Abstract
Male circumcision is highly protective against urinary tract infections, inflammatory conditions of the penis, sexually transmitted infections, and urogenital cancers. We aimed to reintroduce newborn male circumcision through the creation of a training program in Port-au-Prince, Haiti—an area with a considerable burden of preventable urogenital infections, sexually transmitted infections, and low circumcision rate—after an earlier study reported that a majority of Haitian medical providers were in need of and wanted newborn circumcision training. The program was conducted at the GHESKIO Health Centers, a large, non-governmental clinic offering comprehensive pediatric and adult health services. Two Haitian obstetricians and seven nurses learned circumcision procedures. On training completion, one of two obstetricians achieved surgical competence. Introduction of a newborn male circumcision training program was feasible, achieving an acceptable rate of procedural competency and high-quality services. Permanent resources now exist in Haiti to train additional providers to perform newborn male circumcisions.
Keywords: circumcision, global health, HIV/AIDS, Haiti, general pediatrics
Background
Male circumcision is a highly effective medical procedure that is protective against various medical conditions including urinary tract infections, inflammatory conditions of the penis, sexually transmitted infections—such as those caused by human papillomaviruses, herpes simplex virus type 2, and human immunodeficiency virus (HIV)—and urogenital cancers.1-7 Recently, the US Centers for Disease Control and the American Academy of Pediatrics concluded that the health benefits of newborn male circumcision outweighed the risks.8,9 Male circumcision has been found to reduce the susceptibility to heterosexually acquired HIV infection by over 60%.10-12 Newborn male circumcision only requires a safe, rapid, one-time intervention and has been reported to be not only highly cost-effective but also cost saving.13
In a study of Haitian immigrants in the Dominican Republic, it was reported that a majority of the Haitian men were willing to be circumcised if the procedure was offered to them after learning about the medical benefits.14 A recent survey of medical professionals in Haiti found that Haitian medical providers have positive opinions and good knowledge of newborn male circumcision with strong willingness to provide the service, if trained. A large majority of the participants of the survey needed and wanted newborn male circumcision training, with few providers having prior experience with newborn male circumcision.15
Here we report the results of a “train-the-trainers” program, a rapid training and implementation program for newborn male circumcision at the GHESKIO Health Centers in Haiti. Our aim was to help reintroduce newborn male circumcision through the creation of a permanent newborn male circumcision training program in Port-au-Prince, Haiti—an area with a considerable burden of preventable urogenital infections, sexually transmitted infections, and low circumcision rate.14,16-19
Methods
Program Design and Participants
The training was performed at the GHESKIO Health Centers in Port-au-Prince, Haiti. The GHESKIO Health Centers is a large, non-governmental clinic offering comprehensive pediatric and adult health services. The GHESKIO Health Centers treats urban patients infected with HIV and continues to address infectious diseases through service, training, and research.20 Their history, strong urban infrastructure, and large patient pool made them an ideal site to introduce the newborn male circumcision training program to create a sustainable, accessible circumcision training and service center in Haiti.
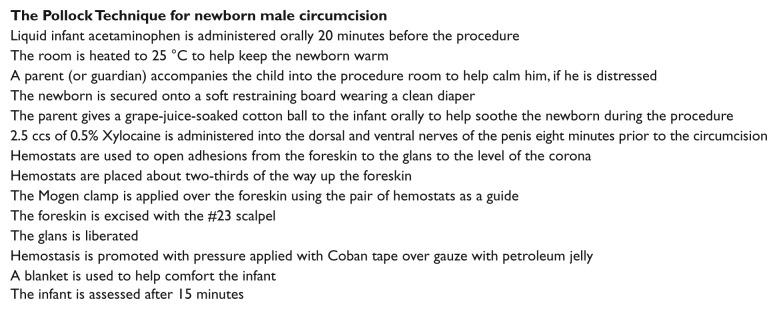
Circumcisions were scheduled for newborns whose mothers were receiving obstetrical and gynecological care from the GHESKIO Health Centers. Inclusion criteria, exclusion criteria, and contraindications for newborn male circumcision are listed in Figure 1. Parents (or guardians) were informed about the risks, benefits, and alternatives to the procedure; observed a 20-minute educational video (available from the authors on request); and provided written documentation of consent. Newborns received physical examinations and tests for HIV status, syphilis status, bleeding time (Duke TS test), and clotting time (Lee and White test).21,22 HIV status was assessed with the Determine HIV-1/2 test (Alere Inc, Waltham, MA). If the test was positive, the newborn was retested with a colloidal gold anti-HIV Antibody Diagnostic Kit (Beijing Wantai Biological Pharmacy Enterprise Co, Ltd, Beijing, China). Syphilis status was tested with the SD Bioline Syphilis 3.0 test (Standard Diagnostics, Giheung-gu, Korea). If the test was positive, the newborn was retested with a Biotec RPR test kit (BIOTEC Laboratories Ltd, Suffolk, UK).
