Abstract
Background:
Serum troponin T (TnT) is a common marker of myocardial injury. However, its implication in the absence of clinical evidence of cardiac reason is not well established.
Aims:
The aim of this study was to identify the implications of positive TnT in traumatic chest injury (TCI) patients regardless of the cardiac involvement.
Materials and Methods:
We conducted a retrospective analysis of all TCI patients admitted to level 1 trauma center between 2008 and 2011. Patients who underwent TnT testing were divided into two groups: Group 1 (positive TnT) and Group 2 (negative TnT). The two groups were analyzed and compared, and multivariate regression analyses were performed to identify predictors of TnT positivity and mortality.
Results:
Out of 993 blunt TCI patients, 19.3% had positive TnT (Group 1). On comparison to Group 2, patients in Group 1 were 5 years younger and more likely to have head, cardiac, hepatic, splenic, and pelvic injuries, in addition to lung contusion. Positive TnT was associated with higher Injury Severity Score (ISS) (P = 0.001), higher chest Abbreviated Injury Score (AIS) (P = 0.001), and longer hospital stay (P = 0.03). In addition, Group 1 patients were more likely to undergo chest tube insertion, exploratory laparotomy, mechanical ventilation, and tracheostomy. Twenty patients had cardiac involvement, and of them 14 had positive TnT. Among 973 patients who showed no evidence of cardiac involvement, 178 had positive TnT (18.3%). There were 104 deaths (60% in Group 1). On multivariate regression analysis, the predictors of hospital mortality were positive TnT, head injury, and high ISS, whereas, the predictors of TnT positivity were cardiac, hepatic, and pelvic injuries; higher ISS; and age.
Conclusions:
Positive TnT in blunt TCI patients is a common challenge, particularly in polytrauma cases. Patients with positive TnT tend to have the worst outcome even in the absence of clinical evidence of acute cardiac involvement. Positive TnT is also a reflection of the severity of chest or extrathoracic injuries; however, further prospective studies are warranted.
Keywords: Blunt trauma, cardiac, chest injury, mortality, troponin
Introduction
Thoracic trauma is responsible for up to 25% of all trauma-related fatalities.[1] Prior data showed that in blunt chest trauma (traumatic chest injury or TCI), the incidence of blunt cardiac injury varied 20-76%.[2,3,4,5] An earlier study reported a 30% incidence of blunt cardiac injury among TCI patients; of those, 5% cases developed in-hospital complications that required acute interventions.[6] Moreover, postmortem findings of blunt trauma patients who died immediately after injury confirmed the presence of cardiac injury in 14% of cases.[7]
Cardiac troponins (cTn), specifically troponin T (TnT) and troponin I (TnI) are released into the circulation in response to acute myocardial injury/necrosis. Currently, cTn is one of the preferred biomarkers for the detection of cardiac injury with higher sensitivity and specificity than creatinine kinase-myocardial band (CK-MB) assay.[3] Earlier studies reported elevated cTn levels in 15-28% of cases presented with abnormal electrocardiogram (ECG) after traumatic blunt TCI.[2,5,8] Evidence based on earlier data has suggested that circulating cTn possesses low sensitivity (12-23%) for detection of blunt cardiac injury but high specificity (97-100%), therefore it has clinical relevance to rule out myocardial injury.[5,9,10] A recent study reported TnT levels to be a significant biomarker of mortality in high-risk non-cardiac surgery patients.[11] However, limited information is available on the implications of TnT in trauma patients who presented with no clinical evidence of cardiac causes. The present study aims to assess the implications and outcomes of positive TnT in patients who sustained blunt TCI with and without apparent acute cardiac injury.
Materials and Methods
This study was approved by the Medical Research Center (IRB# 10129/10 and 12010/12) at Hamad Medical Corporation (HMC), Doha, Qatar. All patients with major blunt TCI who were admitted to the Level I trauma center at HMC were retrospectively reviewed between January 2008 and June 2011. The major blunt TCI was defined as a history of blunt mechanism of injury in the presence of any of the following: Hemothorax, pneumothorax, rib fracture, lung contusion, or major intrathoracic vascular injury. Patients with penetrating injury, with isolated clavicular fracture, having a history of thoracic injury without radiological evidence, and known to have ischemic heart disease or cardiac rhythm abnormalities were excluded. The mechanism of blunt chest trauma included motor vehicle collision (MVC), pedestrian injuries, and falls. Patients with nondocumented TnT measurements were excluded. Patients with blunt TCI were divided into two groups based on their TnT status: Positive TnT (Group 1) versus negative TnT (Group 2).
