Abstract
Purpose:
To evaluate choroidal thickness (CT) change in various grades of diabetic retinopathy (DR) in comparison to age-matched healthy subjects.
Methods:
This prospective observational study included 227 eyes of 125 subjects with diabetes (study group: 58 females) and 197 eyes of 110 age-matched healthy subjects (control group: 66 females). Collected data included age, gender, duration of diabetes, glycemic control, comprehensive ocular examination, fundus photography, and CT measurement on spectral domain ocular coherence tomography using enhanced depth imaging.
Results:
Mean age in the study group was 57.0 ± 9.37 years (43–73 years). The mean age was 41.48 ± 5.43 years in the control group. Subjects with diabetes with (252.8 ± 55.6 microns) and without (261.71 ± 51.8 microns) retinopathy had significantly thinner choroids when compared to the control group (281.7 ± 47.7 microns; P = 0.032). Seventy-four of 227 eyes did not have any evidence of DR, 89 eyes had features of nonproliferative diabetic retinopathy (NPDR), and 33 eyes had treatment naïve proliferative diabetic retinopathy (PDR). Thirty-one PDR eyes had received previous laser photocoagulation. Subjects with diabetes without retinopathy had a greater subfoveal choroidal thickness (SFCT) than subjects with diabetes with retinopathy (P < 0.001). Eyes with PDR (243.9 ± 56.2 microns) had thinner SFCT than those with NPDR (238.98 ± 111.23 microns). There was no difference in the SFCT between treated (laser photocoagulation done; 251.784 ± 103.72 microns) and treatment naïve PDR (258.405 ± 89.47 microns, P = 0.23).
Conclusions:
Control eyes had greater SFCT compared to subjects with diabetes, with and without retinopathy. The thinning progressed with increasing severity of DR. Choroidal thinning may contribute to DR pathogenesis.
Keywords: Choroidal thickness, diabetic retinopathy, nonproliferative diabetic retinopathy, proliferative diabetic retinopathy
The choroid receives a large proportion of ocular blood flow and is responsible for the supply of nutrition to the outer retinal layers. It follows that alterations in choroidal structure or vasculature may affect the retinal function. With the advent of enhanced depth imaging (EDI) in ocular coherence tomography for assessment of the choroid,[1,2,3,4] studies have looked at changes in choroidal structure to provide possible clues to the pathogenesis of disorders such as central serous chorioretinopathy,[5] polypoidal choroidal vasculopathy,[6,7] glaucoma, and age-related macular degeneration.[7]
Findings on scanning electron microscopy in eyes with long-standing diabetes include increased vascular tortuosity, dilation and narrowing, hypercellularity, vascular loop and microaneurysm formation, “drop-out” of choriocapillaries, and sinus-like structure formation between choroidal lobules.[8,9] Blood flow through the choroid also appears to be reduced in subjects with diabetes, especially those with macular edema (ME).[10] In vivo evaluation of choroid using EDI has also shown various changes in choroidal structures in recent literature.[11,12,13,14] It thus follows that, structural alterations in the choroid, if any, may contribute to the pathogenesis of diabetic retinopathy (DR). While analyses of data on choroidal thickness (CT) in subjects with diabetes have been published, recent studies have reported conflicting results. A large population-based study from China reported choroidal thickening in subjects with diabetes, however, DR did not appear to be associated with increased CT.[11] A recent retrospective study from Korea, demonstrated increasing CT with increasing severity of retinopathy.[15] A recent article from Italy, however, reported a significant thinning of the subfoveal choroid in patients with diabetes as compared to controls.[16] There are other reports that suggest choroidal thinning in subjects with diabetes[13,14,17] and increasing thinning with progressive retinopathy.[17] As is evident, there are conflicting reports from several regions of the world on the expected choroidal changes in subjects with diabetes and its relationship with the severity of the DR. Whether ethnicity contributes to this discrepancy, is as of now unknown.
It is thus necessary to evaluate the changes in CT in subjects with diabetes with and without DR and to compare it with age-matched controls. There are no reports from India with regard to CT profile in the subjects with diabetes. This study aims to evaluate CT change in various grades of DR as compared to age-matched healthy subjects and its relationship with various factors such as age, gender, spherical equivalent (SE), and duration of diabetes as well as its correlation with the best corrected distance visual acuity.
