Abstract
Objective:
Previous cross-sectional research has shown that depression and problem gambling co-occur. Longitudinal research, however, allows for a better determination of directionality, as behavioural changes in gambling involvement can be more reliably studied over time. Our study assesses symptoms of depression and problem gambling across 4 waves and addresses whether their relation is directional (with one reliably preceding the other), bidirectional, or pathoplastic.
Method:
As part of the Manitoba Longitudinal Study of Young Adults, prospective data were collected on Canadian young adults’ (Wave 1: n = 679, 51.8% female, aged 18 to 20 years) depressive symptoms, involvement in gambling, and risky gambling behaviour. Recruitment and the first cycle of data collection (Wave 1) took place in fall 2007. Three additional waves of data collection then occurred in 12- to 18-month intervals: fall 2008, spring 2010, and spring 2011. The Problem Gambling Severity Index and the Composite International Diagnostic Interview—Short Form were administered through telephone interview at each wave.
Results:
Bivariate growth curves showed that depressive and problem gambling symptoms were positively correlated at Wave 1, Wave 2, and Wave 4. Neither disorder was found to be a risk factor for the other, and depression and problem gambling were not pathoplastically related (that is, increases in one did not result in increases in the other over time, and vice versa).
Conclusions:
While depression and problem gambling are related, their co-occurrence may be better explained not by depressive- or gambling-related risk, but by the presence of a common underlying factor (such as substance abuse).
Keywords: major depressive disorder, problem gambling, emerging adults, longitudinal, comorbid, bi-directional, risk, pathoplastic effect
Abstract
Objectif:
La recherche transversale antérieure a révélé que la dépression et le jeu pathologique sont co-occurrents. Toutefois, la recherche longitudinale permet de mieux déterminer la directionnalité, car les changements comportementaux de la participation au jeu peuvent être étudiés de façon plus fiable avec le temps. La présente étude évalue les symptômes de dépression et de jeu pathologique sur 4 cycles et cherche à déterminer si leur relation est directionnelle (l’une précédant l’autre de façon fiable), bidirectionnelle, ou pathoplastique.
Méthode:
Dans le cadre de l’Étude longitudinale chez les jeunes adultes au Manitoba, des données prospectives ont été recueillies sur les symptômes dépressifs, la participation au jeu et le comportement de jeu à risque des jeunes adultes canadiens (Cycle 1 : N = 679, 51,8 % femmes, 18-20 ans). Le recrutement et le premier cycle de la collecte de données (Cycle 1) ont eu lieu à l’automne de 2007. Trois cycles additionnels de collecte de données se sont ensuite déroulés à 12 à 18 mois d’intervalle : automne de 2008, printemps de 2010, et printemps de 2011. L’Index du jeu excessif et l’entrevue diagnostique composite internationale – version abrégée ont été administrés par entrevue téléphonique à chaque cycle.
Résultats:
Les courbes de croissance bivariée ont indiqué que les symptômes dépressifs et de jeu pathologique étaient positivement corrélés aux Cycles 1, 2, et 4. Aucun trouble n’a été constaté être un facteur de risque pour l’autre, et la dépression et le jeu pathologique n’étaient pas pathoplastiquement reliés (c.-à-d., les augmentations de l’un n’entraînaient pas d’augmentations dans l’autre avec le temps, et vice versa).
Conclusions:
Bien que la dépression et le jeu pathologique soient reliés, leur cooccurrence s’explique peut-être mieux non pas par un risque lié à la dépression et au jeu pathologique, mais par la présence d’un facteur sous-jacent commun (comme l’abus de substances).
Gambling disorder typically originates in young adulthood—a developmental trend demonstrated by elevated problem gambling (PG) risk in college and university samples. About 42% to 85% of students gamble, with 3% to 23% reporting risky weekly gambling patterns.1,2 Compared with other age groups, emerging adults (aged 18 to 25 years)3 gamble more frequently and are more likely to have a gambling disorder. For example, in the general population, lifetime prevalence of gambling disorder is 0.4% to 1.0% and past-year prevalence is 0.2% to 0.3%.4 This compared with elevated on-campus rates. Among American college students, lifetime prevalence of disordered gambling is 6% to 11%.5 In Canada, 6.2% of undergraduates are moderate-risk gamblers and 1.4% have severe PG.6 As such, a critical review concluded that being younger than 29 years of age is a significant risk factor for PG.7 These results also indicate that a propensity for early gambling can develop into PG. The current generation of North American young adults is the first to grow up with exposure to widespread, legalized, government-operated gambling. This increased accessibility and salience may mean likelihood of PG development is also greater.8 A focus on the correlates of gambling involvement in emerging adults (including risk factors and consequences) is therefore warranted.
