Abstract
Neonatologists and paediatric providers of developmental care have documented poor neurodevelopmental outcomes of infants who have received neonatal intensive care due to prematurity, perinatal neurological insults such as asphyxia or congenital anomalies such as congenital heart disease. In parallel, developmental specialists have researched treatment options in these high-risk children. The goal of this review is connect the main categories of poor outcomes (sensory and motor function, cognition, communication, behaviour) studied by neonatal intensive care follow-up specialists to the research focused on improving these outcomes. We summarise challenges in designing diagnostic and interventional approaches in infants <2 years of age and review the evidence for existing therapies and future treatments aimed at improving functionality.
Preterm birth or perinatal complications that require neonatal intensive care often result in neurodevelopmental delay or impairment. These include abnormalities of vision, hearing, cognition, communication, speech and language, as well as motor problems ranging from feeding disorders, gait abnormalities, motor planning problems or cerebral palsy (CP).1 Early detection and treatment of these problems offers the best opportunity to improve outcomes but is difficult. This review addresses the current state of early neurorehabilitation of high-risk infants, defined as functional recovery from disruptions to normal neural development, and discusses the challenges of developing new evidence-based interventions.
Diagnostic and Design Challenges
Neonatal specialists are often asked to predict outcomes for neonates who receive intensive care for causes including prematurity, congenital heart malformations requiring surgery or perinatal asphyxia. Optimally, the hope of effective interventions would be offered along with a guarded prognosis. However, the availability of evidence-based rehabilitative treatments is limited. Design of new therapies is complicated by the (1) complexity of developmental sequences necessary to establish functional domains, (2) the variability and delays in neurological impairments after an initial insult and (3) the unique characteristics of assessments in infants and very young children.
One complication to therapy design is the context of the developing infant brain (figure 1). Most learning through infancy depends on the prior establishment of sensory and motor systems in order to receive information, interact with the environment and subsequently construct more complex systems. Neural processes such as the formation of multisensory connections and higher-order networks are all built upon the more basic functions (eg, hearing, vision).2 Factors altering the sequence of normal neurodevelopment include interruptions (preterm birth and its complications) or disruptions (injuries resulting from insults such as prolonged hypoxia or illness). Neural plasticity, the process of reorganisation of neural connections after injury or experiences,3 can be a double-edged sword: compensation for a brain lesion or a poorly functioning pathway can be re-established at the expense of another pathway or even of a higher-order process, such as is the case in amblyopia (discussed later in this review). Finally, all of early neurodevelopment is driven by growth and environment, making nutritional, social–emotional and physical environmental factors an essential but complex component of evaluation and treatment in infancy.
Figure 1.
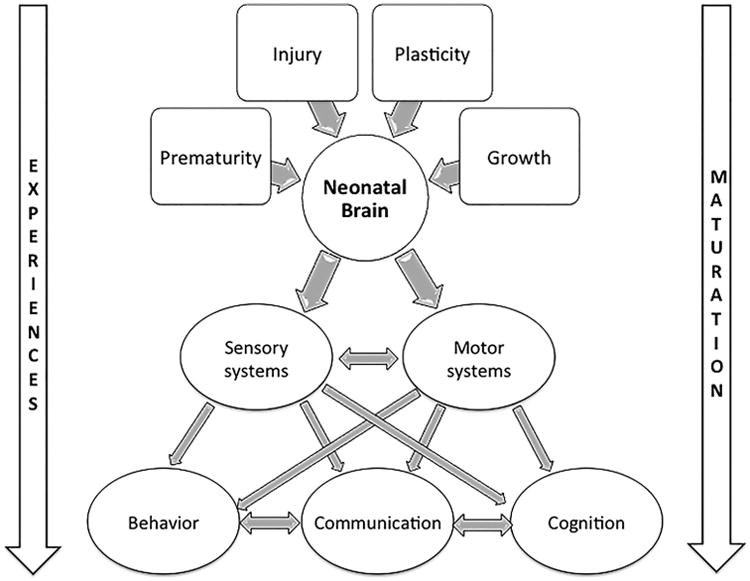
Building blocks of neurodevelopment in neonatal intensive care unit graduates. The neonatal brain is subject to multiple influences during initial critical windows of development of basic pathways. Some of these phases are independent of experience but affected by injury, plasticity and interruption or resumption of normal developmental sequences. Establishment of complex interconnections within and between the sensory and motor systems occurs at critical times during the maturation process and is dependent on experience, and therefore influenced by environmental conditions. The establishment of higher order processes (cognition, communication, behaviour) requires connections between cortical and subcortical areas, as well as among widely distributed functional networks (attention, receptive language, expressive language). These networks in infancy are built upon the information provided by direct sensory experience of the environment as well as indirect feedback from sensory–motor interactions). All higher processes are tightly interconnected and deficits rarely occur in isolation. Throughout neurodevelopment, maturation and experiences shape the construction and function of all systems. In addition to their contributions to the substrate of brain development, prematurity and growth/nutritional conditions may act by altering the maturation process through complications and deficiencies.