Methods
This prospective study was performed from September 2012 to July 2013. Prior approval from the Institutional Review Board of the Institute was used and informed consent was obtained from each study subject. This study was conducted in accordance with the tenets of the Declaration of Helsinki.
For inclusion in the study group, participants were required to have a history of diabetes mellitus (DM) Type II treated with either oral hypoglycemic agents or insulin. The duration of diabetes, recent control of diabetes, and associated systemic illness(es), if any, were noted. All participants underwent a comprehensive ophthalmic examination including visual acuity testing, slit-lamp biomicroscopy, intraocular pressure (IOP) measurement using the Goldmann applanation tonometer and dilated fundoscopic examination. DR classification was performed as per Early Treatment Diabetic Retinopathy Study (ETDRS) criteria.[18] In case there was any doubt as to the stage of DR, fundus fluorescein angiography was performed. Exclusion criteria included history of pan-retinal photocoagulation within 6 months, high myopia or hyperopia (> −6 or + 3 diopters [D] of refractive error), poor image quality, any other associated retinal pathology, or history of any intraocular surgery (other than uncomplicated cataract surgery). The control group consisted of nondiabetics, based on history and laboratory investigations, healthy subjects with no ocular disease and without high refractive power (more than − 6D or + 3D). The patient's glycemic control at the time of entry into the study was noted. For the purpose of this study, a HbA1c level of 6.9% or less was deemed to be “good control,” whereas a level of 7% or more was considered as “uncontrolled diabetes.”
Earlier studies have reported a wide range of difference (thickening or thinning) in the subfoveal choroidal thickness (SFCT) between subjects with and without diabetes (up to 30%), depending on whether they had diabetic ME or treated proliferative diabetic retinopathy (PDR);[12,15] given that these studies were retrospective, there was no sample size calculation performed. This study was designed to detect a 15% difference in the CT between subjects with and without diabetes, with 95% confidence interval. The required sample size was estimated to be 195 eyes in each group. We assumed an attrition rate of 15% at the time of recruitment.
Choroidal imaging
The spectral domain-optical coherence tomography (OCT) scans were obtained by using Cirrus HD-OCT (Carl Zeiss Meditec, Inc., Dublin, CA, USA) after dilatation of the pupil with 1% tropicamide and 10% phenylephrine eye drops. The scan used for imaging in this study is the HD 1-line raster with EDI, which is a 6-mm line consisting of 4096 A-scans, an imaging speed of 27,000 A-scans per second, an axial resolution of 5 microns, and a transverse resolution of 15 microns in tissue and averages 20 frames (B-scans). EDI, which automatically sets the choroid closer to the zero-delay line and thus theoretically provides better visualization of the choroidal-scleral interface, was used for all scans. Scan 3 of the 5, which passes through the fovea, was used for all measurements. Only scans with a signal strength of more or equal to 6 were used for analysis. Scans with a signal strength of more or equal to 6 were used for analysis.
Using the Cirrus linear measurement tool, single observer measured CT, which is defined as the vertical distance from the hyperreflective line of the retinal pigment epithelium along the direction of the scan to the hyperreflective line of the inner surface of the sclera, at 500 microns intervals temporal and nasal from the fovea, up to 3000 microns as published in the literature.[19] Intraclass correlation coefficient for intraobserver reproducibility was 0.97 (95% confidence interval: 0.96–0.98).
Statistical analysis
Descriptive statistics included mean and standard deviation for continuous variables. As both eyes of most subjects were included for analysis, the correlation between the two eyes of the same subject was adjusted using generalized estimating equations (GEEs) during the calculation of the summary of the descriptive parameters. Univariate regression models (based on past studies) were adjusted using GEE and were used to assess significant associations between CT and independent parameters such as age, gender, and duration of diabetes. One-way analysis of variance (ANOVA) and the unpaired t-test were used wherever appropriate. The multivariate models that were adjusted using GEE methods were used to assess the effects of age, gender, SE, and macular thickness on the CT measurements. Statistical analyses were performed using MedCalc for Windows, version 12.5 (MedCalc Software, Ostend, Belgium). The alpha level (Type I error) was set at 0.01. All the graphs were performed using GraphPad Prism version 6.00 for Windows (GraphPad Software, La Jolla California, USA, www.graphpad.com). Statistical significance was set at P < 0.05.