Depression may be one such risk factor. Almost 38% of risky gamblers exhibit some form of mood disorder.9 More specifically, pathological gamblers are more likely to be depressed (26%, compared with 18% of nonpathological gamblers)10 and lifetime major depressive disorder (MDD) is 3 times more common among participants with lifetime PG than among those without.11 In one Canadian study,12 84% of treatment-seeking adults endorsed a lifetime prevalence of at least 5 pathological gambling symptoms and 80% indicated that they gambled to relieve dysphoria. Another 14% had lifetime MDD, 25% had seen a mental health professional for depression, and 16% had attempted suicide (69% of these participants indicated that their suicidal thoughts were related to their gambling-related problems). MDD and PG have therefore been shown to co-occur. This is clinically significant because, among pathological gamblers seeking treatment, those with a comorbid psychiatric disorder tend to exhibit greater gambling pathology and psychopathology.13
Compared with their nongambling peers, young people with PG also have demonstrably poorer coping skills, lower self-esteem, and are more likely to be depressed and to have previously attempted suicide.5 Further, they are at greater risk for delinquency, academic problems, social problems, and other addictions. These results demonstrate that the co-occurrence of PG and MDD can result in serious negative social and academic consequences.
While these studies support the idea that PG and MDD are associated, they do not tell us how or why they are related. If these disorders are causally related, their association may be explained through 1 of 2 pathways. First, depression may lead to escalations in gambling involvement through maladaptive coping. Jacobs’14 general theory of addictions posits that addictive behaviours, like gambling, are reinforced and maintained by permitting escape from a painful reality. Alternatively, PG’s serious negative consequences may be sufficient to trigger MDD.15 These pathways are not mutually exclusive; a bi-directional relation between PG and MDD may also be operative. Further, the two may be pathoplastically related (an increase in one disorder may result in an increase in the other). Finally, it is also possible that depression and PG are not causally related. Instead, their co-occurrence may be better explained by a third variable.
Our Study
Multi-wave data collected as part of the Manitoba Longitudinal Study of Young Adults (MLSYA) were analyzed. Longitudinal research is particularly helpful for examining gambling antecedents and consequences, as changes in levels of risky gambling can be more reliably studied over time.16 Findings could inform targeted prevention or early intervention approaches.
Hypotheses
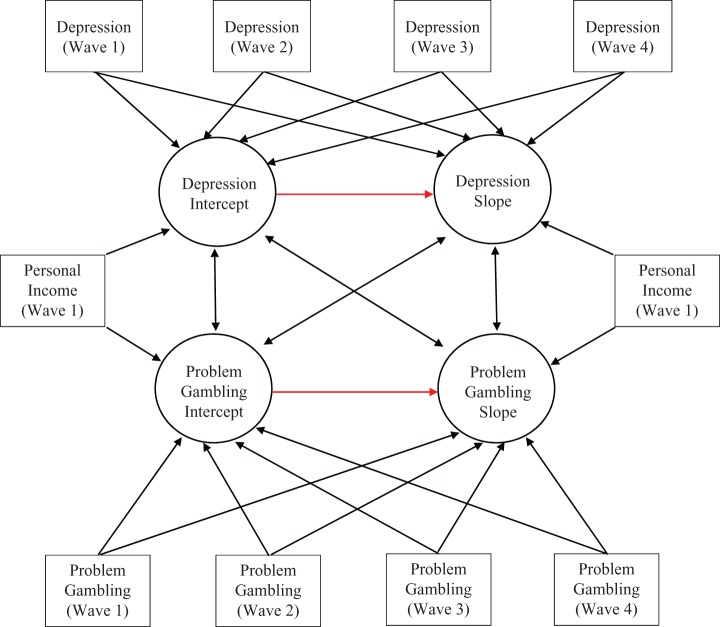
Hypothesis 1 (H1): In accordance with previous literature demonstrating that depressive and PG symptoms are related, it was hypothesized that MDD would be positively correlated with PG at Wave 1. Hypothesis 2 (H2): Based on the theory that depression causes escalations in risky gambling behaviour over time through a maladaptive coping process,14 it was hypothesized that higher levels of Wave 1 MDD symptomology would predict a more pronounced increase in PG symptoms over time. Hypothesis 3 (H3): Based on the theory that PG exacerbates depressive symptoms,15 the reverse was also hypothesized: higher levels of Wave 1 PG involvement would predict a more pronounced increase in MDD symptoms over time. Hypothesis 4 (H4): Finally, pathoplastic effects were predicted (more MDD symptoms would result in more PG symptoms, and vice versa, over time). Figure 1 provides graphical depictions.
Figure 1.
Model of bivariate growth curve hypotheses.
Bivariate growth curve analysis of emotional disorder and gambling symptomology. Rectangles represent measured variables and ovals represent latent intercepts and slopes. Double-headed arrows represent factor loadings.
