Abstract
Context
Nurses are principal caregivers in the neonatal intensive care unit and support mothers to establish and sustain a supply of human milk for their infants. Whether an infant receives essential nutrition and immunological protection provided in human milk at discharge is an issue of health care quality in this setting.
Objectives
To examine the association of the neonatal intensive care unit work environment, staffing levels, level of nurse education, lactation consultant availability, and nurse-reported breastfeeding support with very low birth weight infant receipt of human milk at discharge.
Design and setting
Cross sectional analysis combining nurse survey data with infant discharge data.
Participants
A national sample of neonatal intensive care units (N = 97), nurses (N = 5614) and very low birth weight infants (N = 6997).
Methods
Sequential multivariate linear regression models were estimated at the unit level between the dependent variable (rate of very low birth weight infants discharged on “any human milk”) and the independent variables (nurse work environment, nurse staffing, nursing staff education and experience, lactation consultant availability, and nurse-reported breastfeeding support).
Results
The majority of very low birth weight infants (52%) were discharged on formula only. Fewer infants (42%) received human milk mixed with fortifier or formula. Only 6% of infants were discharged on exclusive human milk. A 1 SD increase (0.25) in the Practice Environment Scale of the Nursing Work Index composite score was associated with a four percentage point increase in the fraction of infants discharged on human milk (p < 0.05). A 1 SD increase (0.15) in the fraction of nurses with a bachelor’s degree in nursing was associated with a three percentage point increase in the fraction infants discharged on human milk (p < 0.05). The acuity-adjusted staffing ratio was marginally associated with the rate of human milk at discharge (p = .056). A 1 SD increase (7%) in the fraction of infants who received breastfeeding support was associated with an eight percentage point increase in the fraction of infants discharged on human milk (p < 0.001).
Conclusions
Neonatal intensive care units with better work environments, better educated nurses, and more infants who receive breastfeeding support by nurses have higher rates of very low birth weight infants discharged home on human milk. Investments by nurse administrators to improve work environments and support educational preparation of nursing staff may ensure that the most vulnerable infants have the best nutrition at the point of discharge.
Keywords: Intensive care, Neonatal; Very low birth weight; Infant; Human milk; Breast feeding; Nurse work environment; Nurse staffing; Practice Environment Scale of the Nursing; Work Index
1. Introduction
Globally, nurses provide the majority of clinical care to sick infants admitted to the neonatal intensive care unit. Current U.S. perinatal standards call for all very low birth weight infants to receive intensive care (American Academy of Pediatrics and the American College of Obstetricians and Gynecologists, 2012). Common reasons for infant admission to the neonatal intensive care unit at birth include prematurity (birth less than 37 weeks gestation) and very low birth weight (birth less than 1500 g) (American Academy of Pediatrics and the American College of Obstetricians and Gynecologists, 2012). Despite international evidence, policy and legislation of breastfeeding as the highest form of infant nutrition, the U.S. lags behind other industrialized nations in initiating and sustaining breastfeeding among infants during the first year of life (Academy of Breastfeeding Medicine, 2008; Bartick and Reinhold, 2010; Centers for Disease Control and Prevention, 2014; United States Breastfeeding Committee, 2010; World Health Organization, 2015). The constant presence of neonatal intensive care nurses ideally positions them to help mothers overcome challenges related to the establishment of a supply of human milk and breastfeeding. Nursing time invested in helping mothers breastfeed and sustain a milk supply is of paramount importance to very low birth weight infants who receive the greatest nutritional benefits and immunological protection provided in their mother’s milk (Boucher et al., 2011; Hallowell et al., 2014; Ip et al., 2007; Lessen and Crivelli-Kovach, 2007; Nelson, 2007; Spatz, 2004, 2010, 2011; U.S. Department of Health and Human Services, 2011).
More than a decade ago researchers began to explore neonatal intensive care unit infant outcomes (Fanaroff et al., 2007; Horbar et al., 2002). Recently, “exclusive breastfeeding” at discharge was included in set of perinatal nurse-sensitive quality measures used to evaluate priority outcomes in the postpartum setting endorsed by the (U.S.) National Quality Forum (National Quality Forum, 2014). This institutional measure of quality of care determines the hospital-wide breastfeeding rate (National Quality Forum, 2014). However, the hospital-wide measure has not been designed to account for the varied modes of human milk provision used to feed very low birth weight infants discharged from the neonatal intensive care unit (American Academy of Pediatrics, 2012; Ip et al., 2007; Lee et al., 2013; United States Breastfeeding Committee, 2010). This study is the first to provide evidence of the relationship between nursing organizational features (nursing practice environment and nursing care) and a human milk outcome for very low birth weight infants in the neonatal intensive care unit.
Evidence suggests that the nutrient composition of human milk though ideal for full-term infants, is insufficient to meet the protein requirement and nutritional needs essential for adequate growth of premature and often concomitantly very low birth weight infants (Kuschel and Harding, 2004; Schanler, 2007; World Health Organization, 2011). Milk produced by mothers of premature infants is initially nutritionally sufficient at birth, however, a sharp decline in nutrients essential for rapid brain development and growth occurs during the subsequent four weeks of lactation (Schanler, 2007). Hence, fortification of human milk and supplementation of feeding low birth weight infants in addition to breastfeeding is recommended worldwide (World Health Organization, 2011). Fortification of human milk for very low birth weight infants is necessary to achieve adequate protein and mineral intake and improve weight gain particularly after hospital discharge (Academy of Breastfeeding Medicine, 2008; American Academy of Pediatrics, 2012; Bishara et al., 2008; Carver, 2005; Kleinman, 2009; O’Connor et al., 2003; Saarela et al., 2005; Schanler, 2007).
Although breastfeeding is the ideal method of feeding an infant, the reality in most U.S. neonatal intensive care units is that few very low birth weight infants go home exclusively feeding from the breast. Vital processes such as skin-to-skin maternal–infant contact, initiation of breast stimulation and human milk extraction using a hospital-grade breast-pump or manual hand expression, imperative to initiate and sustain a human milk supply are often delayed due to prolonged maternal–infant separation due complications related to birth, infant illness and physical immaturity (Bakewell-Sachs and Blackburn, 2003; Edwards and Spatz, 2010; Lessen and Crivelli-Kovach, 2007; McGrath, 2007; Meier et al., 2007; Spatz, 2004, 2011; Spatz and Lessen, 2011; Wambach and Riordan, 2014). In order to promote discharge of very low birth weight infants with exclusive human milk feedings, mothers are encouraged to breastfeed as well as give infants expressed human milk (pumped or hand expressed) that may be fortified with human milk fortifier and given to infants through a variety of methods (Spatz, 2004; Zukowsky, 2007). To account for this range of feeding regimens “human milk provision” rather than breastfeeding is the term used in this study.
Nurse understaffing has been documented as a major concern in neonatal intensive care units in the U.S. and England (Hamilton et al., 2007; Rogowski et al., 2013). Adequate staffing is crucial to the ability of the nurse to inform, educate and support parents during their infants intensive care admission. Two U.S. studies have identified the associations between better nurse staffing and two human milk related outcomes: higher levels of breastfeeding support by nurses (Hallowell et al., 2014) and a higher likelihood that very low birth weight infants would be discharged on human milk from the neonatal intensive care units, controlling for the concentration of black very low birth weight infants cared for in the unit (Lake et al., 2014). However, studies conducted in the U.S. and Canada have associated better nurse staffing ratios with improved infant outcomes including lower infection rates, less care rationing and higher nurse-reported quality of care in neonatal intensive care units (Cimiotti et al., 2006; Rochefort and Clarke, 2010; Rogowski et al., 2013).
Beyond nurse staffing, organizational features of hospitals such as those evaluated through Magnet® hospital designation (an international hospital credential that recognizes excellence in nursing standards) (American Nurses Credentialing Center, 2015), specifically better nursing practice environments largely explain improved patient outcomes documented in Magnet® hospitals (McHugh et al., 2013). Neonatal intensive care units within Magnet® hospitals have demonstrated lower odds of mortality, nosocomial infection, and intraventricular hemorrhage in very low birth weight infants (Lake et al., 2012). These studies provide evidence that specific features of hospital systems such as excellent nursing standards and better nurse staffing are linked to infant outcomes in neonatal intensive care units.
A national recommendation to improve U.S. breastfeeding rates in maternal–infant settings has been to provide better access to resources such as lactation consultants (U.S. Department of Health and Human Services, 2011). Worldwide recognition of the International Breastfeeding Certified Lactation Consultant (IBCLC) indicates a high level training focused on competent, comprehensive consultation in breastfeeding, and lactation management (Bocar, 1992; International Lactation Consultant Association, 2006; Wambach et al., 2005). Use of the title of international board certified lactation consultant is achieved through certification with International Board of Lactation Consultant Examiners. Globally over 27,450 lactation consultants have been certified in over 101 countries (International Board of Lactation Consultant Examiners, 2015). However, not all lactation consultants are certified. Lay persons or anyone with an interest in breastfeeding from any educational or experiential background may call themselves a “lactation consultant” and the number of non-certified persons who use this title is unknown (International Lactation Consultant Association, 2006; La Leche League, 2007; Wambach et al., 2005). In the U.S. there are few certified lactation consultants relative to live births (3 per 1000 births). The majority work in outpatient settings (Centers for Disease Control and Prevention, 2014; Thurman and Allen, 2008). Improved initiation and duration rates of breastfeeding have been demonstrated in neonatal intensive care units with dedicated lactation consultant services (Castrucci et al., 2007; Gonzalez et al., 2003; Pinelli et al., 2001; Wambach et al., 2005). However, lactation consultants are not routinely available in neonatal intensive care units and it is unclear whether they complement or substitute for nursing care that is provided around the clock (Hallowell et al., 2014).
The purpose of this study was to generate evidence linking characteristics of the neonatal intensive care unit: nursing practice environment, staffing, nursing characteristics (level of education and years of experience), lactation resources, and breastfeeding support by nurses to the receipt of human milk by very low birth weight infants from a large national multi-hospital sample.