Another challenge to neurorehabilitation is the difficulty of establishing a diagnosis in the first two years of life when intervention may have the greatest impact. Early diagnosis of impairments is complicated by a changing developmental picture as neonatal insults continue to disrupt normal brain development throughout infancy and childhood. Some downstream effects of initial insults are directly related to the loss of progenitor cells resulting in failure of normal myelination, as in white matter injury of preterm infants. Because myelination is a lengthy process starting in the near-term period and continuing well into school age, the extent of deficits may not be apparent until childhood. The selective vulnerability of neural cell populations and brain regions at different ages can result in variable long-term effects, as well as in term infants with encephalopathy who develop either white or grey matter injury depending on the timing of the insult. Early white matter injury from ischaemia and inflammation seen in children with congenital heart disease can also lead to late impairments in grey matter development. Finally, Wallerian neurodegeneration, the loss of entire pathways or structures in the brain due to lack of trophic support, can occur over a period of several months after an insult.4
In addition to accounting for ongoing neurodevelopmental changes, the design of objective, standardised, norm-referenced tools for early diagnosis must accommodate an infant's limited range of active response capabilities. Child-friendly, non-invasive approaches and brief or modular tests to prevent fatigue are necessary but may be less accurate than the neurological and neuropsychological batteries available for older children. The current toolbox available for early assessment and diagnosis reflects these challenges (table 1). Due to the lack of referenced or standardised measures, some tools are only used for research.
Table 1. Neurodevelopmental assessment toolbox in high-risk children ≤2 years of age.
| Developmental domain | Tool types | Measure examples |
|---|---|---|
| Hearing | Auditory brainstem responses, otoacoustic emissions | Amplitude, latency, range of sound processing |
| Vision | Standardised exams, preverbal function tests | Acuity, contrast sensitivity, resolution of images |
| Somatosensory | Evoked potentials (time-locked EEG) | Amplitude, latency, topography of response to tactile stimuli |
| Motor | Developmental milestones, standardised movement or neurological assessments | Standardised scores, normative patterns, milestone acquisition |
| Oro-motor/feeding | Imaging, pressure and impedance, electrophysiology studies | Qualitative and quantitative measures of phases of feeding and gastrointestinal motility |
| Communication | Standardised assessments, interaction measurements | Composite scores, referenced performance times |
| Speech/language | Vocabulary quantitation, picture word recognition, gaze timing | Scaled or standardised scores, performance times on look/listen tasks |
| Cognition | Standardised assessment batteries | Standardised scores (population specific) |
| Executive function | Directed tasks | Performance on plexiglass barrier task, object permanence |
Research tool indicated in italics.
Tools to measure function are rare for this age group. The tools used for diagnosis, when they exist, often classify a stage of developmental progression or the degree and type of impairment. In contrast, the WHO framework for disabilities5 underlines the need to develop measures of functionality and treatment effectiveness instead. New tools are still being researched in this area (table 1) and hold promise for the future of functional assessments.
Another impediment to the development of interventions is that understanding how to support the establishment of new functional connections after neonatal insults is limited. Design of new interventions is often extrapolated from knowledge of adult processes and therapies that are not always applicable to infants. For example, in adults with stroke, forced use of a paretic arm can overcome the learned non-use after injury. Application of this principle to infants is not always successful because in infants paresis originates from a wider variety of lesions and is affected by different compensatory pathways; this results in a mixed response to the treatment.6
Despite these challenges, attempts at rehabilitation of neonatal intensive care unit (NICU) graduates span multiple medical fields, including developmental medicine, audiology, ophthalmology, neurology, speech and occupational and physical therapy. There are obvious disparities in knowledge between the various types of impairments sustained by NICU graduates. In general, the more complex an affected function is, the less is known about both its diagnosis and rehabilitation. Sensory and motor neurorehabilitation are better studied, while effective cognition, communication and behaviour interventions are scarce.
A Primer of Early Interventions for NICU Graduates
For this overview of rehabilitative interventions, we searched PubMed, the Cochrane Library and Google Scholar using search terms for the developmental domains reported by neonatology outcomes studies (figure 1), limiting our search to infants <2 years of age, and systematic reviews and meta-analyses with publication dates or updates in the past five years. When these types of publications were not available for a specific domain of development, we expanded our search for new and promising studies with same keywords but this time preferentially choosing randomised controlled trials (RCTs), acknowledging that these represent only a small sample of potential research directions.
