Abstract
Background
Video-assisted thoracoscopic (VATS) segmentectomy is an acceptable alternative to lobectomy for treating early-stage lung cancer. Uniportal VATS segmentectomy is a challenging surgical procedure that has substantial technical difficulties and complications. In this study, we reviewed our experience of uniportal thoracoscopic segmentectomy and evaluated the feasibility and learning curve of this procedure.
Methods
Retrospective observational data of 70 patients who underwent uniportal VATS segmentectomy between May 2014 and July 2015 were collected. Perioperative factors, such as demographic characteristics, operation time, blood loss, the number of dissected mediastinal lymph nodes and nodal stations, conversion rate to three-port VATS or thoracotomy, postoperative complications, duration of chest drainage, and postoperative hospital stay, were reviewed. Cumulative summative analysis and one-way ANOVA were used to identify the learning curve of uniportal thoracoscopic segmentectomy.
Results
Forty cases were included in the study. The patients were equally divided into four groups according to the sequence of surgery. Twelve patients were men and the mean age was 53.7±8.3 years. The mean operation time was 174.2±51.5 minutes and mean blood loss was 81.9±57.4 mL. There were no differences in demographic characteristics, blood loss, number of removed lymph nodes, chest tube duration, and hospital stay among the groups. However, the operation time in group 4 was significantly shorter than that in groups 1–3 (P=0.012). The learning curve showed that after 33 patients, the operation time was less than the conventional average operation time. There was no conversion to three-port VATS, two-port VATS or open thoracotomy. Three patients had postoperative complications and all of them recovered after treatment. No patient needed reoperation. There was no postoperative 30-day-related death.
Conclusions
Uniportal thoracoscopic segmentectomy is a safe and feasible technique for treating small pulmonary lesions, with acceptable morbidity and mortality. This technique can be applied to an operation for segments that are technically difficult and anatomically variant. An experienced surgeon can achieve a relatively stable level after 33 cases.
Keywords: Feasibility, learning curve, uniportal, thoracoscopic segmentectomy
Introduction
Environmental pollution has become worse over time. With an improvement of living standards and people’s awareness of health, an increasing amount of small pulmonary nodules are found by physical examination. Lobectomy with mediastinal node dissection is considered as the standard treatment for early-stage non-small cell lung cancer. However, some studies have indicated that segmentectomy is safe and feasible, without significant differences in survival and recurrence of oncology outcomes, compared with lobectomy (1-3). Segmentectomy is also a reasonable alternative procedure for older people who have poor cardiopulmonary reserve.
Generally, total thoracoscopic segmentectomy is performed through three or more thoracic incisions. However, because of advances in endoscopic instruments and video-assisted thoracoscopic (VATS) surgery, fewer surgical ports are needed. Since Gonzalez-Rivas et al. (4) first described uniportal VATS surgery for anatomic segmentectomy, an increasing number of surgeons have chosen this minimally invasive treatment modality. However, uniportal VATS segmentectomy is a complex and time-consuming procedure. A considerable learning curve has to be overcome before a surgeon is proficient in using this technique in pulmonary resections.
To the best of our knowledge, there are no studies concerning the learning curve of single-port VATS segmentectomy. Therefore, this study aimed to review our experience of uniportal thoracoscopic segmentectomy and to evaluate the feasibility and learning curve of this procedure.
Patients and methods
Selection of patients
An informed consent form was signed by each patient. We retrospectively reviewed 70 consecutive patients who underwent single-port thoracoscopic anatomic segmentectomy in the Thoracic Department of Union Hospital of Fujian Medical University from May 2014 to July 2015. A total of 40 patients were enrolled in this study. Preoperative assessments included complete blood counts, serum biochemistry tests, an electrocardiogram, a lung function test, echocardiography, a computed tomographic (CT) scan of the chest, magnetic resonance imaging of the brain, a bone scan, abdominal ultrasound, bronchoscopy, and whole-body positron emission tomography-CT when it was necessary.
