Abstract
Introduction:
Amlapitta is very common disease in society. In present era hectic lifestyle, irregular and faulty dietary habits, etc. are the causative factors of Amlapitta. Most of the symptoms of hyper acidity are enumerated in the conditions of Amlapitta delineated in Ayurvedic classics. The local people and Vaidyas of Saurashtra and Kutchh region have been frequently using Jethimala as Yashtimadhu, botanically known as Taverniera nummularia Baker.
Aim:
To evaluate and compare the clinical efficacy of Jethimala (T. nummularia) and Yasthimadhu (Glycyrrhiza glabra Linn.) in Amlapitta.
Materials and Methods:
In this present clinical study, total 40 patients of Amlapitta were registered and randomly divided into two groups. In group A, Yashtimadhu Moola Choorna (G. glabra root powder) and in group B Jethimala Moola Choorna (T. nummularia root powder) was given for 2 weeks with water. A clinical research proforma was specially designed on the basis of classically reported signs and symptoms of Amlapitta for assessing the efficacy of the study drugs.
Results:
Yashtimadhu and Jethimala significantly relieved the cardinal symptoms of Amlapitta like, Tikta-Amlodgara (eryctations with bitter or sour taste) 67.64% in group A and 60% in group B, Hrit-Kanthadaha (burning sensation in the chest and throat) 69% in group A and 66.06% in group B and Utklesha (nausea) 65.35% in group A and 61.70% in group B.
Conclusion:
Statistically significant improvement was observed in all the symptoms in both the groups. While in comparison Jethimala showed better effect than Yashtimadhu (G. glabra) in Aruchi. It is concluded that Jethimala can be used as a substitute for Yashtimadhu.
Keywords: Amlapitta, Glycyrrhiza glabra, hyper acidity, jethimala, taverniera cuneifolia, Taverniera nummularia, yashtimadhu
Introduction
Amlapitta is very common disease caused due to Agnimandhya (digestive impairment) by increased Drava Guna of Vidagdha Pachaka Pitta (liquid quality of burned digestive Pitta) affecting the Annavaha Strotas (channels that carry the ingested food) and characterized by primary symptoms such as Avipaka (indigestion), Klama (exhaustion without any exertion).[1] This is a burning problem in the society because of irregular and improper food habits and stressful lifestyle.
In Charakasamhita, Acharya Charaka has not mentioned Amlapitta as a separate disease, but many scattered references regarding Amlapitta are available. While describing Grahani Chikitsa, Acharya Charaka described the pathogenesis of Amlapitta.[2] Sushruta while describing the diseases caused by excessive use of Lavana (salt); mentioned a disease “Amlika” which is similar to Amlapitta.[3] Kashyapasamhita is the first available text which explained Amlapitta as separate entity.[4] Madhava Nidana described two types of Amlapitta namely, Urdhvaga (upward) and Adhoga (downward).[5] Chakradutta,[6] Bhavaprakasha,[7] Yogaratnakara,[8] etc., also described this disease with treatment. The line of treatment consists of mainly Shodhanakarma (purification). However, in the present day lifestyle, patients cannot provide enough time to carry forward this type of treatment and so we have to choose the most appropriate and effective Shamana (pacifying) therapy. According to Bhavaprakasha, Yasthimadhu is Pittashamaka drug (pacifying Pitta).[9] Due to its Dahashamaka (pacifying burning sensation) and Pittashamaka properties, it can be used effectively in management of Amlapitta. The roots of Taverniera nummularia locally known as Jethimala are sweet in taste and used as a substitute for the licorice (Glycyrrhiza glabra Linn) by the tribes of Gujarat.[10] T. nummularia as a single drug is not evaluated for their effect on the management of Amlapitta. In the present clinical research, an attempt has been made to assess and compare the effect of Jethimala (T. nummularia) and Yashtimadhu (G. glabra) in the management of Amlapitta.
