Introduction
Osteoradionecrosis (ORN) remains an unintended debilitating complication of radiation therapy despite the advent of intensity-modulated radiation therapy (IMRT) which aims to deliver doses of radiation to the tumor site while minimizing doses to healthy tissues [[1], [2], [3], [4].
The etiopathogenesis of ORN has been attributed to the avascular effect of radiation to the bone resulting in hypoxia, hypovascularity, and hypocellularity [5], [6]. Radiation-induced fibrosis has also been implicated in the pathophysiology of ORN [7. Recent studies have placed reported incidences of ORN at 1–30% [2], [8], [9], [10], [11]. ORN of the jaw was defined as an area of exposed necrotic bone greater than 1 cm in an area of previous irradiation that failed to heal after 6 months [5]. This definition of ORN has been used for years and still remains the most widely used clinical criterion for the diagnosis of ORN though it fails to incorporate cases with radiologic evidence of necrosis with intact mucosa [5], [12], [13], [14], [15].
Although a report by Van Merkesteyn et al. described a case of ORN of the jaw with intact mucosa [16], subsequently only two series have likewise reported this condition. In 2000, Store and Boysen reported 17 patients with radiographic osteoradionecrosis of the jaw (rORN) with intact mucosa at initial diagnosis as did He et al. in a recent article where they described 16 patients presenting with rORN with intact mucosa [17], [18]Thus, it appears that rORN with intact mucosa is underdiagnosed.
The objectives of this article are to: 1. Describe new cases of rORN with intact mucosa. 2. Correlate the dosimetric analyses of the involved area with the radiographic presentation and to determine the best predictor of rORN with intact mucosa. 3. Propose modification of Store and Boysen’s staging system of ORN. 4. Propose clinical guidelines for early identification of rORN with intact mucosa.
Patients and Methods
The study was approved by the MSKCC Institutional Review Board. The panoramic radiographs of patients who had a dental evaluation before IMRT from 2006 to 2013 at MSKCC were evaluated.
In this study, rORN with intact mucosa was defined as radiological evidence of bone necrosis with intact mucosa within the radiation field but no history of antiresorptive medication use or documentation of tumor recurrence.
Following, exclusion of patients that lack post-radiation therapy panoramic radiographs, the panoramic radiographs of the remaining patients were independently reviewed by 2 dental professionals. The medical records of patients with radiographic lytic lesions were reviewed.
To be included in this category, patients had to fulfill the following criteria: (a) Radiographic lytic lesions with intact mucosa evident on post-radiation and not present on pre-radiation dental evaluation. (b) Lack of known recurrence or metastatic tumor to that site. (c) No history of antiresorptive medication. Patients who met these criteria for rORN with intact mucosa had the affected region of the jaw and contralateral side for comparison contoured to calculate the mean and maximum radiation doses delivered using the MSKCC radiation treatment planning software.
Results
A total of 9 patients (male n = 6, female n = 3) met the criteria and were identified with a diagnosis of rORN with intact mucosa. All cases were in the mandible and the patients’ ages ranged from 39 to 74 years. All patients had a primary squamous cell carcinoma with 6 involving the oropharynx (base of tongue and tonsil) and 2 involving the oral tongue and 1 involving the buccal mucosa.
Areas of rORN with intact mucosa coincided with laterality of tumor site except in Case 2 with bilateral rORN with intact mucosa. Six patients received up to 7000 cGy to the primary tumor site; 5 patients received additional radiation to the neck up to 5040 cGy. All patients received a maximum point radiation dose above 6500 cGy (range 6560–7659 cGy, mean 6984 cGy) to the site of rORN. The mean radiation dose to the site of rORN ranged (from 4752 to 7128 cGy). Case 2 received 7641 cGy and 7659 cGy to the right and left posterior regions of the jaw respectively. All rORN lesions were located in the mandibular molar region. Summary of clinical data, radiation dose prescribed, and calculated radiation dose to the affected sites are presented in.
Seven patients presented with tooth mobility (Cases 1–3, 5, 7–9); 3 out of these 7 patients had natural exfoliation of teeth, one patient who had an extraction of impacted mandibular second and third molars, 7 weeks prior radiation had full mucosal coverage but presented with a continuous dull pain after radiation (Case 6), and one patient presented with discomfort from the right lower jaw (Case 4). Radiographically the lesions presented as ill-defined lytic lesions or mixed lytic and sclerotic areas (, Case 3), and in one patient, the rORN with intact mucosa progressed to a pathological fracture (, Case 6). The follow-up period for all patients ranged from 6 months to 9 years after radiotherapy. Management of these patients has been conservative consisting of proper oral hygiene, encouraging restoration and natural exfoliation of teeth instead of extraction. Summary of symptoms, clinical findings on pre, post-radiation dental examination, follow-up information, and therapy instituted are presented in supplemental online Table S1.