Figure 1.
Newborn male circumcision inclusion criteria, exclusion criteria, and contraindications, GHESKIO Health Centers, Haiti, 2014-2015.
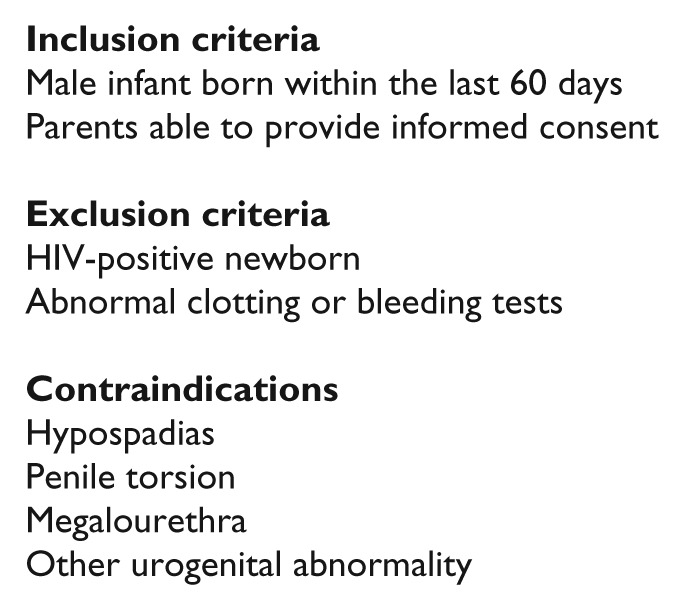
The Pollock Technique
For this low-resource setting, the Pollock technique of newborn male circumcision (see Figure 2), a procedure that utilizes the Mogen clamp, was selected due to its expediency and association with minimal bleeding and pain. Among experienced practitioners, the removal of foreskin can be performed in less than 30 seconds.23,24
Figure 2.
Key aspects of the Pollock technique, GHESKIO Health Centers, Haiti, 2014-2015.
Training Preparation and On-Site Activities
Prior to the training trip, weekly conference calls were held over a period of three months to review the Pollock technique and discuss logistics and supplies with the GHESKIO Health Centers’ staff. Written manuals translated into French and Creole were provided to the GHESKIO Health Centers’ staff to read before the rapid training program started (see Table 1).
Table 1.
Equipment required for up to 500 procedures of the Pollock Technique, GHESKIO Health Centers, Haiti, 2014-2015.
