Abstract
Objective: this study aims to compare the arthrometric and isokinetic examination results from two types of autologous grafts: the central third of the patellar ligament and a graft formed by the tendons of the semitendinosus and gracilis muscles, within the same rehabilitation protocol, six months after the surgery. Methods: the results from examinations carried out on 63 patients were analyzed. These patients were divided in two groups: one group of 30 patients who received a patellar tendon graft and another group of 33 patients who received a graft from the tendons of the semitendinosus and gracilis muscles. Both the grafts were attached in the same way, with Endobutton™ for suspensory fixation to the femur and a bioabsorbable interference screw for fixation in the tibial tunnel. Results: arthrometry 30 did not present any statistical difference between the two study groups. On the other hand, the isokinetic evaluation showed that the patellar tendon group had a larger mean peak torque of flexion and greater extension deficit, while the semitendinosus/gracilis group had a better mean flexion/extension ratio and greater percentage of flexion deficit. There was no statistically significant difference between the groups when measuring peak torque extension. Conclusion: therefore, when the patellar tendon was used, there was greater extensor deficit and, when the semitendinosus/gracilis tendons were used, there was greater flexor deficit.
Keywords: Anterior cruciate ligament, Knee, Reconstruction, Arthroscopy
INTRODUCTION
The first reports of injury to the anterior cruciate ligament of the knee appear in the literature of the nineteenth century(1). The first reports of surgical reconstruction are from the early twentieth century(2), in addition to Campbell's report(3).
Over the past 30 years, several surgical techniques for ACL reconstruction using the structures surrounding the knee have been described. A long path was taken before returning to the technique described by Campbell(3) in 1939, which used the patellar ligament. In the same year, Macey(4) described the first technique using the flexor tendons, the semitendinosus and gracilis (ST-G).
Today, through technological advances, intra-articular reconstruction by arthroscopy reduced postoperative morbidity, though there is still debate among surgeons as to the best graft to be used.
The objective of this paper is to analyze the results of surgical treatment in ACL reconstructions through isokinetic evaluation and arthrometry according to the type of graft chosen.
METHODS
In our department, we assessed the results of 63 patients at six months post-surgery for ACL reconstruction, obtained by means of arthrometric (KT-1000™) and isokinetic (CybexTM) evaluations. Inclusion criteria were: unilateral ACL injury, no history of surgery or pathologies in either knee, and having completed a rehabilitation program with a team of physical therapists from our department.
Exclusion criteria were: age of over 60 years, previous knee surgery, bilateral ACL lesion, and completion of a rehabilitation program in another department.
Patients were divided into two groups by drawing of envelopes: we used the central third of the patellar tendon (PT) as a graft for the first group of 30 patients, and the flexor tendons of the semitendinosus and gracilis muscles (ST-G) for the second group of 33 patients.
The same surgical technique, arthroscopic intra-articular ACL reconstruction, was used in both groups, using EndobuttonTM suspensory fixation for the femur and a bioabsorbable interference screw for fixation of the tibial tunnel. Of the 30 patients in the PT group, three were women and 27 were men, aged between 16 and 37 years. The right side was affected in 18 patients and the left side in 12.
In the 33 patients of the ST-G group, five were women and 28 were men, aged between 16 and 53 years. Thirteen left knees and 20 right knees were injured.
The 63 patients underwent the same rehabilitation program, which was divided into phases. The first phase was initiated in bed with tibiofemoral and patellofemoral mobilization, light isometric exercises, unsupported gait training with crutches and the use of removable joint protection (immobilizer). On the 10th postoperative (PO) day, the second phase, the orthosis is removed and partial load is allowed. Total support and proprioception were allowed on the 14th PO day. As for range of motion (ROM), we advocated for progressive gain from the first postoperative week, reaching the total ROM in the fourth PO week. We started gait training, closed kinetic chain (CKC) exercises, advanced proprioception and mechanotherapy for the hip. Global strengthening, sport-specific proprioception, isokinetic evaluation, balance and functional tests are performed on the sixth PO month.
At the end of the sixth PO month, after isokinetic evaluation, arthrometry, and radiographs, the patient is allowed to return to sports activities.
