Introduction
Molar pregnancy, also known as hydatidiform mole, is the most common form of gestational trophoblastic disease. Although rare, hyperthyroid signs and symptoms may be indicative of molar pregnancy. We describe a case of a teenage girl with type 1 diabetes mellitus who presented with thyrotoxicosis secondary to molar pregnancy.
Patient Report
A 17-year-old Vietnamese-American female with an existing diagnosis of type 1 diabetes presented to the office with complaints of excessive sweating, palpitations, and episodic panic attacks. Her other complaints included intractable nausea, vomiting, and intermittent excessive vaginal bleeding for about a month. She was also experiencing sleep disturbances and more hypoglycemic episodes lately, and she has lost about 4 pounds of weight. She had her menarche at 13 years of age and it has been regular, except for the last month. Her diabetic control has been reasonable and is managed with a basal bolus regimen of insulin.
Physical Examination
She looked pale, anxious, and uncomfortable. Her height was 155 cm (10th percentile), weight 50 kg (20th percentile), blood pressure 130/65, pulse 115 to 120. Examination of neck revealed a uniform enlargement of the thyroid gland involving both lobes, approximately 40 g in size. There was a bruit present over both lobes of the thyroid. There was no cervical lymphadenopathy, and she had no exophthalmos. Deep tendon reflexes were brisk in both extremities. Abdominal examination showed a midline abdominal mass originating from the pelvic area consistent with the size of a 12-week gestational-age pregnant uterus. Her pubertal development is complete. Remainder of physical examination was unremarkable.
Pertinent Laboratory Evaluation
Laboratory evaluation showed a normal complete blood count, hemoglobin 11 g/dL (range = 11-15), random blood glucose 181 mg/dL, hemoglobin A1c 7.8% (range = 3% to 6%), free T4 5.0 ng/dL (range = 0.8-2), thyroid-stimulating hormone (TSH) <0.05 mIUnit/mL (range = 0.4-4.5), total T3 468 ng/dL (range = 80-150), with negative thyroid-stimulating immunoglobulin, thyroid peroxidase, and antithyroglobulin antibodies. Urine pregnancy test was positive and serum human chorionic gonadotropin (hCG) level was >150 000 mIU/mL (Reference 0-5). Pelvic sonogram showed a complete hydatidiform mole with a small embryonic gestational sac with many anechoic cysts (Figure 1). She was started on a long-acting β-blocker, atenolol 25 mg 2 times a day, and was referred to the Obstetrics/Gynecology Department where a complete evacuation of uterine content was performed by dilatation and curettage (D&C). Histology confirmed the diagnosis of complete molar pregnancy. Serial thyroid function tests and hCG levels are shown in Table 1.
Figure 1.
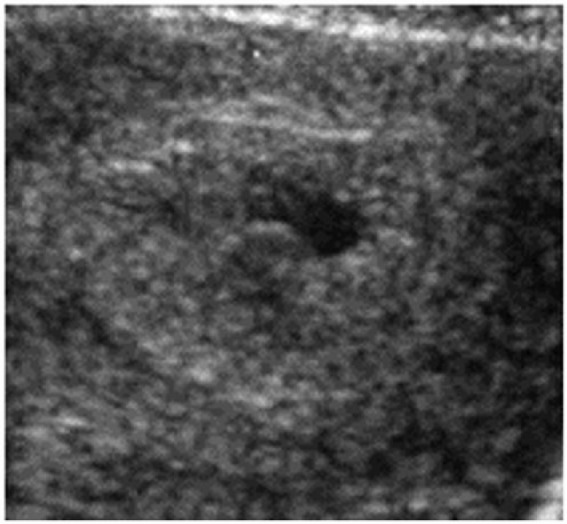
Ultrasound of molar pregnancy.
Magnified transverse sonogram shows complete hydatidiform mole at 8 weeks of menstrual age. There is a small embryonic gestational sac with many anechoic cysts.
Table 1.
Thyroid Function Tests and Human Chorionic Gonadotropin (hCG) Levels Before and After Removal of Molar Pregnancy.
| At Diagnosis | Day 3 After Removal | 1 Week After | 3 Weeks After | |
|---|---|---|---|---|
| Thyroid-stimulating hormone (range = 0.4-4.5 mIU/mL) | <0.05 | <0.06 | 0.2 | 1.3 |
| Free T4 (range = 0.8-2 ng/dL) | 5.0 | 3.0 | 2.2 | 1.78 |
| Total T3 (range = 80-150 ng/dL) | 468 | 257 | 182 | 162 |
| hCG (range = 0-5 mIU/mL) | >150 000 | 9525 | 193 |
Discussion
Hydatidiform mole is a benign gestational trophoblastic disease. It can either be complete or partial. A complete mole usually occurs when an empty ovum is fertilized by a sperm and therefore there is no coexisting fetus. The partial form occurs when a normal ovum is fertilized by 2 sperm and nearly always has a coexistent fetus. The incidence of molar pregnancies in the United States and other developed countries is 1 per 1500 to 2000.1,2 There is a higher incidence of molar pregnancy in Asian and Native American women, women under the age of 20 years, and women over the age of 40.2 The clinical triad of molar pregnancy includes uterine enlargement inconsistent with dates, hyperemesis gravidarum, and markedly elevated serum hCG level.3 Excessive vaginal bleeding mimicking threatened abortion is also a very common early complaint.3 Ultrasound is primarily used to rule out an intrauterine pregnancy. Classic sonographic appearance of a complete mole shows a snowstorm or granular appearance.4 A central heterogeneous mass with numerous anechoic (cystic) spaces and absence of an embryo or fetus is also characteristic.1,4 When sonographic appearance and hCG levels are suspicious for hydatidiform mole, the diagnosis should be confirmed by histology.
