Abstract
Background
Differences in the increase in matrix metalloproteinase (MMP) and decrease in tissue inhibitor of metalloproteinase (TIMP) activity may contribute to the different characteristics observed clinically on decreased intraocular pressure in patients with glaucoma or ocular hypertension. The purpose of this study was to investigate differences in the expression profiles of MMPs and TIMPs induced by the prostaglandin analogs bimatoprost, latanoprost, and tafluprost in human non-pigmented ciliary epithelial cells (HNPCECs).
Methods
HNPCECs were cultured for 24 h with 0, 10, 100, or 1000 μM of the free acid forms of bimatoprost, latanoprost, and tafluprost. We measured the expression levels of MMPs and TIMPs using real-time polymerase chain reaction, and compared the results. Enzyme activities of MMP-2 and −9 in conditioned media were measured by gelatin zymography.
Results
All prostaglandin analogs we examined dose-dependently increased expression levels of MMP-1, −2, −3, −9, and −17, whereas expression levels of TIMP-1 and −2 decreased with increasing concentrations of each analog. Each prostaglandin analog induced different levels of increases in MMPs and decreases in TIMPs.
Conclusions
Unique expression profiles of MMPs and TIMPs induced by bimatoprost, latanoprost, and tafluprost, as shown in HNPCECs, may contribute to clinically different effects on intraocular pressure decreases in patients with glaucoma or ocular hypertension.
Keywords: Human non-pigmented ciliary epithelial cells, Matrix metalloproteinases, Prostaglandin analog, Tissue inhibitor of metalloproteinases
Background
Bimatoprost (amide prodrug of 17-phenyl-PGF2α), latanoprost (ester prodrug of PGF2α), and tafluprost (difluoroprostaglandin derivative of PGF2α) are prostaglandin analogs (PGAs) available for clinical use to lower patients’ intraocular pressure (IOP). Recently, PGAs were approved as a first-line treatment for glaucoma based on their efficacy in lowering IOP, lack of relevant systemic side effects, and requirement for once-daily dosing [1].
The mechanism by which PGAs reduce IOP has been well-studied and is believed to occur by enhancement of uveoscleral outflow due to the regulation of matrix metalloproteinases (MMPs) and resulting remodeling of the extracellular matrix [2–4]. Clinically, we often experience different effects from the different PGAs. Different receptor subtypes for PGAs were proposed, and different PGAs may lower IOP by different mechanisms of action through these different receptor subtypes [5, 6]. However, the precise mechanism through which these PGAs exhibit different effects in individual patients is still unclear. Previous studies reported differential expression of MMPs in the ciliary body or ciliary muscle after bimatoprost, latanoprost, or tafluprost treatment [2–4, 7]. The activity of these endopeptidases is inhibited by endogenous tissue inhibitor of metalloproteinases (TIMPs); thus, the balanced expression of MMPs and TIMPs is important for maintaining homeostasis of the extracellular matrix and for reducing IOP by these PGAs.
Human non-pigmented ciliary epithelial cells (HNPCECs), which comprise the blood-aqueous barrier (BAB), are involved in controlling IOP. HNPCECs secrete aqueous humor. A decrease in aqueous humor secretion occurs in association with uveitis, especially uveitis involving the ciliary body epithelium (iridocyclitis) [8]. We previously showed that TNF-α (tumor necrosis factor-α) promotes the induction of MMPs in HNPCECs, which degrade claudin-1 and occludin, major constituents of tight-junctions between HNPCECs [9]. We found significantly increased permeability of a monolayer of HNPCECs after MMP treatment. We hypothesized that the balance of MMPs and TIMPs that degrade the components of tight junctions in the BAB in HNPCECs modifies the production of aqueous humor, which consequently decreases aqueous secretion and IOP.