Results
The study group had 227 eyes of 125 subjects (58 females) with diabetes with a mean age of 57.0 ± 9.37 years (43–73 years) for analysis as per our eligibility criteria. Mean best-corrected visual acuity (BCVA) was 0.34 ± 0.29 logarithm of minimum angle of resolution (log MAR) (range: 0.0–1.32 log MAR). Forty-two eyes were pseudophakic. Mean SE was 0.05 ± 1.31 D. Mean central macular thickness (CMT) was 280.76 ± 134.7 microns. Mean SFCT was 252.86 ± 55.61 microns. Out of 227 eyes, 74 eyes did not have any evidence of DR, 89 eyes had features of non-PDR (NPDR), and 33 eyes had treatment naïve PDR. Thirty-one eyes had received previous laser photocoagulation for PDR. The baseline characteristics are shown in Table 1.
Table 1.
Baseline characteristics among the study groups
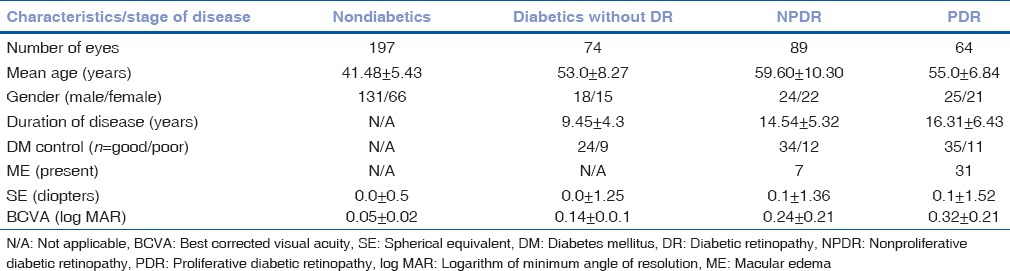
The control group eventually consisted of 197 eyes of 110 healthy subjects for analysis. The mean age was 41.48 ± 5.43 years, with 66 females. Mean SE was 0.17 ± 0.67 D. Mean CMT was 216.86 ± 29.19 microns and mean SFCT was 281.7 ± 47.7 microns.
When SFCT was compared between the subjects with diabetes without any retinopathy (mean SFCT = 261.71 ± 51.8 microns), subjects with diabetes with any form of DR (mean SFCT = 252.8 ± 55.6 microns) and age-matched healthy subjects (mean SFCT = 281.7 ± 47.7 microns), there was a statistically significant difference noted (P = 0.032).
A statistically significant subfoveal choroidal thinning was noted (P < 0.001) in eyes with DR when compared to subjects with diabetes without DR. Eyes with DR had a significantly thinner subfoveal choroid than age-matched healthy eyes (P < 0.011) [Table 2].
Table 2.
Mean choroidal thickness±standard deviation at various locations from fovea in eyes with age-matched subjects without diabetes, no diabetic retinopathy, nonproliferative diabetic retinopathy, and proliferative diabetic retinopathy in subjects with diabetes
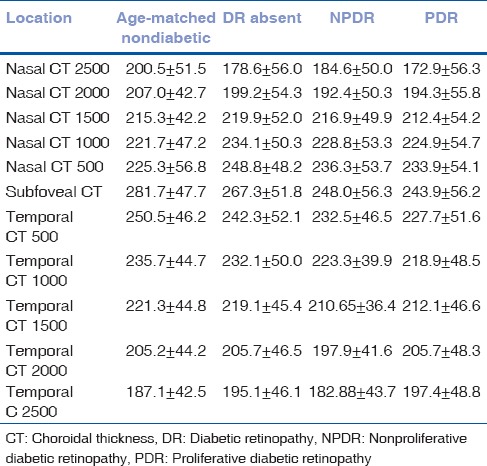
SFCT in eyes with DR, who had undergone pan-retinal photocoagulation (mean SFCT = 258.4 ± 48.3 microns), was not significantly different from eyes that had not undergone pan-retinal photocoagulation (mean SFCT = 251.78 ± 56.9 microns, P = 0.23).
The SFCT decreased with increasing severity of DR. Patients with PDR had statistically significantly (P = 0.021) thinner subfoveal choroids as compared to those with NPDR [Table 2].
The mean SFCT in eyes with ME (256.629 ± 55.24 microns) was not significantly different from eyes without ME (246.805 ± 55.61 microns, P = 0.196). Mean central macular thickness in patients with and without ME was 369.805 ± 131.24 and 225.429 ± 127.47 microns, respectively (P < 0.001).