Materials and Methods
In the present study, 40 patients having signs and symptoms of Amlapitta were registered from the OPD of Dravyaguna Department, IPGT and RA Hospital, Gujarat Ayurved University, Jamnagar. The research protocol was approved by Institutional Ethics Committee (No. PGT/7-A/Ethics/2012-13/1964; dt. 21/09/2012) and registered in Clinical Trials Registry of India (CTRI/2013/03/003510; dt.: 25/03/2013). An informed consent from each enrolled patient was obtained before commencement of the treatment.
Inclusion criteria
Patients of 21–60 years age
Presence of Pratyatmaka Lakshanas (cardinal symptoms) of Amlapitta such as Avipaka (indigestion), Klama (exhaustion without any exertion), Utklesha (nausea), Tikta-Amlodgara (erectations with bitter or sour taste), Gaurava (feeling of heaviness of the body), Hrit-Kanthadaha (burning sensation in the chest and throat), and Aruchi (loss of appetite)
Chronicity <1 year
Patients with gastritis, gastric erosion.
Exclusion criteria
Chronicity >1 year
Patients having any systemic disorders such as hypertension, diabetes
Patient with gastrointestinal complications such as peptic ulcer, duodenal ulcer, perforation, stenosis, bleeding, malaena, and malignancy.
Grouping and posology
All the registered 40 patients were divided into two groups (n = 20 each) randomly by coin tossing method. In group A, 2 g of Yasthimadhu Choorna (root powder of G. glabra) and in group B, 2 g of Jethimala Choorna (root powder of T. nummularia) was administered thrice a day for 2 weeks with water.
Investigations
Investigations such as routine blood examination and urine examination were conducted to assess the general health condition of patients.
Criteria for assessment
Assessment was done on the basis of improvement in signs and symptoms of the Amlapitta on the basis of specific scoring pattern.
Scoring adopted for different parameters was as follows:
-
Amlodgara (erectations with bitter or sour taste)
- No Amlodgara at all 0
- Occasionally during day or night for less than half hour after meals 1
- Amlodgara after every intake of meal any food substance for half to 1 2
- h, and relieved by digestion of food or vomiting Amlodgara disturbing the patient, even small amount of fluid regurgitates 3
- to patient's mouth
-
Aruchi (loss of appetite)
- Willing toward all Bhojya Padartha (dietary elements) 0
- Unwilling toward some specific Rasa that is Katu/Amla/Madhura Ahara 1
- (bitter, sour, and sweet taste) Unwilling toward liking foods but could take meal 2
- Totally unwilling for meal 3
-
Avipaka (indigestion)
- No Avipaka 0
- Avipaka occurs daily after each meal takes 4–6 h for Udgara 1
- Shuddhi Lakshanas Daily after each meals/seldom feels hunger but eats the foods only once in 2
- a day and does not have hunger by evening Never gets hungry always heaviness in abdomen followed by Gaurava, Alasya, etc. Lakshanas 3
-
Gaurava (feeling of heaviness of the body)
- Not at all 0
- Occasionally feeling of heaviness 1
- Heaviness remains up to the Jaranakala (4–6 h) only 2
- Heaviness also followed by Jaranakala for >2 h 3
-
Daha (burning sensation in the chest and throat)
- No Daha at all 0
- Daha of mild degree 1
- Daha of moderate degree 2
- Daha of severe degree 3
-
Klama (exhaustion without any exertion)
- No Klama 0
- Lassitude without Shrama daily for sometimes 1
- Lassitude without Shrama daily for long duration 2
- Always feels tired and have no enthusiasms 3
-
Utklesha (nausea)
- No Utklesha at all 0
- Occasionally but not daily 1
- Daily and after taking meal (1–2 h) 2
- Frequently and feels Amlasyata and Amlagandha 3
Assessment of overall effect of therapy
The total effect of therapy was assessed considering overall improvement in sign and symptoms.
Complete remission: 100%
Marked improvement: 76–99%
Improvement: 51–75%
Mild improvement: 26–50%
Unchanged: Below 25%.
Statistical analysis
The Paired t-test was used to assess the effect of therapy in each group and unpaired t-test was applied to compare the effect of therapies in both groups. Statistical calculations were made with the help of Sigmastat 3.5 software (SYSTAT Software, USA). The results were interpreted as; insignificant P > 0.05, significant P < 0.05, significant P < 0.01, highly significant P < 0.001.