Income is differentially related to MDD and PG, as it is negatively related to depression and positively related to gambling.15 People with past-year PG with mood disorders are also more likely to have lower incomes.15 As a result, personal income was used as a time-invariant covariate in all analyses.
Method
Sampling Procedures
Ethical approval for this secondary analysis study was granted by the Health Sciences Research Ethics Board at Dalhousie University. Recruitment and the first cycle of data collection took place in fall 2007. Random-digit dialing was primarily used; news releases and informational posters placed within gambling facilities also invited self-referral. Three additional waves of data collection occurred in 12- to 18-month intervals: in fall 2008, spring 2010, and spring 2011.
Participants
At Wave 1, 679 18- to 20-year-olds (mean age 18.92, SD 0.79) were enrolled. Just over one-half (51.8%) were female and most (72.5%) self-identified as being of European descent. In addition to being Canadian, 6.2% of participants were Aboriginal (First Nations or Métis), 6.2% Hispanic, 0.8% White, 0.7% Black, 3.8%, Asian, 0.6% Middle Eastern, and 3.8% reported a primary religious affiliation (Jewish or Mennonite). The majority were single (66.4%) university students (69.8%).
Materials
Depressive Symptoms
A structured interview, the major depressive episode (MDE) subscale of the Composite International Diagnostic Interview—Short Form17 (CIDI-SF), was used to assess MDD symptoms. The MDE subscale (which is aligned with the International Statistical Classification of Diseases and Related Health Problems, 10th Revision,18 and the Diagnostic and Statistical Manual of Mental Disorders (DSM), Third Edition, Revised,19 diagnostic criteria) uses an established diagnostic algorithm and incorporates skip logic.
Participants’ responses to the 7 symptom-related questions were examined: feeling tired, weight changes, trouble sleeping, trouble concentrating, feeling down, thoughts about death, and losing interest. Participants indicated whether they had (1) or had not (0) experienced each symptom. The CIDI-SF17 MDE scale was scored continuously: the 7 depressive item scores were summed to create a 0 to 7 total. Continuous scores were deemed to be more appropriate for this community sample (rather than categorical diagnosis, compared with nondiagnosis scores). They allow a greater symptom range to be examined.20,21
The CIDI-SF17 is psychometrically sound. A comprehensive review indicated that its test–retest reliability (κs = 0.95) and interrater reliability (κs from 0.71) was adequate to excellent.22 Further, 89.6% of MDEs were correctly identified using the CIDI-SF, compared with its longer version.17
Problem Gambling Symptoms
The Problem Gambling Severity Index23 (PGSI), a 9-item subscale of the 31-item Canadian Problem Gambling Index24 (CPGI), was used to assess PG. Developed using the DSM-IV-TR25 and the South Oaks Gambling Screen26 (SOGS) criteria for PG, it assesses the extent to which respondents are engaging in problematic gambling behaviours.
Five items address PG’s diagnostic criteria and 4 address the negative consequences of gambling. Using a 4-point Likert scale ranging from 0 (never) to 3 (almost always), respondents indicated frequency within the last 12 months. The PGSI23 was scored continuously: the scores from all 9 items were summed to form a 0 to 27 total. As with depression, continuous scores were deemed to be more appropriate for our community sample27,28 (compared with categorical nongambler, nonproblem gambler, low risk, moderate risk, and problem gambler scores29).
The PGSI23 total score is internally consistent (α = 0.84). Its test–retest reliability over several days is r = 0.78 and it is correlated highly with both the SOGS26 (r = 0.83) and the DSM-IV25 (r = 0.83) criteria for PG, thereby supporting its criterion validity.
Procedure
At Waves 1 to 4, participants were asked to complete a 2-part survey. The CIDI-SF17 and the CPGI24 were administered by research analysts from the Manitoba Gaming Control Commission and Addictions Foundation Manitoba during a telephone interview. Using skip logic, this survey took between 30 and 45 minutes to complete.
Statistical Analysis
Missing data analyses, tests of normality, and descriptive statistics were conducted in SPSS 20.0 (IBM SPSS Inc, Armonk, NY). After assessing each variable, the appropriate distribution was specified in Mplus 7.1 (Munthen & Munthen, Los Angeles, CA). Univariate latent growth curve models were then tested for both MDD and PG. Time was modelled as linear, with Wave 1 as the intercept (time was coded as 0, 1, 2, and 3 for each of the 4 waves). Next, a bivariate growth curve (Figure 1) was run for MDD and PG. Wave 1 personal income was entered as a time-invariant covariate. We also considered controlling for sex, household income, single status, and/or student status but these predictors were nonsignificant and did not substantially change the interpretation of results when added in. Thus, they are not discussed further.