2. Methods
2.1. Design and participants
A retrospective, multi-hospital cohort design was used to study nurse survey data collected in March 2008 and very low birth weight infant hospitalization records from the calendar year 2008 from the database maintained by the Vermont Oxford Network, a voluntary neonatal intensive care unit quality improvement collaborative. Nurse survey data were generated in the parent study, “Acuity-adjusted staffing, nurse practice environments, and NICU outcomes” (Principal Investigator: Dr. Eileen Lake), funded by the Robert Wood Johnson Foundation Interdisciplinary Nursing Quality Research Initiative program. Vermont Oxford Network data on human milk at discharge was obtained to achieve the study aims. Secondary analysis was used to investigate the associations between organizational features of the neonatal intensive care unit (nurse practice environment, acuity-adjusted nurse staffing, nurses’ characteristics, lactation consultant availability), breastfeeding support by nurses and provision of human milk to very low birth weight infants at discharge. Secondary analysis was used to examine the variable of nurse-reported breastfeeding support collected in the parent study as well as unit-level rates of infants discharged on human milk, which were not aims of the parent study. The relationships among organization, process and outcome were examined with aggregate measures (i.e., at the neonatal intensive care unit level) because the data did not link specific nurses to specific infants.
The hospital participants comprised 97 of 104 Vermont Oxford Network neonatal intensive care units recruited for the parent study. Neonatal intensive care units were recruited based on neonatal intensive care unit level of care and geographic region to represent the Network. In 2008, the Network contained 578 hospitals, representing approximately 65 percent of neonatal intensive care units and 80 percent of all very low birth weight infants in the United States (Lake et al., 2012). The Network classifies neonatal intensive care units into three levels A (restriction on ventilation, no surgery), B (major surgery), and C (cardiac surgery), that correspond with levels II, III and IV in the American Academy of Pediatrics’ classification (American Academy of Pediatrics and the American College of Obstetricians and Gynecologists, 2012). Of the 97 neonatal intensive care units eligible for inclusion in the current study: three units in one hospital system were excluded due to outcome data not reported by the hospitals separately and four hospitals were excluded due to the absence or low number of inborn infants (i.e. children’s hospitals where all or nearly all infants were outborn).
The infant sample was comprised of all inborn infants (i.e. born in the same hospital as the neonatal intensive care unit to which they have been admitted) eligible for enteral feeding at discharge. Outborn infants (i.e. transferred to neonatal intensive care unit from another hospital) were excluded to avoid introduction of complex infant and family conditions that could influence whether infants were discharged on enteral feeding. Examination of such heterogeneity was beyond the scope of this study. The fraction of the infant sample (i.e. very low birth weight infants hospitalized in the 97 neonatal intensive care units in 2008) likely to have been among the neonatal intensive care unit infants nurses reported caring for in March 2008 is unknown because the Network data do not contain dates of hospitalization. No individually identifiable data were contained in the nurse or patient data.
The nurses (N = 5614) who responded to the nurse survey in the 97 neonatal intensive care units (parent study response rate = 77%) comprise the nurse participants in this study. Registered nurses who worked at least 16 h per week and had been employed at least 3 months were eligible for the survey. Each neonatal intensive care unit had a site coordinator that distributed invitations to complete the one-time web survey to eligible staff nurses identified by the nurse manager. Completion of this internet/web-based nurse survey was voluntary, anonymous and confidential. An average of 58 nurses per neonatal intensive care unit responded to the survey (range 18–159). Nurses answered questions about the neonatal intensive care unit nursing practice environment, details about the last shift worked, including infants assigned and whether breastfeeding support was provided to parents. Nurse managers also provided data for each neonatal intensive care unit about the nursing staff characteristics (level of education and years of experience as a neonatal intensive care unit nurse) and lactation consultant availability.
Hospitalization records of very low birth weight infants (N = 6997) who were “enteral feeding at discharge” from the 97 neonatal intensive care units were included. The Network defines very low birth weight status as weight between 501 g and 1500 g at birth. The variable used to measure “human milk at discharge” was derived from all infants on enteral feedings within 24 h of discharge to home. Institutional Review Board (IRB) approval was obtained from the University of Pennsylvania and the University of Vermont.
2.2. Measures
The independent variables were derived from nurse manager reports or aggregated from staff nurse responses.
2.2.1. Neonatal intensive care unit nurses’ characteristics
Neonatal intensive care unit nurse managers reported nursing staff qualifications and the availability of a lactation consultant. Nurse managers reported the number of nurses with the highest educational degree in nursing (Associate Degree, Diploma, Bachelor of Science degree in Nursing, Master of Science degree in Nursing or higher) and the length of experience (five categories) in their current neonatal intensive care unit position. The percent of nurses with a Bachelors degree and higher, and five years’ experience was calculated for each unit.
2.2.2. Organizational features of the neonatal intensive care unit
The neonatal intensive care unit nursing practice environment was measured using the Practice Environment Scale of the Nurse Work Index, a nationally endorsed Nurse Quality Forum, nursing care performance measure (National Quality Forum, 2014). This 31-item, 4-point likert-type instrument was used to measure the degree to which certain aspects of a professional practice environment were present in each neonatal intensive care unit (Lake, 2002). The survey responses were strongly disagree, disagree, agree, and strongly agree. The Practice Environment Scale of the Nurse Work Index items are categorized into five subscales that measure the following practice environment domains: nurse participation in hospital affairs (9 items); nursing foundations for quality of care (10 items); nurse manager ability, leadership, and support of nurses (5 items); staffing and resource adequacy (4 items); and collegial nurse–physician relations (3 items). A score of 2.5 is the midpoint between agree and disagree, and a score of 3 or greater indicates agreement that the element is present in the job (Lake, 2002). The total composite score of the Practice Environment Scale of the Nurse Work Index was used in regression models; psychometric evaluation has established the reliability and validity of this measure in hospital settings (Aiken et al., 2008; Friese et al., 2008; Kutney-Lee et al., 2009). Cronbach’s alpha was 0.83 for the sample.
Nurse staffing was measured as the acuity-adjusted nurse-to-patient ratio, calculated as the observed-to-expected ratio (based on the acuity mix of the infants). This ratio was determined in the parent study, where the average nurse cared for two infants (mean observed nurse-to-patient ratio = 0.46). Acuity was classified into five categories of lowest to highest (specific terms were “continuing care” to “unstable”) (American Academy of Pediatrics and the American College of Obstetricians and Gynecologists, 2012). Each nurse reported the acuity of each assigned infant using definitions for the categories that were developed during the parent study in collaboration with the National Association of Neonatal Nurses (Rogowski et al., 2015).
Nurse managers reported whether they had a lactation consultant available on day, night, and weekend shifts. Nurse managers were not asked to identify if lactation consultants were internationally board certified.
2.2.3. Nursing care process measure of the neonatal intensive care unit
Breastfeeding support was measured as a fraction in each neonatal intensive care unit (Hallowell et al., 2014). Nurses provided a response to the question “Please indicate which of the following factors or activities required your time in caring for this infant’s family”. Nurses could report up to eight activities including “breastfeeding support.” The numerator was comprised of all infants whose parents were present and whose nurses reported providing breastfeeding support on the last shift worked. The denominator was comprised of all infants assigned to nurse respondents in the neonatal intensive care unit. The term “breastfeeding support” was not defined in the nurse survey and left open to the interpretation of the individual nurse respondent.
2.2.4. Very low birth weight infant feeding of human milk at discharge
The human milk variable was constructed from the variable “enteral feeding at discharge” in the hospitalization record provided to the Network by the neonatal intensive care unit. Enteral feeding refers to the (intestinal) intake of the infant at discharge and includes feedings at the breast, bottle, or feeding tube (oral, nasogastric, and abdominal) (Kleinman, 2009). Nutritional categories within the enteral feeding variable included “Human Milk Only,” “Human Milk in Combination with Either Fortifier or Formula,” or “Formula.” A binary variable was constructed to indicate infants who received “any human milk” at discharge by summing the categories of exclusive human milk feedings (“human milk only”) and mixed feedings (“human milk in combination with either fortifier or formula”) versus those who did not receive human milk. The percent of infants who received human milk at discharge from was calculated for each neonatal intensive care unit. The numerator was the sum of all infants who were reported to have received “any human milk” at discharge and the denominator was all infants eligible for enteral feeding at discharge, from each neonatal intensive care unit. Missing data were very low (less than three percent for any item) as the Network makes a great effort to ensure that the database is accurate and complete; therefore, no adjustments for missing data were necessary.
2.3. Data analysis
Descriptive statistics were used to describe the hospital sample and the explanatory variables (nurse education, nurse experience, nurse staffing, nurse practice environment, nurse-reported breastfeeding support and lactation consultant availability) and the outcome variable (very low birth weight infant discharge on “any human milk”). All variables were aggregated and analysis was conducted at the neonatal intensive care unit level. Correlations were assessed between the independent and outcome variables.
Sequential multivariate linear regression models were estimated to examine associations with the outcome variable. Explanatory variables significantly correlated with discharge on human milk (p < 0.05) were included in regression models. Continuous variables were standardized for ease of interpretation. The statistical significance level in the multivariate analysis was p < 0.05 for a 2-tailed test. Adjusted R-squared values were used to describe the variability explained by each model.
The staffing and resource adequacy subscale of the Practice Environment Scale of the Nurse Work Index was correlated (r = 0.57, p < 0.001) with acuity-adjusted staffing. Rather than omit this subscale, the Practice Environment Scale of the Nurse Work Index composite score including this subscale was included in the models because of the integrity of the composite as a national nursing standard. However, models in which this subscale was excluded from the composite yielded equivalent results.
The percent of nurses with a Bachelor of Science in Nursing or higher degree was not significantly correlated with the outcome variable. However, prior studies have determined the association between nurse education and a number of patient outcomes (Aiken et al., 2003, 2012; McGrath, 2007; Meier et al., 2007; Spatz, 2004). The nurse education variable was included in the regression models based both on research evidence and clinical relevance.