In the present study, we measured and compared the expression levels of MMPs and TIMPs in HNPCECs cultured with various concentrations of bimatoprost, latanoprost, or tafluprost. Differences in the increase in MMP and decrease in TIMP activity may contribute to the different characteristics observed clinically on decreased IOP in patients with glaucoma or ocular hypertension.
Methods
Cell culture
HNPCECs were prepared as described previously [9].
Cell treatment
Free-acid forms of bimatoprost, latanoprost, or tafluprost (Cayman Chemical Ann Arbor, MI, USA) were prepared in dimethyl sulfoxide (DMSO) and diluted to experimental concentrations (10, 100, and 1000 μM) with serum-free medium and added to the HNPCECs. The cells were then incubated for 24 h.
RNA isolation and cDNA synthesis
Total cellular RNA was isolated from the HNPCECs, and total RNA was used as a template for cDNA synthesis with random primers as described previously [9].
qPCR
cDNA was synthesized from total RNA (50 ng) for each treatment group. The cDNA served as the template for the real-time quantitative polymerase chain reaction (qPCR) assays. The primer sequences for human MMP-1, −2, −3, and −9 were described previously [9]. The primer sequences were human MMP-17 forward (5′-CACCAAGTGGAACAAGAGGAACCT-3′) and reverse (5′-TGGTAGTACGGCCGCATGATGGAGTGTGCA-3′). The primer sequences for human TIMP-1, and −2 were described previously [9]. The qPCR gene expression results were normalized as described previously [9]. The qPCR reaction was carried out as described previously [9].
Gelatin zymography
Gelatin zymography was performed and gelatinolytic band densities were quantified as described previously [9].
Statistical analysis
Experiments were repeated four times. The results are presented as the mean ± standard deviation (SD). Statistical analyses were performed using an analysis of variance model with Bonferroni’s post hoc test for multiple comparisons. The value measured without PAGs was defined as a control. We used the SAS 9.4 software (SAS Institute, Cary, NC, USA) for all statistical analyses. Differences with P-values < 0.05 were considered significant.
Results
We examined the expression levels of MMPs and TIMPs in cellular extracts from HNPCECs treated with 10, 100, or 1000 μM of bimatoprost, latanoprost, or tafluprost. The qPCR results demonstrated that MMP-1, MMP-2, MMP-3, MMP-9, and MMP-17 mRNA expression levels were dose dependently increased with increasing bimatoprost, latanoprost, or tafluprost concentrations (Fig. 1, Table 1). When the concentrations of the PGAs were 1000 μM, the MMP-1, MMP-2, MMP-3, MMP-9, and MMP-17 expression levels significantly increased compared to the control levels. When the PGA concentration was 100 and 1000 μM, TIMP-1 and TIMP-2 mRNA expression levels in HNPCECs significantly decreased compared to the control levels.
Fig. 1.

Quantitative PCR shows gene expression of matrix metalloproteinases (MMPs) and tissue inhibitor of metalloproteinases (TIMPs) in human non-pigmented ciliary epithelial cells (HNPCECs). MMP-1, MMP-2, MMP-3, MMP-9, and MMP-17 mRNA levels were up-regulated in the presence of increasing concentrations of each prostaglandin analog. TIMP-1 and TIMP-2 mRNA levels were down-regulated in the presence of increasing concentrations of each prostaglandin analog. Expression without prostaglandin analog was used as a control. B: bimatoprost, L: latanoprost, T: tafluprost. Data represent the mean ± SD (n = 4). *P < 0.05, **P < 0.01, ***P < 0.001 vs. control; one-way analysis of variance with Bonferroni’s correction
Table 1.
