Abstract
The aim of this study was to conduct a literature review on the potential benefits with the use of Morse taper dental implant connections associated with small diameter platform switching abutments. A Medline bibliographical search (from 1961 to 2014) was carried out. The following search items were explored: “Bone loss and platform switching,” “bone loss and implant-abutment joint,” “bone resorption and platform switching,” “bone resorption and implant-abutment joint,” “Morse taper and platform switching.” “Morse taper and implant-abutment joint,” Morse taper and bone resorption,” “crestal bone remodeling and implant-abutment joint,” “crestal bone remodeling and platform switching.” The selection criteria used for the article were: meta-analysis; randomized controlled trials; prospective cohort studies; as well as reviews written in English, Portuguese, or Spanish languages. Within the 287 studies identified, 81 relevant and recent studies were selected. Results indicated a reduced occurrence of peri-implantitis and bone loss at the abutment/implant level associated with Morse taper implants and a reduced-diameter platform switching abutment. Extrapolation of data from previous studies indicates that Morse taper connections associated with platform switching have shown less inflammation and possible bone loss with the peri-implant soft tissues. However, more long-term studies are needed to confirm these trends.
Keywords: Bone loss, crestal bone remodeling, implant-abutment connection, Morse taper, platform switch, platform switching
INTRODUCTION
Dental implants have achieved long-term success due to the osseointegration of highly biocompatible titanium integrating to the surrounding bone.[1,2] Following the establishment of osseointegration, the implant system depends on the mechanical and chemical stability of the contacting metal joints, which must sustain proper torque originated from the friction between contacting surfaces. Through the development of novel techniques on surface treatment, as well as enhanced implant design, modern implants have improved the prognosis of the long-term osseointegration and performance of dental implants.[1,2,3,4,5,6]
In regards to implant dentistry, criteria for a sustainable, healthy soft tissue outline is a prosthesis that provides mechanical strength and remains esthetically pleasing.[6,7,8] This aesthetic outcome with dental implants is similar to conventional dental prosthetic restorations. However, many edentulous spaces have esthetic and mechanical limitations linked to poor bone quality and the anatomical remodeling of the remaining hard and soft tissues. Due to limitations in bone augmentation procedures and implant screw-retained prostheses associated with dental implants, often the ideal esthetic position is not a viable option.[6,7,8,9]
Regarding studies supporting long-term success rates of implants, the main concern is surprisingly not related to osseointegration. Rather, the focus is on the maintenance of hard and soft tissues over the lifetime of the dental implant system. Considering soft tissue maintenance and implants, the presence or absence of gingival papillae is one of the main concerns. The loss of the interproximal gingival papillae may lead to food accumulation, esthetic deficiencies and phonetic problems.[8,9,10]
Regarding implant dentistry, the soft and hard tissue biological dimensions are initially recorded based upon the timing of the initial load. This difference in record keeping is observed on comparing two-stage dental implant cases when biological dimensions are defined after the initial submerged healing period, versus nonsubmerged/single-stage dental implants, where measurements are recorded at the time of implant placement.[8,9,10,11]
Considering the novelty in technology on dental implant joints, Jokstad et al. noted the development of internal connections showing improved results regarding esthetic outcomes and mechanical stability.[12] Currently, common examples of internal implant-abutment connection designs are the internal hexagonal and the Morse taper connection. A unique design feature of the Morse taper implant-abutment connection is an internal joint design between two conical structures [Figure 1]. This connection was developed by Stephen A. Morse, in 1864, and since has been globally used to connect drilling machines to a removable rotating drill piece. In implant dentistry, a conical “male” abutment is tightened into a “female” conical implant design. This internally tapered design creates significant friction via the high propensity of parallelism between the two structures within the joint space. The Morse taper angle is determined according to the mechanical properties of each material. For instance, titanium-based structures have an ideal relationship between contacting surface angles and coefficient of friction.[12,13]
Figure 1.
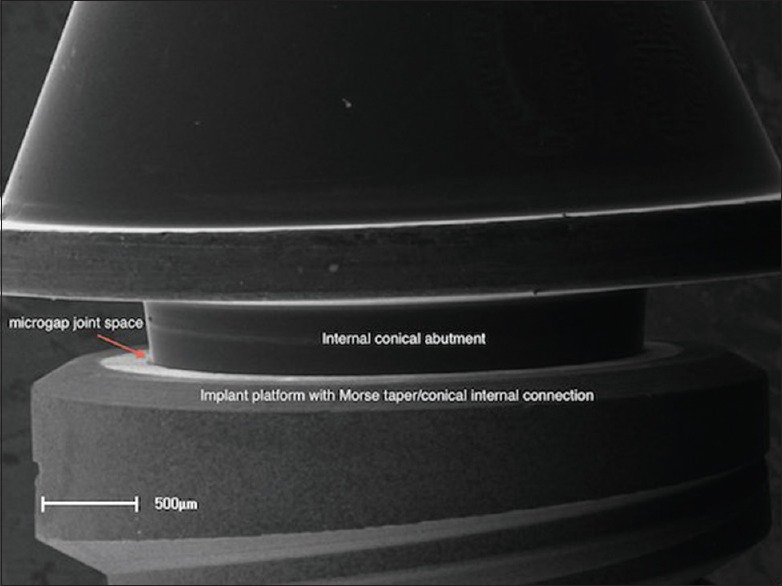
Scanning electron microscopy of Morse taper implant-abutment conical connection design without platform switching
The internal Morse taper implant-abutment design aligns the microgap sizes to be further separated from the marginal bone. In addition, this internally stable design allows for a narrower abutment platform abutment design that can be additionally combined with platform switching [Figure 2]. The platform switching abutment design has shown clinically to reduce marginal bone loss and provide additional space for soft tissue development and maintenance over longer follow-up studies.[14,15,16,17,18,19,20,21,22,23,24]
Figure 2.