To select appropriate patients, the inclusion criteria for this study were as follows: (I) the indication of segmentectomy was discussed through multidisciplinary discussion consultation; (II) uniportal segmentectomy was performed by the same team who was experienced in conventional VATS surgeries and thoracotomy; and (III) the procedures of surgery included segmentectomy for a single segment and mediastinal lymph node dissection or sampling.
Exclusion criteria were as follows: (I) patients with multiple nodules that were located in different segments and the operation involved more than one segment; (II) surgeons performed segmentectomy with lobectomy at the same time; (III) intraoperative pathology results confirmed benign lesions (bronchiectasis, sclerosing hemangioma, tuberculous granulomas, inflammatory pseudotumor, atypical adenoid hyperplasia, and pulmonary metastasis) without lymph node dissection or sampling; (IV) intraoperative pathology-confirmed pleural metastasis; and (V) the operation included separating dense pleural adhesions.
Surgical methods
Surgery was performed under general anesthesia with a double-lumen endotracheal tube and one-lung ventilation. Patients were transitioned to the lateral decubitus position. The surgeon and assistant were standing on both sides of the patients. A surgical incision (3.0–4.5 cm in length) was made in the fourth or fifth intercostal space on the anterior axillary line at the diseased side, according to the patient’s body height and the location of the lesion (Figure 1). Rib spreading was not necessary. A wound protector (VIPA type, 80/90–80/150; Victor Medical) was used to protect the camera lens from oozing by the intercostal muscle.
Figure 1.
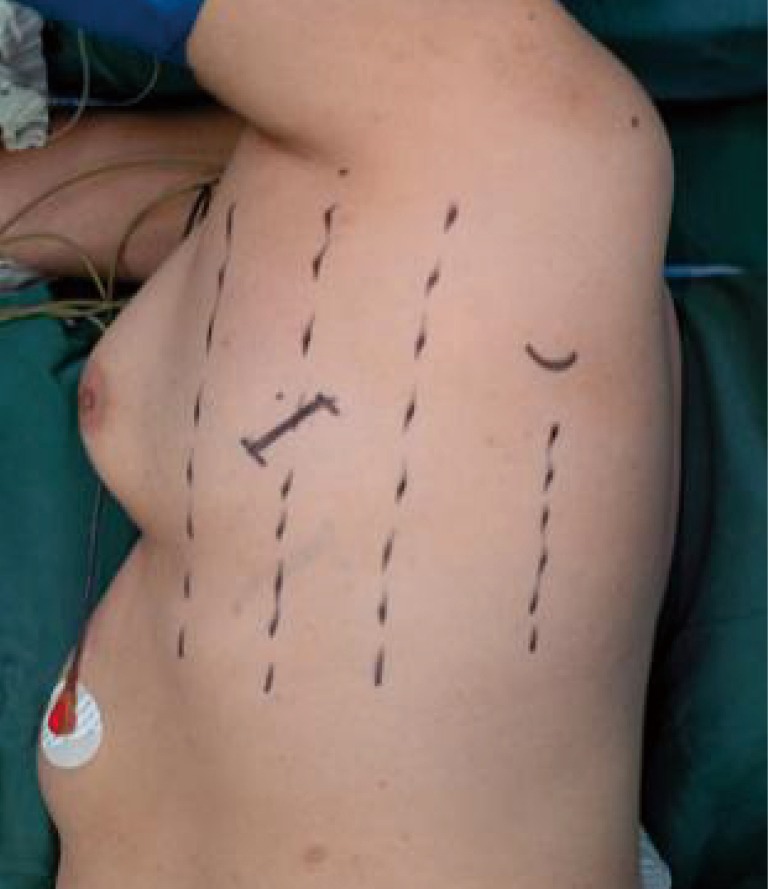
Lateral decubitus position and incision of the uniportal thoracoscopic segmentectomy.
The required instrumentation was not different from that of conventional VATS, including endograspers, oval forceps, a suction device, hook electrocautery, vascular clips, an articulated endoscopic stapler, and a harmonic scalpel. All of the instruments were inserted through the same incision and all procedures were performed under the guidance of a 10-mm, 30-degree, angled thoracoscopic video camera in every patient. Anatomical individual resection of veins, arteries, and the bronchus, as well as complete mediastinal lymph node dissection or sampling, were performed in the same manner as the conventional VATS operation.