Neurosensory Rehabilitation
The study of hearing and vision impairments of high-risk infants has resulted in a solid base of diagnostic tools and rehabilitative strategies. Somatosensory problems, particularly those associated with neonatal pain exposure, were more recently identified and are therefore poorly studied at this time.
The benefits of early hearing screen for high-risk infants have been conclusively demonstrated in multiple large studies.7 Otoacoustic emission or auditory brainstem response measurements are useful for early detection of hearing impairments in infancy, while connections between auditory processing and language understanding and production are still being established. Interventions aimed at improving hearing all use the same basic concept of neurorehabilitation (figure 2): they combine neural stimulation, an elicited electrical activity of a neural pathway (in this case of cranial nerve VIII), with cognitive and behavioural training (the creation of functional associations between a stimulus, a direct response and higher order cortical processes) to re-establish functional connections between speech sounds and language processing. For hearing aids, sound enters a microphone, is amplified and shaped by a processor, and is directed out a tone hook through an earmold into the ear canal.8 Some anchored aids directly use bone conduction to bypass the ear canal. Hearing aids used before 6 months of age confer a significant advantage for language intelligibility, and bilateral aids are recommended as early as 3 months to improve receptive language development. Even in children with mild impairments, increased audibility from hearing aids in the second year of life results in improved preschool speech and language.9
Figure 2.
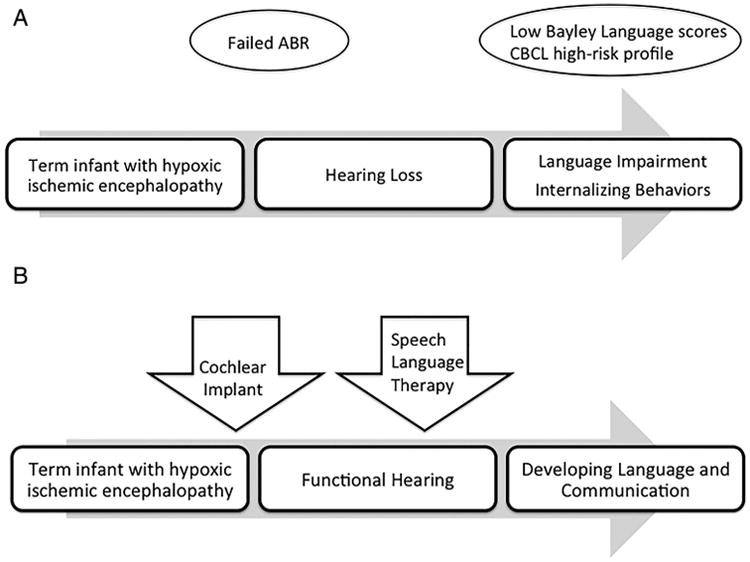
Example of newborn with sensorineural hearing loss due to perinatal hypoxic-ischemic encephalopathy diagnosed early using auditory brainstem response measurements and outcome with and without neurorehabilitation. (A) If hearing impairment is undiagnosed or untreated in the first 12–18 months, the resulting loss of auditory processing can lead to receptive and expressive language impairments. Later, communication impairments can lead to internalising behaviours related to social and emotional isolation, precursors of anxiety and depression. (B) Early diagnosis of hearing impairment followed by aggressive neurorehabilitation has a large downstream effect, preventing the arrest of neurodevelopment and facilitating functional adaptations. Early cochlear implant placement provides neural stimulation to the cochlear nerve and auditory cortex. Combined with speech language therapy (behavioural training), improved auditory processing allows the development of receptive and expressive language. Communication facilitates learning and social–emotional interactions, promoting the development of adaptive behaviours. ABR, auditory brainstem response; CBCL, Child Behavior Checklist.
Cochlear implants consist of receiver-stimulator devices surgically placed under the periosteum of the mastoid bone with electrodes on the scala tympani of the cochlea. A microphone sends sounds to a speech processor that converts them into electronic signals relayed through a transmitter coil to the receiver stimulator. Unlike a hearing aid, the implant can bypass damaged hair cells and directly stimulate the auditory nerve.8 Cochlear implants used earlier (6–12 months) and for longer durations in the first three years of life improve spontaneous expressive and receptive language, as well as other communicative abilities, in infancy and at school age.7
Even partial impairments of vision have profound long-term socioeconomic consequences, resulting in adults with a higher likelihood of having an unskilled profession and poorer function in activities of daily living. Preterm infants have higher rates of retinal detachment after retinopathy of prematurity (ROP), but also of strabismus, myopia, amblyopia and cortical visual impairment.10,11 Standardised ophthalmological exams as well as visual function assessments designed for preverbal children are commonly used for diagnosis. ROP exams start in the NICU and continue throughout infancy, as vasoproliferative disease of the retina can cause retinal detachment and blindness well beyond the neonatal period. Early laser coagulation or cryotherapy of the peripheral retina or bevacizumab injection can usually prevent detachment of the macula, preserving acuity, visual fields and contrast sensitivity.
