Abstract
Background and Aims:
The technique of securing the epidural catheter has a major bearing on the efficacy of epidural analgesia. Specific fixator devices, for e.g., Lockit epidural catheter clamp, which successfully prevents catheter migration, are available. The possibility of catheter snapping and surgical retrieval has been reported with tunneling of catheters. These techniques have not been compared for safety, efficacy and appropriateness of achieving secure epidural catheter fixation in the postoperative period.
Material and Methods:
A total of 200 patients who required postoperative epidural analgesia were included. They were randomized into two groups: Group I (n = 100) in whom epidural catheters were tunneled vertically in the paravertebral subcutaneous tissue and group II (n = 100) wherein a Lockit device was used to fix the catheter. Likert score was used to quantify patient's comfort during procedure. The techniques were compared for migration, catheter dislodgement, local trauma, catheter snapping and catheter obstruction.
Results:
12% of tunneled catheters had migrated significantly outward. 22% of patients had erythema and 77% had significant procedural discomfort in group I. In group II, 3% catheters had kinked and 14% had erythema from device adhesive.
Conclusion:
Our results support the use of Lockit device as a safe and comfortable fixation device compared to subcutaneous tunneling of catheters.
Keywords: Analgesia epidural, catheter, subcutaneous tissue
Introduction
Epidural catheter fixation is very important. Inward migration of the epidural catheter has been reported with intravascular, subdural or subarachnoid injection of repeat doses. Outward migration might lead to loss of analgesia and unsuccessful attempts to re-establish it. Many factors have been correlated with migration, but an appropriate fixation technique for the catheter should form the most practical way to prevent it.[1]
Fixation with a strip of adhesive foam transfixed with a suture,[2] Niko Epi-Fix device,[3] Tegaderm dressing alone or with additional filter shoulder fixation,[3] Lockit device[4] and subcutaneous tunneling of catheter[5] are the techniques evaluated for their efficacy and safety.
Subcutaneous tunneling offers good fixation with transparent dressing. The interposed loop dampens any drag on the catheter, thus protecting the part of the catheter entering the epidural space. This fixation is more acceptable to patients when lying flat. An adhesive dressing over the epidural catheter seals both the catheter entry points and decreased chances of catheter contamination or infection.
We conducted a prospective, randomized study comparing the efficacy and safety of subcutaneous tunneling of the epidural catheter (STEC) and Lockit epidural catheter clamp (LECC) for securing lumbar epidural catheter in orthopedic surgical patients.
Material and Methods
The study protocol was approved by Institutional Ethics Committee. Patients posted for lower limb orthopedic surgeries, with no contraindication to receive a neuraxial block were included in the study after obtaining written consent during September 2013 to August 2014. Patients who had preexisting neurological disabilities, significant spinal deformities and who were unable to understand, express and communicate visual analog scores were excluded. Two hundred patients of either gender between 20 and 65 years of age were randomized by sealed envelope method. Cards with group I or II written were kept in the sealed envelope and randomly one card was chosen for each patient. All patients received combined spinal-epidural anesthesia in the lumbar region (L3-L4, L4-L5) using midline approach. Local anesthetic infiltration was done at the skin puncture site to ensure patient's comfort during institution of the block. Loss of resistance to air was used to identify the epidural space. A volume of 3 ml of 0.5% hyperbaric bupivacaine was deposited in subarachnoid space. A 4 cm length of the epidural catheter was placed in the epidural space and fixed by either of the undermentioned techniques. All catheters were flushed with 3 ml of saline to rule out catheter kink postfixation.
Group I or STEC (n=100) had the epidural catheter subcutaneously tunneled vertically using a Tuohy 18 G epidural needle 1.5 cm lateral to the midline. The epidural needle was used to create the tunnel 3-4 cm long in subcutaneous plane, moving from above downward after local infiltration, with its lower end at the same horizontal level as the epidural puncture site. A small loop of catheter was left between the epidural puncture site and the tunnel entry. A piece of sterile gauze was placed under this loop. The catheter was gently pulled up to the right shoulder, and the entire length was covered by Tegaderm.