| Procedure Materials per Tray | Quantity | Notes |
|---|---|---|
| 2 Sets of surgical gloves | 10 boxes, 100 per box | |
| 1 × 8 Inch petroleum dressings | 5 boxes, 50 per box | |
| Iodine preparation pads | 3 boxes, 200 per box | |
| Coban tape | 5 packages, 12 per pack | |
| 1 Scalpel blade #23 | 5 boxes, 100 per box | |
| 2 Pieces of 3 × 3 inch unsterile gauze (one piece with petroleum jelly) | 5 packages, 200 per pack | |
| 3 mL syringe filled with 2.5 cc of 0.5% Xylocaine | 5 boxes, 100 per box | 60 vials of 20 mL 0.5% Xylocaine |
| 3 Pairs of 5 inch hemostats | 60 | |
| 1 Mogen clamp | 30 | |
| 1 Cotton ball with alcohol | Staff prepared | |
| 2 Sugar balls (cotton balls dipped in grape juice) | 1000 | |
| Other equipment | ||
| Infant restraining board | 6 | 2 extra leg straps |
| Autoclave | 1 | |
| Autoclave stopper bags | As needed | |
| Infant liquid acetaminophen | 30, 15 mL each | |
| Plastic instrument trays | 24 | |
| 18 G needle (to draw up Xylocaine) | 1 box, 100 per box | |
| 30 1/2 G needle for anesthetic | 5 boxes, 100 per box | |
| Petroleum jelly tubes, 30 g | 4 boxes, 144 packets per box | |
| 3 × 3 sterile gauze | 13 trays, 40 per tray | |
| Latex gloves, for training | 2 boxes | |
| Vice grips for training | 1 | |
| Emergency kit | 1 | 1 needle driver |
| 1 chromic gut suture | ||
| 1 pair of scissors | ||
| 2 pairs of hemostats | ||
| 1 tissue forceps | ||
Classroom instruction was given on the first day of the course to the selected GHESKIO Health Centers’ newborn male circumcision staff—two obstetricians and seven nurses—on (a) the technique, (b) common complications and management, and (c) outcome survey data collection. After the lectures, the GHESKIO Health Centers’ obstetricians practiced the technique on latex glove tips made to resemble foreskins under the instruction of the two physician-trainers. Nurses were taught to (a) assemble equipment trays, (b) deliver information for pre- and postprocedure instruction, (c) ensure the sterility of the instruments, and (d) prepare newborns for the procedure.
Over the next 2½ days, the physician-trainers taught the GHESKIO Health Centers’ obstetricians with hands-on demonstrations and supervised procedures. Initially, the physician-trainers performed the procedure with the obstetricians directly observing and assisting. Later, the GHESKIO Health Centers’ obstetricians prepared and performed the procedure while the physician-trainers observed and coached them. Two newborns were assigned to each procedure room to increase training and throughput capacity. Between circumcisions, 15-minute post-procedure check-ups were performed to assess bleeding and outcomes of the procedure.
The obstetricians carried cell phones continuously as “hotlines” to receive notifications of any potential complications related to the circumcision procedure. The newborns’ parents were informed to call the hotline if the newborn had signs of sustained bleeding, fever, excessive fussiness, or for any questions or concerns.
Nurses were trained to ensure proper participant flow, preparation, and education. Nurses administered an infant dose of liquid acetaminophen to the newborns while educating parents prior to the procedure; other nurses (a) prepared aseptic equipment trays, (b) assisted with the circumcision procedures, (c) assigned appointments for 1-day and 1-week follow-ups to assess the healing, and (d) instructed parents about post-procedure care.
Data Collection
Data collection surveys were prepared in English and French for the doctors and nurses. Nurses collected surveys in either French or Creole. The surveys assessed patient satisfaction, complications, and how well the various steps of the Pollock technique were followed.
Ethics Statement
The collection and analysis of the programmatic health services data were approved by the GHESKIO Ethics Committee. The University of California, Los Angeles, institutional review board deemed the review of de-identified data and analysis nonresearch, exempt from institutional review requirements.
Results
In the week prior to the training, 207 male newborns age <2 months were registered for circumcision; 24 newborns were excluded due to medical exam findings (2), testing HIV-positive (16), the lack of HIV test results (2), refusal of testing (1), and inability to contact (3). Of the 183 newborns remaining, 92 (50%) newborns presented during the 2½-day period for the procedure and were circumcised. On training completion, one of two obstetricians achieved procedural competence to perform the technique independently and teach others. All seven nurses achieved competence to assist with the procedure. The second obstetrician will need further training.
The obstetricians and nurses reported that they were very satisfied (100% and 92% respectively) with the training program (Table 2). The staff indicated that they thought the facility could comfortably support between 20 and 40 procedures per day. To improve the program, the obstetricians suggested (a) having four full days of training (vs 3½ days) and (b) spending more time learning to excise excess foreskin post-procedurally. The nurses suggested (a) increasing the number of on-site nurses, (b) decreasing the number of patients per day, (c) increasing the course length, and (d) improving the protocol as a means to expedite follow-up visits.