Amblyopia, reduced visual function due to discrepancy of function between the two eyes, is a common impairment of high-risk infants, with prematurity and birth asphyxia accounting for >50% of early diagnoses.12 It is most commonly associated with anisometropia (differences in refractive errors between both eyes) or strabismus (misalignment of one eye in relation to the other). Amblyopia is a consequence of plasticity, as pathways from the amblyotic eye are reassigned to the functional one, resulting in visual deficits. This is one example of the challenges to neurorehabilitation, when the compensatory abilities of the developing nervous system can happen at the expense of other fully functioning neural networks. Rehabilitation therefore combines neural stimulation to the amblyopic eye by either patching or applying atropine to the more functional eye, combined with active use of the less-functional eye in activities of daily living.13 This principle of forced use with training in relevant activities is similar to that of constraint therapy for hemiplegic CP, which will be discussed later. Early detection and treatment are more efficient in the youngest children (<3 years) with extremely good results in about 75% of all children treated at <7 years.14 For amblyopia, the other essential therapeutic intervention is correction of visual acuity with glasses. However, only about one-fourth of young children treated with glasses alone have complete resolution of the problem.15
Treatment of infantile strabismus, another common ophthalmological problem of NICU graduates, aims to align the visual axes and restore binocularity. However, a Cochrane review attempting to compare various surgical and medical treatments (primarily botulism toxin) for esotropia and hypertropia found only observational cohort studies.16 Results were conflicting on whether surgery prior to 2 years resulted in better long-term outcomes: earlier operation was associated with better sensory or motor outcomes by age 6 (depending on the study), but also with an increased risk of having repeat surgery before age 4.16
White matter damage secondary to infarction or periventricular leukomalacia is associated with a characteristic syndrome of optic nerve hypoplasia.12 Preterm infants with this type of insult may develop other types of visual impairments such as poor visuospatial skills (mental imagery and spatial construction, navigation, distance and depth perception) and hand–eye coordination,17 directly related to worse performance IQ measures. Perceptual learning programmes with intense repetitive practice effectively treat these problems in older children, but their duration and monotony make them poorly adapted for use in infants. Newer, more child-friendly approaches such as computer-assisted visual field training have shown promising improvements in visual fixation and colour discrimination.18
Somatosensory and nociceptive (pain) processing is affected by procedures inherent to NICU hospitalisation such as skin breaks or surgical procedures.19,20 Infants show an increase in internalising behaviours (anxiety/depression/withdrawal) at 18– 22 months associated with the amount of exposure to painful procedures.20 Preterm infants exposed to invasive procedures also have altered sensory thresholds to temperature and negative sensory reactivity (aversion to combinations of sensory stimuli) in childhood.19,21 Parenting types characterised by emotional availability and non-hostility decrease the association between painful procedures and infant internalising behaviours, while higher parenting stress increases it.20 Therefore, interventions aimed at parenting education, such as those currently used to improve communication outcomes (see PremieStart below), could be investigated for their potential to ameliorate neurosensory problems as well.
Motor Rehabilitation
Studies of early intervention from the 1960s to 1990s consisted mostly of attempts to promote a normal developmental sequence using experientially based adjustment of infant movements by therapists. This traditional approach showed no lasting improvement for most motor outcomes and is not supported by systematic reviews, neuroscience or psychology.22,23 Our current scientific understanding indicates that treatments should be based on infant-directed learning and initiation of actions, goal-directed movements and positive reinforcement.23 Fortunately, research in evidence-based motor interventions has been driven by a multidisciplinary group of clinicians, therapists and scientists in the CP community. This group has reviewed and graded the past 40 years of evidence to establish recommendations for early diagnostic tools and interventions designed to take advantage of early brain plasticity, while remaining aware of its potential for causing compensatory deficits in developing children.24 Combined with analyses of risk factors, specific neuroimaging patterns and very early standardised and validated tools such as the General Movements Assessments, the Developmental Assessment of Young Children and the Hammersmith Infant Neurological Assessment, it is possible to diagnose CP by 12 months of age, even in preterm infants whose variable tone often confounds neurological exams.25 Most effective rehabilitative therapies for CP have been shown in preschool-age children to improve function, strength, endurance, posture and interactions with the environment, with lasting positive effects through adolescence.22 Ongoing RCTs such as the baby-Constraint Induced Movement Therapy trial (baby-CIMT; SFO-V4072/2012) are studying the effectiveness of forced use of a paretic arm using a restraint on the less affected arm, only during parent-directed and task-oriented training. The targeted infants are NICU graduates at risk for CP as determined by clinical and neuroimaging correlates. The study is designed to take advantage of maximal brain plasticity before motor tracts to a more affected extremity can be diminished by non-use; at the same time, it ensures that the more functional extremity does not suffer a lack of sensorimotor input from restraint, which could result in future fine motor deficits.26 New interventions for infants with lesions on neonatal neuroimaging have been designed based on principles of infant motor learning and mirror neuron systems: the action-observation arm of the Upper Limb Baby Early Action-Observation Training (UP-BEAT: ACTRN 1261100991910) study27 aims to imprint functional neuromotor patterns in the premotor cortex by having infants watch an action being executed, when voluntary reaching is not yet part of environmental exploration. This RCT tests an intervention between 9 and 18 weeks post-term, when action-imitation may influence the downstream reorganisation of damaged motor pathways. Both baby-CIMT and UP-BEAT results will be available in 2015. Given the constant design and improvement of new evidence-based rehabilitative therapies, it is important to stress to the parents of an NICU graduate with likely motor impairment on neuroimaging that current therapeutic advances can substantially improve their child's function, although the extent is not currently known.