Discussion
Diagnosis of ORN could be challenging due to a lack of standard definition of ORN, with the widely used definition proposed by Marx [12. It does not take into account cases with radiologic evidence of necrosis with intact mucosa. Including this category in a staging system is important because the presence of intact mucosa would not warrant clinicians to further investigate the mandible for any radiologic lytic lesion. The possibility of having an inceptive cancellous bone necrosis before cortical bone thinning, supporting the fact that central radiologic bone changes could occur before the involvement of the peripheral bone and soft tissue after radiation [19.
This condition was first described by Van Merkesteyn et al. [16. Subsequently this condition was reported and elucidated by Store and Boysen in 2000 and they proposed a staging system recognizing the condition (supplemental online Table S2a) [17. In the reported cases by Store and Boysen, all stage 0 patients transitioned to stage II, stage I patients were relatively stable, 9 of 37 stage II patients transitioned to stage I, and 5 of 16 stage III patients transitioned to stage I [17. As 30–50% of bone structural loss is required for detectable radiographic changes to be seen on plain radiographs [20, it is not surprising that all patients in stage 0 transitioned to stage II. We believe that bone exposure by itself makes ORN a more advanced case as compared to rORN with intact mucosa (stage I). Therefore, we would like to modify Store and Boysen’s staging system such that stage 0 corresponds to radiologic evidence of necrotic bone with intact mucosa and stage I to mucosal defects only (supplemental online Table S2b).
Different studies have tried to evaluate what dosimetric values are predictable of the risk of developing ORN [[2], [8], [21]. In our series, maximum dosimetric values were above 6560 cGy, while the mean dosimetric values were above 4752 cGy. Tumor size and site of tumor has been implicated in the dosimetric distribution of radiation doses to the mandible. Our group’s previous study identified that T4 size tumors in the base of tongue had a greater amount of radiation doses to the mandible in all regions compared to T1 and T2 size tumors of the base of tongue [22. One of our cases (Case 2) in this series with a T4 size tumor of the base of tongue received mean radiation doses of over 7000 cGy on both sides of the mandible and presented with rORN with intact mucosa on both sides.
Since this condition may be underdiagnosed, we would like to propose a clinical guideline for the identification of rORN with intact mucosa. We propose that mandibular dosimetry contouring be performed in patients treated with radiation therapy in the head and neck in order to identify patients at high risk for development of rORN. High-risk patients would then undergo yearly radiographic surveillance starting at 1 year post-treatment. Store and Larheim described computed tomography scans as the optimal radiologic tool for diagnosing ORN compared to panoramic radiographs [19. A cone beam computed tomography is a good radiologic assessment tool as it provides better details compared to panoramic radiographs. However, panoramic radiographs could be employed as the first radiographic assessment tool. In our clinical practice, conservative management of these patients have yielded a very good outcome in preventing bone exposure by recommending proper oral hygiene, encouraging restoration and natural exfoliation of teeth instead of extraction. Similar recommendations have been made in the management of patients with medication related osteonecrosis of the jaw [23.
In conclusion, early detection is important for the management of these patients in order to prevent further traumatic manipulation which is imperative to avoiding bone exposure.
Supplementary Material
Figure 1.
