Abstract
To report a case of giant nodular posterior scleritis mimicking a choroidal tumor. A 42-year-old lady with systemic hypertension presented with a 1-week history of unilateral visual loss, pain and redness in her left eye. Examination showed sectoral anterior episcleritis in her left eye as well as a dome-shaped choroidal mass at the inferior-temporal periphery, associated with retinal hemorrhages and subretinal fluid. Systemic evaluation and imaging of the choroidal mass were performed and could not rule out amelanotic choroidal melanoma. At the same time, she was prescribed a 2-week course of oral nonsteroidal anti-inflammatory drug (NSAID) for her sectoral anterior episcleritis. The choroidal mass was found to have resolved completely right before her scheduled fine needle biospy. Diagnosis of nodular posterior scleritis and a trial of oral NSAID can be considered in patients presenting with a choroidal mass before any invasive procedure.
Keywords: Choroidal tumor, nodular scleritis, posterior scleritis
Posterior scleritis is often an under-recognized entity given its low incidence and variable clinical manifestations. It comprises 10% of all cases of scleritis and is associated with systemic diseases in up to one-third of the cases. 17% of the patients have no detectable physical signs on the first examination.[1] A retrospective review of patients attending the Moorfields Eye Hospital in United Kingdom between 1974 and 1996 showed that posterior scleritis was twice as common in women as in men. The mean age at onset was 49 years.[1] Periocular pain, headache, and visual loss were common presenting symptoms.[1,2] A high index of suspicion is necessary to detect this potentially sight-threatening disease early in its course so that effective therapy can be administered to limit visual loss. Despite growing experiences and diagnostic advances, nodular posterior scleritis continues to be a diagnostic challenge as it can often mimic choroidal melanoma clinically. In a large review of 400 patients referred to the ocular oncology service, nodular scleritis accounted for 1.5% of all lesions resembling choroidal melanoma.[3]
We report a case of giant nodular posterior scleritis, mimicking an amelanotic choroidal melanoma, with complete resolution after nonsteroidal anti-inflammatory drug (NSAID) treatment.
Case Report
A 42-year-old Chinese lady with hypertension presented with decreased vision in her left eye for 1 week. Her best-corrected visual acuity of right and left eye was 20/25 and 20/40 respectively. There was no associated pain, proptosis, diplopia or restricted motility. Intraocular pressures were normal. Slit-lamp examination showed mild sectoral episcleritis over a temporal aspect of her left eye. On fundal examination, there was a dome-shaped choroidal mass of about three disc diameters in size, located in the inferotemporal quadrant with subretinal fluid and overlying retinal hemorrhages. There were no lipofuscin, choroidal folds, vitreous cells, or disc swelling [Fig. 1]. There was bilateral mild hypertensive retinopathy.
Figure 1.
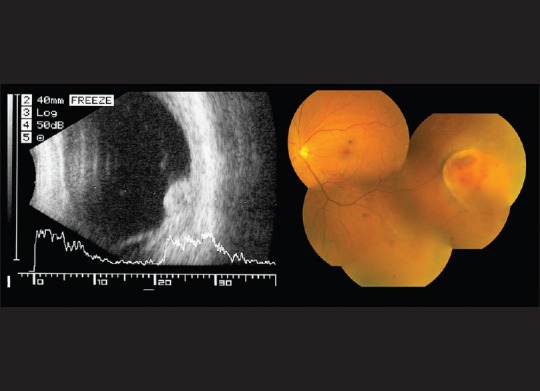
The B-scan ultrasound scan (left) and the composite color fundus photo (right) of the patient's left eye at presentation
B-mode ultrasound confirmed a raised choroidal mass, 3.55 mm thick and 6.99 mm wide at its base, with medium-to-high echogenicity, inferior subretinal fluid, and absence of orbital shadowing. Both fluorescein angiography and indocyanine green angiography showed blocked hypofluorescence of the choroidal mass with multiple leakage sites within and surrounding the mass. There was no evidence of double circulation [Fig. 2].
Figure 2.