Collected data included demographics, mechanism of injury, Injury Severity Score (ISS),[12] chest Abbreviated Injury Score (AIS),[12] associated extrathoracic injuries, need of mechanical ventilation and surgical procedure (laparotomy, thoracotomy, thoracostomy tube drainage, and tracheostomy), ECG findings, length of hospital stay, and in-hospital all-cause mortality.
On admission, three sets of serum TnT level (6 h apart, approximately) were performed for TCI patients and TnT values greater than 0.1 ng/mL were considered positive according to our laboratory cutoff. Additionally, 12-lead ECG was performed serially, if clinically indicated with abnormal initial ECG and cardiac enzymes. As there were no hospital guidelines, serial cardiac markers were requested for selected cases according to the attending physician's discretion. Transthoracic echocardiography (TTE) was ordered in patients with arrhythmias, suspected cardiac injury by auscultation (for any murmurs or abnormal heart sounds), elevated biomarkers, or unexplained hypotension after complete resuscitation. Generally, myocardial injury was suspected in patients who fulfilled at least one of the following criteria: (a) presumably new abnormal cardiac rhythm, or rate, abnormal echocardiographic findings (wall motion, valvular or septal abnormalities); and (b) hemopericardium.[13]
Statistical analysis
Data were presented as proportions, medians [interquartile range (IQR)], or mean [±standard deviation (SD)] as appropriate. Differences between categorical and continuous variables among the two TnT groups were analyzed using the chi-square test and Student's t test, respectively. The correlation between TnT groups and ISS was demonstrated using side-by-side box plots. Multivariate logistic regression analysis was performed for the predictors of in-hospital mortality after adjusting the potential covariates that showed significant differences among the study groups in the univariate analysis. A two-tailed P value of <0.05 was considered significant. Another multivariate analysis looking at the predictors of a positive TnT test among TCI patients was also performed. Receiver-operator characteristic (ROC) curves were plotted for the initial three TnT levels against mortality. The area under the curve (AUC) of 1.0 was considered perfect discrimination and 0.5 considered equal to chance. All data analyses were carried out using the IBM Statistical Package for Social Sciences (SPSS IBM Corp) for Windows, Version 19.0. Armonk, NY, USA.
Results
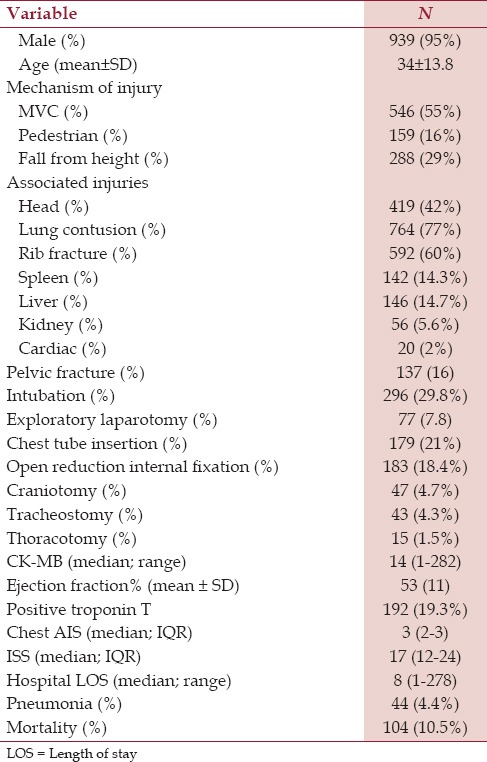
During the study period, 5118 patients were admitted to the trauma section; of them 1358 patients sustained blunt TCI. There were 365 excluded cases in whom TnT readings were not documented. Only 993 cases with TCI and TnT measurements were included in the study. The common mechanisms of injury were MVC (55%), fall from height (29%), and pedestrian hit by car (16%). Frequently encountered injuries included lung contusions (77%), rib fractures (60%), and head injuries (42%). The median chest AIS was 3 (IQR 2-3), ISS was 17 (IQR 12-24), and the length of hospital stay was 8 (range 1-278) days [Table 1]. TnT was positive in 192 (19%) patients.
Table 1.