Patients underwent arthrometric knee evaluation with the KT1000™, and three tests were performed: anterior traction tests with 15, 20 and 30 pounds of force, tests of displacement by active contraction of the quadriceps and the manual maximum anterior traction test. For the interpretation of arthrometric findings, we considered the differences between the values of the affected limb and the normal limb, considering differences larger than 3 mm suggestive of ACL injury, in addition, the positivity of any of the tests classified the patient as having an ACL injury.
The isokinetic evaluation began with 10 minutes of warm up on a stationary bicycle without weightbearing, averaging 65 to 70 rotations/min., followed by stretching the muscles of the lower limb.
First, we tested the healthy limb, followed by the operated limb. In this evaluation, the strength, power, and endurance of the flexors and extensors of the knee, quadriceps, and hamstrings are measured.
To designate the parameters, we structured the test as follows: five repetitions at 60°/second for strength, rest for one minute, five repetitions at 180°/second for power, rest for one minute, and 20 repetitions at 300°/second for resistance, thus performing a total of 30 repetitions.
For the statistics of the study, were first described the groups according to age, gender, and affected side, performing an unpaired Student's t-test(5) to compare groups with respect to age. The Fisher exact test(6) was used to determine the association between group and gender, and the chi-square test of homogeneity(6) was used to investigate the association between the group and the affected side.
An unpaired Student's t-test(5) was used to compare the groups with respect to the tests being evaluated for each measurement and the results illustrated using graphs of the measurements with their respective standard errors(5). The tests were performed at a 5% significance level.
RESULTS
The average age of the ST-G group turned out to be statistically higher than that found in the PT group (p < 0.001). The groups are statistically homogeneous according to gender (p = 0.710) and also with respect to the affected side (p = 0.102) (Tables 1 and 2).
Table 1.
Description of the age for each surgical procedure group.
| Tendon | Mean | SD | Median | Minimum | Maximum | N | p |
|---|---|---|---|---|---|---|---|
| Patellar | 25.77 | 5.38 | 25.5 | 16 | 37 | 30 | < 0.001 |
| Flexor | 33.55 | 9.80 | 33.0 | 16 | 53 | 33 | |
| Total | 29.84 | 8.85 | 30.0 | 16 | 53 | 63 |
Table 2.
Percentages for the gender and affected side for each surgical group.
| Variable | Category | Patellar tendon | Flexor | Total | p | |||
|---|---|---|---|---|---|---|---|---|
| Gender | Female | 3 | 10.0% | 5 | 15.2% | 8 | 12.7% | 0.710 |
| Male | 27 | 90.0% | 28 | 84.8% | 55 | 87.3% | ||
| Side | Right | 18 | 60.0% | 13 | 39.4% | 31 | 49.2% | 0.102 |
| Left | 12 | 40.0% | 20 | 60.6% | 32 | 50.8% | ||
| Total | 30 | 100% | 33 | 100% | 63 | 100% |
The two procedures have different results with respect to the averages of the evaluated measurements. The only measures that do not appear to be different between the two procedures are the percentage of peak extension torque (PEXTT%) and the 30-pound KT1000 (KT 30) test (Figures 1 and 2).
Figure 1.
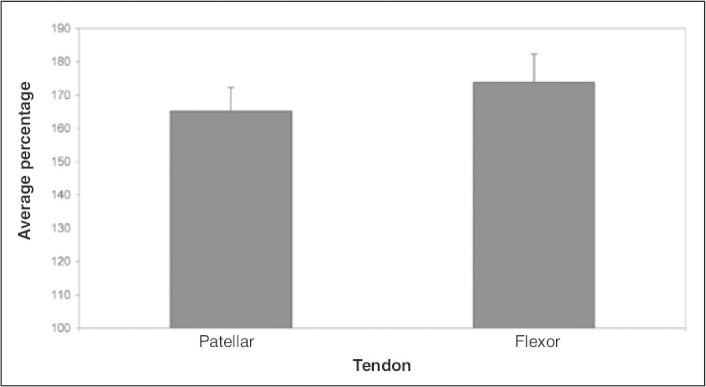
Mean values and standard errors for the PEXTT% measure.
Figure 2.
