Abstract
Aim:
Reducing the psychosocial stress by various methods can improve overall health, and yoga is now considered as an easily available alternative method. The present cross-sectional pilot study was conducted mainly to find the association of yoga practice with periodontal disease by measuring serum cortisol levels.
Materials and Methods:
A total of 70 subjects with age range of 35–60 years suffering with chronic periodontitis were divided into group I (with stress), group II (without stress), and group III (practicing yoga). Psychological evaluation was carried out using Hamilton Anxiety Rating Scale (HAM-A) and Zung Self-rating Depression Scale (ZSDS). Periodontal parameters like plaque index (PI), probing pocket depth (PPD), and clinical attachment level (CAL) at 5–8 mm and >8 mm were recorded. Blood samples were collected and serum cortisol levels were measured.
Results:
Mean age, plaque scores, and number of teeth with PPD and CAL at 5–8 mm and >8 mm were similar in all the groups, except between group I and group III where a multiple comparison with Tukey's post-hoc test showed significant difference in plaque index (P < 0.038) and the number of teeth with CAL 5–8 mm (P < 0.016). Serum cortisol levels and HAM-A scale and ZSDS scores showed highly significant value (P < 0.001) in group I subjects when compared with group II and group III subjects.
Conclusion:
Cross-sectional observation done among three groups showed that individuals practicing yoga regularly had low serum cortisol levels, HAM-A scale and ZSDS scores, and better periodontal health.
Keywords: Cortisol, periodontal disease, serum, stress, yoga
INTRODUCTION
Research in the etiology of periodontal disease over the past few decades has been mainly focused around specific periodontal pathogens and their virulence factors that affect the host resistance. Systemic factors like diabetes mellitus and smoking, osteopenia, neutrophil disorders, and genetic polymorphisms were found to be associated with more severe form of periodontal disease.[1,2,3]
Earlier studies showed that psychosocial stress, physiological stress, anxiety, and depression were associated with significant amount of periodontal disease progression and wound healing.[4] Hans Selye (1946) coined the term stress and postulated the possible mechanism of activation of the adrenocortico-pituitary axis. The stress-induced responses either result in change in behavior or are transmitted to the hypothalamic–pituitary–adrenal (HPA) axis to release corticotrophic releasing hormone (CRH) from the hypothalamus. CRH activates the pituitary gland to release adrenocorticotropic hormone (ACTH), which in turn induces the release of glucocorticosteroids like cortisol from the adrenal cortex.[5,6,7,8]
Normal blood serum cortisol levels in the morning are 6–23 mcg/dl. A higher than normal level is seen when there is excessive growth of the pituitary gland or adrenal gland. Cortisol contributes to hyperglycemia, reduces bone formation, calcium absorption from the intestine, and downregulates the synthesis of collagen. Lower than normal level may indicate Addison disease and hypopituitarism.
Cortisol (the primary glucocorticoid) reduces the number of circulating lymphocytes, monocytes, and other proinflammatory cells resulting in decrease in functions such as chemotaxis and proliferation of effector lymphocytes to differentiate into helper lymphocytes, cytotoxic lymphocytes, natural killer cells, IgG and IgA antibody forming B cells.[9] Decreased functioning of neutrophils and secretory IgA, and IgG antibodies leads to increased susceptibility to periodontal infections, which results in increased production of inflammatory cytokines like IL-1 and matrix metalloproteinases by the periodontal pathogens causing rapid periodontal tissue destruction.
Glucocorticoids induce endogenous anti-inflammatory proteins, and lipocortins inhibit phospholipase A2, thereby inhibiting the production of eicosanoids.[10,11] Glucocorticoids tend to suppress cell-mediated immunity, but enhance humoral immunity by increased IL-4 production, and also interfere with nuclear factor-kappa B (NF-κB) to regulate cytokine production from the inflammatory cells.[12]
Yoga is a 3000-year-old tradition which has been practiced in India. It is now regarded as a holistic approach to health and is classified by the National Institutes of Health (NIH) as a form of Complementary and Alternative Medicine (CAM).[13] In an attempt to overcome the health problems and challenges, the practice of yoga has become increasingly popular all over the world, over the last decade. The common practice of yoga nowadays includes mainly physical postures, breathing exercises, and meditation.
