Abstract
Objective
To determine what proportion of veterans previously colorectal cancer (CRC) screened with fecal immunochemical testing (FIT) would be willing to undergo a second round of FIT screening.
Methods
Iowa City Veterans Affairs Health Care System patients (< 65, asymptomatic, average risk, overdue for CRC screening) who completed a mailed FIT (4/2011–5/2012) were contacted one year later by telephone to collect demographic and recent CRC screening information, and offered a second mailed FIT if eligible.
Results
Of 204 veterans who completed initial FIT testing, 159 were eligible to participate in a second round of FIT screening; 132 (83%) participated in the telephone survey, and 126 (79%) completed a second annual FIT, with 10 (8%) individuals testing positive. The majority of participants (67%) reported being more likely to take a yearly FIT than a colonoscopy every 10 years. Participants overwhelmingly reported that the FIT was easy to use and convenient (89%), and being likely to complete a mailed FIT each year (97%).
Conclusions
Those willing to take a mailed FIT appear satisfied with this method and willing to do it annually. Population-based or provider-based FIT mailing programs have potential to increase CRC screening in overdue populations.
The most recent U.S. Preventive Services Task Force colorectal cancer (CRC) screening guidelines recommend average-risk adults aged 50–75 receive colonoscopy every ten years, sigmoidoscopy every five years with a mid-interval high sensitivity fecal occult blood test (FOBT) every three years, or annual high sensitivity FOBT or fecal immunochemical testing (FIT).1 Several barriers to colonoscopy, such as distance from healthcare facilities and transportation to and from the facility have been reported.2,3 These issues are particularly relevant to the U.S. Department of Veterans Affairs Health Administration (VHA), as over three million (36%) of enrolled veterans reside in rural areas.4
The VHA recently approved use of FIT, a high-sensitivity FOBT which can be administered at home. Advantages of FIT over guaiac FOBT include higher sensitivity for detection of significant adenomas and CRC, lack of diet or medication restrictions, and the need for only one sample.2,3
We previously demonstrated the effectiveness of an initial mailing of a FIT to eligible patients overdue for CRC screening.2,3 Although annual FIT screening is recommended, little is known regarding patients’ willingness to participate in repeated annual FIT screenings. Therefore, the objective of this study was to determine what proportion of patients, who previously screened negative with FIT, would be willing to complete a second round of annual FIT screening and what proportion would screen positive.
The two FIT mail-out interventions have been described previously.2,3 In the initial two interventions, 232 participants completed a FIT. Twenty-eight (12%) of these participants had positive FITs and were referred for follow-up care, while those who tested negative (n=204) were included in this prospective follow-up study to determine willingness to complete a second annual FIT.
Approximately one year after completing their initial FIT, potentially eligible patients received a recruitment letter explaining the study, followed by a telephone call to assess eligibility and willingness to take a brief survey. Immediately following the survey, participants were asked to take a second annual FIT. Those agreeing were mailed a Polymedco OC FIT-CHEK® kit with instructions and a pre-addressed postage-paid envelope to return the FIT.
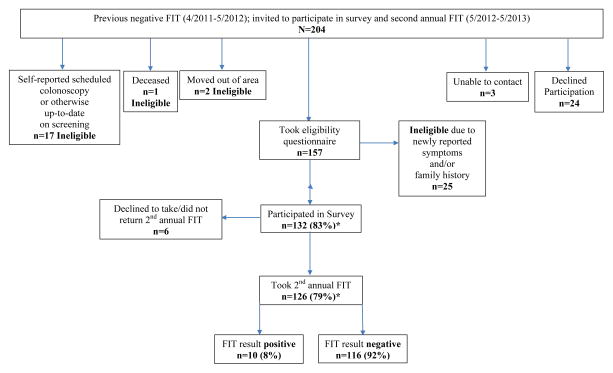
Of those eligible (n=159), 132 (83%) participated in the survey and 126 (79%) returned a second annual FIT. There were 10 (8%) positive FITs, and these patients were referred for follow-up care (Figure 1). Participants overwhelmingly reported the FIT was easy to use and convenient (89%), and they would be likely to complete a mailed FIT each year (97%) (Table 1). There were no significant differences between FIT participants vs. non-participants by age, gender, or rurality (results not shown).
Figure 1.
Study Population, Iowa City VA Health Care System
*Percentage calculated out of total potentially eligible to participate. Out of 204 invited to participate, 45 were found to be ineligible (2 moved out of the area, 1 was deceased, 17 self-reported scheduled colonoscopy or otherwise being up-to date on screening, and 25 reported new symptoms and/or family history on the eligibility questionnaire given prior to the survey), leaving 159 potentially eligible to participate. Three were unable to be contacted and 24 declined participation, and were included in the 159 potentially eligible.
Table 1.