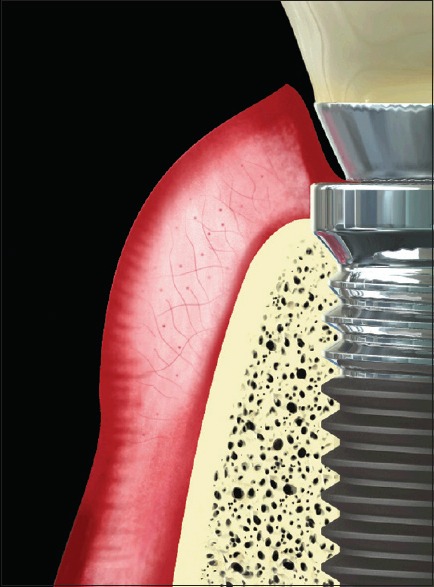
Schematics of a platform switching system and surrounding hard and soft tissue profile
Thus, the main purpose of this study was to review current evidence on the benefits of Morse taper dental implant joints associated with platform switching. It was hypothesized that Morse taper connections involving platform switching would increase the maintenance of peri-implant bone and soft tissues. Thus, likely maintaining the soft tissue profile, reducing the incidence of bone-loss, and ultimately the onset and rate of marginal peri-implantitis associated with the implant-abutment platform.
MATERIALS AND METHODS
A Medline bibliographical search (from 1961 to 2014) was carried out. The following search items were explored: “Bone loss and platform switching,” “bone loss and implant-abutment joint,” “bone resorption and platform switching,” “bone resorption and implant-abutment joint,” “Morse taper and platform switching,” “Morse taper and implant-abutment joint,” “Morse taper and bone resorption,” “crestal bone remodeling and implant-abutment joint,” “crestal bone remodeling and platform switching.”
The eligibility inclusion criteria used for article search were: Meta-analysis; randomized controlled trials; prospective cohort studies; as well as articles and reviews written in English, Portuguese or Spanish languages. The literature selection accepted the following tests: Microbiological assays; physical and mechanical characterization; biomechanics by analytical finite element tests or photoelastic spectrometry; and clinical trials performed in animals or humans under radiographic evaluation.
RESULTS
On the 287 studies identified, 81 relevant and recent studies were selected. The reviewed studies noted a significant clinical outcome with Morse taper implants associated with smaller diameter platform switching abutments. However, some parameters of the scientific inquiry tested may not have direct relevance to the clinical application and long-term treatment outcomes found in implant dentistry.
Within the scientific review, the noted benefits on Morse taper implants and platform switching abutment are listed as follows:
Morse taper design showed a marked decrease in the microgap size found within the abutment-implant joint, thus reducing biofilm accumulation;[14,15,16,17,18,19,20,21,22,23,24,25,26,27,28]
Morse taper implants revealed less peri-implantitis when placed supra-crestally;[2,21,24,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53]
Reduced resorption of crestal bone;[2,30,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59]
The biological width formation takes place apical and laterally around the abutment and the implant's horizontal platform;[8,9,11,30,37,40,41,42,44,54,55,56,57,58,59,60,61,62,63,64,65,66,67]
The smaller abutment diameter in proportion to the implant diameter, naturally augments for increased thickness of the connective soft tissue around the abutment;[40,41,42,56,57]
Torque stability and maintenance of the loaded contacting surface is high due to the biconical Morse system established between the implant and the intermediate screw,;[2,13,68,69,70,71,72,73,74,75,76,77,78,79,80]
The Morse tapered machined connection design was associated with decreased micro-movements during distribution of occlusal forces on the implant;[16,68,69,70,72,73,74,76,79,81]
Morse taper implant-abutment design eliminates the need for additional screw retained connections associated with other implant-abutment designs.[79,82,83,84]
One should accentuate the fact in all the mentioned studies, the distances between implants, of 1, 2 or 3 mm did not show statistically significant differences concerning the bone behavior.[28,52,53,54] Such results support the assumptions the researchers believe to be responsible for the bone behavior around Morse taper implants and abutments incorporating a “platform switch” model.
DISCUSSION
Since clinical dentistry is multifactorial, the results gathered in this study showed a broad range of topics and relevance to the essence of the current article topic. From the articles reviewed, the most common noted concepts throughout the articles relating Morse taper implants and platform switching were marginal bone loss, maintenance of soft tissue anatomical dimensions, implant-abutment microgaps, and aesthetics.