Oromotor impairments often result in feeding difficulties for infants who are preterm, have neonatal encephalopathy or congenital heart defects requiring surgical repair. Most rehabilitative interventions aim at re-establishing patterns of suck–swallow– breathe coordination and increase endurance and efficiency during oral feeding. The most successful use non-nutritive sucking training, which consistently decreases the time from tube to oral feeding.28 Using the same principles as for other motor interventions in infancy, excellent results can be obtained by using positive reinforcement to condition optimal oromotor function. Oral and perioral sensory stimulation demonstrate more variable results, and a recent systematic review concluded that evidence is insufficient to recommend this type of therapy.29 Successful behaviour-based interventions can promote better feeding after NICU discharge by decreasing a child's resistance to oral feeding.28 These interventions are based on basic child psychology principles and conditioning such as positive reinforcement of desired behaviours with differential attention (reward appropriate and ignore inappropriate behaviours), extinction of aversive behaviours and physical guidance (manual assistance to shape movements necessary to feeding). Because they improve oromotor and orosensory function, these behavioural interventions can also be considered successful neurorehabilitation.
Cognitive Interventions
Cognition is the outcome of concern in most large NICU follow-up studies as it describes the sum of many higher order brain functions. This general term encompasses the process of acquiring knowledge and understanding by means of thought, experience and the senses, and includes memory, association, concept formation, pattern recognition, attention, problem solving and emotion. The cognitive outcomes of high-risk infants depend on the establishment of many earlier brain systems, all potentially affected by perinatal insults or dysmaturity (figure 1). In addition, cognition is supported or hindered by experience with the sensory, physical and social–emotional environment.
Improving cognitive outcomes in infancy has been the focus of most early intervention programmes, combined with the previously mentioned neurodevelopmental motor therapy.30 Intervening as early as possible provides the largest return on investment for initiatives aimed at improving cognition, socioemotional skills and mental health. Work by Heckman et al further demonstrates that the gains of early intervention are even more significant for those at the highest socioeconomic and racial disadvantages.31 Because of the potential for brain plasticity and the contributions of the social environment to neurodevelopment, very early intervention is especially relevant to children with cognitive delays originating at birth, such as NICU graduates.
Home programmes aimed at improving parent–infant interactions for preterm infants with exercises, play, exposure to books and effective communication show increases of 1/3 of SD in a combination of cognitive scores during infancy and up to 1/2 SD at preschool age. SD were used as units as they differ between assessments, with SD=15 on the Bayley Scales of Infant and Toddler Development but SD=13 on the Griffiths Mental Development Scales, for example.30 Interventions aimed specifically at teaching parenting skills or involving parents in early care of their child demonstrate a significant increase in favour of treatment (>5 points) on the Bayley Scales of Infant Development Mental Development Index at 12–24 months. However, the effect size of these interventions often dissipates by 5 years,32 suggesting that continued parental education and facilitated involvement may be necessary for long-term cognitive benefits in high-risk infants. In support of this speculation, most school-age studies of NICU infants' performance show that maternal education explains up to 1/4 of the variance in outcomes.
Former preterm infants and infants with congenital heart defects often have deficits in executive functioning such as working memory or attention. Although executive function testing is well established in school-age children, it is still an emerging area in infants. New standardised measurement tools have been developed for preschool-age children.33 However, in children <2 years of age, assessments consist of individual tasks, usually developed to measure the effect of an intervention instead of the standardised battery used in older children. Promising interventions exist to train the gaze-contingent attentional control of typically developing 11-month-old infants using computer-generated tasks with improvements in sustained attention.34 Future research on interventions targeting specific components of cognition for NICU graduates will depend on increasing collaborations with psychology and neuroscience to elucidate infant-learning processes.