Comparison with control group
| Response | Drug | Dose | Mean | SD | P |
|---|---|---|---|---|---|
| MMP-1 | B | 10 | 1.9 | 0.4 | 0.044 |
| B | 100 | 5.0 | 0.6 | <0.001 | |
| B | 1000 | 8.4 | 0.6 | <0.001 | |
| L | 10 | 2.0 | 0.5 | 0.018 | |
| L | 100 | 2.7 | 0.4 | <0.001 | |
| L | 1000 | 7.8 | 0.7 | <0.001 | |
| T | 10 | 3.0 | 0.3 | 0.273 | |
| T | 100 | 4.6 | 2.9 | 0.023 | |
| T | 1000 | 11.2 | 2.3 | <0.001 | |
| MMP-2 | B | 10 | 7.5 | 0.6 | 0.501 |
| B | 100 | 23.1 | 4.5 | 0.002 | |
| B | 1000 | 92.5 | 14.2 | <0.001 | |
| L | 10 | 5.5 | 0.6 | 0.100 | |
| L | 100 | 12.7 | 3.4 | <0.001 | |
| L | 1000 | 41.2 | 5.2 | <0.001 | |
| T | 10 | 3.6 | 0.6 | 0.706 | |
| T | 100 | 14.4 | 3.0 | <0.001 | |
| T | 1000 | 30.5 | 6.4 | <0.001 | |
| MMP-3 | B | 10 | 8.9 | 0.9 | 1.000 |
| B | 100 | 14.9 | 3.8 | 0.604 | |
| B | 1000 | 234.0 | 34.7 | <0.001 | |
| L | 10 | 4.2 | 0.8 | 1.000 | |
| L | 100 | 6.1 | 0.7 | 0.432 | |
| L | 1000 | 69.8 | 10.9 | <0.001 | |
| T | 10 | 11.4 | 2.2 | 0.030 | |
| T | 100 | 31.6 | 5.8 | <0.001 | |
| T | 1000 | 63.3 | 9.2 | <0.001 | |
| MMP-9 | B | 10 | 2.3 | 0.3 | 1.000 |
| B | 100 | 11.5 | 1.6 | 0.001 | |
| B | 1000 | 45.8 | 5.7 | <0.001 | |
| L | 10 | 10.6 | 1.9 | 0.019 | |
| L | 100 | 17.0 | 2.5 | <0.001 | |
| L | 1000 | 86.2 | 8.9 | <0.001 | |
| T | 10 | 6.5 | 0.6 | <0.001 | |
| T | 100 | 9.8 | 0.9 | <0.001 | |
| T | 1000 | 12.6 | 2.1 | <0.001 | |
| MMP-17 | B | 10 | 3.9 | 2.2 | 1.000 |
| B | 100 | 63.2 | 13.4 | 0.006 | |
| B | 1000 | 176.5 | 47.9 | <0.001 | |
| L | 10 | 2.3 | 1.1 | 1.000 | |
| L | 100 | 4.9 | 1.7 | 1.000 | |
| L | 1000 | 173.1 | 74.7 | <0.001 | |
| T | 10 | 4.8 | 1.7 | 0.105 | |
| T | 100 | 8.8 | 1.7 | 0.002 | |
| T | 1000 | 18.5 | 4.8 | <0.001 | |
| TIMP-1 | B | 10 | 67.6 | 8.3 | <0.001 |
| B | 100 | 49.8 | 6.7 | <0.001 | |
| B | 1000 | 39.2 | 5.2 | <0.001 | |
| L | 10 | 71.0 | 10.2 | <0.001 | |
| L | 100 | 61.3 | 11.9 | <0.001 | |
| L | 1000 | 31.3 | 6.5 | <0.001 | |
| T | 10 | 85.9 | 11.5 | 0.038 | |
| T | 100 | 48.1 | 6.3 | <0.001 | |
| T | 1000 | 30.0 | 8.7 | <0.001 | |
| TIMP-2 | B | 10 | 89.2 | 10.8 | 0.082 |
| B | 100 | 50.2 | 7.5 | <0.001 | |
| B | 1000 | 49.6 | 5.3 | <0.001 | |
| L | 10 | 66.7 | 11.6 | <0.001 | |
| L | 100 | 49.7 | 7.1 | <0.001 | |
| L | 1000 | 29.0 | 6.6 | <0.001 | |
| T | 10 | 72.2 | 9.1 | <0.001 | |
| T | 100 | 62.4 | 6.2 | <0.001 | |
| T | 1000 | 30.1 | 4.6 | <0.001 |
P one-way ANOVA with Bonferroni’s post hoc test for multiple comparisons
B bimatoprost, L latanoprost, T tafluprost
Dose: μM