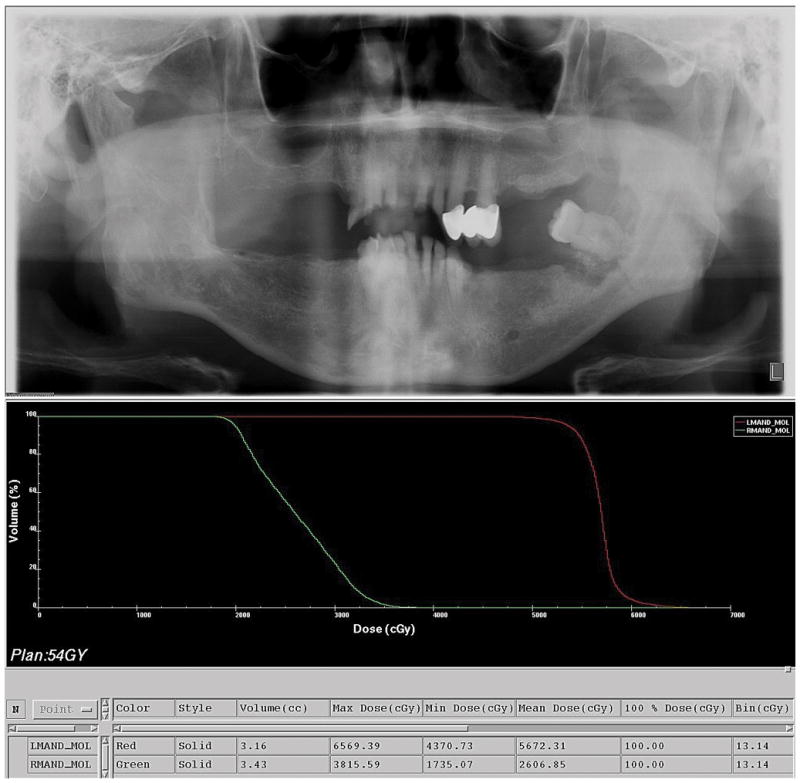
Panoramic radiograph, (Case 3) shows a lytic area in the left molar-ramus region of the mandible (Top). The dose volume histogram showing the amount of radiation doses to the right and left posterior regions of the mandible (Bottom)
Figure 2.
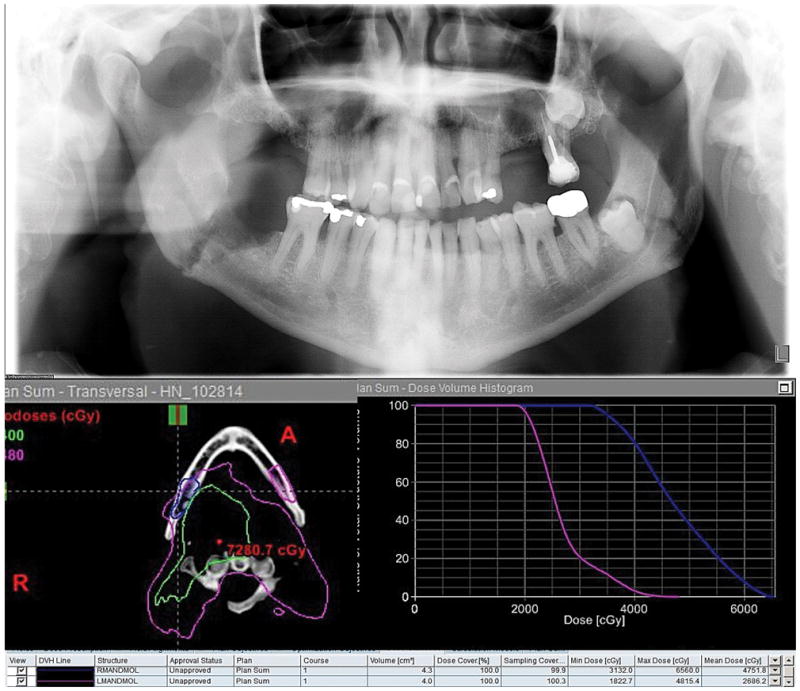
Panoramic radiograph, (Case 6) shows a pathological fracture in the right angle of the mandible (Top). The dose volume histogram showing the amount of radiation doses to the right and left posterior regions of the mandible (Bottom)
Table 1.
Summary of clinical data, radiation dose prescribed, and calculated radiation dose to the affected sites
| Case No | Age | Sex | Cancer diagnosis/Site | Clinical stage | Radiation dose prescribed (Site) (cGy) | Calculated radiation to the affected site(s) (cGy) | |
|---|---|---|---|---|---|---|---|
| Maximum | Mean | ||||||
| 1 | 42 | F | SCC/Left Oral tongue | T2N0M0 | 6600 (oral cavity) | 6808 | 6280 |
| 2 | 52 | F | SCC/Right Base of tongue | T4aN2M0 | 7000 (oropharynx), 5000 (low anterior neck) | 7641 (right), 7659 (left) | 7124 (right), 7128 (left) |
| 3 | 65 | M | SCC/Left Tonsil | T3N1M0 | 7000 (tonsil), 5940 (oropharynx) | 6569 | 5672 |
| 4 | 74 | M | SCC/Right Base of tongue | T1N2bM0 | 7000 (oropharynx and bilateral neck) | 6695 | 5758 |
| 5 | 56 | M | SCC/Right Oral tongue | T3N1M0 | 6600 (oral cavity), 5040 (low anterior neck) | 6866 | 6355 |
| 6 | 66 | M | SCC/Right Tonsil/Base of tongue | T1N1M0 | 7000 (tonsil), 5000 (low anterior neck) | 6560 | 4752 |
| 7 | 60 | M | SCC/Right Base of tongue | T1N2bM0 | 7000 (base of tongue), 5040 (low anterior neck) | 7240 | 5399 |
| 8 | 59 | M | SCC/Left Buccal mucosa | T4N0M0 | 6600 (buccal mucosa), 5000 (low anterior neck) | 6817 | 6730 |
| 9 | 39 | F | SCC/Right Tonsil | T1N1M0 | 7000 (tonsil) | NA | NA |
NA – Not available
Acknowledgments
Funding: This research was funded in part through the NIH/NCI Cancer Center Support Grant P30 CA008748.