If an unexpected situation was encountered during single-incision thoracoscopic surgery, conversion to multiple-incision thoracoscopic surgery or thoracotomy was performed. A protective bag was always used to prevent tumor implantation in the incision when the lung specimen was being withdrawn from the single port.
After the operation, two chest tubes were routinely used. One 28# chest tube (Mingji Medical, Suzhou, China) was placed in the pleural cavity through the anterior part of the incision. The other Abel drainage tube (central venous catheter, 8 Fr-20; Baihe Medical, Guangzhou, China) was inserted at the eighth intercostal space on the posterior axillary line (Figure 2).
Figure 2.

The position of the Abel drainage tube and chest tube.
Data collection
Clinical data, including age, sex, largest tumor size, tumor location, and perioperative parameters, such as operation time, operative blood loss, number of dissected mediastinal nodes and nodal stations, conversion rate, postoperative complication rate, reoperation rate, and postoperative mortality rate, were reviewed. Surgical mortality was defined as death occurring during the same hospitalization or within 30 days after the operation. Pulmonary infection was defined as a bacterial culture detected by sputum tests.
Statistical analysis
Statistical analysis was performed using SPSS 19.0 software. Continuous variables are expressed as mean ± SD. Quantitative variables were tested by analysis of variance. If there was a significant difference, the least significant difference method was used to compare any two groups. Categorical variables were analyzed using Fisher’s exact or the chi-square test. Cumulative summative analysis was used to identify the learning curve of uniportal thoracoscopic segmentectomy. The operation time of conventional VATS segmentectomy performed by the same group at the same period of time was recorded to establish the baseline operating time for comparison with the uniportal segmentectomy time. Statistical analysis was considered to be significant when the probability value was below 0.05.
Results
From May 2014 to July 2015, a total of 40 patients were enrolled in the study. Those who underwent uniportal surgeries had them performed by a single surgeon (Chun Chen) at Union Hospital of Fujian Medical University. The patients consisted of 12 men and 28 women with a mean age of 53.7±8.3 years (range, 34–67 years). Of the 40 patients, 21 (52.5%) had an underlying comorbidity, including hypertension, diabetes mellitus, bronchial asthma, chronic obstructive pulmonary disease, atrial premature beat, lacunar infarction, and a previous lung operation. The mean operation time was 174.2±51.5 minutes. The mean blood loss was 81.9±57.4 mL. The mean harvested number of mediastinal nodes and dissected mediastinal stations was 13.1±7.0 and 5.5±1.6, respectively. The mean length of hospital stay of the patients was 4.6±1.5 days. There was no conversion to three-port VATS, two-port VATS, or open thoracotomy (Table 1).
Table 1. Demographic, clinical and pathological characteristics of patients.
| Variable | Patients (n=40) |
|---|---|
| Age (years) | 53.7±8.3 |
| Sex ratio (male:female) | 12:28 |
| Comorbidity | 21 (52.5%) |
| Previous lung operation | 3 (7.5%) |
| No. of dissected mediastinal stations | 5.5±1.6 |
| Mortality | 0 |
| Tumor size (cm) | 0.3–1.3 |
| Pathological results | MIA |
| Pathological staging | pT1aN0M0 (Ia) |
Data are expressed as mean ± SD or number (%). MIA, microinvasive adenocarcinoma.
The patients were divided equally into four groups with ten patients in each group according to the sequence of surgery. The operation time, blood loss, and postoperative data are listed in Table 2. The operation time in group 4 was significantly shorter (P=0.012) than that in groups 1–3. However, the operation time was similar among groups 1–3. The Pearson correlation coefficient (r) was −0.383 with a two-tailed P=0.015. The mean operation time of conventional VATS segmentectomy was 155 minutes in the same period. Taken together, our data indicated that after 33 patients, an improvement plateau was reached (Figure 3).