Peri-implant management
The biological periodontal morphology and anatomy around the tooth is frequently mentioned in the literature. In 1961, Gargiulo, Wents, and Orban, reported the mean length values of the gingival sulcus to gingival crest at approximately 0.69 mm, junctional epithelium at 0.97 mm and the connective tissue area at 1.04 mm.[60] Subsequently, Vacek et al., carried out an in vivo study confirming the accuracy of the periodontal dimensions surrounding natural dentition with similar mean values of connective tissue (0.77 mm) and the junction epithelium (1.14 mm).[61] Berglundh et al. compared the gingival composition on natural teeth and the contacting mucosa with dental implants. Both tissues showed similar microscopic features such as: A continuous keratinized epithelium linked to the junctional epithelium that comprised a length of 2 mm; the epithelium was separated from the alveolar bone by a connective tissue zone >1 mm.[62,63]
Cochran et al., evaluated the influence of loading on the presence of biological widths surrounding nonsubmerged implants and concluded that the dimensions and relationships of mucous membrane/implant are similar to the dento-gingival tissues.[65] On the tissues, the measurements were similar both on loading as well as the absence of mechanical conditions. These tissue arrangements naturally imply hard tissue remodeling around the implant. After second-stage implant exposure and abutment placement, an implant-abutment connection creates the possibility of a bone resorption occurrence of approximately 1.5–2 mm in the apical direction.[65]
Aside from tissue organization, a biological reason might exist for this phenomenon: If chronic irritants, like bacteria, reach the implant connection area, or if the connections are removed after the initial healing, bone may resorb, creating a gap, and exposing the affected area.[21,22,23,24]
Other additional factors have shown to affect bone loss as well, such as: Surgical trauma, occlusal overload, peri-implantitis, micro-movements, the biological width, and implant anatomy on the crestal region.[29,30,31,32,33,45,46,47,68,69,70,74,75,76,77,78] Tarnow et al. previously reported, through the histological result, similar bone response on sub gingival dental preparations of prosthetic crowns, which disrupted the attachment apparatus on natural teeth.[54,67]
This bone loss, occurring around the implants may interfere with the aesthetic results after accomplishment of the restorative treatment, since the bone crest height may influence the presence or absence of the interdental papilla. The vertical distance between the base of the interproximal contact point of the natural dentition to the bone crest is an important factor on bone preservation and consequently, on the presence of a sufficient interdental papilla.[9,30,54,55,56,57,63] When interdental sites were assessed, it was verified that when the distance occurred around 5.0 mm or less, the interdental papilla was present in 98% of the cases. However, there was a papilla present in 56% of the cases at interdental papilla at 6.0 mm and in 27% at 7.0 mm or more.[54,67]
In a study by Tarnow et al., radiographs were evaluated from 36 patients, which presented two adjacent implants. The lateral bone loss was measured from the bone crest to the implant surface.[54] This data were subdivided into two groups, based on the distance between the implants. The results showed that less crestal bone loss around implants with a distance equal or >3 mm, than around implants with an inter-implant distance <3 mm. The data revealed that besides the vertical components usually studied, there is an influence relating lateral proximity of adjacent implants on the bone loss of the adjacent implant. The increase in the bone crest loss results in an increase of the distance between the contact point from adjacent crowns and the bone crest. This observation can affect the clinical outcome on whether or not significant interdental papilla is present between two neighboring implants. Another study was done to assess the influence of both vertical and horizontal distances concerning the incidence of the interproximal papillae between adjacent implants and between tooth and implant. The authors concluded that when the distance between implants was < 3 mm, there was an absence of a papilla, regardless of the vertical distance. It was, then, described that the proper distance between implants or between tooth/implant varies from 3 to 4 mm.[54,67]
Platform switching
Within the last decade, maintaining the periodontium soft tissue surrounding the dental implant via smaller abutment diameter on platform switching has gradually gained recognition beyond a novel paradigm. Considering geometry of the dental implant system, the concept of a smaller abutment diameter to maintain and enhance the peri-implant soft tissues has continued to show evidence of clinical success.
Atieh et al. (2010) conducted a systematic review on the clinical relevance of platform switching and preservation of peri-implant crest bone levels.[51] Ten clinical studies reported a statistically significant influence of the platform switching on the maintenance of marginal bone levels. Annibali et al. (2012) conducted a similar systematic review on platform switching versus conventionally restored implants or peri-implant marginal bone loss.[52] Ten randomized controlled trials were selected for review dated from 2007 to 2011. Six of the ten clinical studies noted a significant difference of reduced marginal bone loss around platform switching implant-abutment group versus a traditional design. Subgroup analyses show less marginal bone loss as the platform switching mismatch increased. Subsequently, the inward shifting of the implant-abutment joint interface likely reduced microbial leakage and micromovements that have been additionally associated with marginal bone loss.
Microgap and Morse taper connections
Noted at the implant-abutment joint, inflammatory agents and their chemotactic stimulus of neutrophils and other inflammatory cells infiltrate the surrounding localized tissues promoting long-term osteoclastic bone loss within the alveolar bone.[11]
Previous studies conducted in vitro tests using different sized species of bacteria to evaluate inside-outside migration into different type of implant-abutment connections (screwed implant-abutment, cemented implant-abutment and internal conical connections). The internal connection area of different types of implants was inoculated with bacteria suspensions. Following manufacturer's instructions for torque values, abutments were connected to implants either through screw or cementation and submerged in a sterile nutrient solution test for different times. The screw retained implant abutment showed a high frequency of microbial penetration versus the cement and conical connection. The lower penetration of microbial cells into Morse taper connections occur due to a higher contacting area between biconical abutment and implant connection surfaces.[17,18,19,20,21,22]
Bone remodeling and implants
The bone crest around the implant fixture may act as lever fulcrum point when a flexural force is applied.[39] Concerning overloads, photo-spectrometric and finite element analysis has been used to evaluate the stress distribution around implants and the surrounding bone.[9,16,59,68,69,70]
The bone's mechanical integrity is the result from its remodeling.[31,36,38,43,53] Osteocytes play an important role on bone remodeling by influence of chemical mediators that are released within the interstitial fluid under external loads.[2,41,53] Osteoblasts are recruited while osteoclasts are inhibited. In comparison with cortical bone, a higher rate of osteocytes has been associated with cancellous bone.[2,41,53] That suggests a more favorable peri-implant bone-remodeling prognosis to stabilizing mechanical stimuli and external injuries.[7,38,40,44,46,50,52] An additional advantage in sustaining bone levels is optimizing and facilitating the maintenance of the soft tissues surrounding the implant, especially those which surround the cervical third of the dental implant.[11,22,34,37,40,41,44,62]
The bone tissue around the implants continues a natural process of remodeling during the timing of implant placement and the accomplishment of the prosthetic treatment.[7,43] Observations on bone remodeling may be associated with occlusal force stimulation and the distance between adjacent implants.[7,43,45,65] Additionally, the magnitude and the direction of occlusal force can be altered based upon the presence of prosthetic connections and the occlusal load.[7,65,70]
CONCLUSIONS
A majority of the scientific literature noted in the article analyzed studies using in vitro, and animal-based in vivo assays. Many of the studies analyzed in this article lacked long-term patient clinical testing and follow-up data. These specific limitations found in vitro testing and animal-based studies likely do not mimic all of the oral and systemic factors associated with the human oral environment. The current longitudinal clinical studies do not provide significant long-term evidence of the benefits of Morse taper implants that has been highlighted with in vitro laboratory studies.