Group II or LECC (n=100) had the epidural catheter threaded through the central eyelet of Lockit fixator device, after its exit from skin. The adhesive on the Lockit device sticks on the skin and the clamp is closed over the catheter.
The epidurals were activated with 3 ml of 1% lignocaine 1 h after the block placement. In case of obstruction to the drug injection, the entire fixation assembly was checked and redone. About 0.5% bupivacaine was given as 6-8 ml bolus through epidural catheter every hour. The parameters recorded were inserted length of the epidural catheter, incidence of needle stick injury, unusual bleeding and catheter snapping during fixation. Patient's comfort during the procedure was evaluated on Likert scale of −2 to +2. These evaluations were performed by an independent observer. The technique of fixation was not revealed to the co-investigator involved in the statistical analysis of the data.
All patients received 0.125% bupivacaine with 1 ug/ml of fentanyl as continuous postoperative epidural infusion with an elastomeric pump (Royal Fornia Medical Equipment Co Ltd). Erythema, induration, inward and outward migration were noted at the time of catheter removal at 72 h after surgery. Migration more than 1 cm was considered significant enough to be reported. During the first 72 h when epidural analgesia was delivered, pain scores were noted every 4 h. A visual analog scale (VAS) of ≥5 was treated with rescue analgesic tramadol 50 mg intravenous.
Data were expressed as mean with standard deviation for continuous variables. Categorical variables were expressed as numbers and percentages. The statistical analysis was performed using Statistical Package for Social Sciences (SPSS, IL, Chicago, version 17.0). Independent samples t-test was applied to continuous variables. The categorical variables such as gender, Likert score, bleeding, kink, VAS score and outward migration were analyzed by Chi-square test. P < 0.05 was considered as statistically significant.
Sample size estimation was done by following the results of the study by Bougher et al.[5] in 82 patients. They have demonstrated tunneling to be effective in 62% and standard fixation in 38% for prevention of catheter migration. G power statistical analysis was applied, considering an α = 0.01, power (1-ß) = 95% and effect size of one. Totally, 95 cases were suggested to be included in each group.
Results
The study was performed in 200 patients posted for various lower limb orthopedic procedures, requiring combined spinal epidural anesthesia. The neuraxial block was successfully placed in the first attempt in 68% patients. The causes of unsuccessful first attempt were obesity (48%), decreased interspinous distance (36%), faulty technique (13%) and kyphoscoliosis (3%), which required ≥2 attempts.
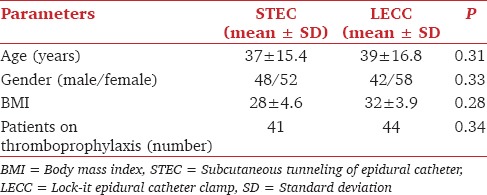
The two groups were comparable with respect to the age and body mass index [Table 1]. The surgeries performed were joint replacements (40%), ilizarov procedures (30%), acetabular fractures (15%) and simultaneous two procedures on lower limbs (15%). About 45% of the patients were receiving preoperative low-molecular-weight heparin for deep vein thrombosis prophylaxis and ASRA guidelines were adhered to for institution of block.
Table 1.
The demographics of the patients enrolled for the study
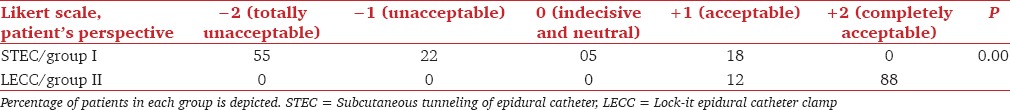
77% patients in STEC group disliked tunneling when specifically enquired by an independent observer in the postoperative ward. The patients who received >2 punctures for initial block citation had negative Likert score. The comparative statistics of Likert score is presented in Table 2 (P = 0.00).
Table 2.