The word yoga is derived from the Sanskrit word “yuj” which means union, yoke, or to join and to direct and concentrate one's attention.[13,14] Regular practise of yoga helps to build a better connectivity between the mind and body through a series of postures, breathing exercises, and meditation. Pratyahara is the fifth of patanjali's eight-limbed path of yoga. It can be an important tool for stress reduction,[15] which can help in almost instant stress reduction by lengthening the exhalation relative to the inhalation, which in turn increases the tone in the sympathetic nervous system. The benefits of yoga include decreased stress and tension, increased strength, balance and flexibility of muscles, lowered blood pressure, and reduction in cortisol levels.[16]
Any form of yoga has emerged as a potential integrative modality for management of several medical diseases such as diabetes, stress, HIV, arthritis, osteoporosis, multiple sclerosis, immune function disorders, and smoking cessation. Consistent yoga practice improves depression and can lead to significant increase in serotonin [5-hydroxytryptamine (5-HT)] levels at nerve synapses, which in turn helps in lifting the mood of an individual. Yoga also decreases the levels of monamine oxidase, an enzyme that breaks down neurotransmitters and cortisol.[17]
Stress is a significant common risk factor for diabetes mellitus, cardiovascular diseases, preterm delivery, and osteoporosis, as well as periodontal disease. Reducing stress levels can greatly improve the health and quality of life, and yoga is arguably the best overall system ever invented for stress reduction. This ancient method gives an insight on the link between physical body and the state of mind, and any system of yoga can greatly help to reduce stress levels.[18]
Although present research strongly supports the association of various forms of stress with periodontal disease, this pilot, cross-sectional study was done mainly to find the association of yoga practice with periodontal disease by measuring the serum cortisol levels.
MATERIALS AND METHODS
A total of 70 subjects of both genders with an age range of 35–60 years and diagnosed with chronic periodontitis were selected. Psychological evaluation of each individual was carried out using Hamilton Anxiety Rating Scale (HAM-A) and Zung Self-rating Depression Scale (ZSDS). Out of 70 patients, 23 patients with anxiety and depression were included in group I and 24 subjects without anxiety and depression were categorized into group II. These patients were recruited from the out-patient department of periodontics, Sibar Institute of Dental Sciences, Takellapadu, Guntur. Remaining 23 subjects who had been practising yoga for the past 5 years were selected from Jeevan Kala Yoga Center, Lakshmipuram, Guntur, and were categorized into group III.
HAM-A consists of 14 items, each defined by series of symptoms and measures of both psychic anxiety and somatic anxiety. Each item is scored on a scale rated 0 (not present) to 4 (severe) on an unanchored severity scale, with the total score range of 0–56. A score of 14 has been suggested as the threshold for clinically (mild) significant anxiety, 18–24 for anxiety of mild to moderate severity, and 25–30 for moderate to severe anxiety.[19]
ZSDS consists of 20 items with rating from 1 to 4 and the highest possible score is 80. Subjects with scores between 50 and 69 are considered to have significant depression.[20]
The study protocol has been approved by the institutional ethical committee and informed written consent was taken from all the recruited subjects before the start of the study.
Periodontal parameters like probing pocket depth (PPD) and clinical attachment level (CAL) were measured using UNC-15 probe (Hu-Friedy, Chicago, IL, USA). All the six surfaces on each tooth excluding third molars were evaluated. The number of teeth with PPD and CAL 5–8 mm and >8 mm was recorded.[21] Plaque index (PI) was calculated,[22] and the frequency of brushing and history of smoking and alcoholism were noted. Subjects with number of teeth less than 20, those who had undergone any form of periodontal treatment in the last 1 year, those suffering from any systemic disease, self-reported psychiatric disorder, or on psychotropic drugs, pregnant women, those on any hormonal treatment, those using contraceptive pills, and those using antibiotics in the previous 3 months were excluded from the study. Serum samples were also adjusted for circadian variation in cortisol levels by matching the time of day at which the samples were collected.
Statistical analysis
Data were collected and statistical analysis was done between the groups. One-way analysis of variance (ANOVA) was used to evaluate interactions between the three groups, in conjunction with Tukey's honestly significant difference (HSD) test to draw single-step multiple comparison.
