy conducted in order to gain range of motion or stretching can result in the worsening of symptoms, especially if it is oriented to the flexion and adduction of the hip. Treatment may temporarily be successful due to the young age of these patients; however, due to a high level of physical activity and sports, it often fails. Because it is an anatomical problem, which has been proven to lead to the progressive destruction of the labrum and articular cartilage and subsequent osteoarthritis, surgical treatment should be performed early in the failure of conservative treatment.
Treatment of impingement is not a new issue. In 1936, Smith-Petersen described femoroacetabular impingement, including treatment for it with acetabular and femoral osteoplasty(20). His poor results may have occurred for having done such interventions in hips with advanced osteoarthritis. We know today that this is not likely to provide good results.
Surgical treatment of femoroacetabular impingement consists of remodeling of the proximal femur, osteoplasty, or reorientation of the acetabular overcoverage and labral repair/reattachment or debridement. Several surgical techniques have been described for the treatment of femoroacetabular impingement, namely periacetabular osteotomy(8), surgical dislocation of the hip(4), arthroscopy with osteochondroplasty through a small incision(21), modified anterior technique(22), and arthroscopy15, 23.
The approach should be chosen according to the complexity of the morphology of the femoroacetabular impingement and the surgeon's training.
Hip arthroscopy has been around for over 15 years(24); however, its use for the treatment of FAI is recent. Advances in arthroscopic techniques, particularly the incorporation of dynamic intraoperative assessment of the impingement, have allowed the FAI to be addressed in a less invasive manner. Arthroscopic anatomy has been thoroughly studied, having established well-defined and safe arthroscopic portals(25) and an anatomical technique for the preservation of the vascularity of the femoral neck(26). Labral repair is possible by arthroscopy(27). The surgeon must be familiar with arthroscopic anatomy, since it may be difficult to orient to the site and the amount of bone resection required, and may lead to insufficient correction and subsequent residual impingement or even excessive resection, which is associated with a risk of femoral neck fracture or instability(28). Anatomical studies have shown neck osteoplasty via open and arthroscopic surgery by trained surgeons to have the same precision(29), and clinical studies have demonstrated the effectiveness of the restoration of femoral offset by arthroscopy(30). Thus, we believe that there is support for stating that arthroscopic treatment of FAI is feasible and reproducible.
Siebenrock et al. (8) evaluated 29 hips that had undergone periacetabular osteotomy due to acetabular retroversion, with a mean follow-up period of 30 months, with good and excellent results in 26 hips (89%).
Regarding surgical treatment for surgical dislocation, Beck et al.(10) obtained excellent results in 68% of cases. Murphy et al.(11) observed that 65% of operated patients, with follow-up for two to 12 years, did not require further intervention. Peters and Erickson(12) evaluated 30 patients, HHS improved from an average of 70 preoperatively to 87 on the most recent postoperative exam. Parvizi et al.(31) reported that 76% of patients had excellent or good results, with an average follow-up period of 4.7 years.
Zebala et al.(32), using the arthroscopic technique with osteochondroplasty via a small incision, with a mean follow-up of 1.5 years, reported a mean preoperative HHS of 63.8 and 92.3 postoperatively, totaling 95.8% good and excellent results.
Ribas et al.(22) reported improvement in pain in all cases using the modified Smith-Petersen access.
As for arthroscopic treatment, Larson and Giveans(33) evaluated the treatment of 47 patients with at least three months of follow-up (mean 9.9 months): 26 hips (55.3%) were rated as excellent, nine (19.1%) as good, five (10.6%) as fair, and seven (14.9%) as poor. The preoperative modified HHS averaged 60.4, 72.8 at six weeks, 81.6 at three months, 83.1 at six months, and 85.4 at one year. Philippon et al.(34) evaluated 45 professional athletes, all with relief of symptoms and return to sports. Sampson(23) evaluated 320 patients, 90% with the sign of impingement eliminated and satisfied with the result. Ilizaturri et al.(35) evaluated 19 patients with cam-type impingement, with a minimum of two years of follow-up; 84% showed improvement of symptoms.
Our results are consistent with the published studies which have an average of 75% to 95% good results. In our study, the average Harris Hip Score was 58.1 preoperatively and 96.9 postoperatively, with an average HHS increase of 38.7 points, results that are also consistent with the literature. What we learned is that the detailed indication of the cases is key to producing good results, because poor indications lead to poor results. From the results of several studies8, 10, 23, 36, it has been observed that patients with radiographic signs of osteoarthritis are not good candidates for preservative surgery.