References
- 1.Yao M, Dornfeld KJ, Buatti JM, Skwarchuk M, Tan H, Nguyen T, et al. Intensity-modulated radiation treatment for head-and-neck squamous cell carcinoma--the University of Iowa experience. International journal of radiation oncology, biology, physics. 2005;63:410–21. doi: 10.1016/j.ijrobp.2005.02.025. [DOI] [PubMed] [Google Scholar]
- 2.Tsai CJ, Hofstede TM, Sturgis EM, Garden AS, Lindberg ME, Wei Q, et al. Osteoradionecrosis and radiation dose to the mandible in patients with oropharyngeal cancer. International journal of radiation oncology, biology, physics. 2013;85:415–20. doi: 10.1016/j.ijrobp.2012.05.032. [DOI] [PubMed] [Google Scholar]
- 3.Lee N, Xia P, Fischbein NJ, Akazawa P, Akazawa C, Quivey JM. Intensity-modulated radiation therapy for head-and-neck cancer: the UCSF experience focusing on target volume delineation. International journal of radiation oncology, biology, physics. 2003;57:49–60. doi: 10.1016/s0360-3016(03)00405-x. [DOI] [PubMed] [Google Scholar]
- 4.De Felice F, Musio D, Tombolini V. Osteoradionecrosis: an old toxicity in the IMRT era? Oral oncology. 2015;51:e60–1. doi: 10.1016/j.oraloncology.2015.03.002. [DOI] [PubMed] [Google Scholar]
- 5.Marx RE. A new concept in the treatment of osteoradionecrosis. Journal of oral and maxillofacial surgery: official journal of the American Association of Oral and Maxillofacial Surgeons. 1983;41:351–7. doi: 10.1016/s0278-2391(83)80005-6. [DOI] [PubMed] [Google Scholar]
- 6.Fenner M, Park J, Schulz N, Amann K, Grabenbauer GG, Fahrig A, et al. Validation of histologic changes induced by external irradiation in mandibular bone. An experimental animal model. Journal of cranio-maxillo-facial surgery: official publication of the European Association for Cranio-Maxillo-Facial Surgery. 2010;38:47–53. doi: 10.1016/j.jcms.2009.07.011. [DOI] [PubMed] [Google Scholar]
- 7.Zhuang Q, Zhang Z, Fu H, He J, He Y. Does radiation-induced fibrosis have an important role in pathophysiology of the osteoradionecrosis of jaw? Medical hypotheses. 2011;77:63–5. doi: 10.1016/j.mehy.2011.03.024. [DOI] [PubMed] [Google Scholar]
- 8.Gomez DR, Estilo CL, Wolden SL, Zelefsky MJ, Kraus DH, Wong RJ, et al. Correlation of osteoradionecrosis and dental events with dosimetric parameters in intensity-modulated radiation therapy for head-and-neck cancer. International journal of radiation oncology, biology, physics. 2011;81:e207–13. doi: 10.1016/j.ijrobp.2011.02.003. [DOI] [PubMed] [Google Scholar]
- 9.Ben-David MA, Diamante M, Radawski JD, Vineberg KA, Stroup C, Murdoch-Kinch CA, et al. Lack of osteoradionecrosis of the mandible after intensity-modulated radiotherapy for head and neck cancer: likely contributions of both dental care and improved dose distributions. International journal of radiation oncology, biology, physics. 2007;68:396–402. doi: 10.1016/j.ijrobp.2006.11.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Reuther T, Schuster T, Mende U, Kubler A. Osteoradionecrosis of the jaws as a side effect of radiotherapy of head and neck tumour patients--a report of a thirty year retrospective review. International journal of oral and maxillofacial surgery. 2003;32:289–95. doi: 10.1054/ijom.2002.0332. [DOI] [PubMed] [Google Scholar]
- 11.Rankow RM, Weissman B. Osteoradionecrosis of the mandible. The Annals of otology, rhinology, and laryngology. 1971;80:603–11. doi: 10.1177/000348947108000426. [DOI] [PubMed] [Google Scholar]