RESULTS
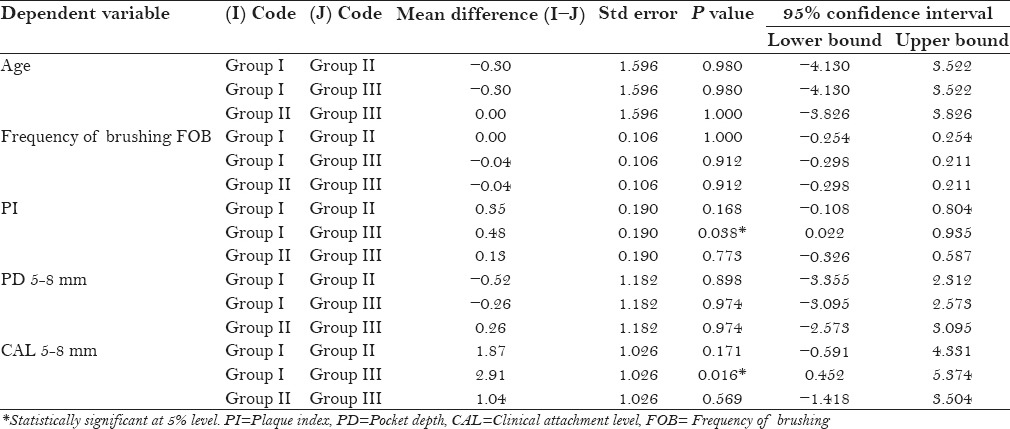
With a total of 70 patients in the study (37 females and 33 males), there was equal distribution of gender among the groups with slightly higher number of females in group III. Seven subjects were current smokers and nine subjects had given history of alcoholism. Most of the patients were brushing once daily in the morning and a maximum of four patients in group III were brushing twice daily. Mean values for all the parameters were calculated and inter group comparisons were made using one-way ANOVA followed by multiple pair wise comparisons using Tukey's post-hoc test among the groups. The mean (SD) values of age in the groups were 46.83 (5.62) in group I, 47.13 (5.40) in group II, and 47.13 (5.20) in group III, which was not statistically significant [Table 1]. PI scores in group I (2.04 ± 0.64), group II (1.70 ± 0.56), and group III (1.57 ± 0.73) were compared, and a significant difference (P = 0.040) was observed between the group I and group III [Table 1]. Mean values for the total number of teeth with pocket depth measuring from 5 to 8 mm in all the three groups (group I = 16.46 ± 4.97, group II = 16.78 ± 3.90, and group III = 16.52 ± 2.87) were compared and there was no significant difference found between the three groups [Table 1]. But a significant difference (P < 0.020) between group I and group III was observed when the mean values (group I = 21.87 ± 3.02, group II = 20.00 ± 3.66, and group III = 18.96 ± 3.99) for total number of teeth with CAL measuring from 5 to 8 mm were compared [Table 1]. Multiple comparison with Tukey's post-hoc test showed significant difference between group I and group III in both PI (P < 0.038) and CAL (P = 0.016) [Table 2].
Table 1.
Comparison of mean values of clinical parameters using one-way ANOVA
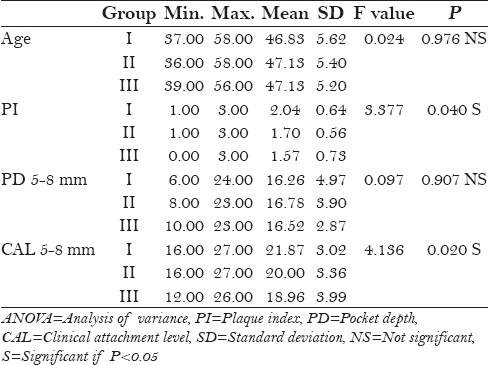
Table 2.
Multiple comparsion of clinical parameters by using Tukey's post-hoc test
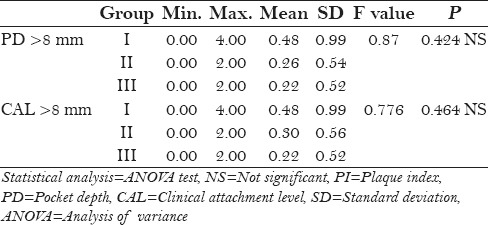
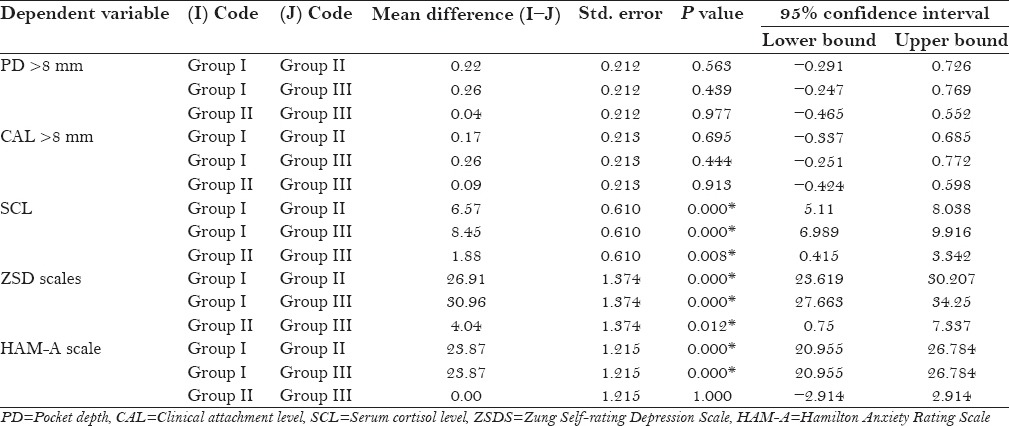
No statistical difference was observed when the mean values for the number of teeth with >8 mm pocket depth (group I = 0.48 ± 0.99 mm, group II = 0.26 ± 0.54 mm, and group III 0.22 ± 0.52 mm) and CAL (group I = 0.48 ± 0.99 mm, group II = 0.24 ± 0.56 mm, and group III = 0.22 ± 0.52 mm) were compared between the groups [Table 3].