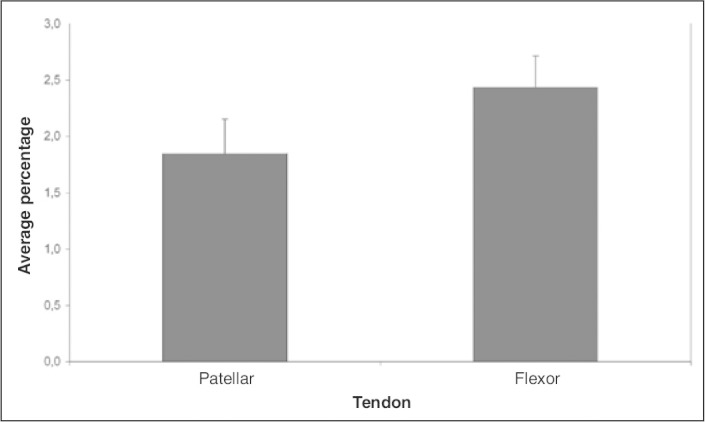
Mean values and standard errors for the KT 30 measure.
From Table 3, it is apparent that the group that uses PT has a higher average peak flexion torque (PFLT%) (p < 0.001) and greater extension deficit (p < 0.001), while the group using the ST-G has, on average, a better relationship between flexors and extensors (FL/EXT) (p < 0.001) and greater flexion deficit percentage (p = 0.048). There were no statistically significant differences between groups for PEXTT% (p = 0.448) or KT 30 measurements (p = 0.157).
Table 3.
Description of the measures evaluated for each group and results of comparative tests.
| Measurement | Patellar |
Flexor |
t value | gl | p | ||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | N | Mean | SD | N | ||||
| PFLT% | 119.18 | 23.82 | 30 | 98.09 | 21.65 | 33 | 3.68 | 61 | <0.001 |
| PEXTT% | 163.96 | 42.73 | 30 | 172.96 | 50.80 | 33 | -0.76 | 61 | 0.448 |
| FL/EXT | 75.42 | 17.79 | 30 | 59.55 | 14.98 | 33 | 3.84 | 61 | <0.001 |
| Flex. Deficit % | -1.46 | 13.24 | 30 | 5.78 | 15.06 | 33 | -2.02 | 61 | 0.048 |
| Ext. Deficit % | 29.36 | 13.30 | 30 | 14.74 | 15.29 | 33 | 4.03 | 61 | <0.001 |
| KT 30 | 1.87 | 1.43 | 30 | 2.41 | 1.57 | 33 | -1.43 | 61 | 0.157 |
| KT Min. x | 2.18 | 1.80 | 30 | 3.36 | 2.45 | 33 | -2.191 | 59 | 0.032 |
DISCUSSION
Over the past 30 years, ACL injuries have had significant changes to their therapeutic approach, returning to a technique that, in 1939, was already using the patellar ligament as a substitute for the ruptured ACL(3).
This return to old techniques was only possible due to advances in anatomical and biomechanical concepts, as well as arthroscopy with new instruments and new fixation techniques, which allow for earlier rehabilitation and better results. During these 30 years, several types of grafts have been used: autologous, allograft, and synthetic. Currently, autologous PT and ST-G grafts are preferred by Wilson and Scott(7). In our clinic, these two types of grafts are also the favorites, the choice for each patient ranging according to the type of sport, type of trauma, and their activities of daily living.
Noyes et al.(8) and Corry et al.(9) observed in studies that PT grafts that were 14 mm wide (bone-graft-bone) require greater force to break than the other ACL substitutes tested separately. However, ST-G grafts, when combined or quadrupled, become similar to or stronger than 10 mm of PT. Steiner et al.(10) studied load resistance to damage of grafts in cadavers: 4500 N for the ST-G, 2646 N for the PT, and 1725 N for the intact ACL.
Marder et al.(11) and Aglietti et al.(12) conducted studies in ACL reconstruction patients, comparing the two types of grafts, ST-G and PT, using the same technique of fixation, that is, suspensory fixation in the femur and interference screw in the tibia for both. They demonstrated that the anteriorization of the tibia, as well as the symptoms, was not significant in either group. These correspond to our findings, we found the values to be statistically equivalent for the ST-G and PT results on the arthrometer 30.