Table 2.
Obstetrician, nurse, and parent satisfaction, GHESKIO Health Centers, Haiti, 2014-2015.
| Obstetrician response (n = 2) | |
| Overall satisfaction with the training program | Very satisfied (100%) |
| Confidence to perform the procedure | Very confident (100%) |
| Number of procedures obstetricians feel comfortable to perform per day | 11-20 |
| Number of procedures obstetricians feel the facility can handle per day | 31-40 |
| Nurse response (n = 5) | |
| Overall satisfaction with the training program | Very satisfied (92%) |
| Confidence to assist with the procedure | Very confident (96%) |
| Number of procedures nurses feel comfortable to assist with per day | 27-36 |
| Number of procedures nurses feel the facility can handle per day | 23-32 |
| Parent (or guardian) response (n = 92) | |
| Overall satisfaction with the procedure | Very satisfied (94%) |
| Percentage of parents (or guardians) of newborns that would recommend newborn male circumcision to a friend | 100% |
| Percentage of parents (or guardians) of newborns agreeing that the procedure gave a satisfactory cosmetic result | 100% |
The parents of the newborns (n = 92) reported that they were very satisfied with the procedure (Table 2). Among the parents, 100% reported they would recommend newborn male circumcision to their friends and 100% reported that they were satisfied with the cosmetic result. One parent reported difficulty with postprocedural care and described that the newborn’s grandparents disapproved of the procedure. Another parent was distressed because her child was crying through the first post-procedural night.
The nurse-collected survey indicated that 100% of the procedures followed the Pollock technique protocol (Table 3). There were no moderate or severe complications. Nurses reported one episode of minor bleeding that quickly resolved with direct pressure.
Table 3.
Outcomes of newborn male circumcision procedures, GHESKIO Health Centers, Haiti, 2014-2015.
| Question | Observations | Percentage |
|---|---|---|
| Adherence to protocol | ||
| Sterilization protocol confirmed for all surgical instruments | 92/92 | 100 |
| Injected anesthesia used | 92/92 | 100 |
| Grape-juice-soaked cotton ball given to the baby | 92/92 | 100 |
| The infant’s penis and surrounding skin cleaned using aseptic technique prior to the procedure | 92/92 | 100 |
| The infant was checked for active bleeding after the procedure and prior to leaving the facility | 92/92 | 100 |
| No complications from the circumcision procedure | 92/92 | 100 |
| Entire glans visible | 92/92 | 100 |
| Complicationsa | ||
| Evidence of injury to the shaft and/or glans (laceration, amputation, etc) and/or to the urethra | 0/92 | 0.0 |
| Other potential findings suggesting a complication resulting from the circumcision | 0/92 | 0.0 |
| Evidence of bleeding | 1/92 | 1.1 |
| Evidence of an infection | 0/92 | 0.0 |
| Evidence of wound disruption | 0/92 | 0.0 |
| Suturing required | 0/92 | 0.0 |
| Problem with the appearance | 0/92 | 0.0 |
| Evidence of an injury to the glans | 0/92 | 0.0 |
| Evidence of a structural issue | 0/92 | 0.0 |
| Problem with appearance of penis | 0/92 | 0.0 |
Complication criteria based on the Male Circumcision Services Quality Assessment Toolkit guidelines provided by the World Health Organization.25
As of January 31, 2015, the GHESKIO Health Centers have dedicated two days a week to perform newborn male circumcisions, averaging 14 procedures per week.
Discussion
We successfully created and implemented a newborn male circumcision training program in Port-au-Prince, Haiti—an area with a considerable burden of preventable urogenital disease, sexually transmitted infections, and low circumcision rate.17,18,26 In 2½ days of procedures, about 40 procedures were completed per day. Surveys indicated a high-level of satisfaction from obstetricians, nurses, and parents of newborns. The complication rates were low and thus far the program has been sustained. Through those measures, we found that implementation of a rapid newborn male circumcision training program was feasible, achieving an acceptable rate of surgical competency and high-quality services.