Two regression models were constructed. The first examined the associations among neonatal intensive care unit nurse characteristics and organizational features of the neonatal intensive care unit with very low birth weight infant discharge on human milk. The second model adds the effect of the process measure breastfeeding support based on evidence from prior work that has established the significant association between breastfeeding support and nurse staffing (Hallowell et al., 2014). The statistical package Stata Version 12.0 software was used for all analysis.
3. Results
3.1. Characteristics of neonatal intensive care units, nurses, and patients
Compared to member neonatal intensive care units of the Network in 2008, the sample contained larger neonatal intensive care units (a mean of 41 vs. 34 beds), with an average staff size of 74 registered nurses (Table 1). Three quarters (75%) of the sample neonatal intensive care units provided subspecialty care including major surgery to infants (level III), followed by level IV (24%), and level II (1%). In comparison, Network neonatal intensive care units had more level II (8.5%), fewer level IV (18.3%), and a similar proportion of level III neonatal intensive care units (73.2%).
Table 1.
Sample characteristics.
| Valuea | |
|---|---|
| Neonatal intensive care unit characteristics | |
| AAP classification,b n = 97 | |
| Level II | 1 (1) |
| Level III | 73 (75) |
| Level IV | 23 (24) |
| Number of beds, mean (SD) | 41 (20) |
| Number of staff nurses, mean (SD) | 74.0 (40.4) |
| Annual volume of very low birth weight admissions, mean (SD) |
107 (65) |
| Nurse respondents per neonatal intensive care unit, mean (SD) |
58 (30) |
| Nurse education (proportion of nurses with a BSN degree or higher), mean (SD) |
55 (15) |
| Years of experience (proportion of neonatal intensive care unit nurses with 5 or more years of neonatal intensive care unit nursing experience), mean (SD) |
61 (17) |
| Very low birth weight infant birth characteristics, n = 6997 | |
| Birth weight (g), mean (SD), n = 6997 | 1105 (266) |
| Gestational age, mean (SD), completed weeks, n = 6997 |
28.6 (2.6) |
| 1-min Apgar score, mean (SD), n = 6989 | 5.6 (2.4) |
| Small for gestational age, n = 6997 | 20 |
| Multiple birth, n = 6997 | 29 |
| Congenital malformation, n = 6997 | 3 |
| Vaginal delivery, n = 6997 | 27 |
| Had prenatal care, n = 6985 | 96 |
| Male, n = 6997 | 49 |
| Maternal race, n = 6984 | |
| Race/ethnicity, % | |
| Non-Hispanic white | 49 |
| Non-Hispanic black | 30 |
| Other | 21 |
Values are number (%) unless otherwise indicated. Percentages may not sum to 100 due to missing values.
2012 AAP classification: level I – well newborn nursery, is not included in this dataset; level II – restriction on ventilation, no surgery; level III – major surgery; level IV – cardiac surgery.
A total of 5614 nurses responded to the survey, with an average of 58 nurse respondents in each neonatal intensive care unit. In a typical unit, over half (55%) of the nurses possessed a bachelor’s degree or higher in nursing. On average, two-thirds (61%) of nurses in a unit had worked there for five years or more (Table 1).
Sample infants had an average birth weight of 1105 g and a gestational age of 28.6 weeks (Table 1). A mean of 72 infants (SD = 44, Min = 6, Max = 187) met eligibility criteria in each neonatal intensive care unit. The mean 1-min Apgar score for these infants was 5.6, where 20% were small for their gestational age. A high proportion (96%) of mothers had prenatal care. The racial and ethnic composition of the sample was 49% non-Hispanic white, 30% non-Hispanic black, and 21% other.
3.2. Very low birth weight infant feeding of human milk at discharge
Table 2 presents the average and standard deviation across sample units of the percent of infants with each type of enteral feeding. Typically, more than half of the eligible very low birth weight infants were discharged on formula only (52%); few infants were discharged on exclusive human milk feedings (6%), and 42% of infants were discharged on human milk with human milk fortifier or mixed feeding of human milk and formula. The mean fraction of infants discharged on any human milk was 48%. Some neonatal intensive care units discharged 100% of their infants discharged on any human milk.
Table 2.
Percent of very low birth weight infants by type of enteral feeding at discharge (n = 97).
| Type of enteral feeding | % | Min | Max |
|---|---|---|---|
| Any human milk, mean (SD) | 48 (19) | 6 | 100 |
| Human milk only, mean (SD) | 6(7) | 0 | 33 |
| Human milk + fortifier/formula, mean (SD) |
42 (20) | 6 | 100 |
| Formula only, mean (SD) | 52 (19) | 0 | 94 |
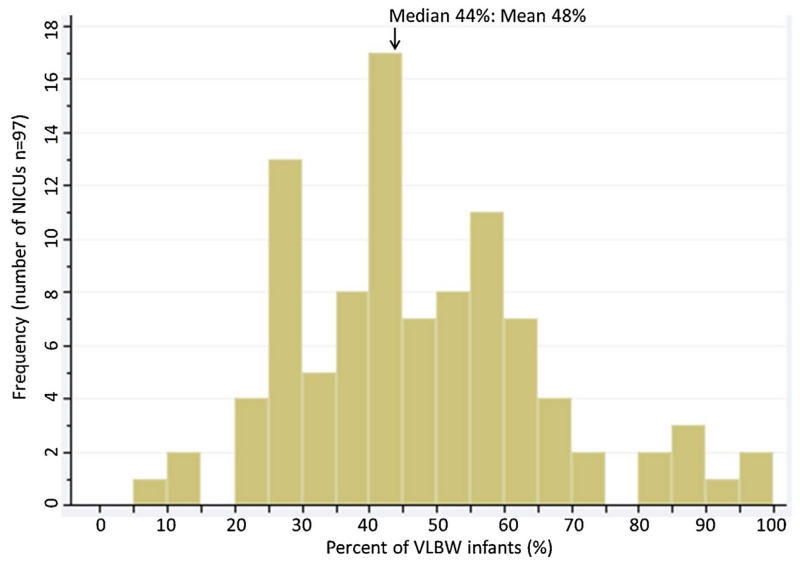
The distribution of the nursing unit percent of very low birth weight infants discharged on any human milk is shown in Fig. 1. The distribution is skewed to the right: most units discharged 25–65% of their infants on any human milk. The largest group of neonatal intensive care units (modal frequency, n = 17) discharged 40–45% of their infants on human milk. Wide variation in the distribution was noted where three units discharged less than 15% of their infants on any human milk and two units discharged 100% of their infants on any human milk.
Fig. 1.
Distribution of very low birth weight infants discharged on any human.
3.3. Neonatal intensive care unit characteristics and correlations with percent of very low birth weight infants discharged to home on any human milk
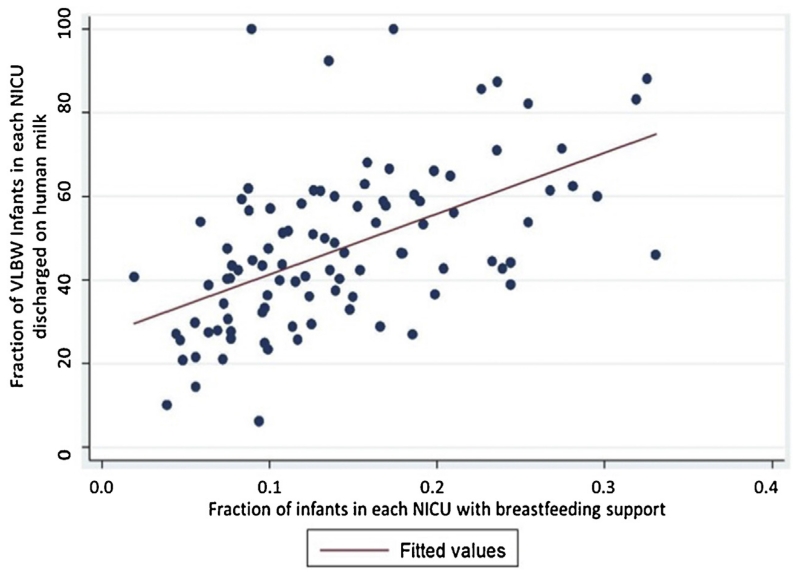
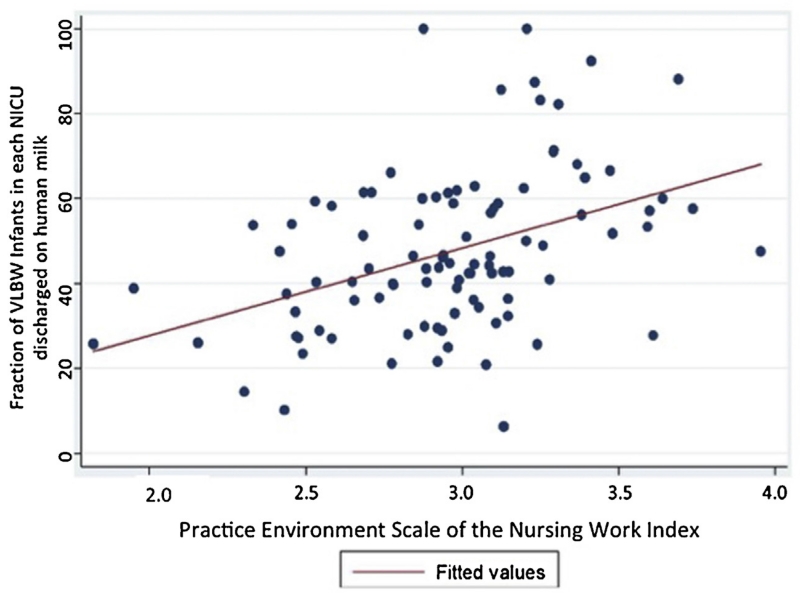
On average, neonatal intensive care unit nurses reported providing breastfeeding support to 14% of infants that they cared for on the last shift they worked (Table 3). The rate of infants discharged on human milk had moderate, positive correlations with breastfeeding support (r = 0.54; p < 0.001), the neonatal intensive care unit nursing practice environment (r = 0.38; p < 0.001), and the acuity-adjusted nurse staffing ratio (r = 0.33; p < 0.001) (Table 3). These correlations are shown by the upward sloping line on each scatterplot (Figs. 2 and 3).