In a comparison of clinical studies on the extent of internal rotation in femoroacetabular impingement, Eijer et al.(37) evaluated nine patients with post-traumatic cam-type impingement; preoperative internal rotation averaged 7°, with an average increase of 9° after resection of bone outgrowth via open surgery. Siebenrock et al.(8) evaluated 29 patients with pincer-type impingement with a mean preoperative internal rotation of 11° who underwent periacetabular osteotomy with a postoperative mean of 21°. Leunig et al.(38) evaluated 14 patients with unspecified femoroacetabular impingement and a preoperative internal rotation averaging 15° (SD = 12). The authors did not report postoperative mobility in this study. Jager et al.(8) evaluated 17 patients with cam-type impingement, with a mean preoperative internal rotation of 8°, who underwent open resection of bony outgrowth with a postoperative mean of 21.7°. Strehl and Ganz(39) evaluated 11 patients with post-traumatic cam-type impingement who had a preoperative internal rotation averaging 15°, who underwent open resection of bony outgrowth, with a postoperative mean of 20°. Wettstein and Dienst(40) evaluated 15 patients with mixed-type impingement that had a preoperative internal rotation of 7° (SD = 12); patients underwent arthroscopy and postoperative mobility was not reported. In a computer simulation of joint mobility acquired through computed tomography, the average internal rotation gain of pincer-type impingement correction was 5.4°, 8.5° for cam-type impingement, and 15.7° for mixed-type impingement(41). Ribas et al.(22) evaluated 14 patients with a mean preoperative internal rotation of -17° (-14° to -28°) who underwent osteochondroplasty via anterior access, with a postoperative mean of 23° (14° to 32°). Stähelin et al.(30) evaluated 23 patients with cam-type impingement with a mean preoperative internal rotation of 5°, who underwent arthroscopic repair with a postoperative mean of 22°. The average postoperative gain in internal rotation was 19° in our study, which is consistent with the literature. Most cases in our series were a mixed-type impingement.
There are some limitations to this study. One is the lack of a control group for the evaluation of treatment outcomes. Another is having sufficient literature to allow for the comparison of results, including the open technique. There is only one (preliminary) study prospectively comparing open and arthroscopic treatment, conducted by Sadri and Hoffmeyer(42), where good results have been demonstrated using both techniques, suggesting that arthroscopic treatment may have the advantage of avoiding the complications of open surgery. Many published studies do not use the same criteria for evaluating postoperative functionality. The HHS is a great tool for functional assessment; however, other authors are developing new clinical scoring systems.
The degree of improvement in our patients is consistent with other studies of open and arthroscopic treatment.
Another point worth discussing is labrum repair. Tannast et al.(43) conducted a study correlating intraoperative findings with computer simulations of the region of greatest femoroacetabular impingement. An association was observed between the presence of labral lesions and degeneration of the adjacent articular surface, which is seen mainly in arthroscopic procedures(44). However, what these studies have in common is that they fail to satisfactorily explain the cause of joint damage. Most authors describe a direct trauma during sports activity as the etiology of labral lesions. In fact, they rarely occur in the absence of morphological changes in bone(45). Therefore, the results of arthroscopic labrum debridement alone without treatment of the underlying anatomical changes (in most cases FAI) are unsatisfactory(46). In our opinion, the vast majority of cases of labral lesions are associated with femoroacetabular impingement, with the acetabular labrum being the first structure to fail(6).
Labrum degeneration has been observed in cases of OA(47). Ikeda et al.(48) postulated that acetabular labrum injuries can compromise their load absorption and stabilization functions, leading to arthritis, similar to that found in meniscal injuries. Finite element studies have shown that, by compromising the sealing functions of the labrum, the cartilaginous stress and shear forces that can contribute to fatigue damage of the adjacent cartilage increase. McCarthy et al.(44) also found an association between labral lesions and lesions of the adjacent cartilage, suggesting that labral lesions and osteoarthritis are a continuum of disease.
Due to the larger forces at the hip joint, labrum reattachment can be challenging. However, even with the development of a sufficiently strong anchoring mechanism, the labral biological matrix's ability to regenerate is required. What leads us to have positive expectations is that Ito et al.(6) observed that, even in advanced cases of osteoarthritis, the tip of the labrum, its place of irrigation, is preserved, allowing for its repair.