Observations
On analysis of Aharajanidana Sevana (intake of dietetic causes), maximum patients (80%) were taking Pittaprkopaka Ahara (Pitta aggravating diet) followed by Atiushnaahara (very hot) (72.50%), Atiguru (eating of very heavy food) (65%), Ajinarjanyaahara (those food causing indigestion) (57.50%), Atiamla (very sour) (55%), Vidahibhojana (those food causing burning sensation) (52.50%), and Viruddhasana (foods which are incompatible combinations) (47.50%). Vegavidharana (suppressions of natural urges) was found in the majority of patients (90%) and Divaswapa (day sleeping after eating) was found in 62.50% of the patients. Krodha (anger), Chinta (anxiety), and Bhaya (fear) were found in 50%, 42.50%, and 15% of the patients, respectively. The majority of the patients were having Hrit-Kanthadaha (92.50%) and Amlodgara (90%). Utklesh and Aruchi were observed in 75% and 70% of patients, respectively.
Results
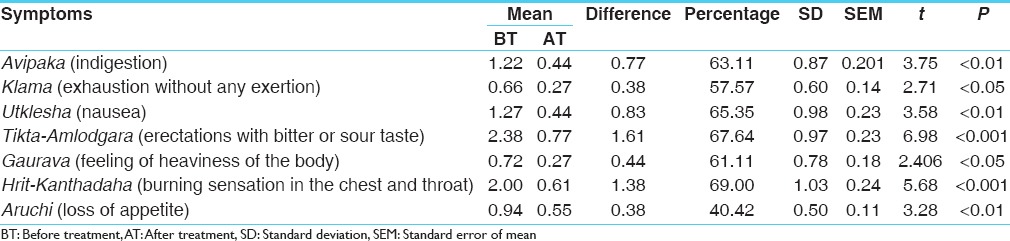
The effectiveness of the treatment is considered positive on the basis of scoring pattern before treatment and after the completion of treatment. Yashtimadhu (G. glabra) group provided a significant improvement in Avipaka 63.11%, Klama 61.11%, Utklesha 65.35%, Tikta-amlodgara 67.64%, Gaurava 61.11%, Hrit-kanthadaha 69.00%, and Aruchi 40.42% [Table 1].
Table 1.
Effect of Glycyrrhiza glabra root powder in group A
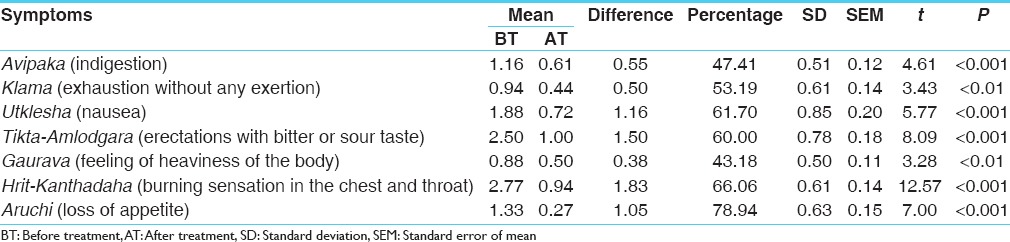
Jethimala (T. nummularia) provided significant relief in Avipaka (47.11%), Klama (53.19%), Utklesha (61.70%), Tikta-Amlodgara (60.00%), Gaurava (43.18%), Hrit-Kanthadaha (66.06%), and Aruchi (78.94%) [Table 2].
Table 2.