Survey Participant Characteristics and Responses, Iowa City VA Health Care System (n=132)
| Characteristics/Preferences, 2012–2013 | n (%) |
|---|---|
|
| |
| Age in years (mean, SD) | 62 (4) |
|
| |
| Male gender | 122 (92%) |
|
| |
| Rural area of residence | 78 (59%) |
|
| |
| Good/Very Good/Excellent general health | 95 (72%) |
|
| |
| Race | |
| White | 123 (93%) |
| Black | 6 (5%) |
| Other | 3 (2%) |
|
| |
| Health insurance in addition to VHA benefits (could report >1) | |
| Private Individual or Group Plan | 34 (26%) |
| Military | 17 (13%) |
| Medicaid | 8 (6%) |
| Medicare | 31 (23%) |
| VHA benefits only | 65 (49%) |
|
| |
| Highest education level ≥ some college or technical school | 74 (56%) |
|
| |
| Have at least 1 child (≤ 18 years) living in household | 17 (13%) |
|
| |
| More than one adult (>18 years) living in household | 89 (67%) |
|
| |
| Currently Married/Partnered | 77 (58%) |
|
| |
| Participant has someone who can bring to healthcare appointments if needed | 121 (92%) |
|
| |
| Has an additional non-VA primary care provider | 30 (23%) |
|
| |
| Healthcare provider has previously recommended a colonoscopy | 95 (72%) |
|
| |
| Ever had a colonoscopy | 60 (45%) |
|
| |
| Ever had colonoscopy performed at VA facility | 12 (20%) |
|
| |
| Who should make the decision for when you should be screened for colon cancer?a | |
| You alone or mostly you | 21 (16%) |
| The doctor and you equally | 77 (58%) |
| Mostly the doctor or the doctor alone | 33 (25%) |
|
| |
| Who should make the decision for which test should be used for screening?a | |
| You alone or mostly you | 37 (28%) |
| The doctor and you equally | 35 (26%) |
| Mostly the doctor or the doctor alone | 59 (45%) |
|
| |
| More likely to take colonoscopy every 10 years or FIT every year? | |
| FIT | 88 (67%) |
| Colonoscopy | 11 (8%) |
| No preference | 32 (24%) |
| Prefer not to be screened | 1 (1%) |
|
| |
| Preferred method to receive CRC screening due reminders (could report >1) | |
| 110 (83%) | |
| Phone | 55 (42%) |
| 30 (23%) | |
| At clinic visit | 40 (30%) |
| No reminder | 1 (1%) |
|
| |
| Preferred method to receive FIT kit | |
| 120 (91%) | |
| Pick-up at nearest VA facility | 1 (1%) |
| No preference | 11 (8%) |
|
| |
| FIT Satisfaction: Answered ‘extremely’ or ‘very’ to the following: | |
|
| |
| How easy was it for you to follow the FIT kit directions? | 117 (89%) |
|
| |
| How convenient was the FIT kit for you? | 118 (89%) |
|
| |
| If the FIT was mailed to you each year, how likely would you be to complete it each year? | 128 (97%) |
1 missing response
Few studies have examined patients’ willingness to participate in follow-up FITs after their initial screening. In this group of largely rural veterans initially overdue for CRC screening, 79% participated in a second annual mailed FIT. Similarly, a population-based FIT screening program in Amsterdam demonstrated that 85% of participants completed a second biennial mailed FIT.5
Several limitations should be considered when interpreting study results. Due to limited sample size, we were unable to conduct subgroup analyses. Although the original cohort was identified based on regular VHA use, a number of persons (n=17) reported scheduled or up-to-date CRC screens from outside the VHA, which we were unable to verify. Furthermore, this sample of veterans who previously participated in a FIT intervention may not be generalizable to other clinic populations. However, this is one of the few studies to present data on repeated FIT testing in the U.S.
In conclusion, FIT mailing programs appear to be an effective method to provide CRC screening for overdue patients, especially those who face barriers to colonoscopy. Providers should consider offering FIT as an option along with other evidence-based methods.
Acknowledgments
Funding Statement: The research reported here was supported by the Department of Veterans Affairs, Veterans Health Administration, Office of Rural Health, Veterans Rural Health Resource Center-Central Region (VRHRC-CR), and the Veterans Affairs Health Services Research and Development (HSR&D) Service, Center for Comprehensive Access and Delivery Research and Evaluation (CADRE) (CIN 13-412). The views expressed in this article are those of the authors and do not necessarily represent the views or policy of the Department of Veterans Affairs or the United States Government. This work was also supported by the University of Iowa Holden Comprehensive Cancer Center, which is funded in part by NIH/NCI P30 CA086862.
The authors thank Stacy Wittrock and Ashley Cozad for their efforts in coordinating this study. We would also like to acknowledge Lindsey Davenport-Landry in the Iowa City VA laboratory for her work in managing all of the laboratory aspects of this project.
Footnotes
Conflicting and Competing Interests: The authors have no conflicting or competing interests to declare.
References
- 1.United States Preventive Services Task Force. Screening for colorectal cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2008;149:627–637. doi: 10.7326/0003-4819-149-9-200811040-00243. [DOI] [PubMed] [Google Scholar]
- 2.Charlton ME, Mengeling MA, Halfdanarson TR, et al. Evaluation of a Home-Based Colorectal Cancer Screening Intervention in a Rural State. J Rural Health. 2014;303:322–32. doi: 10.1111/jrh.12052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schlichting JA, Mengeling MA, Makki NM, et al. Increasing colorectal cancer screening in an overdue population: participation and cost impacts of adding telephone calls to a FIT mailing program. J Community Health. 2014;39:239–247. doi: 10.1007/s10900-014-9830-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fact Sheet: Information about the VHA Office of Rural Health and Rural Veterans. Washington, DC: Veterans Health Administration, Office of Rural Health; [Accessed December 29, 2014]. [updated May 2014]. Available from: http://www.ruralhealth.va.gov/docs/factsheets/ORH_General_FactSheet_2014.pdf. [Google Scholar]
- 5.Denters MJ, Deutekom M, Bossuyt PM, van Rijn AF, Fockens P, Dekker E. Involvement of previous non-participants cannot fully compensate for lower participation in a second round of FIT-screening. Cancer Epidemiol. 2013;37:330–335. doi: 10.1016/j.canep.2013.01.007. [DOI] [PubMed] [Google Scholar]