Byrd and Jones(36) evaluated 30 hips treated with debridement for a labral lesion. Labral lesions were debrided until they became stable. After 10 years of follow-up, patients showing no signs of arthritis had 82% good results, with a mean preoperative HHS of 54 and 90 postoperatively. They note that 88% of patients with osteoarthritis had to be converted to total hip arthroplasty.
Espinosa et al.(19) evaluated the effect of debridement compared with labrum repair/reattachment and found better results in the group undergoing labrum repair after two years of follow-up in regards to pain and the progression of osteoarthritis. It is unclear whether the best results came from a more refined technique or from preserving the labrum, as this was a consecutive series of patients.
Based on all of these claims, although there are still insufficient clinical observations to state that labrum repair leads to better results, we believe it is justified. There is a need to establish criteria for possible labrum preservation/repair. Our results require longer follow-up to compare the significance of the results from the different treatments.
The minimum follow-up used for the evaluation of our series was one year. In the series of Larson and Giveans(33), analysis of the HHS showed improvement in the results, though without any significant improvement after three months of follow-up; it could be interpreted that three months of follow-up time may be enough to evaluate the patients' improvement. On the other hand, Sampson(22) evaluated 158 patients and found a 50% improvement in pain at three months, 75% at five months, and 95% at one year. There was insufficient data in our series to assess this progression. So we opted for a one-year minimum follow-up period. New data will allow us to assess whether there really is a period of improvement up to two years, when there is a new drop in function in patients with poor prognosis (Byrd, personal communication).
According to the literature49, 50, the incidence of complications varies from 0.5 to 5% of cases, with the most common being neuropraxia due to traction. In an analysis of our data16, 50, most complications occurred due to traction (3.6%). After modification of the perineal post, there were no further complications regarding the postoperative changes of the pudendal nerve. Our rates are consistent with those reported in the literature.
Open surgical treatment of FAI is considered the standard; however, as first happened with knee arthroscopy and later with that of the shoulder, a series of injuries came to be treated by arthroscopy. Caution is necessary to prevent an uncontrolled growth of hip arthroscopic procedures, avoiding the phenomenon that occurred in abdominal surgery, where there was an increase in the number of cholecystectomy with the introduction of laparoscopy. Likewise, it is necessary to establish what injury patterns are better treated by open or arthroscopic surgery.
In conclusion, the results of the treatment of femoroacetabular impingement have been promising in the absence of significant chondral lesions at surgery. The prognosis of the hip is significantly better if the impingement is eliminated early(9), so surgery should be recommended when the first symptoms appear10, 11. The question remains as to what to do in cases that have definite but asymptomatic impingement or those that improve completely with conservative treatment. Our approach is to wait and operate only symptomatic patients until definitive evidence arises. The question remains regarding the permanence of the improvements in pain and the possibility of delaying the development of osteoarthritis.
CONCLUSION