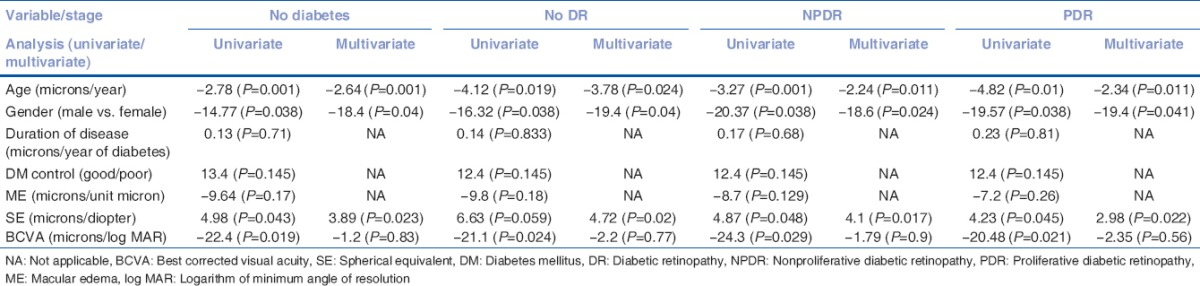
On univariate regression, age, gender, SE as well as BCVA were the significant factors affecting SFCT. However, on multivariate regression, age, gender, and SE were the only factors significantly associated with CT [Table 3]. This was true for all groups.
Table 3.
Univariate and multivariate regression analysis between the various factors and choroidal thickness
Discussion
Our study clearly shows the effect of diabetes on CT. The subjects with diabetes have statistically significant subfoveal choroidal thinning as compared to age-matched controls. In addition, patients with diabetes but without DR had a greater SFCT when compared to subjects with diabetes with DR. The CT was affected by the severity of DR; eyes with PDR had thinner choroids compared to those with NPDR. These findings are in contrast to the Beijing Eye Study,[11] which reported no significant difference in the CT between subjects with diabetes with and without retinopathy. However, the Beijing Eye Study was a population-based study and only 23 patients out of 2041 subjects had DR.
Our findings are in tandem with previous studies reporting choroidal thinning in subjects with diabetes compared to subjects without diabetes. Most studies as per past literature report a progressively decreasing CT with an increasing severity of retinopathy similar to our report.[14,15] There is, however, published literature to the contrary. The Beijing Eye Study[11] reports that there was a significant increase in CT with stage of DR. While admittedly they have the largest sample size and have explored a wide variety of associations, they have only 23 subjects with DR; moreover, most of the patients in the study had minimal retinopathy. This is quite unlike the other studies (including ours), which were hospital-based studies and conducted in referral centers. These studies include eyes with all stages of DR and probably provide more evidence about the change in CT in DR. A hospital-based study from Korea[15] reports an increased CT in patients with increasing severity of DR, and while the exact mechanism as they state is unknown, there is conflicting evidence on the change in retinal blood flow and pulsatile ocular blood flow in subjects with diabetes.[10,20,21] A discussion on ocular blood flow, as well as its effect on CT, however, is beyond the scope of this study.
In our study, the presence of ME did not correlate with the CT. Past literature[10,22,23] has shown reduced blood flow through the choroid in subjects with diabetes, and some studies speculate that the thinner choroid indicates an overall reduction in blood flow in patients with diabetic ME (which might possibly contribute to the pathogenesis of diabetic ME, possibly by resultant relative ischemia). Thus, diabetic ME might not be due solely to retinal dysfunction. In addition, a previous study[12] states that it is unclear whether the choroidal thinning is primary or secondary to the retinal ischemia. This study suggests that choroidal thinning precedes the onset of retinal pathology, and the thinning increases with progressive worsening of the retinopathy.
Univariate correlation showed a significant relationship of age, gender, SE, and BCVA with CT. However, multivariate regression analysis revealed that the age, gender, and SE were the only significant factors affecting CT in all grades of DR. The duration of diabetes and glycemic control did not appear to influence the CT; however, as stated earlier, the severity of the diabetes was closely correlated with CT. We speculate that circulatory disturbance contributes to choroidal thinning and that both retinal and choroidal circulatory disturbances contribute to DR.