The bivariate growth curve contained 4 effects of interest: the correlation between intercepts (or Wave 1 MDD and PG); the correlation between the MDD intercept and PG slope, that tests whether MDD is a risk factor for increased PG; the correlation between the PG intercept and MDD slope, that tests whether PG is a risk factor for increased MDD; and the correlation between slopes, that tests whether MDD and PG are pathoplastically related.
Data Cleaning
Data from 679 participants were analyzed. Retention rates were 91.90% (624 participants), 85.12% (578 participants), and 78.06% (530 participants) for Waves 2 to 4, respectively. See Table 1 for the sample size of each variable at each time point. Separate variable Student t tests indicated that data was missing at random; participants endorsing more, early symptoms of MDD and/or PG were more likely to be missing later data. A full information maximum likelihood approach was used to handle all missing data.
Table 1.
Sample descriptive statistics.
| Wave 1 | Wave 2 | Wave 3 | Wave 4 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Mean | SD | n | Mean | SD | n | Mean | SD | n | Mean | SD | |
| Depression | 679 | 0.79 | 1.81 | 624 | 0.85 | 2.32 | 577 | 0.92 | 2.40 | 678 | 0.43 | 1.45 |
| Problem gambling | 601 | 0.97 | 2.01 | 566 | 0.66 | 1.77 | 529 | 0.59 | 1.96 | 487 | 0.41 | 1.48 |
| Personal income | 536 | 10, 495 | 6, 837.55 | |||||||||
N = 679.
Univariate distributions were assessed by examining skewness, kurtosis, and visual plots. At each wave, MDD and PG were substantially positively skewed. To account for this deviation, variables were modelled as negative binomial distributions using the COUNT(nb) command in Mplus 7.1. Robust standard errors were also calculated using the robust maximum likelihood (MLR) estimator.
We also considered categorical, Poisson, and zero-inflated models (the results of which are available on request from the first author). In the categorical model, PG and MDD were dichotomized to indicate disorder presence or absence. However, many participants experienced only a few symptoms of MDD and/or PG, and did not meet full diagnostic criteria. By calculating total scores, symptom counts below this threshold were made meaningful and distinctions in symptom frequency and severity could be more readily made. This method was therefore deemed to be more appropriate for our community sample. Further, the categorical model replicated the results presented below.
Poisson models, which are discrete probability distributions, were also examined. Here, the linear regression predictor is connected to the outcome through a natural logarithmic function.30 Poisson models assume, though, that variance and mean are equal. Type I error30 is increased in instances where the variance exceeds the mean. Because our data were over-dispersed, the Poisson model yielded statistical tests that were too liberal; many previously null pathways became significant. Negative binomial models were therefore deemed to be more appropriate. The standard error is reliably larger, reflecting the additional outcome variance.
Finally, zero-inflated models were considered. Here, zeroes are modelled as a separate process from the Poisson portion of the model.30,31 While potentially appropriate for univariate growth curves, this approach lacks parsimony when used with bivariate models. Adding a zero-inflated component to Figure 1 would have doubled the number of parameters required (because zero- and Poisson-distributed portions are modelled simultaneously). This would have made our model more difficult to interpret. The negative binomial inflated zero model results replicated those reported below. They were therefore excluded to maintain model parsimony. Having concluded that the negative binomial models with robust standard errors were the best fit for the data, we proceeded with this approach as the primary analytic strategy.
Lastly, by converting the Wave 1 personal income values to z scores and using 3.29 as a cut off, it was determined that many univariate outliers existed. At Wave 1, participants were 18 to 20 years old, it is highly unlikely they would have high annual personal incomes. It was assumed the question was misinterpreted and all 21 outliers were deleted. When the outliers were retained or Winsorized, the models failed to converge because the matrix was not positive definite.
Results
Univariate Growth Curves
Before examining the bivariate growth curve, univariate linear growth curves for both variables of interest were modelled. In terms of diagnoses: 16.1%, 12.5%, 13.9%, and 8.3% of participants met MDD criteria and 31.5%, 19.9%, 16.8%, and 10.8% of participants met PG criteria at Waves 1 to 4, respectively. See Table 1 for symptom count means and standard deviations.
Looking first at the univariate growth curve for MDD, the intercept (intercept = –1.69, P < 0.01) and the variability of the intercept (σ = 5.52, P < 0.05) were significant but the slope (slope = –0.58, P = 0.198) and the variability of the slope (σ = 0.13, P = 0.132) were not. This suggests there are between-subject differences in MDD symptoms, with some emerging adults experiencing more symptoms than others at Wave 1, but no within-subject change in symptoms over time.