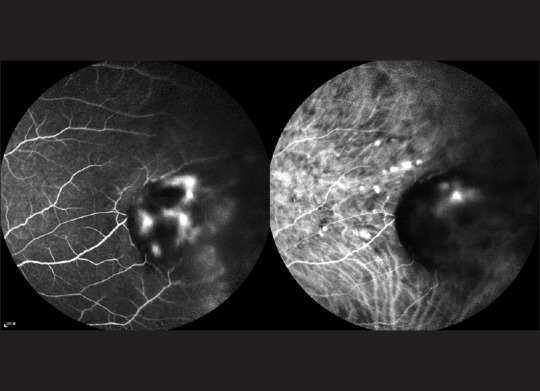
Late phase images of fluorescein angiography and indocyanine angiography of the choroidal mass
Orbital magnetic resonance imaging (MRI) with gadolinium contrast revealed a 4.4 mm × 1.8 mm × 5.8 mm (caudal-cranial × anteroposterior × lateral) T1- hypointense and T2- hyperintense nodule with contrast enhancement at the temporal part of the left globe, bulging into the vitreous. No T1-hyperintense signal was seen in lesion to suggest melanin or subacute hemorrhage. The overlying sclera appeared intact, and there was no infiltration of orbital fat. Features were suggestive of a choroidal tumor such as amelanotic melanoma or choroidal metastasis. Whole-body positron emission tomography-computed tomography scan did not detect any FDG-avid lesion. Choroidal melanoma could not be conclusively excluded at this point. Fine needle aspiration of the choroidal mass was planned to establish a tissue diagnosis.
Preoperatively blood workup including complete blood count, liver function, renal function, syphilis serology, rheumatoid factor, and C-reactive protein were all within normal range. Tumor markers including alpha-fetoprotein, carcinoembryonic antigen, and cancer antigen 153 were also of the normal level. There was an increase in erythrocyte sedimentation rate (ESR) of 71 mm/h, and a raised anti-nuclear antibody (ANA) level of > 1280 (homogenous pattern). Chest X-ray did not show any consolidation or lymphadenopathy suggestive of tuberculosis or sarcoidosis. The patient was referred to an internist for further evaluation. However, she was not diagnosed with any autoimmune disease.
Meanwhile, oral indomethacin 25 mg TDS was given for her sectoral episcleritis. After 10 days, the episcleritis resolved but the choroidal mass remained static. However, at the preoperative visit that was 2 months after her first consultation, the choroidal mass resolved completely. There were pigmented atrophic scar and retinal pigment epithelial changes [Fig. 3]. She was seen again 3 months later with no recurrence of the mass and the best-corrected visual acuity in her left eye returned to 20/20.
Figure 3.
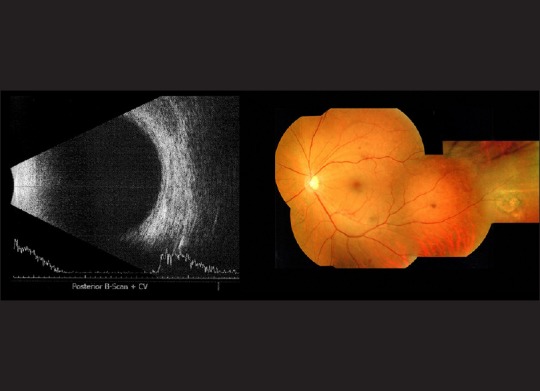
The B-scan ultrasound scan (left) and the composite color fundus photo (right) of the patient's left eye at 2 months after presentation
Discussion
Our case showed that giant nodular posterior scleritis could simulate a choroidal tumor. The initial fundoscopic and radiological findings were suggestive of an amelanotic melanoma. In this case, the episcleritis, elevated ESR and ANA levels and the atypical angiography findings may suggest its inflammatory cause. Despite this, malignancy could not be confidently excluded until the mass resolved upon follow-up. The complete resolution of the lesion after oral NSAID helped us to confirm the diagnosis of nodular posterior scleritis.