Demographics, mechanism of injury, and clinical presentation of traumatic chest injury patients (N = 993)
Patients’ demographics and mechanism of injury were compared among positive and negative TnT groups [Table 2]. On comparison to Group 2, patients in Group 1 (positive TnT) were 5 years younger and more likely to have head, cardiac, hepatic, splenic, and pelvic injuries in addition to lung contusion. Group 1 patients were more likely to undergo chest tube insertion (P = 0.001), exploratory laparotomy (P = 0.001), mechanical ventilation (P = 0.001), tracheostomy (P = 0.001) and long bone open reduction with internal fixation (P = 0.04). Moreover, patients with positive TnT had higher median (IQR) ISS [24 (17-34) versus 16 (10-22); P = 0.001] and chest AIS [3 (3-3) versus 3 (2-3); P = 0.001]. There was a correlation between TnT groups and ISS. Positive TnT was significantly associated with higher ISS [Figure 1].
Table 2.
Analysis of chest injuries according to troponin T status
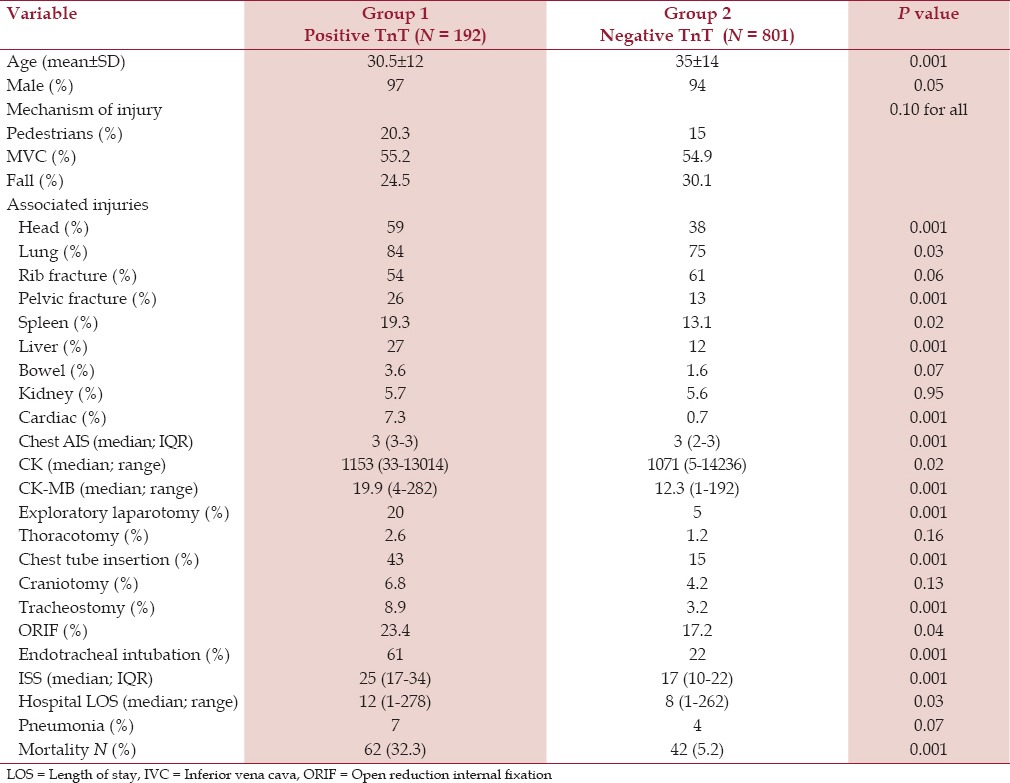
Figure 1.
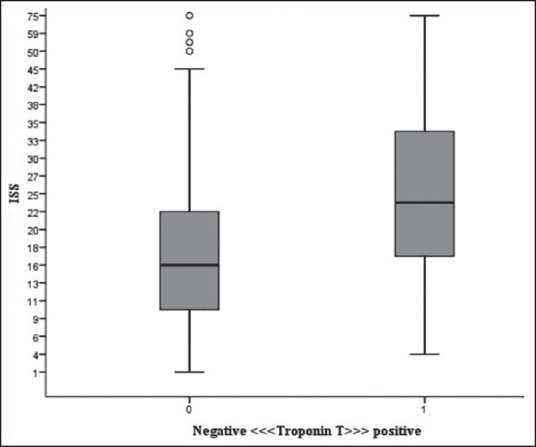
The correlation between TnT and ISS
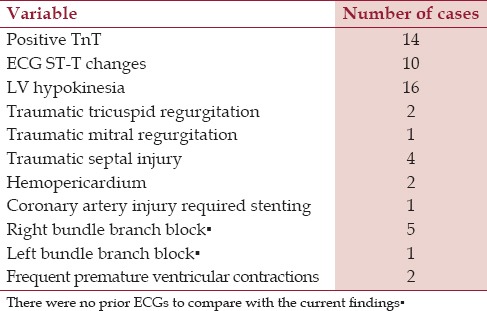
Cardiac evaluation
The frequency of cardiac involvement (N = 20) revealed that 14 had positive TnT and 6 had negative TnT [Table 3]. Subanalysis of cardiac involvement cases revealed no statistically significant difference of mortality between Group 1 and Group 2 patients (28.6% vs 0.0%, P = 0.14).