For PG, the intercept and slope were significant (intercept = –1.17, P < 0.001; slope = –0.84, P < 0.001), suggesting there is systematic change in individual levels of PG symptoms across waves. There was also significant variability in the intercept (σ = 2.50, P < 0.001) and the slope (σ = 0.26, P < 0.001), suggesting on average, some emerging adults experience increased symptoms while others saw a decrease.
Bivariate Growth Curve
The intercept and slope of MDD were uncorrelated; Wave 1 depressive symptoms were unrelated to changes in MDD over time. Neither MDD’s intercept nor its slope was correlated with personal income; Wave 1 income was unrelated to depressive symptoms (both at Wave 1 and over time).
PG’s intercept and slope were positively correlated; greater Wave 1 PG involvement was related to greater escalations in PG over time. The intercept of PG was positively related to personal income; at Wave 1, emerging adults with higher incomes were endorsing greater PG involvement. The slope of PG, however, was uncorrelated with personal income; Wave 1 income was unrelated to changes in PG involvement over time.
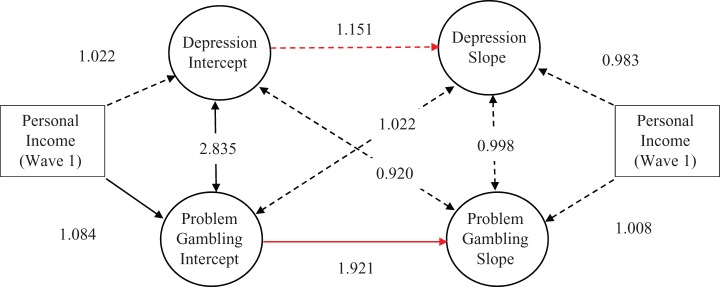
The intercepts of MDD and PG were positively correlated; at Wave 1, emerging adults with greater depressive symptoms were also involved in more PG, and vice versa. The intercept of MDD and the slope of PG were uncorrelated; Wave 1 depressive symptoms were unrelated to changes in PG involvement over time. The intercept of PG and the slope of MDD were also uncorrelated; Wave 1 PG involvement was unrelated to changes in MDD symptomology over time. Finally, the slopes of MDD and PG were uncorrelated; changes in symptoms of one disorder were not associated with changes in symptoms of the other. See Table 2 and Figure 2 for a summary of the bivariate growth curve results.
Table 2.
Depression and problem gambling results.
| β | P | Standard error | Incident rate ratio | 99% CI of incident rate ratio | |
|---|---|---|---|---|---|
| Depression intercept on depression slope | 0.141 | 0.943 | 1.965 | 1.151 | 0.007 to 181.454 |
| Gambling intercept on gambling slopea | 0.653 | <0.001 | 0.123 | 1.921 | 1.402 to 2.635 |
| Depression intercept on gambling slope | –0.083 | 0.751 | 0.262 | 0.920 | 0.469 to 1.808 |
| Gabling intercept on depression slope | 0.022 | 0.952 | 0.370 | 1.022 | 0.394 to 2.651 |
| Depression intercept on gambling intercepta | 1.042 | 0.002 | 0.337 | 2.835 | 1.190 to 6.753 |
| Depression slope on gambling slope | –0.002 | 0.953 | 0.030 | 0.998 | 0.924 to 1.079 |
| Depression intercept on personal income | 0.022 | 0.197 | 0.025 | 1.022 | 0.958 to 1.092 |
| depression slope on personal income | –0.017 | 0.399 | 0.010 | 0.983 | 0.958 to 1.008 |
| Gambling intercept on personal incomea | 0.081 | <0.001 | 0.001 | 1.084 | 1.058 to 1.112 |
| Gambling slope on personal income | 0.008 | 0.288 | 0.006 | 1.008 | 0.993 to 1.022 |
aStatistically significant pathways (P < 0.05).
Figure 2.
Model of depression and problem gambling bivariate growth curve.
Bivariate growth curve analysis of depressive and gambling symptomology. Rectangles represent measured variables and ovals represent latent intercepts and slopes. Double-headed arrows represent factor loadings. Single-headed arrows represent paths. Solid arrows represent statistically significant pathways and dotted arrows represent nonsignificant pathways. Numbers represent incident rate ratios for paths and correlations.
Additional Analyses
In an attempt to better understand the persistence of these findings over time, we re-ran the analyses described above—this time specifying Wave 2, Wave 3, and then Wave 4 as the intercept. In the first, second, and fourth models (when participants were a mean age of 18.92, 19.95, and 22.23 years, respectively), the results held. MDD and PG were consistently positively correlated, but all of the other paths were nonsignificant. This reinforces the reliability of our findings over time. See Table 3 for a summary of the MDD intercept on PG intercept results.
Table 3.