Table 3.
Neonatal intensive care unit characteristics and correlations with percent of very low birth weight infants discharged to home on any human milk (n = 97).
| Min | Max | Pearson’s correlation r (p) |
||
|---|---|---|---|---|
| Practice Environment Scale of the Nurse Work Index Subscales | ||||
| Nurse participation in hospital affairs | 2.95 (0.28) | 2.11 | 3.95 | 0.26* |
| Nursing Foundations for Quality Care | 3.22 (0.20) | 2.72 | 3.97 | 0.25* |
| Nurse manager ability, leadership, and support | 2.92 (0.39) | 1.91 | 3.97 | 0.33** |
| Staffing and resource adequacy | 2.96 (0.38) | 1.82 | 3.96 | 0.42*** |
| Collegial nurse-physician relations | 3.20 (0.32) | 2.01 | 3.97 | 0.20 |
| Practice Environment Scale of the Nurse Work Index composite score | 3.05(0.25) | 2.42 | 3.96 | 0.38*** |
| Acuity-adjusted nurse staffing ratio | 1.00 (0.15) | 0.64 | 1.50 | 0.33*** |
| Nurse qualifications | ||||
| Proportion of neonatal intensive care unit nurses with a baccalaureate or higher degree in nursing, mean (SD) |
.55 (.15) | .23 | .93 | 0.08 |
| Proportion of neonatal intensive care unit nurses with 5 or more years of neonatal intensive care unit nursing experience,a mean (SD) |
.61 (.17) | 0 | .94 | 0.11 |
| Proportion of neonatal intensive care units with lactation consultant available, % | 51 | – | – | 0.20* |
| Proportion of infants with breastfeeding support,b mean (SD) | .14 (.07) | .02 | .33 | 0.54*** |
Nursing experience in the neonatal intensive care unit refers to 5 years or more work experience in the current neonatal intensive care unit.
Nurses reported on infants cared for on the last shift worked.
p < 0.05.
p < 0.01.
p < 0.001.
Fig. 2.
Scatter plot of the relationship between the fractions of very low birth weight infants discharged on human milk and the fraction of infants with process measure nurse-reported breastfeeding support.
Fig. 3.
Scatter plot of the relationship between the fractions of very low birth weight infants discharged on human milk and the organizational feature Practice Environment Scale of the Nursing Work Index.
Lactation consultants were present in 51% of the units, but there was wide variation in their availability; some units had no lactation consultants and some had a lactation consultant on every shift (Table 3). A modest correlation was also noted between the presence of a lactation consultant in a neonatal intensive care unit and infant receipt of human milk at discharge (r = 0.20; p < 0.05) (Table 3).
3.4. Effects of the nursing practice environment, acuity-adjusted nurse staffing and nurse education on infant discharge on human milk
Table 4 describes the results from two regression models, the first model examines the associations between the outcome of the rate of human milk receipt and the explanatory variables: nursing practice environment, acuity-adjusted nurse staffing, nurse education, and lactation consultant presence. The second model adds the variable, breastfeeding support. In the first model, a 1 SD increase (0.25) in the Practice Environment Scale of the Nurse Work Index composite score was associated with a five-percentage point increase in the fraction of very low birth weight infants discharged on human milk (p < 0.01). A 1 SD increase in the acuity-adjusted nurse staffing ratio (an additional 0.15 of a nurse per infant) was associated with a four percentage point increase in the rate of discharge on human milk. The educational composition of nursing staff and the presence of a lactation consultant were not significant.
Table 4.
Associations between fraction of very low birth weight infants discharged to home on any human milk and neonatal intensive care unit nursing characteristics and lactation consultant presence.
| Model 1 |
Model 2 |
|||||||
|---|---|---|---|---|---|---|---|---|
| Adjusted R2 = 0.20 |
Adjusted R2 = 0.37 |
|||||||
| B | SE | 95% CI | p | B | SE | 95% CI | p | |
| Breastfeeding support | 0.08*** | 0.02 | 0.05–0.12 | 0.000 | ||||
| Practice Environment Scale of the Nurse Work Index composite score |
0.05** | 0.02 | 0.12–0.09 | 0.005 | 0.04* | 0.02 | −0.00 to 0.07 | 0.042 |
| Acuity-adjusted nurse staffing ratio | 0.04* | 0.02 | 0.01–0.08 | 0.026 | 0.03 | 0.02 | 0.00–0.07 | 0.056 |
| Bachelor’s degree or higher | 0.03 | 0.02 | −0.00 to 0.07 | 0.074 | 0.03* | 0.02 | −0.00 to 0.06 | 0.039 |
| Lactation consultant presence | 0.06a | 0.04 | −0.01 to 0.13 | 0.096 | 0.04a | 0.03 | −0.03 to 0.10 | 0.261 |
B represents standardized coefficient.
Lactation consultant = availability was a dichotomous variable.
p < 0.05.
p < 0.01.
p < 0.001.
In the second model, the addition of breastfeeding support increased the explained variance from 0.20 to 0.37. A 1 SD increase (7%) in the fraction of infants who received breastfeeding support was associated with an eight-percentage point increase in the fraction of infants discharged on human milk (p < 0.001). In this model, the coefficients for the nursing practice environment and staffing were reduced somewhat and the staffing variable became marginally significant (p = .056). Unlike Model 1, the educational level of nursing staff was significantly related to human milk at discharge (p = 0.039). A 1 SD increase (15%) in the fraction of nurses with a BSN or higher degree in the neonatal intensive care unit was associated with a three-percentage point increase in the fraction of infants discharged on human milk.
4. Discussion
Hospitals that dedicate resources to support the highest proportion of infants discharged feeding human milk provide better quality of care (Davanzo et al., 2009; Lee et al., 2013; National Quality Forum, 2014). This is the first study to use a national sample of neonatal intensive care units to examine how multiple features of unit organization and nursing care relate to nutrition and feeding of very low birth weight infants at the point of hospital discharge. We find that nearly half (48%) of very low birth weight infants receive some human milk when discharged home, yet there are wide variations. At the extremes, two units achieved less than 15% and two units achieved 100% of very low birth weight infants discharged to home with human milk. These wide variations are significantly related to theorized nursing factors, specifically the nursing practice environment, staffing, and level of nurse education. The results from this study fit into the larger body of evidence linking nursing system features to patient outcomes by describing human milk provision at discharge as a suitable outcome that may be used to measure critical features of neonatal health care quality in the U.S. We studied three organizational factors (the nursing practice environment, staffing, and level of nurse education) and one measure of care process (nurse-reported breastfeeding support). We found that a shift of one standard deviation in any of them yielded a moderate, significant increase in the outcome measure (very low birth weight infant discharge on human milk). Neonatal intensive care units with better work environments and staffing, higher levels of education, and higher reported provision of breastfeeding support were associated with a three to eight percentage point increase in very low birth weight infants discharged on human milk (p < 0.001). A sizable improvement could be achieved, given that a one standard deviation increase in the fraction of infants who received breastfeeding support would yield an improvement in the fraction of infants going home on human milk from a median of 44% to 52%.
Administrative investments in nurse staffing and better nurse work environments were associated with greater numbers of very low birth weight infants discharged on human milk. An average neonatal intensive care unit that improved their work environment by one standard deviation could potentially yield an additional four percent of very low birth weight infants being discharged on human milk (i.e., from 48% to 52%). Likewise, if the average neonatal intensive care unit increased their staffing ratio by 0.15 of a nurse per infant, it could potentially yield an additional 3% of very low birth weight infants being discharged on human milk (i.e., from 48% to 51%), acknowledging that this result was marginally significant (p = .056). Neonatal intensive care units that provide nurses with the time, resources, and training to develop nurse-led interventions have been shown to improve breastfeeding and human milk rates at discharge (Callen et al., 2005; Pinelli et al., 2001; Spatz, 2011). Beyond organizational investments, a range of potential hospital and unit-level strategies to achieve improved human milk outcomes in the neonatal intensive care unit include training nurses and other health care providers to become lactation certified, developing peer-to-mother breastfeeding counseling networks and lactation focused discharge instruction and support from nurses (Hallowell et al., 2014; Meier et al., 2013). These strategies involve developing a hospital unit culture that values breastfeeding and the use of human milk as an intervention to improve maternal and infant health.
Several studies have linked hospital nurse staffing and work environments to improved patient outcomes (Shekelle, 2013). This evidence has been reported in North American, European and Asian studies that associate these system level factors with improved adult outcomes (Aiken et al., 2003, 2008, 2014; Cho et al., 2014; Kane et al., 2007; Kutney-Lee et al., 2009; Shekelle et al., 2011). Our study broadens our understanding within the pediatric population. Evidence from the same sample of neonatal intensive care units has shown that poor staffing is associated with higher odds of infection (Rogowski et al., 2013). Differences in hospital staffing and work environment scores have also been associated with disparities in infection and human milk rates in the neonatal intensive care unit (Lake et al., 2014). Poor staffing has also been shown to affect pediatric populations and has been associated with 11–48% higher odds of readmission within 15–30 days discharge in U.S. hospitals (Tubbs-Cooley et al., 2013). Similar findings in nine Canadian neonatal intensive care units significantly associate the nurse practice environment with rationing of parental support and teaching, activities essential to human milk provision and preparation for discharge which may identify a path linking nurse practice environments to provision of human milk to critically ill infants (Rochefort and Clarke, 2010). More globally, neonatal intensive care units in Magnet hospitals (hospitals known for meeting high standards of nursing excellence) have better very low birth weight infant outcomes, (i.e., lower odds of mortality, infection, and severe intraventricular hemorrhage) (Lake et al., 2012).