We did not perform a correlation analysis of various factors such as level of education or urban/rural habitat with CT, as performed in the Beijing Eye Study[11] as the importance of these factors in clinical settings is questionable. In our study, choroidal imaging was not performed at a specific time of the day, therefore, we cannot rule out the effect of diurnal variation on the CT as reported previously.[24]
One of the limitations of this study was that our study does not provide any information about the CT profile of macular area due to an inability to measure CT in nine ETDRS sectors with Cirrus HD-OCT®. Axial length correlates better with CT, especially in eyes with high myopia and pseudophakia. We did not measure axial length in our study; however, we excluded eyes with high refractive errors. We also did not study the influence of IOP on CT.
To conclude, significant choroidal thinning appears to be a feature in subjects with diabetes, especially those with advanced DR. It probably contributes to the pathogenesis of DR. These findings may explain persistent derangement of retinal function in patients who have been treated adequately, both for ocular and systemic manifestations of diabetes. Further studies, however, are warranted to conclusively establish the role of the choroid in retinal dysfunction and the pathogenesis of DR. This is to the best of our knowledge the largest prospective series looking at the SFCT in subjects of Indian ethnicity with Type II DM.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Fujiwara T, Imamura Y, Margolis R, Slakter JS, Spaide RF. Enhanced depth imaging optical coherence tomography of the choroid in highly myopic eyes. Am J Ophthalmol. 2009;148:445–50. doi: 10.1016/j.ajo.2009.04.029. [DOI] [PubMed] [Google Scholar]
- 2.Margolis R, Spaide RF. A pilot study of enhanced depth imaging optical coherence tomography of the choroid in normal eyes. Am J Ophthalmol. 2009;147:811–5. doi: 10.1016/j.ajo.2008.12.008. [DOI] [PubMed] [Google Scholar]
- 3.Rahman W, Chen FK, Yeoh J, Patel P, Tufail A, Da Cruz L. Repeatability of manual subfoveal choroidal thickness measurements in healthy subjects using the technique of enhanced depth imaging optical coherence tomography. Invest Ophthalmol Vis Sci. 2011;52:2267–71. doi: 10.1167/iovs.10-6024. [DOI] [PubMed] [Google Scholar]
- 4.Spaide RF, Koizumi H, Pozzoni MC. Enhanced depth imaging spectral-domain optical coherence tomography. Am J Ophthalmol. 2008;146:496–500. doi: 10.1016/j.ajo.2008.05.032. [DOI] [PubMed] [Google Scholar]
- 5.Imamura Y, Fujiwara T, Margolis R, Spaide RF. Enhanced depth imaging optical coherence tomography of the choroid in central serous chorioretinopathy. Retina. 2009;29:1469–73. doi: 10.1097/IAE.0b013e3181be0a83. [DOI] [PubMed] [Google Scholar]
- 6.Chung SE, Kang SW, Lee JH, Kim YT. Choroidal thickness in polypoidal choroidal vasculopathy and exudative age-related macular degeneration. Ophthalmology. 2011;118:840–5. doi: 10.1016/j.ophtha.2010.09.012. [DOI] [PubMed] [Google Scholar]
- 7.Koizumi H, Yamagishi T, Yamazaki T, Kawasaki R, Kinoshita S. Subfoveal choroidal thickness in typical age-related macular degeneration and polypoidal choroidal vasculopathy. Graefes Arch Clin Exp Ophthalmol. 2011;249:1123–8. doi: 10.1007/s00417-011-1620-1. [DOI] [PubMed] [Google Scholar]
- 8.Fryczkowski AW. Diabetic choroidal involvement: Scanning electron microscopy study. Klin Oczna. 1988;90:145–9. [PubMed] [Google Scholar]
- 9.Fryczkowski AW, Sato SE, Hodes BL. Changes in the diabetic choroidal vasculature: Scanning electron microscopy findings. Ann Ophthalmol. 1988;20:299–305. [PubMed] [Google Scholar]