Depression intercept on gambling intercept results at each wave.
| β | P | Standard error | Incident rate ratio | 99% CI of incident rate ratio | |
|---|---|---|---|---|---|
| Wave 1 | 1.042 | 0.002a | 0.337 | 2.835 | 1.190 to 6.753 |
| Wave 1 | 1.570 | <0.001a | 0.305 | 4.807 | 2.190 to 10.444 |
| Wave 3 | 1.924 | 0.440 | 2.492 | 6.848 | 0.011 to 4204.876 |
| Wave 4 | 2.339 | 0.010a | 0.909 | 10.371 | 0.997 to 107.99 |
aStatistically significant pathways (P < .05).
Discussion
At Waves 1, 2, and 4, MDD and PG were positively correlated (which supports H1 and is consistent with previous literature10,11). Within the emerging adult period, MDD and PG therefore tend to co-occur. Contrary to H2 and H3, though, neither disorder was ever a risk factor for the other. Further, MDD and PG were not pathoplastically related, thus failing to support H4. How might these null findings be explained?
It may be that MDD and PG are associated in the short and not the long term. For example, an individual with depression and PG might go to the casino right after a fight with their significant other or might feel blue right after a big loss—not a year later, when our survey was re-administered. Conversely, the MDD-PG relation may be more proximal than our measurement schedule tested. It is also possible that risk is not conferred within the emerging adult period.
Depressive symptoms tend to emerge between ages 13 to 15 years (for both overall rates of MDD and new cases).32 From 15 to 18 years, symptom rates then increase dramatically, before plateauing from 18 to 21 years. These results are consistent with our univariate MDD growth curve, which showed between- but not within-subject symptom change over time. As there was little evidence of improvement or decompensation in depressive symptoms between 18 to 25 years, this age range may have been ill-suited for the longitudinal study of MDD risk factors. It is therefore unsurprising that PG did not increase MDD risk. Likely, its risk factors exert a greater influence earlier in life. One study found that, in males, depression at 17 was linked to depression and gambling at 23. Similarly, gambling was linked to later gambling involvement and depression.33
Conversely, PG is more transitory and episodic. Mid-adolescent gambling involvement leads to gambling problems which may, in turn, predict continuance of adult gambling problems. Alternatively, adolescents may mature out of their gambling problems.34 These results are consistent with our univariate PG growth curve, which showed systematic change in individual symptom levels over time. Intercept and slope variability suggested some emerging adults experienced increased symptoms while others saw a decrease. This systematic and within-person PG change suggest we had a reasonable chance of finding MDD as a risk factor for PG. However, this hypothesis was unsupported by the data. It is therefore possible the co-occurrence of depressive and gambling symptoms at Wave 1 may be better explained not by MDD-related risk but by the presence of a common underlying causal factor.
A systematic meta-analytic review found that, in addition to depression (weighted mean effect size of 23.1%), regular gamblers also experienced high levels of alcohol misuse (28.1%), illicit drug use (17.2%), and nicotine dependence (60.1%).10 The link between MDD and substance use has been clearly established; both are also related to PG involvement. Substance use may therefore be a third variable underlying the MDD-PG relation at Wave 1. For example, in a sample of 1430 undergraduate students, disordered gamblers (i.e., sub-clinical or pathological) exhibited disproportionately higher depression (40.0%, compared with 23.3% in the general population) and problem drinking (81.6%, compared with 28.1% in the general population) comorbidity rates.35 Further, people with a drinking problem were engaging in more gambling (9.0%, compared with 4.2% for the entire sample) and people who were depressed were engaging in more problematic gambling (9.4%, compared with 4.2% for the entire sample).
Limitations
At Wave 1, in fall 2007, participants were aged 18 to 20 years. Three additional waves of data collection occurred in fall 2008, spring 2010, and spring 2011. At Wave 4, participants were aged about 23 to 25 years. As previously discussed, the time frame and/or year-long wave-to-wave gaps may have been inappropriate for the longitudinal study of depressive and gambling risk in emerging adults.
Second, prevalence of depression and PG involvement were low in our sample, despite the use of symptom count scores. However, our use of negative binomial distributions and robust standard errors helps mitigate this limitation. Further, while retention rates were fairly high, more CIDI-SF17 and PGSI23 data were missing over time. Data were missing at random; participants reporting greater, earlier psychopathology or gambling pathology participated less over time. However, maximum likelihood approaches, used here, are among the most effective for handling missing data.36
Finally, our sample was not representative. It is also possible that we did not have a sufficient number of participants, our analyses were underpowered, and our null results were attributable to increased type II error.