Patient's comfort during epidural fixation - Likert's score
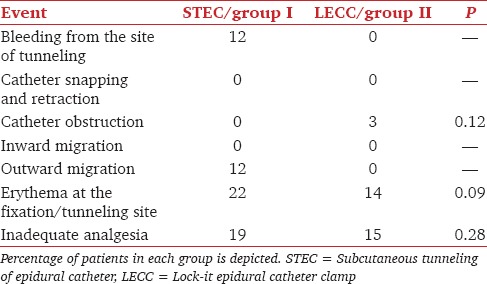
There were three episodes of needle stick injury in STEC group. 9 of the patients with bleeding from the tunneling site were on DVT prophylaxis. The complications are enumerated in Table 3.
Table 3.
Incidence of complications with the two techniques
Discussion
Migration of epidural catheter is a major cause of suboptimal analgesia, and secure fixation is required to prevent catheter dislodgement. The technique should also be operator friendly and comfortable to the patient.
Our study shows that patients were more uncomfortable and nonreceptive toward tunneling procedure. Kumar and Chambers also had similar results.[6] They also outlined the safety concerns, catheter hygiene and daily catheter examination to avoid morbidity from the tunneling procedure, while creating the tunnel. This could have been avoided by the use of needle sheath as a stabilizer to guide the hub of needle.[7]
Burstal et al. have concluded in their review that tunneling decreases the incidence of migration but does not abolish it.[8] LECC has been shown to be 88% successful in preventing the migration, inward as well as outward in a study by Clark et al.[4]
Patients with tunneled catheters in our study showed higher incidence (19%) of poor pain scores with increased requirement of tramadol. This shows that apart from catheter migration, factors such as individual pain threshold and complexity of surgical procedure contribute toward failure of analgesia. Hermanides et al. have reported an incidence of 30% failure in epidural analgesia in clinical practice secondary to incorrect primary catheter placement, subsequent migration after correct initial placement and suboptimal drug dosing.[9] Movement of the catheter at the skin surface does not always translate into the migration of catheter tip inside the epidural space, but does suggest that there has been a displacement of the catheter assembly.[3]
Leaving a loop of catheter on the skin during tunneling was described by Tripathi and Pandey as a strategy to prevent dislodgement.[10] The interposed loop is supposed to dampen the outward traction on the catheter. Their study had a high incidence (29%) of local inflammation at the site of tunneling. There is a possibility of infectious complication with the same epidural needle being used twice.
Snapping of the catheter is a serious complication with the catheter retracting inside the skin. Hobaika has outlined recommendations on the length of catheter to be left in epidural space and indications of surgical retrieval of the catheter fragment.[11] Exploratory laminectomy should be undertaken only if the patient develops signs or symptoms of neurologic changes, if the catheter is inside the subarachnoid space, or whenever the tip of the catheter is emerging out of the skin. In one case report, the catheter had snapped a little away from its point of exit from skin and this was managed as a routine epidural with the filter assembly attached to the severed end.[12]
We experienced three catheter obstructions in group II patients. These patients were morbidly obese with overhanging gluteal fat folds and significant lumbar lordosis. This had resulted in improper contact between skin and device. The Lockit device clamp does not allow any movement of the catheter, once closed. Hence, an improper contact can kink the small portion of catheter in between the skin and the device. The adhesiveness can also be spoiled by excessive perspiration, which explains the accidental removal of the device in one of our patients because of sympathetic overactivity secondary to Cushing's syndrome.
Likert scale is employed in research that employs questionnaires to measure people's attitudes, opinions or perceptions. Although not specific to assess the satisfaction of the patient during a medical intervention, it has been previously employed in anesthetic practice by Baroudi et al.[13] They have validated this five-point scale with −2 to +2 as available scores to quantify the patient's satisfaction after anesthetic exposure comparing different levels of care. Our study had significant numbers of “dislikes” for tunneling. The main complaints were another injection in back after being informed that block is done, the sting of local anesthetic and the painful sensation with Tuohy needle insertion. Two patients in LECC reported a “feeling of something poking into their back” which was equivalent to a dig-in sensation in supine position.