We performed gelatin zymography to measure the enzymatic activity of MMP-2 and MMP-9 in HNPCECs treated with 10, 100, or 1000 μM bimatoprost, latanoprost, or tafluprost (Fig. 2). MMP-2 and MMP-9 controls were used to identify the location of each band (Fig. 2, arrowheads). We detected active MMP-2 forms, but not pro-MMP-9 or pro-MMP-2 forms. We performed a quantitative analysis of the band densities to evaluate active MMP-2 activity in HNPCECs treated with 10, 100, or 1000 μM of bimatoprost, latanoprost, or tafluprost. When the band density of active MMP-2 in HNPCECs treated with 1000 μM bimatoprost was defined as 100, the relative band densities of active MMP-2 in HNPCECs treated with 100 and 1000 μM latanoprost and tafluprost were calculated as 18 and 63 and 31 and 47, respectively. No band was detected in HNPCECs treated with 10 and 100 μM bimatoprost or 10 μM latanoprost and tafluprost. The relative mRNA expression levels of MMP-2 in HNPCECs treated with 1000 μM bimatoprost and with 100 or 1000 μM latanoprost or tafluprost were calculated as 100:14:45:16:33, respectively (Fig. 1), and this relationship appeared similar to the relative band densities of activeMMP-2 in HNPCECs analyzed by gelatin zymography.
Fig. 2.
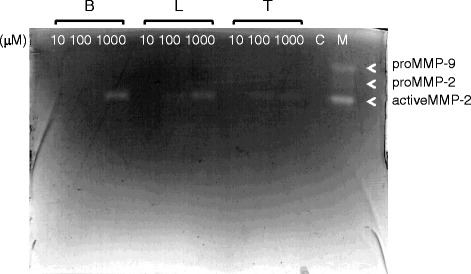
Gelatin zymogram showing the band densities of MMP-2 and MMP-9. Only bands of activeMMP-2 were detected after treatment with the prostaglandin analogs. No bands were detected without treatment (control lane). Samples containing 20 μg of protein were analyzed. B: bimatoprost, L: latanoprost, T: tafluprost. C: control, M: molecular weight marker. Molecular weights of proMMP-9, proMMP-2, and activeMMP-2 are 92 kDa, 72 kDa, and 62 kDa, respectively
Discussion
Previous studies showed that PGAs induce expression of MMP-1, −2, −3, −9, and −17 and TIMP-1 and −2 in the human ciliary body [7, 10–15]. Here, we investigated the expression levels of MMPs and TIMPs in HNPCECs cultured with various concentrations of bimatoprost, latanoprost, or tafluprost, demonstrating different profiles with respect to increases in MMP and decrease in TIMP expression by each PGA.
Each PGA elicited a unique MMP and TIMP expression profile in HNPCECs. At a concentration of 1000 μM, bimatoprost induced greater expression of MMP-2 and MMP-3 than latanoprost and tafluprost. Bimatoprost has a greater effect on lowering IOP than latanoprost [16, 17]. The ability of PGAs to lower IOP may involve MMP-2 and −3. At a concentration of 1000 μM, tafluprost and latanoprost increased the expression MMP-1 and MMP-9, respectively, more than bimatoprost. Some reports showed no significant difference between bimatoprost and latanoprost [18, 19]. Furthermore, Alm showed no clinically significant difference in efficacy between latanoprost and tafluprost [18]. The MMP and TIMP expression profiles of each PGA may be different in individual patients. Thus, the decrease IOP by PGAs may be determined by several diverse factors.
