Abstract
Introduction
Training community health workers (CHWs) builds a workforce that is essential to addressing the chronic disease crisis. This article describes a highly replicable CHW training program that targets heart disease risk among African American women.
Background
African American women suffer disproportionately from heart disease mortality and morbidity. Well-trained CHWs are uniquely positioned to close this disparity gap.
Method
We used a Learning Circle approach to train CHWs in heart health education. The curriculum blended web-based, self-directed learning and in-person peer coaching. CHWs learned through (a) peer-to-peer sharing, (b) problem solving and brainstorming, and (c) leadership and experiential activities. Training evaluation measures were CHWs' (a) self-confidence, (b) heart health knowledge, (c) satisfaction with training, (d) training retention, and (e) replication of training within 90 days after training.
Results
This training resulted in appreciable effects on four of five outcome measures. Heart health knowledge increased significantly among experienced CHWs (p = .011). CHWs were satisfied with training and retention was 100%. CHWs initiated and subsequently delivered 122 person hours of community heart health education and CHW training in their communities.
Discussion/Conclusion
CHW heart health training using Learning Circles is a practical and replicable method of training CHWs and holds significant potential for building capacity in resource-poor community organizations.
Keywords: cardiovascular disease, chronic disease, health disparities, health education, lay health advisors/community health workers, workforce development, Black/African American, minority health
Introduction
An appreciation for the role of community health workers (CHWs) has been steadily gaining in traction and favorability. CHWs perform a valuable role comparable to other health and social services paraprofessionals and are often able to meet the needs of community members that are not being met through the existing workforce of health professionals. There is widespread evidence that CHWs are uniquely positioned to serve as cultural brokers between community members and structural institutions such as the health care and social service systems and help health care professionals respond more appropriately to the community's needs.
The recognition of CHWs as an important part of the health care workforce has led to numerous initiatives in the private and public sectors to negotiate the integration of CHWs into the health care and social service systems. Many entities are committed to developing alternative health care delivery systems in which CHWs are an integral part of the broad spectrum of health care delivery configurations and not simply demonstration projects. Key to this integration is the identification and evaluation of the best practices in traditional and innovative CHW training methodologies. The peer-to-peer training model that was implemented is based on the expectation that CHWs will not only learn themselves but also train others, leading to an institutionalization of heart health education programs that are sustainable beyond limited funding periods.
Background
A growing body of research provides evidence that CHWs are effective in improving individual health status and building community capacity in preventive health care (Brownstein, 2008; Rosenthal, de Heer, Rush, & Holderby, 2008). Large-scale efforts to integrate CHWs into the U.S. health care delivery and social service systems as key constituents of the health care workforce have not yet come to fruition. Numerous reports have delineated the impact of CHWs in community health education and promotion once trained; however, we have little evaluative insight into the best methodological and theoretical practices that should guide the development of CHW peer-to-peer training programs. The fragmentation of CHW training, lack of consistency across training programs, and disparate variability in CHW roles and responsibilities further exacerbate the challenge. This article contributes to filling an important gap in CHW training.
The Patient Protection and Affordable Care Act (PPACA) of 2010 is one vehicle for integration of CHWs and defines a CHW as an “individual who promotes health or nutrition within the community in which the individual resides.” Systematic literature reviews provide strong support for the efficacy and cost-effectiveness of CHWs across a range of health system processes and conditions, including hypertension screening and control (Brownstein et al., 2007), diabetes self-management (Norris et al., 2006), cancer screening (Mock et al., 2007; Wells et al., 2011), asthma control (Margellos-Anast, Gutierrez, & Whitman, 2012; Parker et al., 2008), improving prenatal care (McGlade, Saha, & Dahlstrom, 2004), and HIV/AIDS prevention (Sánchez, Silva-Suarez, Serna, & De La Rosa, 2012). Because CHWs have close ties to the communities they serve, they are able to deliver cost-effective health education and health promotion and prevention services in a more culturally appropriate manner, reach populations that are inaccessible via conventional methods, improve provider–client communication, and increase the impact of outreach efforts through ongoing contact (Kelly et al., 1991; Rhodes, 1994; Viswanathan et al., 2009).
In addition to variability in training, another salient need in CHW training is the development of replicable, explicitly theory-based methods for training CHWs who have no formal education in health care fields. It is imperative that CHW training is highly accessible and culturally sensitive and increases information retention and appropriate use. This training initiative for heart health promotion addresses the dearth of information in CHW peer training methodology. Although there are efforts underway to standardize training for CHWs in Georgia, it will likely include many of the standard didactic methods already in practice in Georgia and other states (Pullen-Smith, Carter-Edwards, & Leathers, 2008). However, including peer-led approaches is one way to support the robustness of standardized training. Furthermore, peer-led approaches must be implemented with reasonable fidelity in both institutionalized CHW training and at the less formal community organization level.