Despite these limitations, the Morse taper implant system with platform switching provides a more effective relationship between the implant and intermediary abutment for prolonged healing and health within the surrounding hard and soft tissues. The relevant studies reviewed noted that of the implant-abutment systems currently on the market, the Morse taper system with the use of a smaller abutment diameter has the following advantages: Preserves more of the peri-implant bone, stabilizes more of the soft tissues, reduces the microgap size found in the abutment-implant connection, and proper geometry for narrower mesio-distal edentulous spaces.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Brånemark PI, Hansson BO, Adell R, Breine U, Lindström J, Hallén O, et al. Osseointegrated implants in the treatment of the edentulous jaw. Experience from a 10-year period. Scand J Plast Reconstr Surg Suppl. 1977;16:1–132. [PubMed] [Google Scholar]
- 2.Albrektsson T, Donos N, Working Group 1. Implant survival and complications. The third EAO consensus conference 2012. Clin Oral Implants Res. 2012;23(Suppl 6):63–5. doi: 10.1111/j.1600-0501.2012.02557.x. [DOI] [PubMed] [Google Scholar]
- 3.De Deus G, Camanho D, Mendes MC, Costa E, Souto C, Saliba FM. Evaluation of the degree of success Neodent implants, Implantology courses of UNESA/Rio de Janeiro- A retrospective study. Rev Implant News. 2007;4:617–20. [Google Scholar]
- 4.Jendressen MD, Allen EP, Bayne SC, Donovan TE, Hansson TL, Klooster J, Preston JD. Annual review of selected dental literature: Report of the Committee on Scientific Investigation of the American Academy of Restorative Dentistry. J Prosthet Dent. 1995;74:60–83. doi: 10.1016/s0022-3913(05)80231-8. [DOI] [PubMed] [Google Scholar]
- 5.van Steenberghe D, Lekholm U, Bolender C, Folmer T, Henry P, Herrmann I, et al. Applicability of osseointegrated oral implants in the rehabilitation of partial edentulism: A prospective multicenter study on 558 fixtures. Int J Oral Maxillofac Implants. 1990;5:272–81. [PubMed] [Google Scholar]
- 6.Zarb GA, Schmitt A. The longitudinal clinical effectiveness of osseointegrated dental implants in posterior partially edentulous patients. Int J Prosthodont. 1993;6:189–96. [PubMed] [Google Scholar]
- 7.Barros RR, Novaes AB, Jr, Muglia VA, Iezzi G, Piattelli A. Influence of interimplant distances and placement depth on peri-implant bone remodeling of adjacent and immediately loaded Morse cone connection implants: A histomorphometric study in dogs. Clin Oral Implants Res. 2010;21:371–8. doi: 10.1111/j.1600-0501.2009.01860.x. [DOI] [PubMed] [Google Scholar]
- 8.Choquet V, Hermans M, Adriaenssens P, Daelemans P, Tarnow DP, Malevez C. Clinical and radiographic evaluation of the papilla level adjacent to single-tooth dental implants. A retrospective study in the maxillary anterior region. J Periodontol. 2001;72:1364–71. doi: 10.1902/jop.2001.72.10.1364. [DOI] [PubMed] [Google Scholar]
- 9.Azzi R, Etienne D, Takei H, Fenech P. Surgical thickening of the existing gingiva and reconstruction of interdental papillae around implant-supported restorations. Int J Periodontics Restorative Dent. 2002;22:71–7. [PubMed] [Google Scholar]
- 10.Tarnow DP, Cho SC, Wallace SS. The effect of inter-implant distance on the height of inter-implant bone crest. J Periodontol. 2000;71:546–9. doi: 10.1902/jop.2000.71.4.546. [DOI] [PubMed] [Google Scholar]
- 11.Buser D, Weber HP, Donath K, Fiorellini JP, Paquette DW, Williams RC. Soft tissue reactions to non-submerged unloaded titanium implants in beagle dogs. J Periodontol. 1992;63:225–35. doi: 10.1902/jop.1992.63.3.225. [DOI] [PubMed] [Google Scholar]
- 12.Jokstad A, Braegger U, Brunski JB, Carr AB, Naert I, Wennerberg A. Quality of dental implants. Int Dent J. 2003;53:409–43. doi: 10.1111/j.1875-595x.2003.tb00918.x. [DOI] [PubMed] [Google Scholar]
- 13.Schmitt CM, Nogueira-Filho G, Tenebaum HC, Lai JY, Brito C, Doring H, Nonhoff J. Performance of conical abutment (Morse taper) connection implants: A systematic review. J Biomed Mater Res A. 2014;102:552–74. doi: 10.1002/jbm.a.34709. [DOI] [PubMed] [Google Scholar]
- 14.Dibart S, Warbington M, Su MF, Skobe Z. In vitro evaluation of the implant-abutment bacterial seal: The locking taper system. Int J Oral Maxillofac Implants. 2005;20:732–7. [PubMed] [Google Scholar]