Effect of Taverniera nummularia root powder in Group B
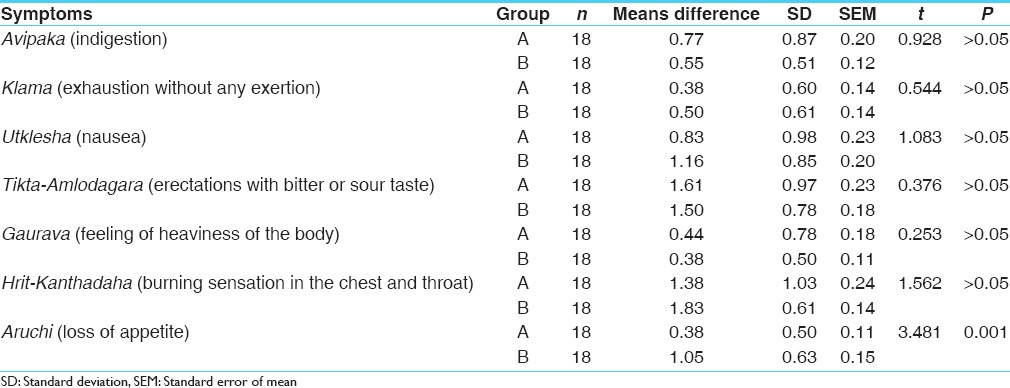
While comparing the effect in between two groups, a statistically significant difference was found only in the symptom-Aruchi; whereas in other symptoms such as Avipaka, Klama, Utklesha, Tikta-Amlodgara, Gaurava and Hrit-Kanthadaha was insignificant [Table 3].
Table 3.
Comparative effect of therapy
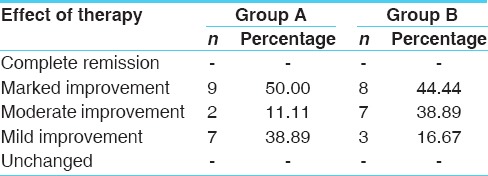
In overall effect of therapies, of 18 patients who completed treatment in group A, 50% of the patients reported marked improvement followed by 38.89% mild improvement and 11.11% were moderate improvement. In group B, total 18 patients completed the treatment of which, maximum that is 44.44% patients reported marked improvement followed by 38.89% mild improvement and 16.67% moderate improvement. Both the treatments have marginal variation on overall effect [Table 4].
Table 4.
Overall effect of therapy
Discussion
On analysis of the Aharajanyanidanas (causative food factors), it was found that maximum patients were having faulty dietary habits, which causes vitiation of Doshas (bodily humor) and impairment of the normal digestive function. 80% of the patients were having the habit of taking Pitta Prakopaka (vitiating Pitta) Ahara which is one of the main causes for Amlapitta. Amla Rasa (sour taste) is Pitta Prakopaka due to its Ushna (hot) property. Acharya Charaka has mentioned Amlapitta in the list of Ati Amla Rasa Sevanjanya Vyadhis (diseases due to excessive intake of sour taste).[11] Vidahi Ahara Sevana is found in 42.5% of the patients, this leads to increase in Ushnata (hotness) and Vidagdhata of Pitta. 90% patients were having Vegavidharana and 62.50% having Divaswapa. Because of Vegavidharana and Divasvapa, even the diet which has been taken in proper quality and quantity does not get digested and leads to Aamdosha. All these things are responsible for the improper digestion of food and vitiation of Doshas. Chinta and Krodha were observed in 42.5% and 50% of the patients respectively. As Acharya Charaka mentioned, Manasikabhavas (mental factor) also play important role in the digestion of food. If a man is under psychological stress such as fear, anxiety, depression, digestion will not be proper even if he takes Pathya Ahara.[12]
In Hrit-Kanthadaha, 69% improvement was found in group A, while 66.06% in group B. The Dosha involved in causing Daha is Pitta. In Amlodgara, 67.64% improvement was found in group A, while 60% in group B. It may be due to Madhura Rasa, Madhura Vipaka and Pitta Shamana property of Yashtimadhu. In Utklesha, 65.35% improvement was found in group A, while 61.70% improvement was found in group B. Yashtimadhu has been stated to be effective in Chhardi (vomiting) and included under Chhardi Nigrahanagana (anti emetics drugs) by Charaka. This property of the drug is validated by the results of the study. Avipaka is the symptom of Agnidusti, 63.11% relief in group A and 47.41% relief in group B. Avipaka may be due to Pittadosha Vriddhi, so in Avipaka Yashtimadhu may counter act the Pitta Dosha by its Madhura Rasa and Sheeta Virya. In Aruchi, 40.42% relief was found in group A while 78.94% relief in group B.