Hospitals committed to fostering nursing excellence hire nursing staff that possesses a higher level of education (baccalaureate level or higher), these workplace settings have been associated with improved patient outcomes (Aiken et al., 2003, 2008; Kutney-Lee et al., 2013). Creating workplaces where nurses may practice to the highest level of their education and training has been associated with safe, high-quality, patient-centered care (Institute of Medicine, 2010). In the U.S. up to 65% of nurses employed in neonatal intensive care units rated with exceptional work environments were baccalaureate prepared (Schmalenberg and Kramer, 2008). Nurses are critical to providing support to parents whose infants are admitted to the neonatal intensive care unit. The lactation specific instructions provided by nurses been associated with higher initiation and maintenance rates for breastfeeding infants in this clinical setting (Crivelli-Kovach, 2011; Lessen and Crivelli-Kovach, 2007; Miracle et al., 2004).
We found that hospitals with neonatal intensive care units employing a higher fraction of nurses with a baccalaureate degree or higher had a modest, positive, and significant correlation (r = 0.20, p < 0.05) with infant discharge on human milk. The effect of education may be related to better critical thinking and clinical judgment skills associated with BSN preparation. In this sample, the interquartile range in the percent of nurses with a BSN or higher was 49–67% indicating that managers can increase the proportion of nursing staff with bachelor’s degrees. More generally, the Institute of Medicine has recognized the importance of increasing the educational level of the registered nurse workforce in order to improve patient outcomes (Institute of Medicine, 2010). This study results add to the evidence that nurse leaders have three overarching strategies for improving patient outcomes: improving RN staffing, improving the work environment, and moving to a better educated RN workforce, where the combination of all three holds the highest potential for the best outcomes (Aiken et al., 2008).
The reason why the workplace environment and nurses within in the neonatal intensive care unit are so critical to whether very low birth weight infants breastfeed and receive human milk at discharge is because the processes are more complex and time consuming for these infants than those discharged from the postpartum setting (McGrath, 2007). Maternal recovery from birth, infant immaturity and illness contribute to the complex nature of human milk provision in the neonatal intensive care unit and nurses must work in partnership with families to support the initiation and maintenance of the maternal milk supply, a process that involves three types of behaviors: assistance with the use of a hospital-grade breast pump, assumption of basic care, and moral support (Meier et al., 2007; Smith et al., 2006; Spatz, 2004). Breastfeeding support from nurses to helps mothers overcome feelings of uncertainty and helplessness related to prolonged-separation from their infants, and empowers them to participate in fundamental infant care through the provision of human milk (Boucher et al., 2011; Cricco-Lizza, 2009; Nelson, 2007). Instructing mothers to master the techniques necessary to assemble breast pump devices can be challenging, especially for mothers for whom good pumping technique must be sustained for weeks and sometimes months at a time (Callen et al., 2005). Earlier work with the sample has identified improved breastfeeding support provided by staff nurses as significantly associated with both acuity-adjusted staffing levels and nurse practice environments (Hallowell et al., 2014). Nurse leaders may improve breastfeeding support rates on their units by ensuring adequate staffing ratios that allow nurses the time to foster vital relationships with families and develop a culture in the neonatal intensive care unit that values human milk (Hallowell et al., 2014; Spatz, 2014). Improved staffing ratios combined with more supportive work environments may both improve breastfeeding support rates and positively influence whether infants are also discharged on human milk.
Available lactation resources in the neonatal intensive care unit include lactation consultants who augment the work of nurses by assisting mothers with processes related to breastfeeding. In this sample, only half the neonatal intensive care units had a lactation consultant available. The presence of a lactation consultant in the neonatal intensive care unit had a modest correlation with infant discharge on human milk (r = 0.20, p < 0.05). In bivariate analysis, a neonatal intensive care unit with a lactation consultant on any shift was associated with an eight percent increase in very low birth weight infant discharge on human milk (p < 0.05). Our findings are consistent with literature that has described the positive influence of lactation consultants in the unit resulting in increases of breastfeeding initiation during the hospital stay, infant discharge on human milk and sustained breastfeeding after discharge (Castrucci et al., 2007). There is a paucity of literature that specifically addresses the utility and contributions of lactation consultants to human milk provision in the neonatal intensive care unit. However, individual hospital studies have described improve breastfeeding initiation rates by 37–50% with implementation of a lactation consultant program dedicated to the neonatal intensive care unit (Castrucci et al., 2007; Gonzalez et al., 2003). Lactation services have also been associated with a higher proportion of infants who receive human milk (60%) during admission to the unit and a significant increase in the percentage of neonates who receive human milk even after discharge (45–75%) (p < 0.05) (Dweck et al., 2008). Despite the declaration by the U.S. Surgeon General in 2011 to improve access to lactation consultants in all settings caring for women and children, current availability is low, there are only three lactation consultants available for every 1000 infants born in the U.S. (U.S. Department of Health and Human Services, 2011). Our results show that the nurse practice environment and nurse staffing exhibit a stronger association than the presence of lactation consultants with the rate of very low birth weight infants discharged on human milk.
The results from this study may be used toward development of perinatal outcome measures applicable for use in the neonatal intensive care unit regarding infant feeding of human milk at discharge. Measurement of infant feeding status at discharge from the neonatal intensive care unit is useful for assessing quality of care (Davanzo et al., 2009, 2013). Development of a patient-centered measure for human milk would gauge the ability and effectiveness of a hospital to employ the highest nutritional standard of care for infants in all settings. Such a measure would be evidence-based, patient directed and cost-efficient (Bartick and Reinhold, 2010). In the U.S., despite the importance of human milk to infant nutrition, immunological protection, and survival, a human milk metric has not been proposed in the neonatal intensive care unit (Academy of Breastfeeding Medicine, 2008; American Academy of Pediatrics, 2012; U.S. Department of Health and Human Services, 2011; World Health Organization, 2001). A human milk measure would be unique since little evidence exists for risk adjustment. In the U.S., risk adjustment would be limited to infant exposure to specific maternal conditions such as infectious disease (i.e. human immune deficiency virus), cancer treatment or illicit drug use and infant metabolic disease (U.S. Department of Health and Human Services, 2011). These risks are virtually eliminated by the increased availability of pasteurized donor human milk in neonatal intensive care units (American Academy of Pediatrics, 2012; U.S. Department of Health and Human Services, 2011). A human milk measure for the neonatal intensive care unit would fulfill desired characteristics of other quality indicators: usefulness for quality improvement, public reporting, and likelihood of being clearly charted in medical records (Romano, 2007). Existing U.S. perinatal outcome measures do not account for the altered processes and complexity of human milk provision to infants in the neonatal intensive care unit (Lee et al., 2013). A potential solution may be to refine the existing hospital measure to report human milk feedings at the point of discharge from neonatal intensive care unit and distinct from breastfeeding in the postpartum unit. A combined measure of breastfeeding and human milk provision would account both for breastfeeding in the postpartum unit and for the range of feeding modalities used in the neonatal intensive care unit to provide a more accurate depiction of hospital rates of human milk feeding. Further development could incorporate clinically relevant data such as the amount and timing of human milk feedings during the neonatal intensive care admission to support a more robust human milk quality measure (Bigger et al., 2014).
This study has several limitations. The cross-sectional design limits causal inference. The parent study was not designed to study breastfeeding support, which limits the capacity to describe this nursing process measure. The term “breastfeeding support” was not defined in the survey. A clearer definition of breastfeeding support is necessary and may include a range of activities nurses might consider supportive to lactation activities including parent education, demonstration and discussion regarding milk storage, and assessment of infant readiness to feed that would strengthen future research. The process measure of breastfeeding support was unable to capture the total number of infants eligible for breastfeeding. Infant data were limited because details regarding the initiation or duration of human milk feeding and the source of human milk (i.e. donor human milk) were unknown. The study would be enhanced if the training or background of the lactation consultants in the neonatal intensive care unit were known and would be strengthened if board certified lactation consultants were identified. Future work should consider the availability of necessary equipment for breastfeeding support and clinical requirements in the neonatal intensive care unit (i.e. parent overnight rooms, supplies for pumping and storage of human milk, presence of hand washing stations). The data were collected in 2008, since that time there have been changes in neonatal intensive care unit culture related to human milk that may influence both the process outcome reported by nurses and the rates of infant discharge on human milk that currently being experienced in neonatal intensive care units (Spatz, 2014). The sample does not fully represent the Vermont Oxford Network or all U.S. hospitals with a neonatal intensive care unit. Our sample contains a larger proportion of level IV neonatal intensive care units than the overall number in the Vermont Oxford Network consortium. This suggests that our findings generalize best to neonatal intensive care units that serve a more complex case mix of infants (levels III and IV).
Despite the limitations of secondary analysis, evidence from a large dataset of more than 5000 nurses and 6000 infants in a national multi hospital sample provides an unprecedented glimpse of the relationship between nurse-provided breastfeeding support and very low birth weight infant discharge on human milk. The study also found that neonatal intensive care units with better work environments and better-educated nurses were also associated with higher rates of very low birth weight infants discharged home on human milk. These data can be used to provide evidence for development of more comprehensive hospital perinatal outcome measures for all infants born in a hospital. The outcomes of this study demonstrate the importance of hospital staffing to provide the best nutritional care to infants.
Nurses are at the forefront of clinical care in the neonatal intensive care unit. This study provides evidence to support organizational features that provide the best evidence-based nutritional care for very low birth weight infants in the neonatal intensive care unit through the provision of human milk. Hospital administrators and neonatal intensive care unit managers may use these results to evaluate their hiring and staffing procedures to ensure that the best-qualified and trained nurses are employed in the neonatal intensive care unit. This study may also provide impetus for managers to provide opportunity and encourage staff nurses to develop clinical practice guidelines and take advantage of educational opportunities to support families wanting to provide human milk to their infants in the neonatal intensive care unit. The results from this research have contributed evidence toward identifying areas where nurse staffing and educational improvement efforts may be focused in order to achieve goals for providing the highest level of nutrition to the most vulnerable infants through the provision of human milk in neonatal intensive care units across the U.S.