Table 2. Comparison of perioperative results between different groups.
| Perioperative parameters | Overall | Group 1 | Group 2 | Group 3 | Group 4 | F | P |
|---|---|---|---|---|---|---|---|
| Surgical time (min) | 174.2±51.5 | 194.5±39.5 | 177.5±68.7 | 190.3±46.6 | 134.3±22.8 | – | – |
| P* | – | – | 0.428 | 0.549 | 0.012 | 3.379 | 0.029 |
| Blood loss (mL) | 81.9±57.4 | 112.0±74.5 | 68.0±36.8 | 80.5±54.1 | 67.0±54.8 | 1.375 | 0.266 |
| DMN | 13.1±7.0 | 12.6±6.9 | 12.0±5.7 | 16.8±9.0 | 11.0±5.5 | 1.363 | 0.270 |
| Chest duration (days) | 5.9±2.5 | 6.9±3.1 | 5.3±1.9 | 5.4±1.9 | 6.1±2.9 | 0.874 | 0.464 |
| Hospital stay (days) | 4.6±1.5 | 4.2±1.5 | 4.5±1.3 | 4.8±1.1 | 4.8±2.1 | 0.333 | 0.802 |
| Complication | 3 | 2 | 0 | 0 | 1 | – | – |
| Age (years) | 53.7±8.3 | 51.4±8.0 | 52.9±8.4 | 55.9±8.1 | 54.5±9.3 | 0.528 | 0.666 |
| S4 + S5 + S6 | 9 | 2 | 3 | 3 | 1 | – | – |
| Other segments | 31 | 8 | 7 | 7 | 9 | – | 0.635 |
*, P value of the difference of operative time, compared with former group; chest duration, chest drainage duration (days). DMN, dissected mediastinal nodes; S4-S5, lingular segment; S6, superior and basilar segment.
Figure 3.
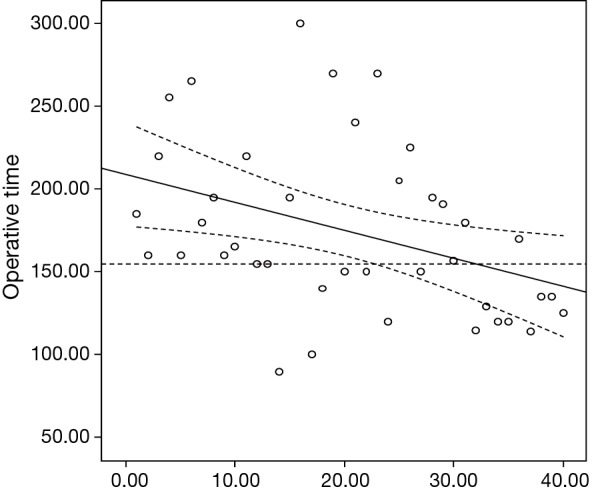
The learning curve of uniportal thoracoscopic segmentectomy and 95% confidence intervals can be seen as dotted lines.
Only three patients had postoperative complications. The complications were two cases of pneumonia and one case of atrial fibrillation. There were no cases of chylothorax, prolonged air leak, and pulmonary infarction. All of the complications disappeared after related treatments. No patient needed reoperation. There was no postoperative 30-day related death.
Discussion
The feasibility and advantages of uniportal VATS in diverse fields of thoracic surgery have already been extensively described. Potential advantages of this approach are less postoperative pain and reduced intercostal nerve injury compared with traditional surgery. Jutley et al. (5) showed that uniportal VATS appeared to have a lower incidence of postoperative pain and paresthesia compared with three-port VATS in treating spontaneous pneumothorax. Another advantage of uniportal VATS is that it offers direct visualization to the target lesion and thus obtains a similar angle of view as with open surgery (6). With advances in uniportal VATS techniques, the indication of this procedure has been greatly broadened, and technical barriers are constantly being broken. The application of uniportal VATS in more complicated procedures, including segmentectomy (7), pneumonectomy (8) and double sleeve lobectomy (9), has also been reported.