Purpose
The Peer-to-Peer Training of Community Health Workers to Improve Heart Health Among African American Women Project was conceptualized to address the increased risk of heart disease among African American women in the local priority area. African American women suffer disproportionately from heart disease mortality and morbidity. CHWs are uniquely positioned to close this disparity. The training initiative incorporated adult participatory learning principles with blended learning delivery of heart health education content. This article describes the training initiative, designed as structured peer learning, to build capacity among a cadre of CHWs and affiliated organizations who are delivering cardiovascular health education to African American women. This training used the National Heart, Lung, and Blood Institute (NHLBI) With Every Heartbeat Is Life: A Community Health Worker's Manual for African Americans (WEHL). Training was designed to (a) increase knowledge of heart healthy habits among CHWs who serve predominantly African American female populations, (b) enhance the core competencies of CHWs who predominantly serve African American females, and (c) build a replicable and sustainable CHW training model for community organizations to address heart health using CHWs as health educators.
The scientific literature is replete with studies indicating that ethnic/racial minority women are at a disproportionally higher risk for morbidity and mortality from heart disease. African American, Hispanic, and Asian women are less aware of heart disease risk and prevention information compared to White women and this disparity has not changed significantly in 15 years (Christian, Rosamond, White, & Mosca, 2007; Mosca, Hammond, Mochari-Greenberger, Towfighi, & Albert, 2013). Mosca, Mochari-Greenberger, Dolor, Newby, and Robb (2010) found that compared to 60% of White women who knew that heart disease was a leading cause of death among women, only 43% of Black women, 44% of Hispanic women, and 34% of Asian women were aware. This is significant because awareness of cardiovascular disease risk has been linked to taking preventive action. Many women remain unfamiliar with heart disease symptoms and what to do if they experience them (Mosca et al., 2010).
The subsequent roles and responsibilities of CHWs post training significantly affect the design of the “training process.” The CHWs participating in this project were being prepared to engage community members in heart health education guided by stage of change assessments, behavior change strategies, and active listening. The training methodology we chose to apply was a peer-to-peer model informed by the participatory approach to adult learning (Jurmo, 1989), an educational methodology first pioneered as the Freirean approach to adult literacy education (Freire, 1970). Participatory learning encourages participants to share their opinions, generate innovative ideas, make informed decisions, evaluate personal experiences, make training enjoyable, and apply principles learned to everyday life.
CHWs are typically considered nontraditional learners, and the peer-to-peer approach employed in this study leaned heavily on knowledge acquisition through less formal participant-directed dialogue as compared to didactics. The peer-to-peer training model was selected over more traditional formal training models because it most closely approximates the typical facilitation styles of CHWs who serve in the role of peer health educators and outreach workers. It also promotes rapid assimilation of large amounts of new information since CHWs are actively engaged and are able to learn about heart health through their own experiences and get relevant skill practice with support and input from their peers and a master facilitator. The strength of participatory peer-led learning is its focus on the learner, personal experiences, group learning, and a reciprocal teaching–learning relationship where the facilitation process enhances both the individual doing the teaching and the one being taught (Topping & Ehly, 2001). CHW training methods, such as role-playing, didactic presentations, experiential learning, or mentored one-on-one learning (Ruiz et al., 2012), are inconsistently reported in the literature and, when described in isolation, generally contrast sharply in key areas with the peer learning approach we describe here. Furthermore, few previous reports identify peer-to-peer participatory training approaches as the primary CHW training method (O'Brien, Squires, Bixby, & Larson, 2009) and even fewer identify the fundamental theory and methodology used to design and deliver CHW training curricula. Here we used the peer-to peer model as our participatory training methodology and approach to adult learning.
Method
Recruitment
CHW recruitment was designed as a stepwise, multiphase process, which included (a) recruitment of community-based organizations (CBOs) and faith-based organizations (FBOs) that had existing relationships with CHWs, with a focus on cardiovascular disease prevention or women's health; (b) recruitment of experienced CHWs who serve the priority area and are formally affiliated with a CBO/an FBO; (c) CHW résumé review and interview; and (d) CHW selection and invitation to training.
We recruited CHWs through the Georgia Community Health Workers Network e-mail list and through the newsletter of an academic medical center that regularly uses CHWs. Recruitment was also conducted through presentations, referrals from Georgia Department of Public Health District Officers, and organizations identified through an ad hoc environmental scan conducted by project staff.