The arthroscopic treatment of femoroacetabular impingement produces satisfactory results.
Footnotes
Study conducted at the Department of Orthopedics and Traumatology, School of Medical Sciences, Santa Casa de Sāo Paulo. Director: Dr. Osmar Avanzi
REFERENCES
- 1.Murray RO. The aetiology of primary osteoarthritis of the hip. Br J Radiol. 1965;38(455):810–824. doi: 10.1259/0007-1285-38-455-810. [DOI] [PubMed] [Google Scholar]
- 2.Ganz R, Leunig M, Leunig-Ganz K, Harris WH. The etiology of osteoarthritis of the hip: an integrated mechanical concept. Clin Orthop Relat Res. 2008;466(2):264–272. doi: 10.1007/s11999-007-0060-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Carlioz H, Pous JG, Rey JC. Les epiphysiolyses femorales superieures. Rev Chir Orthop Reparatrice Appar Mot. 1968;54(5):387–491. [PubMed] [Google Scholar]
- 4.Ganz R, Gill TJ, Gautier E, Ganz K, Krügel N, Berlemann U. Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br. 2001;83(8):1119–1124. doi: 10.1302/0301-620x.83b8.11964. [DOI] [PubMed] [Google Scholar]
- 5.Ganz R, Parvizi J, Beck M, Leunig M, Nötzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;(417):417–420. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 6.Ito K, Leunig M, Ganz R. Histopathologic features of the acetabular labrum in femoroacetabular impingement. Clin Orthop Relat Res. 2004;(429):262–271. doi: 10.1097/01.blo.0000144861.11193.17. [DOI] [PubMed] [Google Scholar]
- 7.Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87(7):1012–1018. doi: 10.1302/0301-620X.87B7.15203. [DOI] [PubMed] [Google Scholar]
- 8.Siebenrock KA, Schoeniger R, Ganz R. Anterior femoro-acetabular impingement due to acetabular retroversion. Treatment with periacetabular osteotomy. J Bone Joint Surg Am. 2003;85-A(2):278–286. doi: 10.2106/00004623-200302000-00015. [DOI] [PubMed] [Google Scholar]
- 9.Crestani MV, Teloken MA, Gusmão PDF. Impacto femoroacetabular: uma das condições precursoras da osteoartrose do quadril. Rev Bras Ortop. 2006;41(8):285–293. [Google Scholar]
- 10.Beck M, Leunig M, Parvizi J, Boutier V, Wyss D, Ganz R. Anterior femoroacetabular impingement: part II. Midterm results of surgical treatment. Clin Orthop Relat Res. 2004;(418):67–73. [PubMed] [Google Scholar]
- 11.Murphy S, Tannast M, Kim YJ, Buly R, Millis MB. Debridement of the adult hip for femoroacetabular impingement: indications and preliminary clinical results. Clin Orthop Relat Res. 2004;(429):178–181. doi: 10.1097/01.blo.0000150307.75238.b9. [DOI] [PubMed] [Google Scholar]
- 12.Peters CL, Erickson JA. Treatment of femoro-acetabular impingement with surgical dislocation and debridement in young adults. J Bone Joint Surg Am. 2006;88(8):1735–1741. doi: 10.2106/JBJS.E.00514. [DOI] [PubMed] [Google Scholar]
- 13.Busse J, Gasteiger W, Tönnis D. Eine neue methode zur röntgenologischen beurteilung eines hüftgelenkes — der hüftwert. Arch Orthop Unfallchir. 1972;72(1):1–9. doi: 10.1007/BF00415854. [DOI] [PubMed] [Google Scholar]
- 14.Byrd JW. Avoiding the labrum in hip arthroscopy. Arthroscopy. 2000;16(7):770–773. doi: 10.1053/jars.2000.7686. [DOI] [PubMed] [Google Scholar]
- 15.Philippon MJ, Schenker ML. Arthroscopy for the treatment of femoroacetabular impingement in the athlete. Clin Sports Med. 2006;25(2):299–308. doi: 10.1016/j.csm.2005.12.006. [DOI] [PubMed] [Google Scholar]
- 16.Polesello GC, Honda EK, Souza BGC, Guimarães RP, Junior WR, Ono NK. 12° Congresso de Ortopedia e Traumatologia do Estado de São Paulo (COTESP). Campinas, SP, 2008. Sociedade Brasileira de Ortopedia e Traumatologia; São Paulo: 2008. Poste Perineal modificado para artroscopia de quadril: um equipamento mais seguro para tração articular. [Google Scholar]