Conclusion
The bivariate growth curves supports the co-occurrence of MDD and PG in emerging adults. Therefore, active screening for, and treatment of, co-occurring mental health disorders like depression may be critical for people with PG seeking help. For example, among clinical gamblers seeking treatment, those with a comorbid psychiatric disorder have been shown to exhibit greater severity of both gambling pathology and psychopathology.13 Further, MDD is associated with suicide, and in a sample of 500 people with PG, 48% reported suicide ideation and 13% reported suicide attempts.37 Outpatients with MDD and bipolar disorder with comorbid PG were more than twice as likely to have attempted suicide in the past month as those without.15
Given the co-occurrence of MDD and PG, clinicians should screen for and provide treatment for both disorders. We cannot assume that treating one will resolve the other, as these disorders were unrelated over time. Once common factors underlying the MDD-PG relation are identified, these should be further targeted in preventative interventions. Although people with comorbid disorders tend to have lower psychosocial functioning, treatment has been found to be effective and satisfying regardless of co-occurring disorder frequency.38
Acknowledgements
This study was supported by a Manitoba Gambling Research Program longitudinal grant (awarded to Dr. Stewart and Dr. Mackinnon; MGRP-FR-12-12-14). We thank the organizers of the MLSYA project for the use of their data. Ms. Chinneck is supported through a Joseph-Armand Bombardier Canada Graduate Master’s Scholarship and a Killam Scholarship. The authors have no conflicts of interest to declare.
Footnotes
Authors' Note: This paper was presented at the 24th Annual Department of Psychiatry Research Day, Halifax, Nova Scotia, 2014 October 24.
References
- 1. LaBrie RA, Shaffer HJ, LaPlante DA, et al. Correlates of college student gambling in the United States. J Am Coll Health. 2003;52:53–62. [DOI] [PubMed] [Google Scholar]
- 2. Lesieur HR, Cross J, Frank M, et al. Gambling and pathological gambling among college students. Addict Behav. 1991;16:517–527. [DOI] [PubMed] [Google Scholar]
- 3. Arnett JJ. Emerging adult: a theory of development from the late teens through the twenties. Am Psychol. 2000;55:469–480. [PubMed] [Google Scholar]
- 4. American Psychiatric Association (APA). Diagnostic and statistical manual of mental disorders. 5th ed. Washington (DC): APA; 2013. [Google Scholar]
- 5. Shaffer HJ, Hall MN. Updating and refining meta-analytic prevalence estimates of disordered gambling behavior in the United States and Canada. Can J Public Health. 2001;92:168–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Williams RJ, Connolly D, Wood RT, et al. Gambling and problem gambling in a sample of university students. Journal of Gambling Issues. 2006;16:1–14. [Google Scholar]
- 7. Johansson A, Grant JE, Kim SW, et al. Risk factors for problematic gambling: a critical literature review. J Gambl Stud. 2009;25:67–92. [DOI] [PubMed] [Google Scholar]
- 8. Petry NM. Pathological gambling: etiology, comorbidity, and treatment. Washington (DC): American Psychological Association; 2004. [Google Scholar]
- 9. Lorains F, Cowlishaw S, Thomas S. Prevalence of comorbid disorders in problem and pathological gambling: systematic review and meta-analysis of population surveys. Addiction. 2011;106:490–498. [DOI] [PubMed] [Google Scholar]
- 10. Adbollahnejad MR, Delfabbro P, Denson L. The clustering of psychiatric disorders in high-risk gambling populations. J Gambl Stud. 2013;30;933–947. [DOI] [PubMed] [Google Scholar]
- 11. Petry NM, Stinson FS, Grant BF. Comorbidity of DSM-IV pathological gambling and other psychiatric disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2005;66:564–574. [DOI] [PubMed] [Google Scholar]
- 12. Beaudoin CM, Cox BJ. Characteristics of problem gambling in a Canadian context: a preliminary study using a DSM-IV-based questionnaire. Can J Psychiatry. 1999;44:483–448. [DOI] [PubMed] [Google Scholar]
- 13. Ibanez A, Blanco C, Donahue E, et al. Psychiatric comorbidity in pathological gamblers seeking treatment. Am J Psychiatry. 2001;158:1733–1735. [DOI] [PubMed] [Google Scholar]
- 14. Jacobs D. A general theory of addictions: A new theoretical model. J Gambl Stud. 1986;12:15–31. [Google Scholar]
- 15. Kennedy SH, Welsh BR, Fulton K, et al. Frequency and correlates of gambling problems in outpatients with major depressive disorder and bipolar disorder. Can J Psychiatry. 2010;55:568–576. [DOI] [PubMed] [Google Scholar]