Communication, Speech and Language Therapies
Numerous studies in high-risk infants have documented delays and impairments in these three overlapping outcomes.35,36 Communication is the ability to receive, send and comprehend concepts or verbal, non-verbal and graphic symbol systems. Speech is therefore only one form of communication, involving the production of speech sounds through articulation, fluency and voice. In parallel, language is a construct of rules on the meaning and creation of new words, as well as combinations of words in grammar, syntax and context. Language can be expressive (spoken or directed towards others) or receptive (understood through symbolic or auditory patterns from others). Until children have reached a stage of brain maturation allowing connections between verbal labels and actions/objects, interventions aimed at direct and specific language acquisition have little effect. Therefore, most interventions in infants <2 years of age aim to improve prelinguistic skills and other forms of communication. A successful example of this type of therapy is ‘responsivity teaching and prelinguistic milieu teaching’, a speech/ language intervention that combines both parent and child training. In children with severe developmental and cognitive delays, it results in increased frequency of child-initiated comments and requests, as well as lexical density.37 Some communication interventions, such as the Mother–Infant Transaction Program and its modification, PremieStart, are targeted specifically at infants during their NICU hospitalisation.38 PremieStart improves mother–infant dyad interactions through an intensive training programme in NICU, followed by a session after discharge. Parents are trained to recognise and minimise stress responses in preterm infants and are taught non-verbal communication tools such as touch, movement and multisensory interactions. At 6 months after the intervention, infants in PremieStart had significantly higher scores compared with controls on the Symbolic Behavior Scales Developmental Profile. A Cochrane review39 studied the effectiveness of a variety of speech and language therapy interventions (including individual and group, and administration by therapist or trained parents) for children with primary speech and language disorders. When limited to interventions for children <2 years of age, the analysis demonstrates moderate effectiveness of interventions aimed at speech and expressive language evaluated at preschool and school age, but no conclusive evidence with regards to receptive language.
Behavioural Interventions
Former NICU infants are at increased risk of developing challenging behavioural problems throughout childhood, such as autism spectrum disorders (ASDs) and internalising behaviours (potential precursors of anxiety and depression in childhood and adolescence). However, most of these diagnoses are still evolving in the first two years and difficult to establish with certainty. Measurements of eye contact have shown promise in diagnosing ASDs in infancy;40 however, these tools require extensive training and equipment and thus are still far from being widely used. Mounting evidence suggests that earlier identification and treatment of ASDs results in improved outcomes and decreased socioeconomic burden. A systematic review of interventions in infants and toddlers, not targeted at survivors of neonatal intensive care, concluded that both focused interventions (aimed at specific deficits, eg, repetitive behaviours) and comprehensive ones (aimed at improving overall functioning) result in moderate to large effects on social communication skills such as prelinguistic joint-attention and social reciprocity.41
Conclusion
Specialists in disciplines including neurology, ophthalmology, audiology, psychology, neonatology, developmental medicine, physical medicine and rehabilitative therapies are improving the outcomes of NICU graduates. Progress has been made in sensory and motor neurorehabilitation through large multicentre studies and collaborations between subspecialties. Less is known about rehabilitation of more complex functions such as cognition, communication and behaviour but promising therapies include involving parents through education or active participation and directed application of principles of infant learning, psychology and the neuroscience of connectivity. Important challenges include the rapidly changing brain of an infant or child, the difficulties of establishing stable or functionally based diagnoses, the rarity of infant-specific studies of brain plasticity and the paucity of registries for specific developmental disorders. Further advances will depend on increased knowledge in all these areas through transdisciplinary research. Given current scientific imperatives and large projects such as the European Brain Project and US Brain Initiative, as well as worldwide connectivity, it is reasonable to expect exponential progress in all areas of infant neurorehabilitation in the near future. These accomplishments will make it possible for physicians who care for NICU infants to not only predict developmental problems but also offer the hope of overcoming them.
Footnotes
Competing interests None.
Provenance and peer review Commissioned; externally peer reviewed.