Hage et al. also reported two cases of nodular posterior scleritis mimicking choroidal metastasis.[4] Differentiating between them remains a diagnostic challenge. Failure to make the correct diagnosis could lead to misguided treatment. There were reports of cases in which misdiagnosis resulted in misdirected treatment, and even enucleations.[5,6] Symptoms of pain are rarely found in patients with choroidal tumor, and direct questioning of this symptom may be helpful. The subtle ocular redness may be easily overlooked, but this sign is often suggestive of an inflammatory condition. Other features which help us to differentiate posterior scleritis from an amelanotic choroidal mass include orange color of the mass; light transmission on transillumination; hypofluorescence and absence of double circulation on fluorescein angiography; and the presence of scleral thickening, fluid in Tenon's space and absence of posterior acoustic shadowing on B-scan ultrasonography. On MRI, hyperintensity in T1 images reflects paramagnetic substances such as blood, melanin or inflammatory cells. In addition, increased T2 signal intensity adjacent to the nodular lesion is suggestive of an inflammatory process.[7]
Nodular posterior scleritis can be treated by a variety of agents including the use of corticosteroid and nonsteroidal anti-inflammatory agents.[4,8,9] McCluskey et al. used systemic corticosteroids and immunosuppressive therapy when the posterior scleritis involved the optic nerve or was associated systemic diseases.[1] Sridharan et al. treated their case of giant nodular posterior scleritis with a 6-week course of oral steroid.[9] There was one case report of giant nodular posterior scleritis which remained stable with preserved visual acuity without any treatment for years.[10] Our patient received a short-course of oral NSAID with good response. It is this therapeutic response that helped us to confirm the diagnosis of nodular posterior scleritis. Subtle evidence of inflammation such as episcleritis raised autoimmune markers may provide a clue to the diagnosis of this uncommon condition.
Clinical misinterpretation of nodular posterior scleritis as malignant melanoma can lead to misguided therapy and devastating outcomes, including enucleation. When a choroidal mass presents with atypical features of melanoma, any evidence of inflammation may suggest its inflammatory rather than malignant cause. A trial of anti-inflammatory medication may serve as a therapeutic test and help spare patients from invasive and unnecessary interventions.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.McCluskey PJ, Watson PG, Lightman S, Haybittle J, Restori M, Branley M. Posterior scleritis: Clinical features, systemic associations, and outcome in a large series of patients. Ophthalmology. 1999;106:2380–6. doi: 10.1016/S0161-6420(99)90543-2. [DOI] [PubMed] [Google Scholar]
- 2.Biswas J, Mittal S, Ganesh SK, Shetty NS, Gopal L. Posterior scleritis: Clinical profile and imaging characteristics. Indian J Ophthalmol. 1998;46:195–202. [PubMed] [Google Scholar]
- 3.Shields JA, Augsburger JJ, Brown GC, Stephens RF. The differential diagnosis of posterior uveal melanoma. Ophthalmology. 1980;87:518–22. doi: 10.1016/s0161-6420(80)35201-9. [DOI] [PubMed] [Google Scholar]
- 4.Hage R, Jean-Charles A, Guyomarch J, Rahimian O, Donnio A, Merle H. Nodular posterior scleritis mimicking choroidal metastasis: A report of two cases. Clin Ophthalmol. 2011;5:877–80. doi: 10.2147/OPTH.S21255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Accuracy of diagnosis of choroidal melanomas in the Collaborative Ocular Melanoma Study. COMS report no 1. Arch Ophthalmol. 1990;108:1268–73. doi: 10.1001/archopht.1990.01070110084030. [DOI] [PubMed] [Google Scholar]
- 6.Finger PT, Perry HD, Packer S, Erdey RA, Weisman GD, Sibony PA. Posterior scleritis as an intraocular tumour. Br J Ophthalmol. 1990;74:121–2. doi: 10.1136/bjo.74.2.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Osman Saatci A, Saatci I, Kocak N, Durak I. Magnetic resonance imaging characteristics of posterior scleritis mimicking choroidal mass. Eur J Radiol. 2001;39:88–91. doi: 10.1016/s0720-048x(01)00278-9. [DOI] [PubMed] [Google Scholar]
- 8.Shukla D, Kim R. Giant nodular posterior scleritis simulating choroidal melanoma. Indian J Ophthalmol. 2006;54:120–2. doi: 10.4103/0301-4738.25835. [DOI] [PubMed] [Google Scholar]
- 9.Sridharan S, Juneja R, Hussain A, Biswas J. Giant nodular posterior scleritis mimicking choroidal tumor. Retin Cases Brief Rep. 2007;1:65–7. doi: 10.1097/01.ICB.0000264802.71612.1c. [DOI] [PubMed] [Google Scholar]
- 10.Demirci H, Shields CL, Honavar SG, Shields JA, Bardenstein DS. Long-term follow-up of giant nodular posterior scleritis simulating choroidal melanoma. Arch Ophthalmol. 2000;118:1290–2. doi: 10.1001/archopht.118.9.1290. [DOI] [PubMed] [Google Scholar]