Rasa Nirdharana (identification of taste) of Jethimala (T. nummularia) revealed that the drug has Madhura, Tikta Rasa. According to Acharya Charaka Tikta Rasa is Arochakagna (bitter taste itself nonrelishing destroys disrelish), Deepana (appetiser) and Pachana (digestive).[13] In Aruchi, Jethimala by virtue of its Tikta Rasa and Deepana Pachana Karma (carminative and digestive) showed better result than Yashtimadhu.
T. nummularia is one of the synonyms of T. cuneifolia (Roth.) Arn.[14] Both the drugs T. cuneifolia and G. glabra were found to be similar phytochemically. At least eighteen chromatophores were found similar in both the plants including the sweetening principle, glycyrrhizin.[15] The products of glycyrrhizin may be helpful in the treatment of peptic ulcers; they cause mucus production in the digestive tract and thickening of tissues. They also interfere with prostaglandins and can help in the healing of peptic ulcers. Glycyrrhizin acts in a similar manner to cortisone. It will have slight to moderate anti-inflammatory effects. G. glabra have various pharmacological actions like; ulcer healing, anti-ulcerogenic, choleretic effects, anti-bacterial, antioxidant activity, and memory enhancing activity with good convincing results.[16] T. cuneifolia is also proved for gastro protective and antioxidant activity.[17] By virtue of these activities, both drugs useful in the management of the various symptoms of Amlapitta. In general, these results suggest that, G. glabra and T. nummularia can be used in the management of Amlapitta.
Amlapitta is a Pitta dominant disease in which Agni Vaishamya (Agnimandaya) (improper body fire), Pitta-Prokopa, Rasavaha (channels that carry the nutrient body fluid), Annahava (channels that carry the ingested food) and Purishavaha Srotasa Dushti (vitiation in channels carrying fecal matter) occurs. According to textual references, it is clearly quoted that Pitta-Shamakadravya is generally advised for the management of Amlapitta.
Yashtimadhu is having Madhura Rasa, Guru Guna, Sheeta Virya and Madhura Vipaka, it is Pitta-Vata Shamaka (Pitta-Vata pacifying) and is Dahashamaka, Balya (tonics), Glani (depression of mind), and Kshayahara (relieving wasting disorders).[18] Madhura Rasa and Sheeta Virya of Yashtimadhu acts by decreasing the vitiation of Pitta Dosha. Amlapitta is a Pittaja Vyadhi, where some association of Vata can also be traced. Yashtimadhu is having Pitta-Vatashamaka property, and could work in Samprapti Vighatana (breakdown in the pathogenesis) of Amlapitta. From the organoleptic characters and Rasa Nirdharana of T. nummularia it was observed that the drug possesses Madhura, Tikta Rasa. Both the drugs G. glabra (Yashtimadhu) and T. nummularia (Jethimala) possess Pittashamaka property and helps in the management of Amlapitta.
Conclusion
Yasthimadhu (G. glabra Linn.) and Jethimala (T. nummularia Baker.) are effective in relieving the cardinal symptoms. Significant improvement observed in almost all the symptoms in both the groups but group A (G. glabra) showed better effect than group B and but in Aruchi T. nummularia showed better effect than G. glabra. Therefore, Jethimala can be used as a substitute for Yashtimadhu.