Conclusion
Epidural catheters do migrate despite the best efforts in securing the catheter. However, a patient friendly technique with no additional needle pricks, lesser incidence of erythema and bleeding complications is more appropriate. Lockit epidural device was found to be more efficacious than subcutaneous tunneling in our study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Phillips DC, Macdonald R. Epidural catheter migration during labour. Anaesthesia. 1987;42:661–3. doi: 10.1111/j.1365-2044.1987.tb03096.x. [DOI] [PubMed] [Google Scholar]
- 2.Chadwick VL, Jones M, Poulton B, Fleming BG. Epidural catheter migration: A comparison of tunnelling against a new technique of catheter fixation. Anaesth Intensive Care. 2003;31:518–22. doi: 10.1177/0310057X0303100505. [DOI] [PubMed] [Google Scholar]
- 3.Burns SM, Cowa CM, Barclay PM, Wilkes RG. Intrapartum epidural catheter migration: A comparative study of three dressing applications. Br J Anaesth. 2001;86:565–7. doi: 10.1093/bja/86.4.565. [DOI] [PubMed] [Google Scholar]
- 4.Clark MX, O’Hare K, Gorringe J, Oh T. The effect of the Lockit epidural catheter clamp on epidural migration: A controlled trial. Anaesthesia. 2001;56:865–70. doi: 10.1046/j.1365-2044.2001.02089.x. [DOI] [PubMed] [Google Scholar]
- 5.Bougher RJ, Corbett AR, Ramage DT. The effect of tunnelling on epidural catheter migration. Anaesthesia. 1996;51:191–4. doi: 10.1111/j.1365-2044.1996.tb07714.x. [DOI] [PubMed] [Google Scholar]
- 6.Kumar N, Chambers WA. Tunnelling epidural catheters: A worthwhile exercise? Anaesthesia. 2000;55:625–6. doi: 10.1046/j.1365-2044.2000.01645.x. [DOI] [PubMed] [Google Scholar]
- 7.Rose GL. Subcutaneous catheter tunneling. Reg Anesth Pain Med. 2009;34:379. doi: 10.1097/AAP.0b013e3181ac9d0c. [DOI] [PubMed] [Google Scholar]
- 8.Burstal R, Wegener F, Hayes C, Lantry G. Subcutaneous tunnelling of epidural catheters for postoperative analgesia to prevent accidental dislodgement: A randomized controlled trial. Anaesth Intensive Care. 1998;26:147–51. doi: 10.1177/0310057X9802600203. [DOI] [PubMed] [Google Scholar]
- 9.Hermanides J, Hollmann MW, Stevens MF, Lirk P. Failed epidural: Causes and management. Br J Anaesth. 2012;109:144–54. doi: 10.1093/bja/aes214. [DOI] [PubMed] [Google Scholar]
- 10.Tripathi M, Pandey M. Epidural catheter fixation: Subcutaneous tunnelling with a loop to prevent displacement. Anaesthesia. 2000;55:1113–6. doi: 10.1046/j.1365-2044.2000.01547-2.x. [DOI] [PubMed] [Google Scholar]
- 11.Hobaika AB. Breakage of epidural catheters: Etiology, prevention, and management. Rev Bras Anestesiol. 2008;58:227–33. doi: 10.1590/s0034-70942008000300005. [DOI] [PubMed] [Google Scholar]
- 12.Kishore K, Sahu S, Singh MK, Agarwal A, Singh P. A novel way of managing shearing of epidural catheter during tunnelling. Indian J Anaesth. 2010;54:586. doi: 10.4103/0019-5049.72663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Baroudi DN, Nofal WH, Ahmad NA. Patient satisfaction in anesthesia: A modified Iowa Satisfaction in Anesthesia Scale. Anesth Essays Res. 2010;4:85–90. doi: 10.4103/0259-1162.73513. [DOI] [PMC free article] [PubMed] [Google Scholar]