The learning curve shows the progress in mastering a new method. Learning is completed when the monitored parameters reach a steady state and when the final results can be compared with the literature (10). Learning curves for different surgical techniques are considerable, especially in laparoscopic surgery, but little is known about the learning curve for lung surgery. Because uniportal VATS segmentectomy is a complex and time-consuming procedure, inexperienced surgeons may suffer from fatigue, which may lead to thoughts of abandoning the operation. Therefore, exploring the learning curve is meaningful, and allows surgeons to understand how many cases are needed to achieve a relatively stable level. Zhao et al. (11) found that an improvement plateau was reached for VATS lobectomy after 30 cases. Uniportal VATS segmentectomy also has a considerable learning curve.
At the beginning of performing uniportal segmentectomy, when multiple views of conventional VATS are forfeited, obstruction of the view and interference commonly occur. However, our results suggested that the operation time for uniportal segmentectomy was decreased after the surgeon had performed 33 procedures. The assistant stood ipsilaterally to the surgeon at first and then gradually changed to the opposite side, which increased the surgeon’s activity space and reduced unnecessary collision. Most of the reported segmentectomies were related to segments that can be easily excised, such as the lingular, superior, and basilar segments (12). To date, we have performed 70 cases of uniportal segmentectomy with good postoperative outcomes. Furthermore, we have successfully completed nearly all segments of the lungs, especially some difficult segments including the following: (I) right upper lobe apico-posterior segmentectomy (S1-S2); (II) right upper lobe apical segmentectomy (S1); (III) left upper lobe trisegmentectomy (S1-S2-S3); and (IV) left upper lobe anterior segmentectomy (S3) (Table 3).
Table 3. Comparison of other segments between different groups.
| Segments | Group 1 | Group 2 | Group 3 | Group 4 |
|---|---|---|---|---|
| Right S1 | 0 | 1 | 2 | 2 |
| Right S2 | 0 | 1 | 0 | 1 |
| Right S3 | 2 | 0 | 1 | 2 |
| Right S1 + S3 | 0 | 1 | 1 | 1 |
| Left S1 | 0 | 1 | 0 | 0 |
| Left S3 | 1 | 1 | 1 | 1 |
| Left S1 + S3 | 1 | 0 | 1 | 0 |
| Left S1 + S2 + S3 | 3 | 1 | 1 | 2 |
| Left S7 + S8 | 1 | 1 | 0 | 0 |
There are many factors that reduce the learning curve of segmentectomy. First, accumulated experience in performing uniportal surgeries is necessary. Pleural adhesions have a major effect on the operation time. Therefore, in this study, we excluded patients with dense pleural adhesions, as mentioned above. For patients with incomplete pulmonary fissure, this makes surgery more difficult, but we have adequate experience in thoracotomy and thoracoscopic surgery. Therefore, there is no substantive difficulty with technology. Second, cooperation with the surgeon and the assistant is needed. Third, specially developed equipment is also important. No studies have been published concerning the learning curve of single-port VATS segmentectomy. Wang et al. (13) found no significant difference in the operation time, blood loss, length of stay, and complications between lobectomy and segmentectomy via a single incision.
Recent studies (14,15) have suggested that segmentectomy is an alternative to lobectomy in patients with clinical T1N0M0 disease, especially when the nodule is smaller than 2 cm in diameter, and there is ground glass opacity or a peripheral tumor. However, there is controversy in segmentectomy. Lung nodule pathologically confirmed adenocarcinoma in situ or microinvasive adenocarcinoma is suitable for anatomical segmentectomy and lymph node sampling. However, for invasive adenocarcinoma or a solid nodule less than 2 cm, whether radical resection by segmentectomy should be performed is controversial. Further validation via a prospective study is required.
There are some limitations to our study: there is a lack of long-term follow-up and the number of included patients was not sufficient. In conclusion, uniportal thoracoscopic segmentectomy is a safe and feasible technique for treatment of small pulmonary lesions, with acceptable morbidity and mortality. On the basis of accumulated experience of uniportal VATS lobectomy, the learning curve for uniportal thoracoscopic segmentectomy is relatively short. This learning curve would be longer for surgeons who have no experience in thoracoscopic surgery. Uniportal segmentectomy can be performed for segments that are technically difficult and anatomically variant.