Financial support and sponsorship
IPGT and RA, Gujarat Ayurved University, Jamnagar.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Shastri S, editor. Ch. 51, Ver. 2. Reprint ed. Varanasi: Chaukhambha Prakashan; 2014. Commentator. Madhava Nidana Uttaraadhra of Madhavakara; p. 203. [Google Scholar]
- 2.Acharya JT, editor. Ch. 15, Ver. 47. Reprint ed. Varanasi: Chaukhambha Surabharati Prakashana; 2013. Charaka Samhita of Agnivesha, Chikitsa Sthana; p. 517. [Google Scholar]
- 3.Acharya YT, editor. Ch. 42, Ver. 9 3. Reprint ed. Varanasi: Chaukhambha Orientalia; 2013. Sushruta Samhita of Sushruta, Sutra Sthana; p. 185. [Google Scholar]
- 4.Sharma PH, editor. Ch. 16, Ver. 9 Reprint ed. Varanasi: Chaukhamba Sanskrit Sansthan; 2006. Kashyapa Samhita of Vruddha Jivaka, Khilasthana; p. 336. [Google Scholar]
- 5.Parmar D, editor. Ch.51, Ver. 6, Reprint ed. Ahmedabad: Sarsvati Pustaka Bhandara; 1994. Madhava Nidana Uttaraadhra of Madhavakara; p. 683. [Google Scholar]
- 6.Tripathi I, editor. Varanasi: Chaukhambha Sanskrit Sansthan; 2005. Chakradutta of Chakrapanidutta, Amlapitta Chikitsa, Ver.1-60. Reprint ed; pp. 295–300. [Google Scholar]
- 7.Mishra BS. 11th ed. Varanasi: Chaukhambha Sanskrit Sansthan; 2009. Bhavaprakasha of Bhavamishra (Uttarakhanda), Amlapitta-Sleshma-Pittadhikara, Ver. 1.10; pp. 121–5. [Google Scholar]
- 8.Shastri L, editor. Varanasi: Chaukhamba Sanskrit Sansthan; 2010. Yogaratanakara, Amlapitta Chikitsa, Ver. 1.5. Reprint ed; pp. 239–44. [Google Scholar]
- 9.Shashtri GM, editor. Ch. 6, Ver. 1. Reprint ed. Mumbai: Sastu Sahitya; 1966. Bhavaprakasha (Purvakhanda) of Bhavamishra; pp. 210–11. [Google Scholar]
- 10.Jamdhade VC, Balkhande SV, Surwase BS. Micropropagation of Taverniera cuneifolia (Roth) Arn. A substitute for commercial liquorice. Int J Pharm Bio Sci. 2012;3:204–12. [Google Scholar]
- 11.Acharya JT, editor. Ch. 26, Ver. 422 Reprint ed. Varanasi: Chaukhambha Surabharati Prakashana; 2013. Charaka Samhita of Agnivesha, Sutra Sthana; p. 144. [Google Scholar]
- 12.Acharya JT, editor. Ch. 2, Ver. 9 Reprint ed. Varanasi: Chaukhambha Surabharati Prakashana; 2013. Charaka Samhita of Agnivesha, Vimana Sthana; p. 238. [Google Scholar]
- 13.Acharya JT, editor. Ch. 26, Ver. 425 Reprint ed. Varanasi: Chaukhambha Surabharati Prakashana; 2013. Charaka Samhita of Agnivesha, Sutra Sthana; p. 144. [Google Scholar]
- 14.Khare CP. New York (USA): Springer Science and Business Media; 2007. Glossary of Indian medicinal plants an illustrated dictionary. Reprint Edition; p. 647. [Google Scholar]
- 15.Zore GB, Winston UB, Surwase BS, Meshram NS, Sangle VD, Kulkarni SS, Mohan Karuppayil S. Chemoprofile and bioactivities of Taverniera cuneifolia (Roth) Arn: A wild relative and possible substitute of Glycyrrhiza glabra Linn. Phytomedicine. 2008;15:292–300. doi: 10.1016/j.phymed.2007.01.006. [DOI] [PubMed] [Google Scholar]
- 16.Prajapati SM, Patel BR. Phyto pharmacological perspective of Yashtimadhu (Glycyrrhiza glabra Linn) – A review. Int J Pharm Biol Arch. 2013;4:833–41. [Google Scholar]
- 17.Jamdhade VC, Tembhurne SV, Kamble S. Gastroprotective and Antioxidant potential of methanol root extract of Taverniera cuneifolia (Roth.) Arn. in albino wister rat. J Biologically Active Prod Nat. 2015;5:150–62. [Google Scholar]
- 18.Mishra BS, editor. 7th ed. Varanasi: Chaukhambha Sanskrita Bhavan; 2012. Bhavaprakash Nighantu (Purvardha) of Bhavamishra, Haritakyadi Varga 1, Ver. 145; p. 65. [Google Scholar]