The ratio of infiltration of each PGA from the ophthalmic solution into the aqueous humor and the concentration of each PGA may be essential for the efficacy of each agent. We investigated PGAs at 10, 100, and 1000 μM, concentrations intentionally ranged within those of commercial ophthalmic solutions. In clinical use, 0.03 % bimatoprost, 0.005 % latanoprost, and 0.0015 % tafluprost ophthalmic solutions are available, corresponding to 720 μM, 110 μM, and 33 μM, respectively. The concentration of each PGA in the aqueous humor is lower than that in the ophthalmic solution. In an in vitro study, peak aqueous concentrations after topical administration were 0.009 μg/ml, 0.028 μg/ml, and 0.00875 μg/ml, respectively [20–22], with each concentration corresponding to 22 nM, 65 nM, and 19 nM for bimatoprost, latanoprost, and tafluprost, respectively. The relative infiltration ratios of bimatoprost, latanoprost, and tafluprost from ophthalmic solutions into the aqueous humor are calculated as 1.00:19.3:18:8, respectively. This suggests a more favorable infiltration ratio of the ester prodrugs latanoprost and tafluprost than the free acid form of bimatoprost.
To measure the MMP and TIMP expression levels in HNPCECs in the present study, we did not use the ester prodrugs of latanoprost and tafluprost, but rather used the free acid forms to avoid differences in efficacy owing to hydrolysis by esterases. We obtained scattered MMP and TIMP expression levels when the ester forms of latanoprost and tafluprost were used in the experiments. The varying efficacy of PGAs due to hydrolysis by esterases in the cornea, depending on levels expressed in each patient, may consequently determine the effectiveness of latanoprost and tafluprost.
Our results showed a consistency in the expression levels of MMP-2 mRNA and MMP-2 enzyme activity as measured by qPCR and gelatin zymography, respectively. On the other hand, we did not detect other MMP bands by gelatin zymography, possibly because the levels were beyond the sensitivity of the assay. As a consequence, we estimated the enzymatic level of the other MMPs by the mRNA levels of each MMP.
Claudin-1 and occludin in HNPCECs and non-pigmented ciliary epithelial cells, which comprise the BAB in the uvea, are candidate substrates of MMPs. We previously showed that MMP-1, MMP-3, and MMP-9 degraded claudin-1 and occludin in HNPCECs and in non-pigmented ciliary epithelial cells of a swine ciliary body and showed increased expression of MMP-1, MMP-3, and MMP-9 in the presence of TNF-α in HNPCECs [9]. Interestingly MMP-17 can activate TNF-α [23]. These data suggest that inflammation in the ciliary body, like in iridocyclitis, may be involved in the reduction of IOP.
Fibrillin-1, versican, and hyaluronan (FiVerHy) in the ciliary nonpigmented epithelium are other candidate substrates of MMPs expressed in HNPCECs [24]. Versican was digested by MMP-3 [25], and fibrillin-1 was digested by MMP-2 and MMP-9 [26]. The increased expression levels of MMP-2, MMP-3, and MMP-9 in HNPCECs induced by PGAs may lead the degradation of the physiological complex of FiVerHy in the ciliary nonpigmented epithelium. The precise function of FiVerHy is still unknown, but the dense localization of hyaluronan in this high molecular complex on the surface of the ciliary nonpigmented epithelium may exhibit a protective effect of the ciliary nonpigmented epithelium from the MMPs in the vitreous humor [27–30], and the destruction of FiVerHy by MMPs may induce mild iridocyclitis.
Conclusion
In conclusion, unique expression profiles of MMPs and TIMPs induced by bimatoprost, latanoprost, and tafluprost, as shown in HNPCECs, may contribute to clinically different effects on intraocular pressure decreases in patients with glaucoma or ocular hypertension. This information may be important in the selection of the best PGA for individual patients.