Trainees
In response to the multiple challenges faced with recruiting in a stepwise fashion, the recruitment protocol was amended to recruit both community organizations and CHWs simultaneously. Eligibility requirements were also amended to include CHWs whose affiliation and work with CBOs/FBOs is less formal and less structured.
Forty-four CHWs responded to recruitment and 37 eligible CHWs completed the application process. Twenty-five CHWs were selected to receive the training. The selection process included a review of CHWs' experience, their performance in a phone interview, and a letter of support from their affiliated CBO/FBO. Training of two cohorts (n = 10) and (n = 15) were conducted 30 days apart.
Training: Learning Circle Training
In-person training was delivered using a Learning Circle approach, a highly interactive group participation method that helps create meaning and drive understanding (Riel & Polin, 2004) and where learners actively create learning content for themselves and others. Each training cycle required a 28-hour time commitment over 2 weeks and provided CHWs with a stipend. The Learning Circle supported participation from all CHWs while providing participants with the WEHL heart health content, tools to assimilate and subsequently communicate heart health information, and the confidence to be an engaged peer learner. CHWs were trained to model their subsequent community education and CHW training initiatives using Learning Circle methods. The peer-led learner experience was modeled so that CHWs learned heart health content through (a) peer sharing and listening, (b) problem solving and problem posing/brainstorming, and (c) leadership and experiential learning. Each of the 10 heart-related sessions lasted 90 to 120 minutes and covered areas such as heart anatomy; risk factors for heart disease, heart attacks, and stroke; diet and exercise; comorbid conditions that affect heart disease risk; and smoking cessation. An additional session focused on CHW core competency training was a 7-hour session.
Peer Sharing and Listening
Every session began with both informal opportunities for open dialogue and a guided review of information covered in previous sessions. Ongoing discussion incorporated personal experiences and reaction to—or recollection of—previous sessions. Room seating enhanced the training environment. A horseshoe seating arrangement conveyed a sense of visual connectedness and “equality of status” among learners and provided flexibility for breakout group work.
Problem Solving and Problem Posing/Brainstorming
This was another important aspect of the training. CHWs completed problem-solving exercises as a large group and in dyads, typically using case scenarios and prepared exercises. These varied from simple exercises to role-playing to opportunities to create new training content. The brainstorming/problem-posing exercises, in contrast, were used to create options for resolving CHWs' hypothetical and real-life problems. In these exercises, the directive is not to seek consensus or achieve resolution but primarily to generate actionable options for the problems posed.
Leadership and Experiential Learning
This was integrated throughout the training experience. The CHWs had multiple opportunities to lead their peers through sections of the WEHL manual and facilitate exercises. Each CHW was also required to facilitate an abbreviated train-the-trainer session with their peers. Incorporating opportunities for group leadership and group facilitation throughout training gave CHWs simulated exposure to training facilitation.
Training: Self-Directed/Web-Based Training
The WEHL curriculum was adapted to create Web-based learning resources, including brief study guides, audio/video presentations that supported self-directed learning, and access to other NHLBI educational resources, including the electronic versions of the WEHL manual and accompanying picture cards. This content, consisting of 10 PowerPoint presentations, 10 videos, and other text available on the project website and YouTube channel, remains publicly accessible for CHWs to use in facilitating their own CHW trainings and community education sessions.