- 15.Ding TA, Woody RD, Higginbottom FL, Miller BH. Evaluation of the ITI Morse taper implant/abutment design with an internal modification. Int J Oral Maxillofac Implants. 2003;18:865–72. [PubMed] [Google Scholar]
- 16.Erneklint C, Odman P, Ortengren U, Karlsson S. An in vitro load evaluation of a conical implant system with 2 abutment designs and 3 different retaining-screw alloys. Int J Oral Maxillofac Implants. 2006;21:733–7. [PubMed] [Google Scholar]
- 17.Jansen VK, Conrads G, Richter EJ. Microbial leakage and marginal fit of the implant-abutment interface. Int J Oral Maxillofac Implants. 1997;12:527–40. [PubMed] [Google Scholar]
- 18.O’Mahony A, MacNeill SR, Cobb CM. Design features that may influence bacterial plaque retention: A retrospective analysis of failed implants. Quintessence Int. 2000;31:249–56. [PubMed] [Google Scholar]
- 19.Persson LG, Lekholm U, Leonhardt A, Dahlén G, Lindhe J. Bacterial colonization on internal surfaces of Brånemark system implant components. Clin Oral Implants Res. 1996;7:90–5. doi: 10.1034/j.1600-0501.1996.070201.x. [DOI] [PubMed] [Google Scholar]
- 20.Quirynen M, Bollen CM, Eyssen H, van Steenberghe D. Microbial penetration along the implant components of the Brånemark system. An in vitro study. Clin Oral Implants Res. 1994;5:239–44. doi: 10.1034/j.1600-0501.1994.050407.x. [DOI] [PubMed] [Google Scholar]
- 21.Quirynen M, De Soete M, van Steenberghe D. Infectious risks for oral implants: A review of the literature. Clin Oral Implants Res. 2002;13:1–19. doi: 10.1034/j.1600-0501.2002.130101.x. [DOI] [PubMed] [Google Scholar]
- 22.Quirynen M, Papaioannou W, van Steenberghe D. Intraoral transmission and the colonization of oral hard surfaces. J Periodontol. 1996;67:986–93. doi: 10.1902/jop.1996.67.10.986. [DOI] [PubMed] [Google Scholar]
- 23.Quirynen M, van Steenberghe D. Bacterial colonization of the internal part of two-stage implants. An in vivo study. Clin Oral Implants Res. 1993;4:158–61. doi: 10.1034/j.1600-0501.1993.040307.x. [DOI] [PubMed] [Google Scholar]
- 24.Quirynen M, Vogels R, Peeters W, van Steenberghe D, Naert I, Haffajee A. Dynamics of initial subgingival colonization of ’pristine’ peri-implant pockets. Clin Oral Implants Res. 2006;17:25–37. doi: 10.1111/j.1600-0501.2005.01194.x. [DOI] [PubMed] [Google Scholar]
- 25.Larrucea Verdugo C, Jaramillu Nunez G, Acevedo Avila A, Larrucea San Martin C. Microleakage of the prosthetic abutment/implant interface with internal and external connection:In vitro study. Clin Oral Implants Res. 2014;25:1078–83. doi: 10.1111/clr.12217. [DOI] [PubMed] [Google Scholar]
- 26.Tenenbaum H, Schaaf JF, Cuisinier FJ. Histological analysis of the Ankylos peri-implant soft tissues in a dog model. Implant Dent. 2003;12:259–65. doi: 10.1097/01.id.0000075720.78252.54. [DOI] [PubMed] [Google Scholar]
- 27.D’Ercole S, Tripodi D, Marzo G, Bernardi S, Continenza MA, Piattelli A, Iacullli F, Mummolo S. Microleakage of bacteria in different implant-abutment assemblies: An in vitro study. J Appl Biomater Funct Mater. 2014;19:13. doi: 10.5301/jabfm.5000214. [DOI] [PubMed] [Google Scholar]
- 28.Gross M, Abramovich I, Weiss EI. Microleakage at the abutment-implant interface of osseointegrated implants: A comparative study. Int J Oral Maxillofac Implants. 1999;14:94–100. [PubMed] [Google Scholar]
- 29.Mangano C, Mangano F, Piattelli A, Iezzi G, Mangano A, La Colla L. Prospective clinical evaluation of 1920 Morse taper connection implants: Results after 4 years of functional loading. Clin Oral Implants Res. 2009;20:254–61. doi: 10.1111/j.1600-0501.2008.01649.x. [DOI] [PubMed] [Google Scholar]
- 30.Novaes AB, Jr, de Oliveira RR, Muglia VA, Papalexiou V, Taba M. The effects of interimplant distances on papilla formation and crestal resorption in implants with a Morse cone connection and a platform switch: A histomorphometric study in dogs. J Periodontol. 2006;77:1839–49. doi: 10.1902/jop.2006.060162. [DOI] [PubMed] [Google Scholar]
- 31.Pontes AE, Ribeiro FS, da Silva VC, Margonar R, Piattelli A, Cirelli JA, et al. Clinical and radiographic changes around dental implants inserted in different levels in relation to the crestal bone, under different restoration protocols, in the dog model. J Periodontol. 2008;79:486–94. doi: 10.1902/jop.2008.070145. [DOI] [PubMed] [Google Scholar]
- 32.Brägger U, Karoussis I, Persson R, Pjetursson B, Salvi G, Lang N. Technical and biological complications/failures with single crowns and fixed partial dentures on implants: A 10-year prospective cohort study. Clin Oral Implants Res. 2005;16:326–34. doi: 10.1111/j.1600-0501.2005.01105.x. [DOI] [PubMed] [Google Scholar]