Table 3.
Mean comparsion of PD >8 mm and CAL >8 mm among the groups using one-way ANOVA
The mean serum cortisol levels obtained were: Group I (20.77 ± 1.48 μg/dl), group II (14.19 ± 2.34 μg/dl), and group III (12.31 ± 2.27 μg/dl). When the mean serum cortisol levels in all the subjects were compared using one-way ANOVA, statistically significant (P < 0.001) difference was observed in all the three groups [Table 4].
Table 4.
Mean comparsion of serum cortisol level SCL, ZSDS, and HAM-A scale among the groups using one-way ANOVA
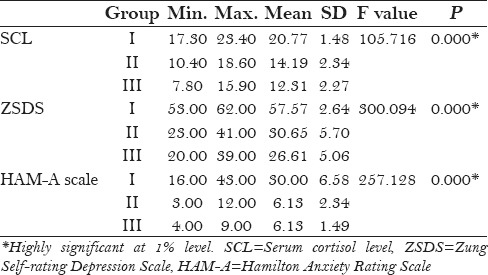
Anxiety and depression levels were assessed using HAM-A scale and ZSDS, which showed statistically highly significant difference (P < 0.001) in group I subjects when compared with group II and group III subjects [Table 4]. Multiple comparison with Tukey's post-hoc test showed that both ZSDS and HAM-A scale values were significant (P < 0.001) at 1% level in all the groups, except between group II and group III where ZSDS values were significant (P 0.012) at 5% level and HAM-A values were not statistically significant [Table 5].
Table 5.
Multiple comparsion of PD >8 mm, CAL >8 mm, SCL, ZSDS, and HAM-A scale by Tukey's post-hoc test
DISCUSSION
Stress is considered as an important factor in the etiology and maintenance of many chronic inflammatory diseases like rheumatoid arthritis, inflammatory bowel disease, and periodontal disease.[23] The role of psychosocial disturbances in the etiology of periodontal disease was proposed by Burstone, Miller, Firestone et al.[11] in the early. literature. The association between psychosocial stress, measures of distress, and coping behaviors was investigated in an epidemiologic study of 1426 participants aged between 25 and 74 years in the Eric County, NY. The stress levels of subjects were measured with five psychosocial instruments, which indicated significant association of stress with greater alveolar bone loss.[10]
According to Miller and Firestone,[5] Moulton et al.,[6] and Belting and Gupta, 1961[7], psychological disturbances can lead patients to neglect oral hygiene, resulting in greater amounts of of plaque accumulation, which is detrimental to the periodontal tissues. Moulton et al.[6] reported that severe cases of acute necrotizing ulcerative gingivitis (ANUG) were preceded by acute anxiety. By assessment of psychiatric patients and normal subjects, Baker et al. 1961[11] found significant corelations between periodontal status and factors such as age, broken home, marital adjustment, and hysteria. Belting and Gupta[7] reported that psychiatric patients presented significantly higher periodontal scores than their controls and concluded that the severity of inflammatory periodontal disease increased significantly with the degree of anxiety.
The cellular and molecular interaction between the immune system and CNS mediates the effects of stress in maintaining immunologic and behavioral homeostasis. Kamma et al. (2004) stated that smoking and stress-related factors can increase the cytokine levels significantly in aggressive periodontitis patients compared with controls.[24] There were increased levels of Tannerella forsythus, Porphyromonas gingivalis, and Aggregatibacter actinomycetemcomitans among individuals with high depression scores, suggesting a positive psychoneuroimmunologic link.[25,26] A cross-sectional study done by Marcenes and Sheiham[27] to establish the association of oral health status with work stress found that there was a significant association between poor periodontal status and high work demand with low marital quality.