- 16. Little TD, Preacher KJ, Selig JP, et al. New developments in latent variable panel analyses of longitudinal data. ISSBD Bull. 2007;31:357–365. [Google Scholar]
- 17. Kessler RC, Andrews G, Mroczek D, et al. The World Health Organization Composite International Diagnostic Interview Short Form (CIDI-SF). Int J Methods Psychiatr Res. 1998;7:171–185. [Google Scholar]
- 18. World Health Organization (WHO). International statistical classification of diseases and related health problems. 10th ed. Geneva (CH): WHO; 2010. [Google Scholar]
- 19. American Psychiatric Association (APA). Diagnostic and statistical manual of mental disorders. 3rd ed. Text rev Washington (DC): APA; 1987. [Google Scholar]
- 20. Haarasilta L, Marttunen M, Kaprio J, et al. Major depressive episode and physical health in adolescents and young adults: results from a population-based interview survey. Eur J Public Health. 2005;15:489–493. [DOI] [PubMed] [Google Scholar]
- 21. Karsten J Hartman CA, Ormel J, et al. Subthreshold depression based on functional impairment better defined by symptom severity than by number of DSM-IV symptoms. J Affect Disord. 2010;123:230–237. [DOI] [PubMed] [Google Scholar]
- 22. Wittchen HU. Reliability and validity studies of the WHO-Composite International Diagnostic Interview (CIDI): a critical review. J Psychiatr Res. 1994;28:57–84. [DOI] [PubMed] [Google Scholar]
- 23. Wynne H. Introducing the Canadian Problem Gambling Index. Edmonton (AB): Wynne Resources; 2003. [Google Scholar]
- 24. Ferris J, Wynne H. The Canadian Problem Gambling Index: final report. Ottawa (ON): Canadian Centre on Substance Abuse; 2011. [Google Scholar]
- 25. American Psychiatric Association (APA). Diagnostic and statistical manual of mental disorders. 4th ed. Text rev Washington (DC): American Psychiatric Association; 2000. [Google Scholar]
- 26. Lesieur HR, Blume S. The South Oaks Gambling Screen (SOGS): a new instrument for the identification of pathological gamblers. Am J Psychiatry. 1987;144:1184–1188. [DOI] [PubMed] [Google Scholar]
- 27. Dellis A, Sharp C, Hofmeyr A, et al. Criterion-related and construct validity of the Problem Gambling Severity Index in a sample of South African gamblers. S Afr J Psychol. 2014;44:243–257. [Google Scholar]
- 28. Slutske WS, Jackson KM, Sher KJ. The natural history of problem gambling from age 18 to 29. J Abnorm Psychol. 2003;112:263–274. [DOI] [PubMed] [Google Scholar]
- 29. Currie SR, Hodgins DC, Casey DM. Validity of the Problem Gambling Severity Index interpretive categories. J Gambl Stud. 2013;29:311–327. [DOI] [PubMed] [Google Scholar]
- 30. Atkins DC, Baldwin SA, Zheng C, et al. A tutorial on count regression and zero-altered count models for longitudinal substance use data. Psychol Addict Behav. 2013;27:166–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Atkins D, Gallop RJ. Rethinking how family researchers model infrequent outcomes: a tutorial on count regression and zero-inflated models. J Fam Psychol. 2007;21:726–735. [DOI] [PubMed] [Google Scholar]
- 32. Hankin BL, Abramson LY, Moffit TE, et al. Development of depression from preadolescence to young adulthood: emerging gender differences in a 10-year longitudinal study. J Abnorm Psychol. 1998;107:128–140. [DOI] [PubMed] [Google Scholar]
- 33. Dussault F, Brendgen M, Vitaro F, et al. Longitudinal links between impulsivity, gambling problems and depressive symptoms: a transactional model from adolescence to early adulthood. J Child Psychol Psychiatry. 2011;52:130–138. [DOI] [PubMed] [Google Scholar]
- 34. Wanner B, Vitaro F, Carbonneau R, et al. Cross-lagged links among gambling, substance use, and delinquency from mid-adolescence to young adulthood: additive and moderating effects of common risk factors. Psychol Addict Behav. 2009;23:91–104. [DOI] [PubMed] [Google Scholar]
- 35. Martin RJ, Usdan S, Cremeens J, et al. Disordered gambling and co-morbidity of psychiatric disorders among college students: an examination of problem drinking, anxiety, and depression. J Gambl Stud. 2014;30:321–333. [DOI] [PubMed] [Google Scholar]
- 36. Enders CK, Bandalos DL. The relative performance of full information maximum likelihood estimation for missing data in structural equation models. Structural Equation Modelling. 2001;8;430–457. [Google Scholar]
- 37. Frank ML, Lester D, Wexler A. Suicidal behaviour among members of Gamblers Anonymous. J Gambl Stud. 1991;7:249–254. [DOI] [PubMed] [Google Scholar]
- 38. Soberay A, Faragher JM, Barbash M, et al. Pathological gambling, co-occurring disorders, clinical presentations, and treatment outcomes at a university-based counselling clinic. J Gambl Stud. 2014;30:61–69. [DOI] [PubMed] [Google Scholar]