The success of the training project was largely based on community support, the experience of the trainers, and a dedicated and capacitated local non-governmental health organization.15 Prior models for teaching newborn male circumcision procedures exist, but often long-term, international training programs are not feasible due to difficulties obtaining travel visas, identifying patients, and finding suitable mentors.1 The greatest challenges in enacting our training program were (a) transferring equipment, materials, and supplies; (b) coordinating physician-trainers’ schedules with those of local staff; and (c) ensuring an adequate number of eligible newborns were available for the procedure during the training period. Compared to prior reports, our training program was unique in terms of the speed with which it was implemented and the reduced time commitment from mentors.27
The GHESKIO Health Centers have dedicated two days a week for permanent newborn male circumcision services since the completion of the program. Additional non-governmental health organizations in Haiti are planning to train their staff in the procedure. Efforts will continue to secure funding and supplies for long-term sustainability and ultimately introduction in the government-funded health systems.
Newborn male circumcision is a highly effective medical procedure to reduce urinary tract infections, inflammatory conditions of the penis, sexually transmitted infections, and urogenital cancers. Recent conclusions from the US Centers for Disease Control and the American Academy of Pediatrics found that the health benefits of newborn male circumcision outweigh the risks. We aimed to help reintroduce newborn male circumcision through the creation of a training program in Port-au-Prince, Haiti, after an earlier study reported that a majority of Haitian medical providers were in need of and wanted newborn circumcision training. We found that implementing a rapid newborn male circumcision training program was feasible, achieving an acceptable rate of procedural competency and high-quality services. Permanent resources now exist in Haiti to train additional providers to perform newborn male circumcisions.
Acknowledgments
The authors acknowledge the GHESKIO Health Centers for hosting the clinical implementation of the Pollock Technique in Port-au-Prince, Haiti, the nurses of the GHESKIO Health Centers, and Dr. Traci Wells for assistance with French translation.
Footnotes
Author Contributions: NK generated the survey, analysed data, and wrote the paper with the guidance of CCB and JDK. NK, JDK, NP and PC assisted with the implementation of the program. HT, JB, CFSG, JGD, and JWP coordinated the program in Haiti.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Funding for this program evaluation was provided by the UCLA Center for AIDS Research (CFAR) NIH/NIAID AI028697 and NIH/NICHD R21HD076685.
References
- 1. World Health Organization. Manual for Early Infant Male Circumcision Under Local Anesthesia. Geneva, Switzerland: World Health Organization; 2010. [Google Scholar]
- 2. Auvert B, Sobngwi-Tambekou J, Cutler E, et al. Effect of male circumcision on the prevalence of high-risk human papillomavirus in young men: results of a randomized controlled trial conducted in Orange Farm, South Africa. J Infect Dis. 2009;199:14-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Gray RH, Kigozi G, Serwadda D, et al. The effects of male circumcision on female partners’ genital tract symptoms and vaginal infections in a randomized trial in Rakai, Uganda. Am J Obstet Gynecol. 2009;200:42.e1-e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Klausner JD, Morris BJ. Benefits of male circumcision. JAMA. 2012;307:455-456. [DOI] [PubMed] [Google Scholar]
- 5. Shaikh N, Morone NE, Bost JE, Farrell MH. Prevalence of urinary tract infection in childhood: a meta-analysis. Pediatr Infect Dis J. 2008;27:302-308. [DOI] [PubMed] [Google Scholar]