Numerous studies have shown that yoga practice has become an increasingly widespread therapy to reduce stress by reducing anxiety, depression, and other mood disorders. Yoga inhibits the posterior or sympathetic area of hypothalamus and restores autonomic regulatory reflex mechanisms associated with stress, leading to decreased production of ACTH from the anterior pituitary gland.[28] Consistent yoga practice can improve individual's physical, mental, and spiritual components of health particularly related with stress, resulting in decrease production of cortisol from the adrenal gland.[29,30]
In the present study, serum cortisol levels were assessed to find the existing relationship between stress and periodontitis by comparing with yoga practising individuals. Serum, saliva, and gingival crevicular fluid are three different media considered for examining cortisol levels. Non-invasive methods of collecting the sample like saliva and gingival crevicular fluid are also preferred, but due to chairside sample collection, storage, and other patient-related factors, serum cortisol assessm ent was considered.
In this cross-sectional study, all the included subjects were evaluated for their stress levels with the help of a questionaire and the periodontal health status was correlated with cortisol levels. Plaque level in all the subjects was high, but slightly higher levels were noticed in subjects with stress and periodontitis. This is in agreement with previous studies by Rosania et al.,[31] Johannsen et al.,[32] and Klages et al.[33] According to Deinzer et al., students who are under academic stress show high plaque values as well as severe gingival inflammation.[34] High plaque values in group I subjects may be due to infrequent or inefficient tooth brushing of these individuals. Similar to the previous studies, it was noticed that stress may interfere with tooth brushing and plaque control measures.[35]
PPD and CAL of 5–8 mm in the present investigation showed no differences for the levels of anxiety and depression among subjects in all three groups with different levels of periodontal disease. In addition, of the three groups, subjects in group I showed slightly higher frequency of PPD and CAL 5–8 mm. This may be due to the action of behavioral pathogens, neglect of oral hygiene, dietary inadequacies, poor sleep patterns, and use of tobacco products which constitute an important class of psychosocial stress that contributes to the severe form of advanced periodontal inflammation and disease.[36] When the association of the levels of cortisol with the severity of PPD and CAL was determined, it was noticed that in all subjects there was positive association of cortisol levels with severity of both PPD and CAL.
Genco et al.[11] first verified the association between cortisol levels and periodontal disease and reported that the mean cortisol levels were higher in patients with the periodontal disease and stress. In another study, Mengel et al.[37] examined the interaction of periodontal disease with psychosocial stress and stated that there were no statistically significant correlations among the immunological mediators (IL-1, IL-6), cortisol, and stress.
Cortisol levels in the peripheral blood and saliva follow a circadian rhythm, showing highest titers in the early morning during the final hours of sleep, followed by a gradual decline over the course of the day, with minimum titer reached in the early evening.[38] Different physiological cortisol concentrations have been reported in the blood (from 5 × 10−8 M to 1.2 × 10−6 M), saliva (from 5.5 × 10−9 M to 6 × 10−9 M), and gingival crevicular fluid (from 35 to 97 × 10−9 M). External factors such as inflammatory, physical, and psychosocial stress are known to increase cortisol release.[39]
In this study, cortisol levels were mostly associated with psychosocial stress measured with HAM-A and ZSDS. HAM-A is an observer rating scale, which is a more reliable and accurate tool for assessing the severity of anxiety symptoms than the other self-reported scales. HAM-A scale is widely used today in clinical research setting to detect the current state of psychopathology of a subject.[40] ZSDS is a valid and sensitive scale used effectively to assess the depression state of an individual.[41] Both ZSDS values and HAM-A values were high in group I patients and showed a positive relationship with cortisol levels. Very few subjects in the other two groups showed lower ZSDS and HAM-A values with high cortisol levels. This reveals that a significant number of individuals showed direct relationship of the severity of stress with cortisol levels. Some other studies reported earlier revealed that the association between cortisol levels and stress is not regular, due to various factors like how an individual deals with stress by different strategies of coping stress in the HPA axis (cortisol).[36]
Yoga is now considered as a new form of medicine that integrates an individual's physical, mental, and spiritual components to improve health in a stress-related illness.[42] Evidence shows that stress causes negative emotional states in an individual, which would contribute to the etiology of various chronic diseases. In recent years, millions of people all over the world are practising yoga to overcome stress in everyday life and now it is regarded as a CAM in treating stress-related anxiety and depression.[43] In the present study, a total of 23 patients who were practicing yoga showed significantly less anxiety and depression scores similar to the scores of non-stress individuals. Plaque scores, probing depth and CAL both at 5–8 mm and >8 mm were low when compared with other groups, suggesting that regular practice of yoga improves physical health, fitness, and relieves stress, thus enhancing the oral hygiene and periodontal health status.