- 33.Welander M, Abrahamsson I, Berglundh T. Subcrestal placement of two-part implants. Clin Oral Implants Res. 2009;20:226–31. doi: 10.1111/j.1600-0501.2008.01637.x. [DOI] [PubMed] [Google Scholar]
- 34.Canullo L, Iurlaro G, Iannello G. Double-blind randomized controlled trial study on post-extraction immediately restored implants using the switching platform concept: Soft tissue response. Preliminary report. Clin Oral Implants Res. 2009;20:414–20. doi: 10.1111/j.1600-0501.2008.01660.x. [DOI] [PubMed] [Google Scholar]
- 35.Covani U, Marconcini S, Crespi R, Barone A. Bacterial plaque colonization around dental implant surfaces. Implant Dent. 2006;15:298–304. doi: 10.1097/01.id.0000226823.58425.19. [DOI] [PubMed] [Google Scholar]
- 36.Canullo L, Fedele GR, Iannello G, Jepsen S. Platform switching and marginal bone-level alterations: The results of a randomized-controlled trial. Clin Oral Implants Res. 2010;21:115–21. doi: 10.1111/j.1600-0501.2009.01867.x. [DOI] [PubMed] [Google Scholar]
- 37.Canullo L, Pellegrini G, Allievi C, Trombelli L, Annibali S, Dellavia C. Soft tissues around long-term platform switching implant restorations: A histological human evaluation. Preliminary results. J Clin Periodontol. 2011;38:86–94. doi: 10.1111/j.1600-051X.2010.01641.x. [DOI] [PubMed] [Google Scholar]
- 38.Cappiello M, Luongo R, Di Iorio D, Bugea C, Cocchetto R, Celletti R. Evaluation of peri-implant bone loss around platform-switched implants. Int J Periodontics Restorative Dent. 2008;28:347–55. [PubMed] [Google Scholar]
- 39.Lazzara RJ, Porter SS. Platform switching: A new concept in implant dentistry for controlling postrestorative crestal bone levels. Int J Periodontics Restorative Dent. 2006;26:9–17. [PubMed] [Google Scholar]
- 40.Canullo L, Rasperini G. Preservation of peri-implant soft and hard tissues using platform switching of implants placed in immediate extraction sockets: A proof-of-concept study with 12- to 36-month follow-up. Int J Oral Maxillofac Implants. 2007;22:995–1000. [PubMed] [Google Scholar]
- 41.Luongo R, Traini T, Guidone PC, Bianco G, Cocchetto R, Celletti R. Hard and soft tissue responses to the platform-switching technique. Int J Periodontics Restorative Dent. 2008;28:551–7. [PubMed] [Google Scholar]
- 42.Farronato D, Santoro G, Canullo L, Botticelli D, Maiorana C, Lang NP. Establishment of the epithelial attachment and connective tissue adaptation to implants installed under the concept of “platform switching”: A histologic study in minipigs. Clin Oral Implants Res. 2012;23:90–4. doi: 10.1111/j.1600-0501.2011.02196.x. [DOI] [PubMed] [Google Scholar]
- 43.Oh TJ, Yoon J, Misch CE, Wang HL. The causes of early implant bone loss: Myth or science? J Periodontol. 2002;73:322–33. doi: 10.1902/jop.2002.73.3.322. [DOI] [PubMed] [Google Scholar]
- 44.Abrahamsson I, Berglundh T, Wennström J, Lindhe J. The peri-implant hard and soft tissues at different implant systems. A comparative study in the dog. Clin Oral Implants Res. 1996;7:212–9. doi: 10.1034/j.1600-0501.1996.070303.x. [DOI] [PubMed] [Google Scholar]
- 45.Hermann JS, Cochran DL, Nummikoski PV, Buser D. Crestal bone changes around titanium implants. A radiographic evaluation of unloaded nonsubmerged and submerged implants in the canine mandible. J Periodontol. 1997;68:1117–30. doi: 10.1902/jop.1997.68.11.1117. [DOI] [PubMed] [Google Scholar]
- 46.Hürzeler M, Fickl S, Zuhr O, Wachtel HC. Peri-implant bone level around implants with platform-switched abutments: Preliminary data from a prospective study. J Oral Maxillofac Surg. 2007;65:33–9. doi: 10.1016/j.joms.2007.03.024. [DOI] [PubMed] [Google Scholar]
- 47.Albrektsson T, Zarb G, Worthington P, Eriksson AR. The long-term efficacy of currently used dental implants: A review and proposed criteria of success. Int J Oral Maxillofac Implants. 1986;1:11–25. [PubMed] [Google Scholar]
- 48.Hagiwara Y. Does platform switching really prevent crestal bone loss around implants? Jpn Dent Sci Rev. 2010;46:122–31. [Google Scholar]
- 49.Chou CT, Morris HF, Ochi S, Walker L, DesRosiers D. AICRG, part II: Crestal bone loss associated with the Ankylos implant: Loading to 36 months. J Oral Implantol. 2004;30:134–43. doi: 10.1563/1548-1336(2004)30<134:APICBL>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 50.Derks J, Tomasi C. Peri-implant health and disease. A systematic review of current epidemiology. J Clin Periodontol. 2015;42:S158–71. doi: 10.1111/jcpe.12334. [DOI] [PubMed] [Google Scholar]