- 17.Jamali AA, Mladenov K, Meyer DC, Martinez A, Beck M, Ganz R. Anteroposterior pelvic radiographs to assess acetabular retroversion: high validity of the “cross-over-sign“. J Orthop Res. 2007;25(6):758–765. doi: 10.1002/jor.20380. [DOI] [PubMed] [Google Scholar]
- 18.Preiser G. Statische Gelenkerkrankungen. Enke, Stuttgart; 1911. p.78
- 19.Espinosa N, Rothenfluh DA, Beck M, Ganz R, Leunig M. Treatment of femoroacetabular impingement: preliminary results of labral refixation. J Bone Joint Surg Am. 2006;88(5):925–935. doi: 10.2106/JBJS.E.00290. [DOI] [PubMed] [Google Scholar]
- 20.Smith-Petersen MN. Treatment of malum coxae sinilis, old slipped upper femoral epiphysis, intrapelvic protusion of the acetabulum, and coxa plana by means of acetabuloplasty. J Bone Joint Surg Am. 1936;18:869–880. doi: 10.1007/s11999-008-0670-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Clohisy JC, McClure JT. Treatment of anterior femoroacetabular impingement with combined hip arthroscopy and limited anterior decompression. Iowa Orthop J. 2005;25:164–171. [PMC free article] [PubMed] [Google Scholar]
- 22.Ribas M, Ginebreda I, Candioti L, Vilarrubias JM. Surgical treatment of the anterior femoroacetabular impingement syndrome of the hip. J Bone Joint Surg Br. 2005;87(Suppl 1):84. [Google Scholar]
- 23.Sampson TG. Arthroscopic treatment of femoroacetabular impingement: a proposed technique with clinical experience. Instr Course Lect. 2006;55:337–346. [PubMed] [Google Scholar]
- 24.Lage LA, Costa RC. Artroscopia do quadril: indicações e técnica. Rev Bras Ortop. 1995;30(8):555–558. [Google Scholar]
- 25.Robertson WJ, Kelly BT. The safe zone for hip arthroscopy: a cadaveric assessment of central, peripheral, and lateral compartment portal placement. Arthroscopy. 2008;24(9):1019–1026. doi: 10.1016/j.arthro.2008.05.008. [DOI] [PubMed] [Google Scholar]
- 26.Sussmann PS, Ranawat AS, Shehaan M, Lorich D, Padgett DE, Kelly BT. Vascular preservation during arthroscopic osteoplasty of the femoral head-neck junction: a cadaveric investigation. Arthroscopy. 2007;23(7):738–743. doi: 10.1016/j.arthro.2007.01.025. [DOI] [PubMed] [Google Scholar]
- 27.Kelly BT, Weiland DE, Schenker ML, Philippon MJ. Arthroscopic labral repair in the hip: surgical technique and review of the literature. Arthroscopy. 2005;21(12):1496–1504. doi: 10.1016/j.arthro.2005.08.013. [DOI] [PubMed] [Google Scholar]
- 28.Mardones RM, Gonzalez C, Chen Q, Zobitz M, Kaufman KR, Trousdale RT. Surgical treatment of femoroacetabular impingement: evaluation of the effect of the size of the resection. J Bone Joint Surg Am. 2005;87(2):273–279. doi: 10.2106/JBJS.D.01793. [DOI] [PubMed] [Google Scholar]
- 29.Sussmann PS, Ranawat AS, Lipman J, Lorich DG, Padgett DE, Kelly BT. Arthroscopic versus open osteoplasty of the head-neck junction: a cadaveric investigation. Arthroscopy. 2007;23(12):1257–1264. doi: 10.1016/j.arthro.2007.07.012. [DOI] [PubMed] [Google Scholar]
- 30.Stähelin L, Stähelin T, Jolles BM, Herzog RF. Arthroscopic offset restoration in femoroacetabular cam impingement: accuracy and early clinical outcome. Arthroscopy. 2008;24(1):51–57. doi: 10.1016/j.arthro.2007.08.010. [DOI] [PubMed] [Google Scholar]
- 31.Parvizi J, Ganz R, Beck M, Leunig M, Sibenrock K. Femoroacetabular impingement: mid-term clinical results. Abstracts from the AAHKS Thirteenth Annual Meeting. J Arthroplasty. 2004;19:261–262. [Google Scholar]
- 32.Zebala L, Clohisy JC, Hinkle S, McClure JT, Robison JF. Adult reconstruction hip 5: nonarthroplasty operative treatments, economic issues and miscellaneous. Combined hip arthroscopy and limited open osteochondroplasty for treating impingement disease. [Podium 468]. In: 2007 Annual Meeting Podium Presentations. San Diego: American Academy of Orthopaedic Surgeons, American Association of Orthopaedic Surgeon; 2007.