CONCLUSION
Studies to date strongly suggest that psychosocial stress is an important risk indicator for systemic diseases such as diabetes, cardiovascular disease, preterm delivery, osteoporosis, and periodontal disease. Yoga practice may help to improve systemic health of patients, reduced depression and anxiety, and cause better wound healing, and might have therapeutic benefits in the severity or progression of periodontal diseases like other chronic inflammatory diseases which are influenced by various risk factors such as stress. As mind–body fitness programs such as yoga continue to increase, it is important for healthcare professionals to inform about the nature of yoga and its therapeutic effects.
This early observation of association of yoga with periodontal disease will require further extensive studies to understand the benefits of yoga in stress relief, as well as its benefits in the control of periodontal disease progression and maintenance.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Genco RJ, Ho AW, Grossi SG, Dunford RG, Tedesco LA. Relationship of stress, distress, and inadequate coping behaviors to periodontal disease. J Periodontol. 1999;70:711–23. doi: 10.1902/jop.1999.70.7.711. [DOI] [PubMed] [Google Scholar]
- 2.Grossi SG, Zambon JJ, Ho AW, Koch G, Dunford RG, Machtei EE, et al. Assessment of risk for periodontal disease. I. Risk indicators for attachment loss. J Periodontol. 1994;65:260–7. doi: 10.1902/jop.1994.65.3.260. [DOI] [PubMed] [Google Scholar]
- 3.Grossi SG, Genco RJ, Machtei EE, Ho AW, Koch G, Dunford R, et al. Assessment of risk for periodontal disease. II. Risk indicators for alveolar bone loss. J Periodontol. 1995;66:23–9. doi: 10.1902/jop.1995.66.1.23. [DOI] [PubMed] [Google Scholar]
- 4.Boyapati L, Wang HL. The role of stress in periodontal disease and wound healing. Periodontol 2000. 2007;44:195–210. doi: 10.1111/j.1600-0757.2007.00211.x. [DOI] [PubMed] [Google Scholar]
- 5.Miller SC, Firestone JM. Psychosomatic factors in the etiology of periodontal disease; a critical review of the literature. Oral Surg Oral Med Oral Pathol. 1947;33:675–86. doi: 10.1016/0096-6347(47)90119-1. [DOI] [PubMed] [Google Scholar]
- 6.Moulton R, Ewen S, Thieman W. Emotional factors in periodontal disease. Oral Surg Oral Med Oral Pathol. 1952;5:833–60. doi: 10.1016/0030-4220(52)90314-9. [DOI] [PubMed] [Google Scholar]
- 7.Belting CM, Gupta OP. The influence of psychiatric disturbances on the severity of periodontal disease. J Periodontol. 1961;32:219–26. [Google Scholar]
- 8.Green LW, Tryon WW, Marks B, Huryn J. Periodontal disease as a function of life events stress. J Human Stress. 1986;12:32–6. doi: 10.1080/0097840X.1986.9936764. [DOI] [PubMed] [Google Scholar]
- 9.Cupps TR, Fauci AS. Corticosteroid-mediated immunoregulation in man. Immunol Rev. 1982;65:133–55. doi: 10.1111/j.1600-065x.1982.tb00431.x. [DOI] [PubMed] [Google Scholar]
- 10.Williams TJ, Yarwood H. Effect of glucocorticosteroids on microvascular permeability. Am Rev Respir Dis. 1990;141:39–43. [PubMed] [Google Scholar]
- 11.Genco RJ, Ho AW, Kopman J, Grossi SG, Dunford RG, Tedesco LA. Models to evaluate the role of stress in periodontal disease. Ann Periodontol. 1998;3:288–302. doi: 10.1902/annals.1998.3.1.288. [DOI] [PubMed] [Google Scholar]
- 12.Daynes RA, Araneo BA. Contrasting effects of glucocorticoids on the capacity of T cells to produce the growth factors interleukin 2 and interleukin 4. Eur J Immunol. 1989;19:2319–25. doi: 10.1002/eji.1830191221. [DOI] [PubMed] [Google Scholar]