5. Conclusions
Neonatal intensive care units with better nurse staffing and work environments have higher rates of very low birth weight infants discharged home on human milk. This is the first study of a national sample of hospitals to examine how multiple features of neonatal intensive care unit organization and care provision relate to the nutritional status of very low birth weight infants at the point they are discharged to home. A common clinical idiom suggests that patient discharge begins on the day of admission; therefore establishment of a human milk supply must occur from the moment an infant is admitted to the neonatal intensive care unit. The constant presence of nurses in the neonatal intensive care unit positions them to achieve lactation goals determined by the infants medical needs and desires of the mother to provide human milk for her child. Although lactation consultants play an important supportive role in the neonatal intensive care unit they are a limited resource. Neonatal intensive care unit administrators must consider how to provide adequate staffing, improve nurse practice environments, and invest in the educational preparation of their nursing staff in order to ensure that the most vulnerable infants receive the best nutrition in the form of human milk at the point of discharge. In the U.S. nurse staffing has a significant association with infant outcomes related to evidence based nutrition through human milk provision in the neonatal intensive care unit. These findings suggest that global health for the sickest newborns may be improved through better hospital organization and nursing care.
What is already known about the topic?
Human milk has indisputable nutritional and immunological benefits and is considered the optimal form of nutrition for preterm (<37 weeks gestation) and/or very low birth weight (VLBW; <1500 g at birth) infants.
Neonatal intensive care unit (NICU) work environments have been linked to rationing of parental support by nurses.
NICU nurse staffing has been linked to breastfeeding support by nurses. NICU staffing and work environments have not been explored in relation to optimal nutrition in this setting.
What this paper adds.
The majority of VLBW infants (52%) are discharged from the NICU on formula only. Fewer infants (42%) receive human milk mixed with fortifier or formula. Only 6% of VLBW infants are discharged on exclusive human milk.
Better nurse work environments and better educated staff nurses in U.S. NICUs are associated with a higher provision of human milk for VLBW infants.
In NICUs where more infants receive breastfeeding support from nurses, more VLBW infants are receiving human milk at the point of discharge to home.
Acknowledgement
The authors thank Dr. Jeffrey Horbar for his support.
Funding: Research reported in this publication was supported by the National Institute of Nursing Research of the National Institutes of Health under award number T32NR007104 “Advanced Training in Nursing Outcomes Research” (Aiken, PI) – post-doctoral funding.
University of Pennsylvania School of Nursing, Office of Nursing Research, 2012 Student Research Pilot Grant (Hallowell, PI) – pre-doctoral funding.
Robert Wood Johnson Foundation Interdisciplinary Nursing Quality Research Initiative grant “Acuity-Adjusted Staffing, Nurse Practice Environments and NICU Outcomes” (Lake, PI). Parent Study for dataset funding.
The content is solely the responsibility of the author(s) and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Ethical approval: IRB exemption was granted by (1) University of Pennsylvania: Protocol#: 816173, Review Board: IRB#8; and (2) University of Vermont: CHRMS: M07-220.
Conflict of interest: None declared.
References
- Academy of Breastfeeding Medicine Position on Breastfeeding. Breastfeed. Med. 2008;3(4):267–270. doi: 10.1089/bfm.2008.9988. [DOI] [PubMed] [Google Scholar]
- Aiken LH, Cimiotti JP, Sloane DM, Smith HL, Flynn L, Neff DF. Effects of nurse staffing and nurse education on patient deaths in hospitals with different nurse work environments. J. Nurs. Adm. 2012;42(10 Suppl.):S10–S16. doi: 10.1097/01.NNA.0000420390.87789.67. http://dx.doi.org/10.1097/01.NNA.0000420390.87789.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aiken LH, Clarke SP, Cheung RB, Sloane DM, Silber JH. Educational levels of hospital nurses and surgical patient mortality. JAMA. 2003;290(12):1617–1623. doi: 10.1001/jama.290.12.1617. http://dx.doi.org/10.1001/jama.290.12.1617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aiken LH, Clarke SP, Sloane DM, Lake ET, Cheny T. Effects of hospital care environment on patient mortality and nurse outcomes. J. Nurs. Adm. 2008;38(5):223–229. doi: 10.1097/01.NNA.0000312773.42352.d7. http://dx.doi.org/10.1097/01.NNA.0000312773.42352.d7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aiken LH, Sloane DM, Bruyneel L, Van den Heede K, Griffiths P, Busse R, Diomidous M, Kinnunen J, Kózka M, Lesaffre E, McHugh MD, Moreno-Casbas MT, Rafferty AM, Schwendimann R, Scott PA, Tishelman C, van Achterberg T, Sermeus W. Nurse staffing and education and hospital mortality in nine European countries: a retrospective observational study. Lancet. 2014;383(9931):1824–1830. doi: 10.1016/S0140-6736(13)62631-8. http://dx.doi.org/10.1016/s0140-6736(13)62631-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Academy of Pediatrics Policy statement breastfeeding and the use of human milk. Pediatrics. 2012;129(3):e827–e841. doi: 10.1542/peds.2011-3552. http://dx.doi.org/10.1542/peds.2011-3552. [DOI] [PubMed] [Google Scholar]
- American Academy of Pediatrics and the American College of Obstetricians and Gynecologists . Inpatient perinatal care services. In: Lemons LCJA, editor. Guidelines for Perinatal Care. 7th American Academy of Pediatrics and American College of Obstetricians and Gynecologists; Elk Grove Village, IL: 2012. pp. 21–60. [Google Scholar]
- American Nurses Credentialing Center Magnet Model. 2015 Retrieved from: http://www.nursecredentialing.org/Magnet/ProgramOverview/New-Magnet-Model.
- Bakewell-Sachs S, Blackburn S. State of the science: achievements and challenges across the spectrum of care for preterm infants. JOGNN – J. Obstetr. Gynecol. Neonatal Nurs. 2003;32(5):683–695. doi: 10.1177/0884217503257342. [DOI] [PubMed] [Google Scholar]
- Bartick M, Reinhold A. The burden of suboptimal breastfeeding in the United States: a pediatric cost analysis. Pediatrics. 2010;125(5):e1048–e1056. doi: 10.1542/peds.2009-1616. http://dx.doi.org/10.1542/peds.2009-1616. [DOI] [PubMed] [Google Scholar]
- Bigger HR, Fogg LJ, Patel A, Johnson T, Engstrom JL, Meier PP. Quality indicators for human milk use in very low-birthweight infants: are we measuring what we should be measuring? J. Perinatol. 2014;34(4):287–291. doi: 10.1038/jp.2014.5. http://dx.doi.org/10.1038/jp.2014.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bishara R, Dunn MS, Merko SE, Darling P. Nutrient composition of hindmilk produced by mothers of very low birth weight infants born at less than 28 weeks’ gestation. J. Hum. Lact. 2008;24(2):159–167. doi: 10.1177/0890334408316085. http://dx.doi.org/10.1177/0890334408316085. [DOI] [PubMed] [Google Scholar]
- Bocar LC. The lactation consultant: part of the health care team. NAACOG’s Clin. Issues Perinat. Women’s Health Nurs. 1992;3(4):731–737. [PubMed] [Google Scholar]
- Boucher CA, Brazal PM, Graham-Certosini C, Carnaghan-Sherrard K. Mothers’ breastfeeding experiences in the NICU. Neonatal Netw. – J. Neonatal Nurs. 2011;30(1):21–28. doi: 10.1891/0730-0832.30.1.21. [DOI] [PubMed] [Google Scholar]
- Callen J, Pinelli J, Atkinson S, Saigal S. Qualitative analysis of barriers to breastfeeding in very-low birthweight infants in the hospital and postdischarge. Adv. Neonatal Care. 2005;5(2):99–103. doi: 10.1016/j.adnc.2004.12.005. http://dx.doi.org/10.1016/j.adnc.2004.12.005. [DOI] [PubMed] [Google Scholar]
- Carver JD. Nutrition for preterm infants after hospital discharge. Adv. Pediatr. 2005;52:23–47. doi: 10.1016/j.yapd.2005.03.002. [DOI] [PubMed] [Google Scholar]
- Castrucci BC, Hoover KL, Lim S, Maus KC. Availability of lactation counseling services influences breastfeeding among infants admitted to neonatal intensive care units. Am. J. Health Promot. 2007;21(5):410–415. doi: 10.4278/0890-1171-21.5.410. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention Breastfeeding Report Card–United States, 2014. 2014 Retrieved from: http://www.cdc.gov/breastfeeding/pdf/2012BreastfeedingReportCard.pdf.