- 33.Larson CM, Giveans MR. Arthroscopic management of femoroacetabular impingement: early outcomes measures. Arthroscopy. 2008;24(5):540–546. doi: 10.1016/j.arthro.2007.11.007. [DOI] [PubMed] [Google Scholar]
- 34.Philippon M, Schenker M, Briggs K, Kuppersmith D. Femoroacetabular impingement in 45 professional athletes: associated pathologies and return to sport following arthroscopic decompression. Knee Surg Sports Traumatol Arthrosc. 2007;15(7):908–914. doi: 10.1007/s00167-007-0332-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ilizaliturri VM, Jr, Orozco-Rodriguez L, Acosta-Rodríguez E, Camacho-Galindo J. Arthroscopic treatment of cam-type femoroacetabular impingement. Arthroplasty. 2008;23(2):226–234. doi: 10.1016/j.arth.2007.03.016. [DOI] [PubMed] [Google Scholar]
- 36.Byrd JWT, Jones KS. Hip arthroscopy for labral pathology: prospective analysis with 10-year follow-up (SS-57) Arthroscopy. 2008;24(6):e32–e33. doi: 10.1016/j.arthro.2009.02.001. [DOI] [PubMed] [Google Scholar]
- 37.Eijer H, Myers SR, Ganz R. Anterior femoroacetabular impingement after femoral neck fractures. J Orthop Trauma. 2001;15(7):475–481. doi: 10.1097/00005131-200109000-00003. [DOI] [PubMed] [Google Scholar]
- 38.Leunig M, Podeszwa D, Beck M, Werlen S, Ganz R. Magnetic resonance arthrography of labral disorders in hips with dysplasia and impingement. Clin Orthop Relat Res. 2004;(418):74–80. doi: 10.1097/00003086-200401000-00013. [DOI] [PubMed] [Google Scholar]
- 39.Strehl A, Ganz R. Anterior femoroacetabular impingement after healed femoral neck fractures. Unfallchirurg. 2005;108(4):263–273. doi: 10.1007/s00113-004-0886-8. [DOI] [PubMed] [Google Scholar]
- 40.Wettstein M, Dienst M. Hip arthroscopy for femoro-acetabular impingement. Orthopade. 2006;35(1):85–93. doi: 10.1007/s00132-005-0897-3. [DOI] [PubMed] [Google Scholar]
- 41.Kubiak-Langer M, Tannast M, Murphy SB, Siebenrock KA, Langlotz F. Range of motion in anterior femoroacetabular impingement. Clin Orthop Relat Res. 2007;458:117–124. doi: 10.1097/BLO.0b013e318031c595. [DOI] [PubMed] [Google Scholar]
- 42.Sadri H, Hoffmeyer P. Treatment of femoroacetabular impingement by hip arthroscopy compared to open surgery with a minimum 2 year follow-up. In: Advances in Hip Arthroscopy Meeting. Paris; 2006.
- 43.Tannast M, Goricki D, Beck M, Murphy SB, Siebenrock KA. Hip damage occurs at the zone of femoroacetabular impingement. Clin Orthop Relat Res. 2008;(466):466–480. doi: 10.1007/s11999-007-0061-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.McCarthy JC, Noble PC, Schuck MR, Wright J, Lee J. The Otto E. Aufranc Award: The role of labral lesions to development of early degenerative hip disease. Clin Orthop Relat Res. 2001;(393):25–37. doi: 10.1097/00003086-200112000-00004. [DOI] [PubMed] [Google Scholar]
- 45.Wenger DE, Kendell KR, Miner MR, Trousdale RT. Acetabular labral tears rarely occur in the absence of bony abnormalities. Clin Orthop Relat Res. 2004;(426):145–150. doi: 10.1097/01.blo.0000136903.01368.20. [DOI] [PubMed] [Google Scholar]
- 46.Kim KC, Hwang DS, Lee CH, Kwon ST. Influence of femoro-acetabular impingement on results of hip arthroscopy in patients with early osteoarthritis. Clin Orthop Relat Res. 2007;(456):128–132. doi: 10.1097/01.blo.0000246542.49574.2c. [DOI] [PubMed] [Google Scholar]
- 47.Lage LA, Costa RC. Villar RN. A importincia do “labrum” acetabular: revisão da literatura. Rev Bras Ortop. 1996;31(10):792–796. [Google Scholar]
- 48.Ikeda T, Awaya G, Suzuki S, Okada Y, Tada H. Torn acetabular labrum in young patients: arthroscopic diagnosis and management. J Bone Joint Surg Br. 1988;70(1):13–16. doi: 10.1302/0301-620X.70B1.3339044. [DOI] [PubMed] [Google Scholar]
- 49.Clarke MT, Arora A, Villar RN. Hip arthroscopy: complications in 1054 cases. Clin Orthop Relat Res. 2003;(406):84–88. doi: 10.1097/01.blo.0000043048.84315.af. [DOI] [PubMed] [Google Scholar]
- 50.Polesello GC, Honda EK, Souza BGC, Dani WS, Guimarães RP, Junior WR, et al. Complicações em artroscopia do quadril. In: 12° Congresso de Ortopedia e Traumatologia do Estado de São Paulo (COTESP). Campinas, SP, 2008. São Paulo: Sociedade Brasileira de Ortopedia e Traumatologia; 2008.