- 12.Marx RE. Osteoradionecrosis: a new concept of its pathophysiology. Journal of oral and maxillofacial surgery: official journal of the American Association of Oral and Maxillofacial Surgeons. 1983;41:283–8. doi: 10.1016/0278-2391(83)90294-x. [DOI] [PubMed] [Google Scholar]
- 13.Epstein JB, Wong FL, Stevenson-Moore P. Osteoradionecrosis: clinical experience and a proposal for classification. Journal of oral and maxillofacial surgery: official journal of the American Association of Oral and Maxillofacial Surgeons. 1987;45:104–10. doi: 10.1016/0278-2391(87)90399-5. [DOI] [PubMed] [Google Scholar]
- 14.Chen JA, Wang CC, Wong YK, Wang CP, Jiang RS, Lin JC, et al. Osteoradionecrosis of mandible bone in patients with oral cancer-associated factors and treatment outcomes. Head & neck. 2014 doi: 10.1002/hed.23949. [DOI] [PubMed] [Google Scholar]
- 15.Chronopoulos A, Zarra T, Troltzsch M, Mahaini S, Ehrenfeld M, Otto S. Osteoradionecrosis of the mandible: A ten year single-center retrospective study. Journal of cranio-maxillo-facial surgery: official publication of the European Association for Cranio-Maxillo-Facial Surgery. 2015;43:837–46. doi: 10.1016/j.jcms.2015.03.024. [DOI] [PubMed] [Google Scholar]
- 16.van Merkesteyn JP, Balm AJ, Bakker DJ, Borgmeyer-Hoelen AM. Hyperbaric oxygen treatment of osteoradionecrosis of the mandible with repeated pathologic fracture. Report of a case. Oral surgery, oral medicine, and oral pathology. 1994;77:461–4. doi: 10.1016/0030-4220(94)90224-0. [DOI] [PubMed] [Google Scholar]
- 17.Store G, Boysen M. Mandibular osteoradionecrosis: clinical behaviour and diagnostic aspects. Clinical otolaryngology and allied sciences. 2000;25:378–84. doi: 10.1046/j.1365-2273.2000.00367.x. [DOI] [PubMed] [Google Scholar]
- 18.He Y, Liu Z, Tian Z, Dai T, Qiu W, Zhang Z. Retrospective analysis of osteoradionecrosis of the mandible: proposing a novel clinical classification and staging system. International journal of oral and maxillofacial surgery. 2015 doi: 10.1016/j.ijom.2015.04.006. [DOI] [PubMed] [Google Scholar]
- 19.Store G, Larheim TA. Mandibular osteoradionecrosis: a comparison of computed tomography with panoramic radiography. Dento maxillo facial radiology. 1999;28:295–300. doi: 10.1038/sj/dmfr/4600461. [DOI] [PubMed] [Google Scholar]
- 20.Malska WI. Microdensitometric analysis of the influence of X-irradiation on mature bone in humans. Acta Med Pol. 1971;12:357–8. [PubMed] [Google Scholar]
- 21.Chang DT, Sandow PR, Morris CG, Hollander R, Scarborough L, Amdur RJ, et al. Do pre-irradiation dental extractions reduce the risk of osteoradionecrosis of the mandible? Head & neck. 2007;29:528–36. doi: 10.1002/hed.20538. [DOI] [PubMed] [Google Scholar]
- 22.Hansen HJ, Maritim B, Bohle GC, 3rd, Lee NY, Huryn JM, Estilo CL. Dosimetric distribution to the tooth-bearing regions of the mandible following intensity-modulated radiation therapy for base of tongue cancer. Oral surgery, oral medicine, oral pathology and oral radiology. 2012;114:e50–4. doi: 10.1016/j.oooo.2012.01.024. [DOI] [PubMed] [Google Scholar]
- 23.Hinchy NV, Jayaprakash V, Rossitto RA, Anders PL, Korff KC, Canallatos P, et al. Osteonecrosis of the jaw - prevention and treatment strategies for oral health professionals. Oral oncology. 2013;49:878–86. doi: 10.1016/j.oraloncology.2013.06.008. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