- 6. Tobian AA, Gray RH. The medical benefits of male circumcision. JAMA. 2011;306:1479-1480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Klausner JD. Newborn circumcision: ensuring universal access. Sex Transm Dis. 2013;40:526-527. [DOI] [PubMed] [Google Scholar]
- 8. Centers for Disease Control & Prevention. Recommendations for Providers Counseling Male Patients and Parents Regarding Male Circumcision and the Prevention of HIV Infection, STIs, and Other Health Outcomes. Washington, DC: US Department of Health and Human Services; 2014. [Google Scholar]
- 9. American Academy of Pediatrics Task Force on Circumcision. Circumcision policy statement. Pediatrics. 2012;130:585-586. [PubMed] [Google Scholar]
- 10. Gray RH, Kigozi G, Serwadda D, et al. Male circumcision for HIV prevention in men in Rakai, Uganda: a randomised trial. Lancet. 2007;369:657-666. [DOI] [PubMed] [Google Scholar]
- 11. Auvert B, Taljaard D, Lagarde E, Sobngwi-Tambekou J, Sitta R, Puren A. Randomized, controlled intervention trial of male circumcision for reduction of HIV infection risk: the ANRS 1265 Trial. PLoS Med. 2005;2:e298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bailey RC, Moses S, Parker CB, et al. Male circumcision for HIV prevention in young men in Kisumu, Kenya: a randomised controlled trial. Lancet. 2007;369:643-656. [DOI] [PubMed] [Google Scholar]
- 13. Binagwaho A, Pegurri E, Muita J, Bertozzi S. Male circumcision at different ages in Rwanda: a cost-effectiveness study. PLoS Med. 2010;7:e1000211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Brito MO, Caso LM, Balbuena H, Bailey RC. Acceptability of male circumcision for the prevention of HIV/AIDS in the Dominican Republic. PLoS One. 2009;4:e7687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Saxena A, Gaston S, Jean-Gilles M, et al. Acceptability of medical male circumcision (MMC) among health care providers in Port-au-Prince, Haiti (poster). Presented at the APHA 142nd Annual Meeting & Expo New Orleans, LA, USA. [Google Scholar]
- 16. Manganiello M, Hughes CD, Hagander L, et al. Urologic disease in a resource-poor country. World J Surg. 2013;37:344-348. [DOI] [PubMed] [Google Scholar]
- 17. Joint United Nations Programme on HIV/AIDS. UNAIDS Report on the Global AIDS Epidemic. Geneva, Switzerland: Joint United Nations Programme on HIV/AIDS; 2012. [Google Scholar]
- 18. Joint United Nations Programme on HIV/AIDS. 2009 AIDS Epidemic Update. Geneva, Switzerland: Joint United Nations Programme on HIV/AIDS; 2009. [Google Scholar]
- 19. The Global Fund to Fight AIDS, Tuberculosis and Malaria. Global Fund Eligibility List 2014. Geneva, Switzerland: The Global Fund to Fight AIDS, Tuberculosis and Malaria; 2014. [Google Scholar]
- 20. Rouzier V, Farmer PE, Pape JW, et al. Factors impacting the provision of antiretroviral therapy to people living with HIV: the view from Haiti. Antivir Ther. 2014;19(suppl 3):91-104. [DOI] [PubMed] [Google Scholar]
- 21. Duke W. The relation of blood platelets to hemorrhagic disease. JAMA. 1910;55(14):8. [PubMed] [Google Scholar]
- 22. Lee RI, White PD. A clinical study of the coagulation time of blood. Am J Med Sci. 1913;145(4):9. [Google Scholar]
- 23. Taddio A, Pollock N, Gilbert-MacLeod C, Ohlsson K, Koren G. Combined analgesia and local anesthesia to minimize pain during circumcision. Arch Pediatr Adolesc Med. 2000;154:620-623. [DOI] [PubMed] [Google Scholar]
- 24. Pollock Clinics Circumcision. http://www.pollockclinics.com/circumcision. Accessed May 15, 2015.
- 25. World Health Organization. Male Circumcision Services Quality Assessment Toolkit. Geneva, Switzerland: World Health Organization; 2009. [Google Scholar]
- 26. United Nations Development Programme. Human Development Report 2013; The Rise of the South: Human Progress in a Diverse World. Geneva, Switzerland: United Nations Development Programme; 2013. [Google Scholar]
- 27. Orolorin E, Johnson P. Male Circumcision Under Local Anaesthesia: Course Handbook for Participants. Geneva, Switzerland: World Health Organization; 2008. [Google Scholar]