- 51.Atieh MA, Ibrahim HM, Atieh AH. Platform switching for marginal bone preservation around dental implants: A systematic review and meta-analysis. J Periodontol. 2010 Oct;81(10):1350–66. doi: 10.1902/jop.2010.100232. [DOI] [PubMed] [Google Scholar]
- 52.Annibali S, Bignozzi I, Cristalli MP, Graziani F, La Monaca G, Polimeni A. Peri-implant marginal bone level: A systematic review and meta-analysis of studies comparing platform switching versus conventionally restored implants. J Clin Periodontol. 2012 Nov;39(11):1097–113. doi: 10.1111/j.1600-051X.2012.01930.x. [DOI] [PubMed] [Google Scholar]
- 53.Papalexiou V, Novaes AB, Jr, Ribeiro RF, Muglia V, Oliveira RR. Influence of the interimplant distance on crestal bone resorption and bone density: A histomorphometric study in dogs. J Periodontol. 2006;77:614–21. doi: 10.1902/jop.2006.050172. [DOI] [PubMed] [Google Scholar]
- 54.Tarnow DP, Magner AW, Fletcher P. The effect of the distance from the contact point to the crest of bone on the presence or absence of the interproximal dental papilla. J Periodontol. 1992;63:995–6. doi: 10.1902/jop.1992.63.12.995. [DOI] [PubMed] [Google Scholar]
- 55.Scarano A, Assenza B, Piattelli M, Thams U, San Roman F, Favero GA, et al. Interimplant distance and crestal bone resorption: A histologic study in the canine mandible. Clin Implant Dent Relat Res. 2004;6:150–6. doi: 10.1111/j.1708-8208.2004.tb00222.x. [DOI] [PubMed] [Google Scholar]
- 56.Novaes AB, Jr, Barros RR, Muglia VA, Borges GJ. Influence of interimplant distances and placement depth on papilla formation and crestal resorption: A clinical and radiographic study in dogs. J Oral Implantol. 2009;35:18–27. doi: 10.1563/1548-1336-35.1.18. [DOI] [PubMed] [Google Scholar]
- 57.de Oliveira RR, Novaes AB, Jr, Papalexiou V, Muglia VA, Taba M., Jr Influence of interimplant distance on papilla formation and bone resorption: A clinical-radiographic study in dogs. J Oral Implantol. 2006;32:218–27. doi: 10.1563/793.1. [DOI] [PubMed] [Google Scholar]
- 58.Degidi M, Nardi D, Piattelli A. One abutment at one time: Non-removal of an immediate abutment and its effect on bone healing around subcrestal tapered implants. Clin Oral Implants Res. 2011;22:1303–7. doi: 10.1111/j.1600-0501.2010.02111.x. [DOI] [PubMed] [Google Scholar]
- 59.Choi KS, Lozada JL, Kan JY, Lee SH, Kim CS, Kwon TG. Study of an experimental microthreaded scalloped implant design: Proximal bone healing at different interimplant distances in a canine model. Int J Oral Maxillofac Implants. 2010;25:681–9. [PubMed] [Google Scholar]
- 60.Gargiulo AW, Wentz FM, Orban B. Dimension and relations of the dentogingival junction in humans. J Periodontol. 1961;32:261–7. [Google Scholar]
- 61.Vacek JS, Gher ME, Assad DA, Richardson AC, Giambarresi LI. The dimensions of the human dentogingival junction. Int J Periodontics Restorative Dent. 1994;14:154–65. [PubMed] [Google Scholar]
- 62.Berglundh T, Lindhe J, Ericsson I, Marinello CP, Liljenberg B, Thomsen P. The soft tissue barrier at implants and teeth. Clin Oral Implants Res. 1991;2:81–90. doi: 10.1034/j.1600-0501.1991.020206.x. [DOI] [PubMed] [Google Scholar]
- 63.Gastaldo JF, Cury PR, Sendyk WR. Effect of the vertical and horizontal distances between adjacent implants and between a tooth and an implant on the incidence of interproximal papilla. J Periodontol. 2004;75:1242–6. doi: 10.1902/jop.2004.75.9.1242. [DOI] [PubMed] [Google Scholar]
- 64.Belser U, Buser D, Higginbottom F. Consensus statements and recommended clinical procedures regarding esthetics in implant dentistry. Int J Oral Maxillofac Implants. 2004;19(Suppl):73–4. [PubMed] [Google Scholar]
- 65.Cochran DL, Hermann JS, Schenk RK, Higginbottom FL, Buser D. Biologic width around titanium implants. A histometric analysis of the implanto-gingival junction around unloaded and loaded nonsubmerged implants in the canine mandible. J Periodontol. 1997;68:186–98. doi: 10.1902/jop.1997.68.2.186. [DOI] [PubMed] [Google Scholar]
- 66.Tarnow D, Stahl SS, Magner A, Zamzok J. Human gingival attachment responses to subgingival crown placement. Marginal remodelling. J Clin Periodontol. 1986;13:563–9. doi: 10.1111/j.1600-051x.1986.tb00848.x. [DOI] [PubMed] [Google Scholar]