- 13.Williams K, Steinberg L, Petronis J. Therapeutic application of Iyengar yoga for healing chronic low back pain. Int J Yoga Ther. 2003;13:55–67. [Google Scholar]
- 14.Raub JA. Psychophysiologic effects of Hatha yoga on musculoskeletal and cardiopulmonary function: A literature review. J Altern complement Med. 2002;8:797–812. doi: 10.1089/10755530260511810. [DOI] [PubMed] [Google Scholar]
- 15.Lipton L. Using yoga to treat disease: An evidence-based review. JAAPA. 2008;21:34–6. doi: 10.1097/01720610-200802000-00012. [DOI] [PubMed] [Google Scholar]
- 16.Vadiraja HS, Raghavendra RM, Nagarathna R, Nagendra HR, Rekha M, Vanitha N, et al. Effects of a yoga program on cortisol rhythm and mood states in early breast cancer patients undergoing adjuvant radiotherapy: A randomized controlled trial. Integr Cancer Ther. 2009;8:37–46. doi: 10.1177/1534735409331456. [DOI] [PubMed] [Google Scholar]
- 17.McCall T. Yoga as Medicine. New York: Bantam Dell a Division of Random House Inc; 2007. [Google Scholar]
- 18.Laster J. The heart of Patanjali. Yoga J. 1997;137:134–44. [Google Scholar]
- 19.Hamilton M. The assessment of anxiety states by rating. Br J Med Psychol. 1959;32:50–5. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- 20.Zung WW. A self-rating depression scale. Arch Gen Psychiatry. 1965;12:63–70. doi: 10.1001/archpsyc.1965.01720310065008. [DOI] [PubMed] [Google Scholar]
- 21.Rai B, Kaur J, Anand SC, Jacobs R. Salivary stress markers, stress, and periodontitis: A pilot study. J Periodontol. 2011;82:287–92. doi: 10.1902/jop.2010.100319. [DOI] [PubMed] [Google Scholar]
- 22.Löe H. The gingival index, the plaque index and the retention index systems. J Periodontol. 1967;38(Suppl):610–6. doi: 10.1902/jop.1967.38.6.610. [DOI] [PubMed] [Google Scholar]
- 23.LeResche L, Dworkin SF. The role of stress in inflammatory disease, including periodontal disease: Review of concepts and current findings. Periodontol 2000. 2002;30:91–103. doi: 10.1034/j.1600-0757.2002.03009.x. [DOI] [PubMed] [Google Scholar]
- 24.Kamma JJ, Giannopoulou C, Vasdekis VG, Mombelli A. Cytokine profile in gingival crevicular fluid of aggressive periodontitis: Influence of smoking and stress. J Clin Periodontol. 2004;31:894–902. doi: 10.1111/j.1600-051X.2004.00585.x. [DOI] [PubMed] [Google Scholar]
- 25.Moss ME, Beck JD, Kaplan BH, Offenbacher S, Weintraub JA, Koch GG, et al. Exploratory case control analysis of psychosocial factors and adult periodontitis. J Periodontol. 1996;67(Suppl):1060–9. doi: 10.1902/jop.1996.67.10s.1060. [DOI] [PubMed] [Google Scholar]
- 26.Houri-Haddad Y, Itzchaki O, Ben-Nathan D, Shapira L. The effect of chronic emotional stress on the humoral immune response to porphyromonas gingivalis in mice. J Periodontal Res. 2003;38:204–9. doi: 10.1034/j.1600-0765.2003.20390.x. [DOI] [PubMed] [Google Scholar]
- 27.Marcenes WS, Sheiham A. The relationship between work stress and oral health status. Soc Sci Med. 1992;35:1511–20. doi: 10.1016/0277-9536(92)90054-t. [DOI] [PubMed] [Google Scholar]
- 28.Bagga OP, Gandhi A. A comparative study of the effect of transcedential meditation (T.M.) and shavasana practice on cardiovascular system. Indian Heart J. 1983;35:39–45. [PubMed] [Google Scholar]
- 29.Kamei T, Toriumi Y, Kimura H, Ohno S, Kumano H, Kimura K. Decrease in serum cortisol during yoga exercise is correlated with alpha wave activation. Percept Mot Skills. 2000;90:1027–32. doi: 10.2466/pms.2000.90.3.1027. [DOI] [PubMed] [Google Scholar]