Table 3.
Cardiac involvements (N = 20)
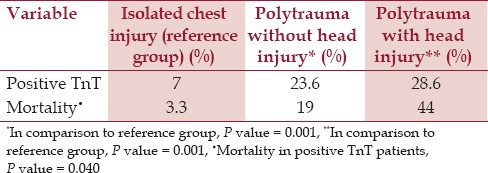
Among 973 TCI patients with no cardiac involvement, 178 had positive TnT (18.3%). The in-hospital mortality rate was significantly higher in noncardiac patients with positive TnT as compared to negative TnT (32.6% vs 5.3%, P = 0.001). These findings suggested a clinical relevance of positive TnT in patients without cardiac injury. TTE was performed in 72% of patients with positive TnT; of them, only 19% showed abnormal left ventricular (LV) function. A subanalysis was performed to address the TnT positivity in isolated chest injury versus polytrauma patients (with and without head injury). TnT positivity was significantly higher in the two polytrauma subgroups with head injury (28.6% vs 7%; P = 0.001) and without head injury (23.6% vs 7%; P = 0.001) in comparison to isolated chest injuries [Table 4]. Moreover, the mortality rate was higher in polytrauma involving head injury in comparison to the other subanalysis groups.
Table 4.
Comparison of Troponin T (TnT) positivity and outcomes (isolated chest injury versus polytrauma)
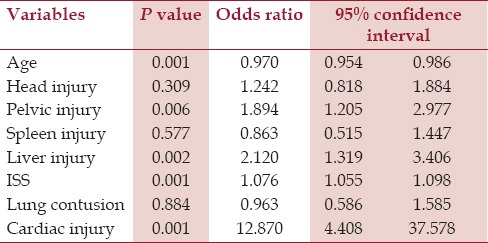
Predictors of TnT positivity
Relevant variables in terms of age, head injury, cardiac injury, lung contusion, splenic injury, hepatic injuries, and ISS were used in multivariate regression analysis. The analysis showed that cardiac [odds ratio (OR) 12.9; P = 0.001], hepatic (OR 2.1; P = 0.002), and pelvic injuries (OR 1.9; P = 0.006) in addition to high ISS (OR 1.1; P = 0.001) and age (OR 0.97; P = 0.001) were the independent predictors of TnT positivity [Table 5].
Table 5.
Predictors of troponin T positivity in TCI
Outcomes
Prolonged hospitalization (P = 0.03) and a higher rate of pneumonia (P = 0.07) were evident in Group 1 when compared with Group 2 [Table 2]. The overall mortality in the study population was 10.5% (N = 104); the majority of them had positive TnT. The mortality rate was 6 times greater in patients who had positive TnT in comparison to those who had negative TnT (32% vs 5.2%; P = 0.001).
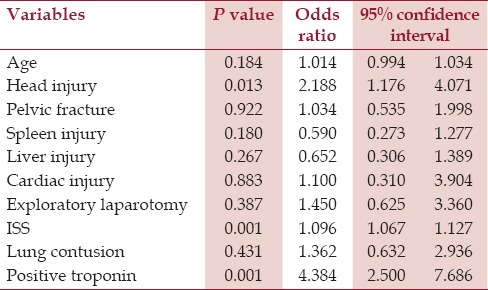
Predictors of mortality
Multivariate regression analysis used 10 relevant variables with significant differences in the univariate analysis [Table 6]. Positive TnT (OR 4.4, P = 0.001), associated head injury (OR 2.2, P = 0.01), and higher ISS (OR 1.1, P = 0.001) were the independent predictors of mortality among TCI patients.
Table 6.
Predictors of mortality in TCI
ROC curve and AUC using the initial readings of TnT levels were performed for the prediction of mortality [Figure 2]. This showed that the TnT cutoff level of 0.4 ng/mL predicted hospital mortality more accurately when compared to the other cutoff reading (0.11 ng/mL), P = 0.01.