Laxdal et al.(13) and Moisala et al.(14) also consider that there is no difference between the two groups in terms of laxity. Iorio et al.(15) and Ejerhed et al.(16) also found no significant differences in arthrometry.
Albrecht et al.(17) reported that isokinetic and functional tests are used to assess knee ligament reconstruction after surgery, in order to estimate the recovery of muscle strength and the agonist/antagonist relationship. They concluded that the unoperated limb is a good reference for isokinetic study, achieving 95% symmetry between the limbs. These aforementioned characteristics justify the use of isokinetic evaluation in our study.
Huston and Wojtys(18) observed that the muscle strength recovery time is greater in patients with an ACL injury when compared with other injuries.
Publications with results similar to those seen in this study were found regarding the postoperative analysis of hamstring and quadriceps deficits. Coombs and Cochrane(19) studied the recuperation of knee flexor muscle strength after ACL reconstruction with ST-G. The results showed that there are strength deficits in the operated knee flexors.
As was found by Carter and Edinger(20), our results also demonstrate strength deficits of the quadriceps and flexor muscles after six months of ACL reconstructive surgery with the PT and ST-G, and most patients did not have normal muscle strength at the end of six PO months.
Feller and Webster(21) also reported greater extension deficits in the patellar tendon group, with higher peak torque deficits in the evaluation about four and eight months postoperatively, but not later. They also found greater flexion deficits in the ST-G group at eight to 24 months of follow-up.
The literature also reveals some conflicting studies. Terreri et al.(22) studied 18 athletes with a mean age of 21.6 years (16-32 years) to evaluate the performance after ACL reconstruction with the PT. They found no significant difference between the injured and uninjured knees. The mean ratio of flexion/extension at 60°/second for the injured knee was 60% and 57% for the uninjured knee. Therefore, with increasing speed, deficits also increase due to the improved performance of the flexors, which is not accompanied by extensors.
CONCLUSION
The study showed that there are similarities between the two grafts used. Arthrometry presents equivalent results. Although there are some differences in the short–term described previously in this paper, the isokinetic test results are not confirmed in the long-term according to the literature, and do not alter the surgical outcome.
Thus, the choice of the graft remains at the discretion of the surgeon.
Footnotes
Study conducted at the Study Center, Center for Orthopedics and Rehabilitation in Sports, Hospital do Coraçāo. No: 08/0005
REFERENCES
- 1.Stark J. Two cases of ruptured ligaments of the knee joint. Edinburgh Med Surg. 1850;74:267–271. [PMC free article] [PubMed] [Google Scholar]
- 2.Hey-Groves EW. Operation for the repair of the crucial ligaments. Lancet. 1917;2:674–675. [Google Scholar]
- 3.Campbell WC. Reconstruction of the ligaments of the knee. Am J Surg. 1939;43:473–480. [Google Scholar]
- 4.Macey BH. A new operative procedure for repair of ruptured cruciate ligaments of the knee joint. Surg Gynaecol Obstet. 1939;69:108–109. [Google Scholar]
- 5.Bussab WO, Morettin PA. Estatística básica. 4a ed. Atual; São Paulo: 1987. [Google Scholar]
- 6.Agresti A. Categorical data analysis. 2nd ed. Wiley; New York: 1990. [Google Scholar]
- 7.Wilson AB, Scott WN. Ligamento cruzado anterior. In: Tria AJ, editor. Lesões ligamentares do joelho. Revinter; Rio de Janiero: 2002. pp. 159–184. [Google Scholar]
- 8.Noyes FR, Butler DL, Grood ES, Zernicke RF, Hefzy MS. Biomechanical analysis of human ligament grafts used in knee ligament repairs and reconstrcutions. J Bone Joint Surg Am. 1984;66(3):344–352. [PubMed] [Google Scholar]