- 30.Schmidt T, Wijga A, Von Zur Mühlen A, Brabant G, Wagner TO. Changes in cardiovascular risk factors and hormones during a comprehensive residential three month kriya yoga training and vegetarian nutrition. Acta Physiol Scand Suppl. 1997;640:158–62. [PubMed] [Google Scholar]
- 31.Rosania AE, Low KG, McCormick CM, Rosania DA. Stress, depression, cortisol and periodontal disease. J Periodontol. 2009;80:260–6. doi: 10.1902/jop.2009.080334. [DOI] [PubMed] [Google Scholar]
- 32.Johannsen A, Asberg M, Söder PO, Söder B. Anxiety, gingival inflammation and periodontal disease in non-smokers and smokers-an epidemiological study. J Clin Peridontol. 2005;32:488–91. doi: 10.1111/j.1600-051X.2005.00704.x. [DOI] [PubMed] [Google Scholar]
- 33.Klages U, Weber AG, Wehrbein H. Approximal plaque and gingival sulcus bleeding in routine dental care patients: Relations to life stress, somatization and depression. J Clin Periodontol. 2005;32:575–82. doi: 10.1111/j.1600-051X.2005.00716.x. [DOI] [PubMed] [Google Scholar]
- 34.Deinzer R, Hilpert D, Bach K, Schawacht M, Herforth A. Effects of academic stress on oral hygiene--a potential link between stress and plaque-associated disease? J Clin Periodontol. 2001;28:459–64. doi: 10.1034/j.1600-051x.2001.028005459.x. [DOI] [PubMed] [Google Scholar]
- 35.Abegg C, Croucher R, Marcenes WS, Sheiham A. How do routines of daily activities and flexibility of daily activities affect tooth-cleaning behaviour? J Public Health Dent. 2000;60:154–8. doi: 10.1111/j.1752-7325.2000.tb03321.x. [DOI] [PubMed] [Google Scholar]
- 36.Vettore MV, Leão AT, Monteiro Da Silva AM, Quintanilha RS, Lamarca GA. The relationship of stress and anxiety with chronic periodontitis. J Clin Periodontol. 2003;30:394–402. doi: 10.1034/j.1600-051x.2003.10271.x. [DOI] [PubMed] [Google Scholar]
- 37.Mengel R, Bacher M, Flores-De-Jacoby L. Interactions between stress, interleukin-1beta, interleukin-6 and cortisol in periodontally diseased patients. J Clin Periodontol. 2002;29:1012–22. doi: 10.1034/j.1600-051x.2002.291106.x. [DOI] [PubMed] [Google Scholar]
- 38.Cury PR, Araújo VC, Canavez F, Furuse C, Araújo NS. Hydrocortisone affects the expression of matrix metalloproteinases (MMP-1, -2, -3, -7, and -11) and tissue inhibitor of matrix metalloproteinases (TIMP-1) in human gingival fibroblasts. J Periodontol. 2007;78:1309–15. doi: 10.1902/jop.2007.060225. [DOI] [PubMed] [Google Scholar]
- 39.Buckingham JC, Loxley HD, Christian HC, Philip JG. Activation of the HPA axis by immune insults: Roles and interactions of cytokines, eicosanoids, glucocorticoids. Pharmacol Biochem Behav. 1996;54:285–98. doi: 10.1016/0091-3057(95)02127-2. [DOI] [PubMed] [Google Scholar]
- 40.Nayak SU, Nayak DG, Uppoor AS, Pai KK. Evaluation of cortisol levels in gingival crevicular fluid and saliva in anxious and non-anxious patients with chronic periodontitis. Dent Res J (Isfahan) 2013;10:474–81. [PMC free article] [PubMed] [Google Scholar]
- 41.Szklo-Coxe M, Young T, Peppard PE, Finn LA, Benca RM. Prospective associations of insomnia markers and symptoms with depression. Am J Epidemiol. 2010;171:709–20. doi: 10.1093/aje/kwp454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Atkinson NL, Permuth-Levine R. Benefits, barriers, and cues to action of yoga practice: A focus group approach. Am J Health Behav. 2009;33:3–14. doi: 10.5993/ajhb.33.1.1. [DOI] [PubMed] [Google Scholar]
- 43.Chen KM, Chen MH, Lin MH, Fan JT, Lin HS, Li CH. Effects of yoga on sleep quality and depression in elders in assisted living facilities. J Nurs Res. 2010;18:53–61. doi: 10.1097/JNR.0b013e3181ce5189. [DOI] [PubMed] [Google Scholar]