Figure 2.
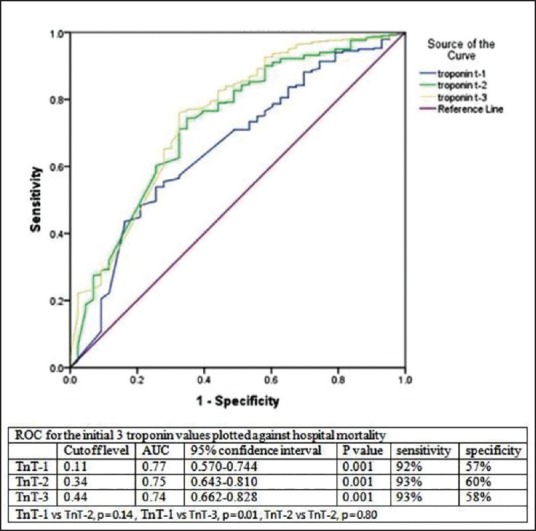
ROC curve and AUC for three readings of TnT levels for prediction of mortality
Discussions
There are a few reports describing the implication of positive TnT in patients presented with blunt TCI.[4,10,14,15] The present analysis revealed several key findings. In our series, 19% of blunt TCI patients had positive TnT. Moreover, in the absence of an apparent cardiac cause, almost one-fifth of patients had positive TnT. The overall mortality was 10.5% and of them 60% had positive TnT. Interestingly, the current study identified the predictors of positive TnT in patients with TCI, which included cardiac, hepatic, and pelvic injuries; high ISS; and age. The study highlighted the association between positive TnT and worse hospital outcomes (i.e., the need for interventions, longer length of stay, and mortality) in patients with TCI regardless of the clinical evidence of acute cardiac involvement. Our study uniquely showed a correlation between high ISS and a tendency for positive TnT. Moreover, positive TnT was independently associated with a fourfold increased risk of in-hospital mortality. In addition to positive TnT, the associated head injury and ISS were also predictors of mortality in our study cohort.
In general, diagnosis of cardiac injury in patients with TCI remains controversial.[2] Symptoms such as chest pain in patients with myocardial injury may mimic a concomitant rib fracture or muscular injury.[9,10] Chest imaging such as computed tomography is a useful tool for diagnosing injury in the great vessels and the skeletal or pulmonary structures, but it lacks sensitivity for the detection of cardiac injury.[13,16]
It has been reported that patients with severe traumatic cardiac injuries or fatal cardiac rhythm disturbances warrant immediate evaluation and treatment.[15] On the other hand, further cardiac workup and diagnosis of cardiac injury could be missed in some cases due to a lack of clinical signs and symptoms after severe trauma.[14,17] Some investigators have observed a significant correlation between cardiac injury and mortality.[18]
Moreover, due to the lack of an optimal test for myocardial injury in trauma, the exact incidence of a cardiac injury in patients with blunt TCI is not well established. Therefore, a wide variation has been reported in the incidence of cardiac injury in studies based on autopsies (15-20%), clinical presentation (9-76%), and troponin assay.[15,19]
Interestingly, higher TnT levels have been observed in severe traumatic brain injury patients. Salim et al.[20] reported that TnT is independently associated with adverse outcomes in patients with traumatic brain injury. In our cohort, fewer than half of the TCI patients had associated head injury, and mortality among those with positive TnT was 4 times higher in comparison to patients who had no associated head injury.
In addition, increased TnT levels are frequently found in septic or critically ill patients. It has been observed that 50-85% of critically ill patients had significantly elevated levels of cTn, which correlated well with disease severity.[21,22,23,24]
Earlier studies reported that the development of hypotension and/or multiple organ dysfunction was more frequent in patients with elevated TnT as compared to patients with negative TnT.[24,25] This finding enlightened a link between the positivity of TnT and the degree of myocardial injury in intensive care unit (ICU) patients, which could be mainly related to a physiologic stress or illness rather than mechanical chest trauma or direct cardiac injury. In our study, a proportion of trauma cases with evidence of cardiac injury were cases of young patients with no prior history of atherosclerotic coronary artery disease.