Acknowledgements
None.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Tsutani Y, Miyata Y, Nakayama H, et al. Oncologic outcomes of segmentectomy compared with lobectomy for clinical stage IA lung adenocarcinoma: propensity score-matched analysis in a multicenter study. J Thorac Cardiovasc Surg 2013;146:358-64. [DOI] [PubMed] [Google Scholar]
- 2.Okada M, Yoshikawa K, Hatta T, et al. Is segmentectomy with lymph node assessment an alternative to lobectomy for non-small cell lung cancer of 2 cm or smaller? Ann Thorac Surg 2001;71:956-60; discussion 961. [DOI] [PubMed] [Google Scholar]
- 3.Okada M, Koike T, Higashiyama M, et al. Radical sublobar resection for small-sized non-small cell lung cancer: a multicenter study. J Thorac Cardiovasc Surg 2006;132:769-75. [DOI] [PubMed] [Google Scholar]
- 4.Gonzalez-Rivas D, Fieira E, Mendez L, et al. Single-port video-assisted thoracoscopic anatomic segmentectomy and right upper lobectomy. Eur J Cardiothorac Surg 2012;42:e169-71. [DOI] [PubMed] [Google Scholar]
- 5.Jutley RS, Khalil MW, Rocco G. Uniportal vs standard three-port VATS technique for spontaneous pneumothorax: comparison of post-operative pain and residual paraesthesia. Eur J Cardiothorac Surg 2005;28:43-6. [DOI] [PubMed] [Google Scholar]
- 6.Bertolaccini L, Rocco G, Viti A, et al. Geometrical characteristics of uniportal VATS. J Thorac Dis 2013;5 Suppl 3:S214-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gonzalez-Rivas D. Single incision video-assisted thoracoscopic anatomic segmentectomy. Ann Cardiothorac Surg 2014;3:204-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gonzalez-Rivas D, Delgado M, Fieira E, et al. Uniportal video-assisted thoracoscopic pneumonectomy. J Thorac Dis 2013;5 Suppl 3:S246-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gonzalez-Rivas D, Delgado M, Fieira E, et al. Double sleeve uniportal video-assisted thoracoscopic lobectomy for non-small cell lung cancer. Ann Cardiothorac Surg 2014;3:E2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Buchmann P, Dinçler S. Learning curve--calculation and value in laparoscopic surgery. Ther Umsch 2005;62:69-75. [DOI] [PubMed] [Google Scholar]
- 11.Zhao H, Bu L, Yang F, et al. Video-assisted thoracoscopic surgery lobectomy for lung cancer: the learning curve. World J Surg 2010;34:2368-72. [DOI] [PubMed] [Google Scholar]
- 12.Atkins BZ, Harpole DH, Jr, Mangum JH, et al. Pulmonary segmentectomy by thoracotomy or thoracoscopy: reduced hospital length of stay with a minimally-invasive approach. Ann Thorac Surg 2007;84:1107-12; discussion 1112-3. [DOI] [PubMed] [Google Scholar]
- 13.Wang BY, Liu CY, Hsu PK, et al. Single-incision versus multiple-incision thoracoscopic lobectomy and segmentectomy: a propensity-matched analysis. Ann Surg 2015;261:793-9. [DOI] [PubMed] [Google Scholar]
- 14.Landreneau RJ, Normolle DP, Christie NA, et al. Recurrence and survival outcomes after anatomic segmentectomy versus lobectomy for clinical stage I non-small-cell lung cancer: a propensity-matched analysis. J Clin Oncol 2014;32:2449-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhao X, Qian L, Luo Q, et al. Segmentectomy as a safe and equally effective surgical option under complete video-assisted thoracic surgery for patients of stage I non-small cell lung cancer. J Cardiothorac Surg 2013;8:116. [DOI] [PMC free article] [PubMed] [Google Scholar]