- Cho E, Sloane DM, Kim EY, Kim S, Choi M, Yoo IY, Lee HS, Aiken LH. Effects of nurse staffing, work environments, and education on patient mortality: an observational study. Int. J. Nurs. Stud. 2014 doi: 10.1016/j.ijnurstu.2014.08.006. http://dx.doi.org/10.1016/j.ijnurstu.2014.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cimiotti JP, Haas J, Saiman L, Larson EL. Impact of staffing on bloodstream infections in the neonatal intensive care unit. Arch. Pediatr. Adolesc. Med. 2006;160(8):832–836. doi: 10.1001/archpedi.160.8.832. http://dx.doi.org/10.1001/archpedi.160.8.832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cricco-Lizza R. Rooting for the breast: breastfeeding promotion in the NICU. MCN – Am. J. Matern. Child Nurs. 2009;34(6):356–364. doi: 10.1097/01.NMC.0000363684.43186.fe. http://dx.doi.org/10.1097/01.NMC.0000363684.43186.fe. [DOI] [PubMed] [Google Scholar]
- Crivelli-Kovach A. An evaluation of hospital breastfeeding policies in the Philadelphia metropolitan area 1994–2009: a comparison with the baby-friendly hospital initiative ten steps. Breastfeed. Med. 2011;6(2):77–84. doi: 10.1089/bfm.2010.0009. http://dx.doi.org/10.1089/bfm.2010.0009. [DOI] [PubMed] [Google Scholar]
- Davanzo R, Monasta L, Ronfani L, Brovedani P, Demarini S, Breastfeeding in Neonatal Intensive Care Unit Study, G. Breastfeeding at NICU discharge: a multicenter Italian study. J. Hum. Lact. 2013;29(3):374–380. doi: 10.1177/0890334412451055. http://dx.doi.org/10.1177/0890334412451055. [DOI] [PubMed] [Google Scholar]
- Davanzo R, Ronfani L, Brovedani P, Demarini S, Breastfeeding in Neonatal Intensive Care Unit Study, G. Breast feeding very-low-birthweight infants at discharge: a multicentre study using WHO definitions. Paediatr. Perinat. Epidemiol. 2009;23(6):591–596. doi: 10.1111/j.1365-3016.2009.01068.x. http://dx.doi.org/10.1111/j.1365-3016.2009.01068.x. [DOI] [PubMed] [Google Scholar]
- Dweck N, Augustine M, Pandya D, Valdes-Greene R, Visintainer P, Brumberg HL. NICU lactation consultant increases percentage of outborn versus inborn babies receiving human milk. J. Perinatol. 2008;28(2):136–140. doi: 10.1038/sj.jp.7211888. http://dx.doi.org/10.1038/sj.jp.7211888. [DOI] [PubMed] [Google Scholar]
- Edwards TE, Spatz DL. An innovative model for achieving breastfeeding success in infants with complex surgical anomalies. J. Perinat. Neonatal Nurs. 2010;24(3):254–255. doi: 10.1097/JPN.0b013e3181e8d517. http://dx.doi.org/10.1097/JPN.0b013e3181f3aa5a. [DOI] [PubMed] [Google Scholar]
- Fanaroff AA, Stoll BJ, Wright LL, Carlo WA, Ehrenkranz RA, Stark AR, Bauer CR, Donovan EF, Korones SB, Laptook AR, Lemons JA, Oh W, Papile LA, Shankaran S, Stevenson DK, Tyson JE, Poole WK, Network NNR. Trends in neonatal morbidity and mortality for very low birthweight infants. Am. J. Obstet. Gynecol. 2007;196(2):147.e1–147.e8. doi: 10.1016/j.ajog.2006.09.014. http://dx.doi.org/10.1016/j.ajog.2006.09.014. [DOI] [PubMed] [Google Scholar]
- Friese CR, Lake ET, Aiken LH, Silber JH, Sochalski J. Hospital nurse practice environments and outcomes for surgical oncology patients. Health Serv. Res. 2008;43(4):1145–1163. doi: 10.1111/j.1475-6773.2007.00825.x. http://dx.doi.org/10.1111/j.1475-6773.2007.00825.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez KA, Meinzen-Derr J, Burke BL, Hibler AJ, Kavinsky B, Hess S, Pickering LK, Morrow AL. Evaluation of a lactation support service in a children’s hospital neonatal intensive care unit. J. Hum. Lact. 2003;19(3):286–292. doi: 10.1177/0890334403255344. http://dx.doi.org/10.1177/0890334403255344. [DOI] [PubMed] [Google Scholar]
- Hallowell SG, Spatz DL, Hanlon AL, Rogowski JA, Lake ET. Characteristics of the NICU work environment associated with breastfeeding support. Adv. Neonatal Care. 2014;14(4):290–300. doi: 10.1097/ANC.0000000000000102. http://dx.doi.org/10.1097/anc.0000000000000102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton KE, Redshaw ME, Tarnow-Mordi W. Nurse staffing in relation to risk-adjusted mortality in neonatal care. Arch. Dis. Child. Fetal Neonatal Ed. 2007;92(2):F99–F103. doi: 10.1136/adc.2006.102988. http://dx.doi.org/10.1136/adc.2006.102988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horbar JD, Badger GJ, Carpenter JH, Fanaroff AA, Kilpatrick S, LaCorte M, Phibbs R, Soll RF, Members of the Vermont Oxford, N. Trends in mortality and morbidity for very low birth weight infants, 1991–1999. Pediatrics. 2002;110(1 Pt 1):143–151. doi: 10.1542/peds.110.1.143. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine The Future of Nursing – Leading Change, Advancing Health, Report Recommendations – October, 2010. 2010 Retrieved from: https://iom.nationalacademies.org/~/media/Files/Report%20Files/2010/The-Future-of-Nursing/Future%20of%20Nursing%202010%20Recommendations.pdf.
- International Board of Lactation Consultant Examiners International Board of Lactation Consultant Examiners. 2015 Retrieved from: http://iblce.org.
- International Lactation Consultant Association About ILCA. 2006 Retrieved from: http://www.ilca.org/i4a/pages/index.cfm?pageid=3281.
- Ip S, Chung M, Raman G, Chew P, Magula N, DeVine D, Trikalinos T, Lau J. Breastfeeding and Maternal and Infant Health Outcomes in Developed Countries (1530–4396) Rockville, MD: 2007. Retrieved from. http://elinks.library.upenn.edu/sfx_local?sid=OVID:medline&id=pmid:17764214. [PMC free article] [PubMed] [Google Scholar]
- Kane RL, Shamliyan T, Mueller C, Duval S, Wilt T. Nursing Staffing and Quality of Patient Care. Rockville, MD: 2007. Retrieved from. http://archive.ahrq.gov/downloads/pub/evidence/pdf/nursestaff/nursestaff.pdf. [PMC free article] [PubMed] [Google Scholar]
- Kleinman RE, American Academy of Pediatrics. Committee on Nutrition . Pediatric Nutrition Handbook. 6th American Academy of Pediatrics; Elk Grove Village, IL: 2009. [Google Scholar]
- Kuschel CA, Harding JE. Multicomponent fortified human milk for promoting growth in preterm infants. Cochrane Database Syst. Rev. 2004;(1):Cd000343. doi: 10.1002/14651858.CD000343.pub2. http://dx.doi.org/10.1002/14651858.CD000343.pub2. [DOI] [PubMed] [Google Scholar]
- Kutney-Lee A, Lake ET, Aiken LH. Development of the hospital nurse surveillance capacity profile. Res. Nurs. Health. 2009;32(32):217–228. doi: 10.1002/nur.20316. http://dx.doi.org/10.1002/nur.20316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kutney-Lee A, Sloane DM, Aiken LH. An increase in the number of nurses with baccalaureate degrees is linked to lower rates of postsurgery mortality. Health Aff. (Millwood) 2013;32(3):579–586. doi: 10.1377/hlthaff.2012.0504. http://dx.doi.org/10.1377/hlthaff.2012.0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- La Leche League The LLL Leader and the IBCLC – A Partnership in Breastfeeding History. 2007 Retrieved from: http://www.llli.org/llleaderweb/lv/lvjunjul00p52.html.
- Lake ET. Development of the practice environment scale of the Nursing Work Index. Res. Nurs. Health. 2002;25(3):176–188. doi: 10.1002/nur.10032. http://dx.doi.org/10.1002/nur.10032. [DOI] [PubMed] [Google Scholar]
- Lake ET, Staiger D, Horbar J, Cheung R, Kenny MJ, Patrick T, Rogowski J. Association between hospital recognition for nursing excellence and outcomes of very low-birth-weight infants. JAMA. 2012;307(16):1709–1716. doi: 10.1001/jama.2012.504. http://dx.doi.org/10.1001/jama.2012.504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lake ET, Staiger D, Horbar J, Kenny MJ, Patrick T, Rogowski JA. Disparities in perinatal quality outcomes for very low birth weight infants in neonatal intensive care. Health Serv. Res. 2014;50(2) doi: 10.1111/1475-6773.12225. http://dx.doi.org/10.1111/1475-6773.12225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee HC, Jegatheesan P, Gould JB, Dudley RA. Hospital-wide breastfeeding rates vs. breastmilk provision for very-low-birth-weight infants. Acta Paediatr. 2013;102(3):268–272. doi: 10.1111/apa.12096. http://dx.doi.org/10.1111/apa.12096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lessen R, Crivelli-Kovach A. Prediction of initiation and duration of breast-feeding for neonates admitted to the neonatal intensive care unit. J. Perinat. Neonatal Nurs. 2007;21(3):256–266. doi: 10.1097/01.JPN.0000285817.51645.73. [DOI] [PubMed] [Google Scholar]
- McGrath JM. Breast-feeding success for the high-risk infant and family: nursing attitudes and beliefs. J. Perinat. Neonatal Nurs. 2007;21(3):183–185. doi: 10.1097/01.JPN.0000285804.39077.fa. Retrieved from:In: http://elinks.library.upenn.edu/sfx_local?sid=OVID:medline&id=pmid:17700091. [DOI] [PubMed] [Google Scholar]
- McHugh MD, Kelly LA, Smith HL, Wu ES, Vanak JM, Aiken LH. Lower mortality in magnet hospitals. Med. Care. 2013;51(5):382–388. doi: 10.1097/MLR.0b013e3182726cc5. http://dx.doi.org/10.1097/MLR.0b013e3182726cc5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meier PP, Engstrom JL, Rossman B. Breastfeeding peer counselors as direct lactation care providers in the neonatal intensive care unit. J. Hum. Lact. 2013;29(3):313–322. doi: 10.1177/0890334413482184. http://dx.doi.org/10.1177/0890334413482184. [DOI] [PubMed] [Google Scholar]
- Meier PP, Furman LM, Degenhardt M. Increased lactation risk for late preterm infants and mothers: evidence and management strategies to protect breastfeeding. J. Midwifery Women’s Health. 2007;52(6):579–587. doi: 10.1016/j.jmwh.2007.08.003. http://dx.doi.org/10.1016/j.jmw.2007.08.003. [DOI] [PubMed] [Google Scholar]
- Miracle DJ, Meier PP, Bennett PA. Mothers’ decisions to change from formula to mothers’ milk for very-low-birth-weight infant. JOGNN – J. Obstetr. Gynecol. Neonatal Nurs. 2004;33:692–703. doi: 10.1177/0884217504270665. http://dx.doi.org/10.1177/0884217504270665. [DOI] [PubMed] [Google Scholar]
- National Quality Forum Practice Environment Scale – Nursing Work Index (PES-NWI) (composite and five subscales) Secondary Practice Environment Scale – Nursing Work Index (PES-NWI) (composite and five subscales) 2014 Retrieved from: http://www.qualityforum.org/QPS/0206.