References
- 1.Mwaniki MK, Atieno M, Lawn JE, et al. Long-term neurodevelopmental outcomes after intrauterine and neonatal insults: a systematic review. Lancet. 2012;379:445–52. doi: 10.1016/S0140-6736(11)61577-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thompson RA, Nelson CA. Developmental science and the media. Early brain development. Am Psychol. 2001;56:5–15. doi: 10.1037/0003-066x.56.1.5. [DOI] [PubMed] [Google Scholar]
- 3.Galván A. Neural plasticity of development and learning. Hum Brain Mapp. 2010;31:879–90. doi: 10.1002/hbm.21029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Miller SP, Ferriero DM. From selective vulnerability to connectivity: insights from newborn brain imaging. Trends Neurosci. 2009;32:496–505. doi: 10.1016/j.tins.2009.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization. International classification of functioning, disability, and health. World Health Organization; 2007. [Google Scholar]
- 6.Kuhnke N, Juenger H, Walther M, et al. Do patients with congenital hemiparesis and ipsilateral corticospinal projections respond differently to constraint-induced movement therapy? Dev Med Child Neurol. 2008;50:898–903. doi: 10.1111/j.1469-8749.2008.03119.x. [DOI] [PubMed] [Google Scholar]
- 7.Wolff R, Hommerich J, Riemsma R, et al. Hearing screening in newborns: systematic review of accuracy, effectiveness, and effects of interventions after screening. Arch Dis Child. 2010;95:130–5. doi: 10.1136/adc.2008.151092. [DOI] [PubMed] [Google Scholar]
- 8.Nikolopoulos TP, Vlastarakos PV. Treating options for deaf children. Early Hum Dev. 2010;86:669–74. doi: 10.1016/j.earlhumdev.2010.10.001. [DOI] [PubMed] [Google Scholar]
- 9.Tomblin JB, Oleson JJ, Ambrose SE, et al. The influence of hearing aids on the speech and language development of children with hearing loss. JAMA Otolaryngol Head Neck Surg. 2014;140:403–9. doi: 10.1001/jamaoto.2014.267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.VanderVeen DK, Bremer DL, Fellows RR, et al. Prevalence and course of strabismus through age 6 years in participants of the Early Treatment for Retinopathy of Prematurity randomized trial. J AAPOS. 2011;15:536–40. doi: 10.1016/j.jaapos.2011.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Edwards AD, Brocklehurst P, Gunn AJ, et al. Neurological outcomes at 18 months of age after moderate hypothermia for perinatal hypoxic ischaemic encephalopathy: synthesis and meta-analysis of trial data. BMJ. 2010;340:c363. doi: 10.1136/bmj.c363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Garcia ML, Ty EB, Taban M, et al. Systemic and ocular findings in 100 patients with optic nerve hypoplasia. J Child Neurol. 2006;21:949–56. doi: 10.1177/08830738060210111701. [DOI] [PubMed] [Google Scholar]
- 13.Davidson S, Quinn GE. The impact of pediatric vision disorders in adulthood. Pediatrics. 2011;127:334–9. doi: 10.1542/peds.2010-1911. [DOI] [PubMed] [Google Scholar]
- 14.Gunton KB. Advances in amblyopia: what have we learned from PEDIG trials? Pediatrics. 2013;131:540–7. doi: 10.1542/peds.2012-1622. [DOI] [PubMed] [Google Scholar]
- 15.Taylor K, Elliott S. Interventions for strabismic amblyopia. Cochrane Database Syst Rev. 2014;7:CD006461. doi: 10.1002/14651858.CD006461.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Elliott S, Shafiq A. Interventions for infantile esotropia. Cochrane Database Syst Rev. 2013;7:CD004917. doi: 10.1002/14651858.CD004917.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Goyen TA, Lui K, Woods R. Visual-motor, visual-perceptual, and fine motor outcomes in very-low-birthweight children at 5 years. Dev Med Child Neurol. 1998;40:76–81. doi: 10.1111/j.1469-8749.1998.tb15365.x. [DOI] [PubMed] [Google Scholar]
- 18.Tsai LT, Meng LF, Wu WC, et al. Effects of visual rehabilitation on a child with severe visual impairment. Am J Occup Ther. 2013;67:437–47. doi: 10.5014/ajot.2013.007054. [DOI] [PubMed] [Google Scholar]
- 19.Walker SM, Franck LS, Fitzgerald M, et al. Long-term impact of neonatal intensive care and surgery on somatosensory perception in children born extremely preterm. Pain. 2009;141:79–87. doi: 10.1016/j.pain.2008.10.012. [DOI] [PubMed] [Google Scholar]
- 20.Grunau RE, Whitfield MF, Petrie-Thomas J, et al. Neonatal pain, parenting stress and interaction, in relation to cognitive and motor development at 8 and 18 months in preterm infants. Pain. 2009;143:138–46. doi: 10.1016/j.pain.2009.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chorna O, Solomon JE, Slaughter JC, et al. Abnormal sensory reactivity in preterm infants during the first year correlates with adverse neurodevelopmental outcomes at 2 years of age. Arch Dis Child Fetal Neonatal Ed. 2014;99:F475–9. doi: 10.1136/archdischild-2014-306486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Novak I, Mcintyre S, Morgan C, et al. A systematic review of interventions for children with cerebral palsy: state of the evidence. Dev Med Child Neurol. 2013;55:885–910. doi: 10.1111/dmcn.12246. [DOI] [PubMed] [Google Scholar]