- 10.Nagaoka T, Kitaya N, Sugawara R, Yokota H, Mori F, Hikichi T, et al. Alteration of choroidal circulation in the foveal region in patients with type 2 diabetes. Br J Ophthalmol. 2004;88:1060–3. doi: 10.1136/bjo.2003.035345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Xu J, Xu L, Du KF, Shao L, Chen CX, Zhou JQ, et al. Subfoveal choroidal thickness in diabetes and diabetic retinopathy. Ophthalmology. 2013;120:2023–8. doi: 10.1016/j.ophtha.2013.03.009. [DOI] [PubMed] [Google Scholar]
- 12.Regatieri CV, Branchini L, Carmody J, Fujimoto JG, Duker JS. Choroidal thickness in patients with diabetic retinopathy analyzed by spectral-domain optical coherence tomography. Retina. 2012;32:563–8. doi: 10.1097/IAE.0b013e31822f5678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Esmaeelpour M, Považay B, Hermann B, Hofer B, Kajic V, Hale SL, et al. Mapping choroidal and retinal thickness variation in type 2 diabetes using three-dimensional 1060-nm optical coherence tomography. Invest Ophthalmol Vis Sci. 2011;52:5311–6. doi: 10.1167/iovs.10-6875. [DOI] [PubMed] [Google Scholar]
- 14.Esmaeelpour M, Brunner S, Ansari-Shahrezaei S, Nemetz S, Povazay B, Kajic V, et al. Choroidal thinning in diabetes type 1 detected by 3-dimensional 1060 nm optical coherence tomography. Invest Ophthalmol Vis Sci. 2012;53:6803–9. doi: 10.1167/iovs.12-10314. [DOI] [PubMed] [Google Scholar]
- 15.Kim JT, Lee DH, Joe SG, Kim JG, Yoon YH. Changes in choroidal thickness in relation to the severity of retinopathy and macular edema in type 2 diabetic patients. Invest Ophthalmol Vis Sci. 2013;54:3378–84. doi: 10.1167/iovs.12-11503. [DOI] [PubMed] [Google Scholar]
- 16.Querques G, Lattanzio R, Querques L, Del Turco C, Forte R, Pierro L, et al. Enhanced depth imaging optical coherence tomography in type 2 diabetes. Invest Ophthalmol Vis Sci. 2012;53:6017–24. doi: 10.1167/iovs.12-9692. [DOI] [PubMed] [Google Scholar]
- 17.Vujosevic S, Martini F, Cavarzeran F, Pilotto E, Midena E. Macular and peripapillary choroidal thickness in diabetic patients. Retina. 2012;32:1781–90. doi: 10.1097/IAE.0b013e31825db73d. [DOI] [PubMed] [Google Scholar]
- 18.Grading diabetic retinopathy from stereoscopic color fundus photographs – An extension of the modified Airlie house classification. ETDRS report number 10. Early treatment diabetic retinopathy study research group. Ophthalmology. 1991;98(5 Suppl):786–806. [PubMed] [Google Scholar]
- 19.Yamashita T, Yamashita T, Shirasawa M, Arimura N, Terasaki H, Sakamoto T. Repeatability and reproducibility of subfoveal choroidal thickness in normal eyes of Japanese using different SD-OCT devices. Invest Ophthalmol Vis Sci. 2012;53:1102–7. doi: 10.1167/iovs.11-8836. [DOI] [PubMed] [Google Scholar]
- 20.Savage HI, Hendrix JW, Peterson DC, Young H, Wilkinson CP. Differences in pulsatile ocular blood flow among three classifications of diabetic retinopathy. Invest Ophthalmol Vis Sci. 2004;45:4504–9. doi: 10.1167/iovs.04-0077. [DOI] [PubMed] [Google Scholar]
- 21.Geyer O, Neudorfer M, Snir T, Goldstein M, Rock T, Silver DM, et al. Pulsatile ocular blood flow in diabetic retinopathy. Acta Ophthalmol Scand. 1999;77:522–5. doi: 10.1034/j.1600-0420.1999.770507.x. [DOI] [PubMed] [Google Scholar]
- 22.Shiragami C, Shiraga F, Matsuo T, Tsuchida Y, Ohtsuki H. Risk factors for diabetic choroidopathy in patients with diabetic retinopathy. Graefes Arch Clin Exp Ophthalmol. 2002;240:436–42. doi: 10.1007/s00417-002-0451-5. [DOI] [PubMed] [Google Scholar]
- 23.Schocket LS, Brucker AJ, Niknam RM, Grunwald JE, DuPont J, Brucker AJ. Foveolar choroidal hemodynamics in proliferative diabetic retinopathy. Int Ophthalmol. 2004;25:89–94. doi: 10.1023/b:inte.0000031744.93778.60. [DOI] [PubMed] [Google Scholar]
- 24.Tan CS, Ouyang Y, Ruiz H, Sadda SR. Diurnal variation of choroidal thickness in normal, healthy subjects measured by spectral domain optical coherence tomography. Invest Ophthalmol Vis Sci. 2012;53:261–6. doi: 10.1167/iovs.11-8782. [DOI] [PubMed] [Google Scholar]