Complete molar pregnancy has the highest incidence of hyperthyroidism, predominantly affecting younger women and presents with vaginal bleeding.3 Prevalence of hyperthyroidism in complete molar pregnancy is as high as 7%.5 The causes of hyperthyroidism in molar pregnancy are multifactorial. The most important one is the extremely elevated hCG level. The beta subunit of the hCG molecule is very structurally similar to TSH, and therefore can bind to the TSH receptor on thyroid follicular cells.6 Although hCG is a weak thyrotropic agonist, very high concentrations in molar pregnancy makes it formidable. It has been estimated that for every 10 000 mU/mL increase in serum hCG, free T4 increases by 0.1 ng/dL and TSH decreases by 0.1 mIU/mL.7
The molecular variants of hCG found in molar pregnancy also increase thyrotropic potency.8,9 In one of the variants, the 47–48 peptide bond in the beta subunit loop of hCG is nicked, leading to the desalination of hCG. This reduces the sialic acid content of the hCG molecule, which further enhances its thyrotropic potency.8 These changes in the molecules may also increase the half-life of hCG, which may be another etiological factor resulting in hyperthyroidism. There are other variants in molar pregnancy that may enhance thyrotrophic activity also.5,8 The molecular changes discussed above are not uniformly present in all molar pregnancies and that may be the reason for the absence of clinical and biochemical hyperthyroidism in many molar pregnancies.
Hyperthyroidism in molar pregnancy is treated by performing a complete evacuation of the uterus by D&C or a hysterectomy for older women, if future pregnancy is not desired.2 Prior to D&C, the patient can be stabilized by using a β-blocker. Depending on the degree of hyperthyroidism in some patients, anti-thyroid drugs like methimazole or propylthiouracil may be necessary to control the overt hyperthyroidism. Our patient was managed with a long-acting β-blocker prior to D&C. Thyroid function was normal after 3 weeks, and hCG level was normal after 3 months. It is very important to monitor hCG level after D&C. Persistently elevated hCG may suggest a progression to persistent gestational tropoblastic neoplasia. We do not believe type 1 diabetes played any role in molar pregnancy in our patient.
Footnotes
Author Contributions: AMK contributed to conception and design; contributed to acquisition; drafted manuscript; critically revised manuscript; gave final approval; agrees to be accountable for all aspects of work ensuring itegrity and accuracy. SKB contributed to conception and design; contributed to acquisition, analysis, and interpretation; critically revised manuscript; gave final approval; agrees to be accountable for all aspects of work ensuring itegrity and accuracy.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Green CL, Angtuaco TL, Shah HR, Parmley TH. Gestational trophoblastic disease: a spectrum of radiologic diagnosis. Radiographics. 1996;16:1371-1384. [DOI] [PubMed] [Google Scholar]
- 2. Lurain JR. Gestational trophoblastic disease I: epidemiology, pathology, clinical presentation and diagnosis of gestational trophoblastic disease, and management of hydatidiform mole. Am J Obstet Gynecol. 2010;203:531-539. [DOI] [PubMed] [Google Scholar]
- 3. Bhat S, Maletkovic J. A hydatidiform mole can cause severe gestational hyperthyroidism. Clin Thyroidol. 2013;25:298-300. [Google Scholar]
- 4. Lazarus E, Hulka C, Siewert B, Levine D. Sonographic appearance of early complete molar pregnancies. J Ultrasound Med. 1999;18:589-594. [DOI] [PubMed] [Google Scholar]
- 5. Garner EI, Goldstein DP, Feltmate CM, Berkowitz RS. Gestational trophoblastic disease. Clin Obstet Gynecol. 2007;50:112-122. [DOI] [PubMed] [Google Scholar]
- 6. Hershman JM. Role of human chorionic gonadotropin as a thyroid stimulator. J Clin Endocrinol Metab. 1992;74:258-259. [DOI] [PubMed] [Google Scholar]
- 7. Glinoer D. The regulation of thyroid function in pregnancy: pathways of endocrine adaptation from physiology to pathology. Endocr Rev. 1997;18:404-433. [DOI] [PubMed] [Google Scholar]
- 8. Pekary AE, Jackson IM, Goodwin TM, Pang XP, Hein MD, Hershman JM. Increased in vitro thyrotropic activity of partially sialated human chorionic gonadotropin extracted from hydatidiform moles of patients with hyperthyroidism. J Clin Endocrinol Metab. 1993;76:70-74. [DOI] [PubMed] [Google Scholar]
- 9. Yoshimura M, Hershman JM. Thyrotropic action of human chorionic gonadotropin. Thyroid. 1995;5:425-434. [DOI] [PubMed] [Google Scholar]