- 23.Shepherd RB. Cerebral palsy in infancy. Elsevier Health Sciences. 2013 [Google Scholar]
- 24.Vienna, Austria: 2014. Early Identification and Early Neurorehabilitation in Cerebral Palsy. http://impact.cerebralpalsy.org.au/activities/research-summits/2014-summit/ [Google Scholar]
- 25.Novak I. Evidence-based diagnosis, health care, and rehabilitation for children with cerebral palsy. J Child Neurol. 2014;29:1141–56. doi: 10.1177/0883073814535503. [DOI] [PubMed] [Google Scholar]
- 26.Eliasson AC, Strand LS, Ek L, et al. Efficacy of baby-CIMT: study protocol for a randomised controlled trial on infants below age 12 months, with clinical signs of unilateral CP. BMC Pediatr. 2014;14:141. doi: 10.1186/1471-2431-14-141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Guzzetta A, Boyd RN, Perez M, et al. UP-BEAT (Upper Limb Baby Early Action-observation Training): protocol of two parallel randomised controlled trials of action-observation training for typically developing infants and infants with asymmetric brain lesions. BMJ Open. 2013;3:e002512. doi: 10.1136/bmjopen-2012-002512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Howe TH, Wang TN. Systematic Review of Interventions Used in or Relevant to Occupational Therapy for Children With Feeding Difficulties Ages Birth–5 Years. Am J Occup Ther. 2013;67:405–12. doi: 10.5014/ajot.2013.004564. [DOI] [PubMed] [Google Scholar]
- 29.Arvedson J, Clark H, Lazarus C, et al. Evidence-based systematic review: effects of oral motor interventions on feeding and swallowing in preterm infants. Am J Speech Lang Pathol. 2010;19:321–40. doi: 10.1044/1058-0360(2010/09-0067). [DOI] [PubMed] [Google Scholar]
- 30.Spittle A, Orton J, Anderson P, et al. Early developmental intervention programmes post-hospital discharge to prevent motor and cognitive impairments in preterm infants. Cochrane Database Syst Rev. 2012;12:CD005495. doi: 10.1002/14651858.CD005495.pub3. [DOI] [PubMed] [Google Scholar]
- 31.Heckman JJ. Schools, Skills, and Synapses. Econ Inq. 2008;46:289. doi: 10.1111/j.1465-7295.2008.00163.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Vanderveen JA, Bassler D, Robertson CMT, et al. Early interventions involving parents to improve neurodevelopmental outcomes of premature infants: a meta-analysis. J Perinatol. 2009;29:343–51. doi: 10.1038/jp.2008.229. [DOI] [PubMed] [Google Scholar]
- 33.Atkinson J, Braddick O. Visual attention in the first years: typical development and developmental disorders. Dev Med Child Neurol. 2012;54:589–95. doi: 10.1111/j.1469-8749.2012.04294.x. [DOI] [PubMed] [Google Scholar]
- 34.Wass S, Porayska-Pomsta K, Johnson MH. Training attentional control in infancy. Curr Biol. 2011;21:1543–7. doi: 10.1016/j.cub.2011.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Barre N, Morgan A, Doyle LW, et al. Language abilities in children who were very preterm and/or very low birth weight: a meta-analysis. J Pediatr. 2011;158:766–774.e1. doi: 10.1016/j.jpeds.2010.10.032. [DOI] [PubMed] [Google Scholar]
- 36.Marino BS, Lipkin PH, Newburger JW, et al. Neurodevelopmental outcomes in children with congenital heart disease: evaluation and management: a scientific statement from the American Heart Association. Circulation. 2012;126:1143–72. doi: 10.1161/CIR.0b013e318265ee8a. [DOI] [PubMed] [Google Scholar]
- 37.Yoder PJ, Warren SF. Effects of prelinguistic milieu teaching and parent responsivity education on dyads involving children with intellectual disabilities. J Speech Lang Hear Res. 2002;45:1158–74. doi: 10.1044/1092-4388(2002/094). [DOI] [PubMed] [Google Scholar]
- 38.Milgrom J, Newnham C, Martin PR, et al. Early communication in preterm infants following intervention in the NICU. Early Hum Dev. 2013;89:755–62. doi: 10.1016/j.earlhumdev.2013.06.001. [DOI] [PubMed] [Google Scholar]
- 39.Law J, Garrett Z, Nye C. Speech and language therapy interventions for children with primary speech and language delay or disorder (Review) Cochrane Database Syst Rev. 2003;(3):CD004110. doi: 10.1002/14651858.CD004110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jones W, Klin A. Attention to eyes is present but in decline in 2-6-month-old infants later diagnosed with autism. Nature. 2013;504:427–31. doi: 10.1038/nature12715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Morgan LJ, Rubin E, Coleman JJ. Impact of social communication interventions on infants and Toddlers with or at-risk for Autism A systematic review. Focus Autism Dev Disabil. 2014 Published Online First. [Google Scholar]