Availability of materials and methods
The dataset supporting the conclusions of this article is available in the repository: https://mynotebook.labarchives.com/share_attachment/BLT%2520data/MTkuNXwxNjc1NTEvMTUtMi9UcmVlTm9kZS80MDg0NzExOTY0fDQ5LjU=
Acknowledgement
This study was supported by Strategic Research Foundation Grant-Aided Project for Private Universities from the Ministry of Education, Culture, Sports, Science, and Technology, Japan (MEXT), 2011–2015 (S1101027).
Abbreviations
- BAB
blood-aqueous barrier
- DMSO
dimethyl sulfoxide
- FBS
fetal bovine serum
- FiVerHy
fibrillin-1, versican, and hyaluronan
- HNPCEC
human non-pigmented ciliary epithelial cell
- IOP
intraocular pressure
- MMP
matrix metalloproteinase
- PGA
prostaglandin analog
- TIMP
tissue inhibitor of metalloproteinase
- TNF
tumor necrosis factor
Footnotes
Competing interests
The authors declare that they have no competing interest.
Authors’ contributions
HY was responsible for, collection of data, analysis and interpretation of results and wrote the first draft of the manuscript. MY participated in its design and supervised the experiments. MG performed the statistical analysis. TK was involved in data collection. MZ conceived the study. All authors reviewed and approved the final manuscript.
Contributor Information
Hiroshi Yamada, Email: h25yam@hotmail.com.
Masahiko Yoneda, Email: yoneda@nrs.aichi-pu.ac.jp.
Masahiko Gosho, Email: masagosho@gmail.com.
Tomohiro Kato, Email: tomo.juventus@gmail.com.
Masahiro Zako, Phone: +81 52264 4811, Email: zako@aichi-med-u.ac.jp.
References
- 1.Winkler NS, Fautsch MP. Effects of prostaglandin analogues on aqueous humor outflow pathways. J Ocul Pharmacol Ther. 2014;30:102–9. doi: 10.1089/jop.2013.0179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Toris CB, Gabelt BT, Kaufman PL. Update on the mechanism of action of topical prostaglandins for intraocular pressure reduction. Surv Ophthalmol. 2008;53:S107–20. doi: 10.1016/j.survophthal.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ooi YH, Oh DJ, Rhee DJ. Effect of bimatoprost, latanoprost, and unoprostone on matrix metalloproteinases and their inhibitors in human ciliary body smooth muscle cells. Invest Ophthalmol Vis Sci. 2009;50:5259–65. doi: 10.1167/iovs.08-3356. [DOI] [PubMed] [Google Scholar]
- 4.Woodward DF, Wang JW, Poloso NJ. Recent progress in prostaglandin F2α ethanolamide (prostamide F2α) research and therapeutics. Pharmacol Rev. 2013;65:1135–47. doi: 10.1124/pr.112.007088. [DOI] [PubMed] [Google Scholar]
- 5.Woodward DF, Regan JW, Lake S, Ocklind A. The molecular biology and ocular distribution of prostanoid receptors. Surv Ophthalmol. 1997;41:S15–21. doi: 10.1016/S0039-6257(97)80003-3. [DOI] [PubMed] [Google Scholar]
- 6.Ishida N, Odani-Kawabata N, Shimazaki A, Hara H. Prostanoids in the therapy of glaucoma. Cardiovasc Drug Rev. 2006;24:1–10. doi: 10.1111/j.1527-3466.2006.00001.x. [DOI] [PubMed] [Google Scholar]