- Nelson AM. Maternal–newborn nurses’ experiences of inconsistent professional breastfeeding support. J. Adv. Nurs. 2007;60(1):29–38. doi: 10.1111/j.1365-2648.2007.04373.x. http://dx.doi.org/10.1111/j.1365-2648.2007.04373.x. [DOI] [PubMed] [Google Scholar]
- O’Connor DL, Jacobs J, Hall R, Adamkin D, Auestad N, Castillo M, Connor WE, Connor SL, Fitzgerald K, Groh-Wargo S, Hartmann EE, Janowsky J, Lucas A, Margeson D, Mena P, Neuringer M, Ross G, Singer L, Stephenson T, Szabo J, Zemon V. Growth and development of preterm infants fed predominantly human milk, predominantly preterm infant formula, or a combination of human milk and preterm formula. J. Pediatr. Gastroenterol. Nutr. 2003;37(4):437–446. doi: 10.1097/00005176-200310000-00008. [DOI] [PubMed] [Google Scholar]
- Pinelli J, Atkinson SA, Saigal S. Randomized trial of breastfeeding support in very low-birth-weight infants. Arch. Pediatr. Adolesc. Med. 2001;155:548–553. doi: 10.1001/archpedi.155.5.548. http://dx.doi.org/10.1001/archpedi.155.5.548. [DOI] [PubMed] [Google Scholar]
- Rochefort CM, Clarke SP. Nurses’ work environments, care rationing, job outcomes, and quality of care on neonatal unit. J. Adv. Nurs. 2010;66(10):2213–2224. doi: 10.1111/j.1365-2648.2010.05376.x. http://dx.doi.org/10.1111/j.1365-2648.2010.05376.x. [DOI] [PubMed] [Google Scholar]
- Rogowski JA, Staiger D, Patrick T, Horbar J, Kenny M, Lake ET. Nurse staffing and NICU infection rates. JAMA Pediatr. 2013;167(5):444–450. doi: 10.1001/jamapediatrics.2013.18. http://dx.doi.org/10.1001/jamapediatrics.2013.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogowski JA, Staiger DO, Patrick TE, Horbar JD, Kenny MJ, Lake ET. Nurse staffing in neonatal intensive care units in the United States. Res. Nurs. Health. 2015 doi: 10.1002/nur.21674. http://dx.doi.org/10.1002/nur.21674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romano PS. Development & evaluation of the forthcoming AHRQ neonatal quality measures; Session 3C, Overview of the AHRQ Quality Indicators at the AHRQ 2007 Annual Conference; Bethesda, MD. 2007; Retrieved from: http://www.qualityindicators.ahrq.gov/Downloads/Resources/Presentations/2007/ahrq_neonatal_qis_usermeeting2007.pdf. [Google Scholar]
- Saarela T, Kokkonen J, Koivisto M. Macronutrient and energy contents of human milk fractions during the first six months of lactation. Acta Paediatr. 2005;94(9):1176–1181. doi: 10.1111/j.1651-2227.2005.tb02070.x. http://dx.doi.org/10.1080/08035250510036499. [DOI] [PubMed] [Google Scholar]
- Schanler RJ. Evaluation of the evidence to support current recommendations to meet the needs of premature infants: the role of human milk. Am. J. Clin. Nutr. 2007;85(2):625S–628S. doi: 10.1093/ajcn/85.2.625S. Retrieved from:In: http://elinks.library.upenn.edu/sfx_local?sid=OVID:medline&id=pmid:17284767. [DOI] [PubMed] [Google Scholar]
- Schmalenberg C, Kramer M. Clinical units with the healthiest work environments. Crit. Care Nurse. 2008;28(3):65–77. [PubMed] [Google Scholar]
- Shekelle PG. Nurse–patient ratios as a patient safety strategy: a systematic review. Ann. Intern. Med. 2013;158(5 Pt 2):404–409. doi: 10.7326/0003-4819-158-5-201303051-00007. http://dx.doi.org/10.7326/0003-4819-158-5-201303051-00007. [DOI] [PubMed] [Google Scholar]
- Shekelle PG, Pronovost PJ, Wachter RM, Taylor SL, Dy SM, Foy R, Hempel S, McDonald KM, Ovretveit J, Rubenstein LV, Adams AS, Angood PB, Bates DW, Bickman L, Carayon P, Donaldson L, Duan N, Farley DO, Greenhalgh T, Haughom J, Lake ET, Lilford R, Lohr KN, Meyer GS, Miller MR, Neuhauser DV, Ryan G, Saint S, Shojania KG, Shortell SM, Stevens DP, Walshe K. Advancing the science of patient safety. Ann. Intern. Med. 2011;154(10):693–696. doi: 10.7326/0003-4819-154-10-201105170-00011. http://dx.doi.org/10.7326/0003-4819-154-10-201105170-00011. [DOI] [PubMed] [Google Scholar]
- Smith JR, Jamerson PA, Bernaix LW, Schmidt CA, Seiter L. Fathers’ perceptions of supportive behaviors for the provision of breast milk to premature infants. Adv. Neonatal Care. 2006;6(6):341–348. doi: 10.1016/j.adnc.2006.08.005. Retrieved from:In: http://elinks.library.upenn.edu/sfx_local?sid=OVID:medline&id=pmid:17208165. [DOI] [PubMed] [Google Scholar]
- Spatz DL. Ten steps for promoting and protecting breastfeeding for vulnerable infants. J. Perinat. Neonatal Nurs. 2004;18(4):385–396. doi: 10.1097/00005237-200410000-00009. Retrieved from:In: http://journals.lww.com/jpnnjournal/pages/default.aspx. [DOI] [PubMed] [Google Scholar]
- Spatz DL. The critical role of nurses in lactation support. JOGNN – J. Obstetr. Gynecol. Neonatal Nurs. 2010;39(1):499–500. doi: 10.1111/j.1552-6909.2010.01166.x. http://dx.doi.org/10.1111/j.1552-6909.2010.01166.x. [DOI] [PubMed] [Google Scholar]
- Spatz DL. Report of a staff program to promote and support breastfeeding in the care of vulnerable infants at a children’s hospital. J. Perinat. Educ. 2011;14(1):30–38. doi: 10.1624/105812405X23630. http://dx.doi.org/10.1624/105812405X23630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spatz DL. Changing institutional culture to value human milk. Adv. Neonatal Care. 2014;14(4):234–235. doi: 10.1097/ANC.0000000000000128. http://dx.doi.org/10.1097/ANC.0000000000000128. [DOI] [PubMed] [Google Scholar]
- Spatz DL, Lessen R. The risks of not breastfeeding. In: International Lactation Consultants Association, editor. Position Statement. International Lactation Consultant Association; Morrisville, NC: 2011. [Google Scholar]
- Thurman SE, Allen PJ. Integrating lactation consultants into primary health care services: are lactation consultants affecting breastfeeding success? Pediatr. Nurs. 2008;34(5):419–425. [PubMed] [Google Scholar]
- Tubbs-Cooley HL, Cimiotti JP, Silber JH, Sloane DM, Aiken LH. An observational study of nurse staffing ratios and hospital readmission among children admitted for common conditions. BMJ Qual. Saf. 2013;22(9):735–742. doi: 10.1136/bmjqs-2012-001610. http://dx.doi.org/10.1136/bmjqs-2012-001610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- US Department of Health and Human Services . U.S. Department of Health and Human Services. Office of the Surgeon General; Washington, DC: 2011. The Surgeon General’s Call to Action to Support Breastfeeding. Retrieved from:In: http://www.surgeongeneral.gov/library/calls/breastfeeding/calltoactiontosupportbreastfeeding.pdf. [Google Scholar]
- United States Breastfeeding Committee Implementing the Joint Commission Perinatal Care Core Measure on Exclusive Breast Milk Feeding. 2010 Retrieved from: http://www.usbreastfeeding.org/Portals/0/Coalitions/2010-NCSBC/BTT-Handouts/BTT-29-Handout.pdf.
- Wambach K, Campbell SH, Gill SL, Dodgson JE, Abiona TC, Heinig MJ. Clinical lactation practice: 20 years of evidence. J. Hum. Lact. 2005;21(3):245–258. doi: 10.1177/0890334405279001. http://dx.doi.org/10.1177/0890334405279001. [DOI] [PubMed] [Google Scholar]
- Wambach K, Riordan J. Breastfeeding and Human Lactation. 5th Jones & Bartlett Publishers; 2014. [Google Scholar]
- World Health Organization The Optimal Duration of Exclusive Breastfeeding: A Systematic Review. 2001 Retrieved from: http://www.who.int/nutrition/publications/optimal_duration_of_exc_bfeeding_report_eng.pdf.
- World Health Organization . WHO Guidelines Approved by the Guidelines Review Committee Guidelines on Optimal Feeding of Low Birth-Weight Infants in Low- and Middle-Income Countries. World Health Organization; Geneva: 2011. [PubMed] [Google Scholar]
- World Health Organization Breastfeeding. Health Topics. 2015 Retrieved from: http://www.who.int/topics/breastfeeding/en/
- Zukowsky K. Breast-fed low-birth-weight premature neonates: developmental assessment and nutritional intake in the first 6 months of life. J. Perinat. Neonatal Nurs. 2007;21(3):242–249. doi: 10.1097/01.JPN.0000285815.66892.c5. [DOI] [PubMed] [Google Scholar]