In the present study, the median ISS showed an association with the elevated TnT that may reflect a degree of ongoing physiologic stress. In addition, elevated TnT could possibly be associated with the severity of chest trauma or other extrathoracic associated injuries, such as head and abdomen injury. In our series, TnT positivity was significantly higher in the polytrauma cases with and without associated head injury. An earlier study suggested that elevated serum troponin (TnI) levels post trauma correlated well with the degree of the overall injury and physiologic stress and were not related to chest trauma alone.[24] Positive TnT in patients with no obvious cardiac causes could be in part explained with the possibility of a silent or minor degree of cardiac injury. However, we cannot exclude the possibility of false-positive elevations due to TnT release under other clinical situations.[5,26]
Earlier studies included trauma[20,24] and high-risk surgical patients,[27] and found elevated TnT levels to be associated with significant increase in morbidity and mortality. A recent study demonstrated an association between TnT levels and mortality in patients undergoing noncardiac surgery.[28] The authors suggested that the peaked values of TnT after the first 3 days of surgery were significantly correlated with the 30-day mortality. Moreover, a dose/response relationship has been observed between the troponin levels (TnI) and the risk of mortality after noncardiac surgery.[29] Our findings showed that in comparison to negative TnT, TCI patients with positive TnT had prolonged hospital length of stay, increased need of invasive procedures, and greater frequency of hospital complications and mortality. Based on the ROC and AUC, a TnT cutoff of 0.4 ng/mL would predict in-hospital mortality in TCI patients as compared to other cutoff values. However, our laboratory protocol considers TnT values greater than 0.1 as a positive test.
Elevated serum troponins have wide implications, as elevated levels of TnT or TnI and abnormal ECG indicate poor prognosis with increased risk of cardiac complications. Therefore, such patients should be evaluated thoroughly with echocardiography and serial ECGs.[4,19] However, there are a few studies showing lower sensitivity and predictive values of TnT and TnI for the diagnosis of myocardial contusion.[4] Despite this, the authors still considered TnI to be relatively more specific than TnT. The present study reported 6 patients who had clinically relevant myocardial injury without significant troponin release. Our findings are in agreement with earlier studies that the TnT test alone has low sensitivity for diagnosing myocardial injury[5,14] and so it may have more clinical relevance to rule out myocardial injury.
Recently in 2015, Skinner et al.[30] studied 169 TCI cases over 3 years, of whom 50% were found to have blunt cardiac injury. These authors reported that TnI, ECG, and TTE were performed in only 71%, 34%, and 45% of cases. They also mentioned a couple of limitations in their study interpretation. For instance, the definition applied to TCI in their study was not universally accepted. They reported that only 45% of blunt cardiac injury patients underwent TTE, which may have a potential of underestimated cardiac injuries. In addition, TTE was performed by different operators, which might contribute to the proposed variability in interpreting the study findings. Moreover, there was significant heterogeneity in the assays used for serum troponin detection due to changes over time.[30]
Limitations
The present analysis has some limitations, including the retrospective design and use of TTE instead of transesophageal echocardiography, which might miss a few cardiac cases due to poor view windows in patients with rib and/or lung injuries. The lack of autopsy findings to confirm myocardial injury is also a limitation. One-fourth of patients with positive TnT had no echocardiographic assessment. We could not find a reason for that in the database, and this may mean underestimation of the presence of cardiac injury. For risk stratification in patients with blunt TCI, TnT is considered less sensitive relative to TnI.[15] However, the assessment of troponin levels in TCI (TnT or TnI) has important prognostic implications. Due to the retrospective nature of our study, we relied only on TnT, as TnI was not frequently used in our trauma unit during the study period. We cannot assure that all the abnormal ECG or TTE findings were new or old; the latter limitation may explain in part the negative TnT in some cases. The exact information for the time of blood sampling is lacking. Parameters supporting diagnosis of cardiac stress were not addressed, therefore further prospective study may be appropriate to answer these issues. At this stage, the recommendation of routine cardiac workup for all blunt chest trauma patients is not well settled unless there is a clinical suspicion. Additionally, the optimum timing and cutoff levels need further revision. Although it is not reported in our database and rarely encountered in our experience, sternal fracture could be of importance in such analysis.
Conclusion
Positive TnT in patients with blunt TCI is common, particularly in polytrauma cases. Moreover, it is associated with worse outcome even in the absence of sound clinical evidence of cardiac involvement. TnT elevation in TCI is not only a reflection of the overall severity of chest injury as well as the associated extrathoracic injuries, but is also an indicator of prolonged hospitalization and mortality. Further prospective studies are required to support our findings. Moreover, TCI with positive TnT is a major challenge in critical trauma care, therefore well-established guidelines are warranted.
Financial support and sponsorship
Nil.
Conflicts of interest
The authors declare that they have no competing interests. All authors have no financial issues to disclose.