- 7.Oh DJ, Martin JL, Williams AJ, Peck RE, Pokorny C, Russell P, Birk DE, Rhee DJ. Analysis of expression of matrix metalloproteinases and tissue inhibitors of metalloproteinases in human ciliary body after latanoprost. Invest Ophthalmol Vis Sci. 2006;47:953–63. [DOI] [PubMed]
- 8.Gablet B, Kiland JA, Tian B, Kaufman PL, Aqueous humor: Secretion and dynamics. Kiel JW. Physiology of the eye and visual system. In: Tasman W, Jaeger EA, editors. Duane’s ophthalmology on CD-ROM. 2006. Philadelphia: Lippincott Williams & Wilkins; 2006. [Google Scholar]
- 9.Yamada H, Yoneda M, Inaguma S, Watanabe D, Banno S, Yoshikawa K, Mizutani K, Iwaki M, Zako M. Infliximab counteracts tumor necrosis factor-α-enhanced induction of matrix metalloproteinases that degrade claudin and occludin in non-pigmented ciliary epithelium. Biochem Pharmacol. 2013;85:1770–82. [DOI] [PubMed]
- 10.Oh DJ, Martin JL, Williams AJ, Russell P, Birk DE, Rhee DJ. Effect of latanoprost on the expression of matrix metalloproteinases and their tissue inhibitors in human trabecular meshwork cells. Invest Ophthalmol Vis Sci. 2006;47:3887–95. doi: 10.1167/iovs.06-0036. [DOI] [PubMed] [Google Scholar]
- 11.Weinreb RN, Kashiwagi K, Kashiwagi F, Tsukahara S, Lindsey JD. Prostaglandins increase matrix metalloproteinase release from human ciliary smooth muscle cells. Invest Ophthalmol Vis Sci. 1997;38:2772–80. [PubMed] [Google Scholar]
- 12.Ocklind A. Effect of latanoprost on the extracellular matrix of the ciliary muscle. A study on cultured cells and tissue sections. Exp Eye Res. 1998;67:179–91. doi: 10.1006/exer.1998.0508. [DOI] [PubMed] [Google Scholar]
- 13.el-Shabrawi Y, Eckhardt M, Berghold A, Faulborn J, Auboeck L, Mangge H, Ardjomand N. Synthesis pattern of matrix metalloproteinases (MMPs) and inhibitors (TIMPs) in human explant organ cultures after treatment with latanoprost and dexamethasone. Eye (Lond). 2000;14:375–83. [DOI] [PubMed]
- 14.Lindsey JD, Kashiwagi K, Boyle D, Kashiwagi F, Firestein GS, Weinreb RN. Prostaglandins increase proMMP-1 and proMMP-3 secretion by human ciliary smooth muscle cells. Curr Eye Res. 1996;15:869–75. doi: 10.3109/02713689609017628. [DOI] [PubMed] [Google Scholar]
- 15.Anthony TL, Lindsey JD, Weinreb RN. Latanoprost’s effects on TIMP-1 and TIMP-2 expression in human ciliary muscle cells. Invest Ophthalmol Vis Sci. 2002;43:3705–11. [PubMed] [Google Scholar]
- 16.Simmons ST, Dirks MS, Noecker RJ. Bimatoprost versus latanoprost in lowering intraocular pressure in glaucoma and ocular hypertension: results from parallel-group comparison trials. Adv Ther. 2004;21:247–62. doi: 10.1007/BF02850157. [DOI] [PubMed] [Google Scholar]
- 17.Noecker RS, Dirks MS, Choplin NT, Bernstein P, Batoosingh AL, Whitcup SM, Bimatoprost/Latanoprost Study Group. A six-month randomized clinical trial comparing the intraocular pressure-lowering efficacy of bimatoprost and latanoprost in patients with ocular hypertension or glaucoma. Am J Ophthalmol. 2003;135:55–63. [DOI] [PubMed]