- 67.Tarnow D, Elian N, Fletcher P, Froum S, Magner A, Cho SC, et al. Vertical distance from the crest of bone to the height of the interproximal papilla between adjacent implants. J Periodontol. 2003;74:1785–8. doi: 10.1902/jop.2003.74.12.1785. [DOI] [PubMed] [Google Scholar]
- 68.Maeda Y, Miura J, Taki I, Sogo M. Biomechanical analysis on platform switching: Is there any biomechanical rationale? Clin Oral Implants Res. 2007;18:581–4. doi: 10.1111/j.1600-0501.2007.01398.x. [DOI] [PubMed] [Google Scholar]
- 69.Kitagawa T, Tanimoto Y, Odaki M, Nemoto K, Aida M. Influence of implant/abutment joint designs on abutment screw loosening in a dental implant system. J Biomed Mater Res B Appl Biomater. 2005;75:457–63. doi: 10.1002/jbm.b.30328. [DOI] [PubMed] [Google Scholar]
- 70.Chun HJ, Shin HS, Han CH, Lee SH. Influence of implant abutment type on stress distribution in bone under various loading conditions using finite element analysis. Int J Oral Maxillofac Implants. 2006;21:195–202. [PubMed] [Google Scholar]
- 71.Oshida Y, Tuna EB, Aktören O, Gençay K. Dental implant systems. Int J Mol Sci. 2010;11:1580–678. doi: 10.3390/ijms11041580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Perriard J, Wiskott WA, Mellal A, Scherrer SS, Botsis J, Belser UC. Fatigue resistance of ITI implant-abutment connectors – A comparison of the standard cone with a novel internally keyed design. Clin Oral Implants Res. 2002;13:542–9. doi: 10.1034/j.1600-0501.2002.130515.x. [DOI] [PubMed] [Google Scholar]
- 73.Steinmann SG, Winter GD, Leray JL, de Groot K, editors. In Evaluation of Biomaterials. New York, USA: John Wiley and Sons; 1980. pp. 1–34. [Google Scholar]
- 74.Dedigi M, Novaes AB, Nardi D, Piattelli A. Immediately loaded titanium implant with a tissue-stabilizing/maintaining design (beyond platform switch) retrieved from man after 4 weeks: A histological and histomorphometrical evaluation. A case report. Clin Oral Implants Res. 2008;19:276–82. doi: 10.1111/j.1600-0501.2007.01449.x. [DOI] [PubMed] [Google Scholar]
- 75.Krebs M, Schmenger K, Neumann K, Weigl P, Moser W, Nentwig GH. Long-term evaluation of Ankylos® dental implants, part I: 20-year life table analysis of a longitudinal study of more than 12,500 implants. Clin Implant Dent Relat Res. 2015;17:2–12. doi: 10.1111/cid.12154. [DOI] [PubMed] [Google Scholar]
- 76.Bozkaya D, Müftü S. Mechanics of the tapered interference fit in dental implants. J Biomech. 2003;36:1649–58. doi: 10.1016/s0021-9290(03)00177-5. [DOI] [PubMed] [Google Scholar]
- 77.Morris HF, Ochi S, Crum P, Orenstein IH, Winkler S. AICRG, part I: A 6-year multicentered, multidisciplinary clinical study of a new and innovative implant design. J Oral Implantol. 2004;30:125–33. doi: 10.1563/1548-1336(2004)30<125:APIAYM>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 78.Berglundh T, Persson L, Klinge B. A systematic review of the incidence of biological and technical complications in implant dentistry reported in prospective longitudinal studies of at least 5 years. J Clin Periodontol. 2002;29(Suppl 3):197–212. doi: 10.1034/j.1600-051x.29.s3.12.x. [DOI] [PubMed] [Google Scholar]
- 79.Gracis S, Michalakis K, Vigolo P, Vult von Steyen P, Zwahlen M, Sailer I. Internal vs external connections for abutments/reconstructions: A systematic review. Clin Oral Implants. 2012;23:202–16. doi: 10.1111/j.1600-0501.2012.02556.x. [DOI] [PubMed] [Google Scholar]
- 80.Brägger U, Aeschlimann S, Bürgin W, Hämmerle CH, Lang NP. Biological and technical complications and failures with fixed partial dentures (FPD) on implants and teeth after four to five years of function. Clin Oral Implants Res. 2001;12:26–34. doi: 10.1034/j.1600-0501.2001.012001026.x. [DOI] [PubMed] [Google Scholar]
- 81.Chapman RJ, Grippo W. The locking taper attachment for implant abutments: Use and reliability. Implant Dent. 1996;5:257–61. doi: 10.1097/00008505-199600540-00004. [DOI] [PubMed] [Google Scholar]
- 82.Garber DA, Salama MA, Salama H. Immediate total tooth replacement. Compend Contin Educ Dent. 2001;22:210–6. 218. [PubMed] [Google Scholar]
- 83.Sutter F, Weber H, Sorensen J. The new restorative concept of the ITI dental implant system: Design and engineering. Int J Periodontics Restorative Dent. 1993;13:409–31. [Google Scholar]
- 84.Weigl P. New prosthetic restorative features of the Ankylos implant system. J Implantol. 2004;30:178–88. doi: 10.1563/1548-1336(2004)30<178:NPRFOT>2.0.CO;2. [DOI] [PubMed] [Google Scholar]