Acknowledgment
The authors thank the entire registry database team in the section of trauma surgery. The Medical Research Center (IRB# 10129/10 and 12010/12) at HMC, Qatar, approved the study. This study was presented in part at the Southeastern Surgical Congress, February 22-25, 2014, Georgia, USA.
References
- 1.Ekpe EE, Eyo C. Determinants of mortality in chest trauma patients. Niger J Surg. 2014;20:30–4. doi: 10.4103/1117-6806.127107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.El-Menyar A, Al Thani H, Zarour A, Latifi R. Understanding traumatic blunt cardiac injury. Ann Card Anaesth. 2012;15:287–95. doi: 10.4103/0971-9784.101875. [DOI] [PubMed] [Google Scholar]
- 3.Babuin L, Jaffe AS. Troponin: The biomarker of choice for the detection of cardiac injury. CMAJ. 2005;173:1191–202. doi: 10.1503/cmaj.050141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bertinchant JP, Polge A, Mohty D, Nguyen-Ngoc-Lam R, Estorc J, Cohendy R, et al. Evaluation of incidence, clinical significance, and prognostic value of circulating cardiac troponin I and T elevation in hemodynamically stable patients with suspected myocardial contusion after blunt chest trauma. J Trauma. 2000;48:924–31. doi: 10.1097/00005373-200005000-00018. [DOI] [PubMed] [Google Scholar]
- 5.Ferjani M, Droc G, Dreux S, Arthaud M, Goarin JP, Riou B, et al. Circulating cardiac troponin T in myocardial contusion. Chest. 1997;111:427–33. doi: 10.1378/chest.111.2.427. [DOI] [PubMed] [Google Scholar]
- 6.Biffl WL, Moore FA, Moore EE, Sauaia A, Read RA, Burch JM. Cardiac enzymes are irrelevant in the patient with suspected myocardial contusion. Am J Surg. 1994;168:523–8. doi: 10.1016/s0002-9610(05)80115-1. [DOI] [PubMed] [Google Scholar]
- 7.Baum V. Anesthetic complications during emergency noncardiac surgery in patients with documented cardiac contusions. J Cardiothorac Vasc Anesth. 1991;5:57–60. doi: 10.1016/1053-0770(91)90095-b. [DOI] [PubMed] [Google Scholar]
- 8.Salim A, Velmahos GC, Jindal A, Chan L, Vassiliu P, Belzberg H, et al. Clinically significant blunt cardiac trauma: Role of serum troponin levels combined with electrocardiographic findings. J Trauma. 2001;50:237–43. doi: 10.1097/00005373-200102000-00008. [DOI] [PubMed] [Google Scholar]
- 9.Schultz JM, Trunkey DD. Blunt cardiac injury. Crit Care Clin. 2004;20:57–70. doi: 10.1016/s0749-0704(03)00092-7. [DOI] [PubMed] [Google Scholar]
- 10.Sakka SG, Huettemann E, Giebe W, Reinhart K. Late cardiac arrhythmias after blunt chest trauma. Intensive Care Med. 2000;26:792–5. doi: 10.1007/s001340051248. [DOI] [PubMed] [Google Scholar]
- 11.Lake F. Troponin T highlighted as a biomarker of mortality following noncardiac surgery. Biomark Med. 2012;6:507–9. doi: 10.2217/bmm.12.59. [DOI] [PubMed] [Google Scholar]
- 12.Trauma Scoring. [Accessed January 20, 2015]. at http://www.trauma.org/archive/scores/iss.html .