- 18.Alm A. Latanoprost in the treatment of glaucoma. Clin Ophthalmol. 2014;8:1967–85. doi: 10.2147/OPTH.S59162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Parrish RK, Palmberg P, Sheu WP, XLT Study Group A comparison of latanoprost, bimatoprost, and travoprost in patients with elevated intraocular pressure: a 12-week, randomized, masked-evaluator multicenter study. Am J Ophthalmol. 2003;135:688–703. doi: 10.1016/S0002-9394(03)00098-9. [DOI] [PubMed] [Google Scholar]
- 20.Fukano Y, Odani-Kawabata N, Nakamura M, Kawazu K. Intraocular penetration and intraocular pressure-lowering effect of new formulation 0.0015 % tafluprost ophthalmic solution with reduced benzalkonium chloride. Atarashii Ganka. 2010;27:691–4. [Google Scholar]
- 21.Camras CB, Toris CB, Sjoquist B, Milleson M, Thorngren JO, Hejkal TW, Patel N, Barnett EM, Smolyak R, Hasan SF, Hellman C, Meza JL, Wax MB, Stjernschantz J. Detection of the free acid of bimatoprost in aqueous humor samples from human eyes treated with bimatoprost before cataract surgery. Ophthalmology. 2004;111:2193–8. [DOI] [PubMed]
- 22.Sjöquist B, Stjernschantz J. Ocular and systemic pharmacokinetics of latanoprost in humans. Surv Ophthalmol. 2002;47:S6–12. doi: 10.1016/S0039-6257(02)00302-8. [DOI] [PubMed] [Google Scholar]
- 23.English WR, Puente XS, Freije JM, Knauper V, Amour A, Merryweather A, Lopez-Otin C, Murphy G. Membrane type 4 matrix metalloproteinase (MMP17) has tumor necrosis factor-alpha convertase activity but does not activate pro-MMP2. J Biol Chem. 2000;275:14046–55. [DOI] [PubMed]
- 24.Ohno-Jinno A, Isogai Z, Yoneda M, Kasai K, Miyaishi O, Inoue Y, Kataoka T, Zhao JS, Li H, Takeyama M, Keene DR, Sakai LY, Kimata K, Iwaki M, Zako M. Versican and fibrillin-1 form a major hyaluronan-binding complex in the ciliary body. Invest Ophthalmol Vis Sci. 2008;49:2870–7. [DOI] [PubMed]
- 25.Muir EM, Adcock KH, Morgenstern DA, Clayton R, von Stillfried N, Rhodes K, Ellis C, Fawcett JW, Rogers JH. Matrix metalloproteases and their inhibitors are produced by overlapping populations of activated astrocytes. Brain Res Mol Brain Res. 2002;100:103–17. [DOI] [PubMed]
- 26.Ashworth JL, Murphy G, Rock MJ, Sherratt MJ, Shapiro SD, Shuttleworth CA, Kielty CM. Fibrillin degradation by matrix metalloproteinases: implications for connective tissue remodelling. Biochem J. 1999;340:171–81. [PMC free article] [PubMed]
- 27.Takeyama M, Yoneda M, Takeuchi M, Isogai Z, Ohno-Jinno A, Kataoka T, Li H, Sugita I, Iwaki M, Zako M. Increase in matrix metalloproteinase-2 level in the chicken retina after laser photocoagulation. Lasers Surg Med. 2010;42:433–41. [DOI] [PubMed]
- 28.Vaughan-Thomas A, Gilbert SJ, Duance VC. Elevated levels of proteolytic enzymes in the aging human vitreous. Invest Ophthalmol Vis Sci. 2000;41:3299–304. [PubMed] [Google Scholar]
- 29.De La Paz MA, Itoh Y, Toth CA, Nagase H. Matrix metalloproteinases and their inhibitors in human vitreous. Invest Ophthalmol Vis Sci. 1998;39:1256–60. [PubMed] [Google Scholar]
- 30.Plantner JJ, Smine A, Quinn TA. Matrix metalloproteinases and metalloproteinase inhibitors in human interphotoreceptor matrix and vitreous. Curr Eye Res. 1998;17:132–40. doi: 10.1076/ceyr.17.2.132.5610. [DOI] [PubMed] [Google Scholar]