- 9.Corry IS, Webb JM, Clingeleffer AJ, Pinczewski LA. Arthroscopic reconstruction of the anterior cruciate ligament: a comparison of patellar tendon autograft and four-strand hamstring tendon autograft. Am J Sports Med. 1999;27(4):444–454. doi: 10.1177/03635465990270040701. [DOI] [PubMed] [Google Scholar]
- 10.Steiner ME, Hecker AT, Brown CH, Jr, Hayes WC. Anterior cruciate ligament graft fixation: comparison of hamstring and patellar tendon grafts. Am J Sports Med. 1994;22(2):240–247. doi: 10.1177/036354659402200215. [DOI] [PubMed] [Google Scholar]
- 11.Marder RA, Raskind JR, Carroll M. Prospective evaluation of arthroscopycally assisted anterior cruciate ligament reconstruction: patellar tendon versus semitendinosus and gracilis tendons. Am J Sports Med. 1991;19(5):478–484. doi: 10.1177/036354659101900510. [DOI] [PubMed] [Google Scholar]
- 12.Aglietti P, Buzzi R, Zaccherotti G, De Biase P. Patellar tendon versus doubled semitendinosus and gracilis tendons for anterior cruciate ligament reconstruction. Am J Sports Med. 1994;22(2):211–218. doi: 10.1177/036354659402200210. [DOI] [PubMed] [Google Scholar]
- 13.Laxdal G, Sernert N, Ejerhed L, Karlsson J, Kartus JT. A prospective comparison of bone-patellar tendon-bone and haminstring tendon grafts for anterior cruciate ligament reconstruction in male patients. Knee Surg Sports Traumatol Arthrosc. 2007;15(2):115–125. doi: 10.1007/s00167-006-0165-z. [DOI] [PubMed] [Google Scholar]
- 14.Moisala AS, Järvelä T, Kannus T, Järvinen M. Muscle streghth evaluations after ACL reconstrcution. Int J Sports Med. 2007;28(10):868–872. doi: 10.1055/s-2007-964912. [DOI] [PubMed] [Google Scholar]
- 15.Iorio R, Ciardini R, Russo A, Conteduca F, Ferretti A. Reconstruction of the anterior cruciate ligament with the tendons of the semitendinosus and gracilis doubled: a comparison with reconstruction using the patellar tendon. Chir Organi Mov. 2005;90(4):379–386. [PubMed] [Google Scholar]
- 16.Ejerhed L, Kartus J, Sernert N, Köhler K, Karlsson J. Patellar tendon or semitendinosus tendon autografts for anterior cruciate ligament reconstruction?: a prospective randomized study with a two-year follow-up. Am J Sports Med. 2003;31(1):19–25. doi: 10.1177/03635465030310011401. [DOI] [PubMed] [Google Scholar]
- 17.Albrecht M, Baron R, Petschnig The relationship between isokinetic quadriceps strength test and hop tests for distance and one-legged vertical jump test following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 1998;28(1):23–31. doi: 10.2519/jospt.1998.28.1.23. [DOI] [PubMed] [Google Scholar]
- 18.Huston LJ, Wojtys EM. Neuromuscular performance characteristics in elite female athletes. Am J Sports Med. 1996;24(4):427–436. doi: 10.1177/036354659602400405. [DOI] [PubMed] [Google Scholar]
- 19.Coombs R, Cochrane T. Knee flexor strength following anterior cruciate ligament reconstruction with the semitendinosus and gracilis tendons. Int J Sports Med. 2001;22(8):618–622. doi: 10.1055/s-2001-18528. [DOI] [PubMed] [Google Scholar]
- 20.Carter TR, Edinger S. Isokinetic evaluation of anterior cruciate ligament reconstruction: hamstring versus patellar tendon. Arthroscopy. 1999;15(2):169–172. doi: 10.1053/ar.1999.v15.0150161. [DOI] [PubMed] [Google Scholar]
- 21.Feller JA, Webster KE. A randomized comparison of patellar tendon and hamstring tendon anterior cruciate ligament reconstruction. Am J Sports Med. 2003;31(4):564–573. doi: 10.1177/03635465030310041501. [DOI] [PubMed] [Google Scholar]
- 22.Terreri M, Ambrosio MA, Pedrinelli A, Albuquerque RFM, Andrusaitis F, Greve JMD. Avaliação isocinética do equilíbrio flexo-extensor do joelho nos atletas com ruptura total do ligamento cruzado anterior. Rev Hosp Clin Fac Med São Paulo. 1999;54(2):35–38. doi: 10.1590/s0041-87811999000200001. [DOI] [PubMed] [Google Scholar]