- 13.Omert L, Yeaney WW, Protetch J. Efficacy of thoracic computerized tomography in blunt chest trauma. Am Surg. 2001;67:660–4. [PubMed] [Google Scholar]
- 14.Fulda GJ, Giberson F, Hailstone D, Law A, Stillabower M. An evaluation of serum troponin T and signal-averaged electrocardiography in predicting electrocardiographic abnormalities after blunt chest trauma. J Trauma. 1997;43:304–12. doi: 10.1097/00005373-199708000-00016. [DOI] [PubMed] [Google Scholar]
- 15.Karalis DG, Victor MF, Davis GA, McAllister MP, Covalesky VA, Ross JJ, Jr, et al. The role of echocardiography in blunt chest trauma: A transthoracic and transesophageal echocardiographic study. J Trauma. 1994;36:53–8. doi: 10.1097/00005373-199401000-00008. [DOI] [PubMed] [Google Scholar]
- 16.Zinck SE, Primack SL. Radiographic and CT findings in blunt chest trauma. J Thorac Imaging. 2000;15:87–96. doi: 10.1097/00005382-200004000-00003. [DOI] [PubMed] [Google Scholar]
- 17.Dubrow TJ, Mihalka J, Eisenhauer DM, de Virgilio C, Finch M, Mena IG, et al. Myocardial contusion in the stable patient: What level of care is appropriate? Surgery. 1989;106:267–74. [PubMed] [Google Scholar]
- 18.Healey MA, Brown R, Fleiszer D. Blunt cardiac injury: Is this diagnosis necessary? J Trauma. 1990;30:137–46. [PubMed] [Google Scholar]
- 19.Collins JN, Cole FJ, Weireter LJ, Riblet JL, Britt LD. The usefulness of serum troponin levels in evaluating cardiac injury. Am Surg. 2001;67:821–6. [PubMed] [Google Scholar]
- 20.Salim A, Hadjizacharia P, Brown C, Inaba K, Teixeira PG, Chan L, et al. Significance of troponin elevation after severe traumatic brain injury. J Trauma. 2008;64:46–52. doi: 10.1097/TA.0b013e31815eb15a. [DOI] [PubMed] [Google Scholar]
- 21.ver Elst KM, Spapen HD, Nguyen DN, Garbar C, Huyghens LP, Gorus FK. Cardiac troponins I and T are biologic markers of left ventricular dysfunction in septic shock. Clin Chem. 2000;46:650–7. [PubMed] [Google Scholar]
- 22.Ammann P, Fehr T, Minder EI, Günter C, Bertel O. Elevation of troponin I in sepsis and septic shock. Intensive Care Med. 2001;27:965–9. doi: 10.1007/s001340100920. [DOI] [PubMed] [Google Scholar]
- 23.Arlati S, Brenna S, Prencipe L, Marocchi A, Casella GP, Lanzani M, et al. Myocardial necrosis in ICU patients with acute non-cardiac disease: A prospective study. Intensive Care Med. 2000;26:31–7. doi: 10.1007/s001340050008. [DOI] [PubMed] [Google Scholar]
- 24.Martin M, Mullenix P, Rhee P, Belzberg H, Demetriades D, Salim A. Troponin increases in the critically injured patient: Mechanical trauma or physiologic stress? J Trauma. 2005;59:1086–91. doi: 10.1097/01.ta.0000190249.19668.37. [DOI] [PubMed] [Google Scholar]
- 25.Edouard AR, Benoist JF, Cosson C, Mimoz O, Legrand A, Samii K. Circulating cardiac troponin I in trauma patients without cardiac contusion. Intensive Care Med. 1998;24:569–73. doi: 10.1007/s001340050617. [DOI] [PubMed] [Google Scholar]
- 26.Mannu GS. The non-cardiac use and significance of cardiac troponins. Scott Med J. 2014;59:172–8. doi: 10.1177/0036933014540090. [DOI] [PubMed] [Google Scholar]
- 27.Higham H, Sear JW, Sear YM, Kemp M, Hooper RJ, Foex P. Peri-operative troponin I concentration as a marker of long-term postoperative adverse cardiac outcomes - A study in high-risk surgical patients. Anaesthesia. 2004;59:318–23. doi: 10.1111/j.1365-2044.2004.03660.x. [DOI] [PubMed] [Google Scholar]
- 28.Devereaux PJ, Chan MT, Alonso-Coello P, Walsh M, Berwanger O, Villar JC, et al. Vascular Events in Noncardiac Surgery Patients Cohort Evaluation (VISION) Study Investigators. Association between postoperative troponin levels and 30-day mortality among patients undergoing noncardiac surgery. JAMA. 2012;307:2295–304. doi: 10.1001/jama.2012.5502. [DOI] [PubMed] [Google Scholar]
- 29.Kim LJ, Martinez EA, Faraday N, Dorman T, Fleisher LA, Perler BA, et al. Cardiac troponin I predicts short-term mortality in vascular surgery patients. Circulation. 2002;106:2366–71. doi: 10.1161/01.cir.0000036016.52396.bb. [DOI] [PubMed] [Google Scholar]
- 30.Skinner DL, Laing GL, Rodseth RN, Ryan L, Hardcastle TC, Muckart DJ. Blunt cardiac injury in critically ill trauma patients: A single centre experience. Injury. 2015;46:66–70. doi: 10.1016/j.injury.2014.08.051. [DOI] [PubMed] [Google Scholar]