Evaluation Plan
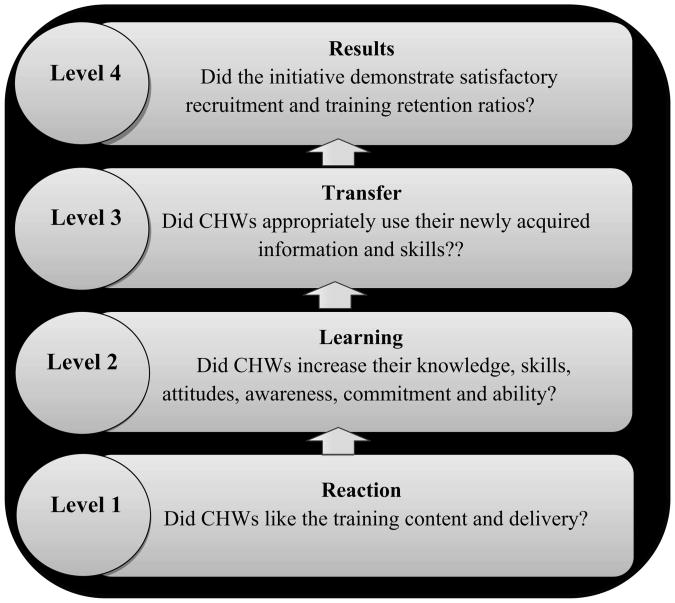
Figure 1 outlines Kirkpatrick's (1998) evaluation model that guided the evaluation of the peer-to-peer CHW heart health training. The Kirkpatrick four-level training evaluation model is one of the most widely used methods for evaluating training and learning. It provides opportunity to measure the effectiveness of training and identify areas for improvement. The four levels are (a) Reaction: Did CHWs like the training? (b) Learning: Did CHWs knowledge and skills increase? (c) Behavior: Was the new information and skills subsequently used? (d) Results: Did the initiative demonstrate appreciable impact? Although CHW training evaluations are as varied as the design of trainings themselves, this evaluation of CHW training assessed both the quality and effectiveness of training. It was consistent with recommendations in the literature that suggest that a comprehensive CHW training evaluation may reasonably include an assessment of (a) CHW knowledge via pretest–posttest or posttest, (b) CHW skills learned, (c) CHW perceptions of training, and (d) impact of training on CHW performance (Calhoun et al., 2010; Carter-Pokras et al., 2011; Kuhajda et al., 2006).
Figure 1. Kirkpatrick's Four Levels of evaluation.
The effectiveness of the training was operationalized using five outcome measures that paralleled the Kirkpatrick model. They were CHWs' (a) change in confidence to appropriately use WEHL manual, (b) change in heart health knowledge, (c) level of satisfaction with the training, (d) training retention, and (e) self-reported replication of training up to 90 days after training.
Data collection tools included a self-administered, pretest/posttest questionnaire (which scored a correct response as 1 point and an incorrect response as 0 points for a maximum score of 27); a training session evaluation form; a 30-day post-training feedback questionnaire; and a 90-day post-training feedback questionnaire. The self-administered assessment tools were provided by the initiative's national funders.
Statistical Analyses
The data analysis was generated using SAS software, Version 9.2. All outcomes were reported as percentages and the knowledge scores were assessed as means. The mean knowledge score change between pre- and posttest was analyzed using paired t tests. The Student t test or analysis of variance was used to compare the knowledge score changes between different demographic characteristics. The percentage change in confidence levels between pre- and posttest was assessed using McNemar test. CHW satisfaction with training was reported as percentages. A generalized linear model analysis was used to test the combined effect of several covariates on confidence, and knowledge. The statistical significance was set at p < .05 for all tests.
Results
Participating CHWs were predominantly female (85%) and self-identified as African American or Black (85%) and English speaking (100%). Forty-three percent of CHWs had less than a college degree. Other key demographic characteristics of the CHWs are described in Table 1. This training resulted in appreciable effects on four of five outcome measures.
Table 1. Demographic Characteristics of CHWs Participating in CHW Peer-to-Peer Heart Health Training Project.
| Demographic Characteristics | N = 21 | % |
|---|---|---|
| Gender | ||
| Female | 18 | 85.7 |
| Male | 3 | 14.3 |
| Country of birth | ||
| United States | 20 | 95.2 |
| Other | 1 | 4.8 |
| Education | ||
| GED/graduated from high School | 2 | 9.5 |
| Some technical/ vocational school | 1 | 4.8 |
| Graduated technical/ vocational school | 2 | 9.5 |
| Some college/university | 4 | 19.1 |
| Graduated college/university | 7 | 33.3 |
| Some postgraduate school | 4 | 19.1 |
| Graduated postgraduate school | 1 | 4.8 |
| CHW experience, years | ||
| <1 | 1 | 4.8 |
| 1-5 | 5 | 23.8 |
| 5-10 | 6 | 28.6 |
| >10 | 1 | 4.8 |
| No response | 3 | 14.3 |
Note: CHW = community health worker.
CHW Confidence
Prior to training, 52.6% of CHWs reported feeling “very confident” about teaching the NHLBI heart health content to others. After completing training, 66.6% of CHWs reported feeling “very confident” about teaching the NHLBI heart health content (p = .50; Table 2). Follow-up assessments of CHW confidence were administered at 30 and 90 days posttraining. At the 30-day assessment, CHW confidence levels for teaching the manual to community members remained fairly constant, with 63.1% of CHWs and 21.1% of CHW reporting being “very confident” and “confident,” respectively. At 90-day follow-up, there was a slight total increase in confidence among the CHWs who responded. Sixty percent (60.0%) of responding CHWs were “very confident” and 40.0% of CHWs were “confident” about teaching the manual to community members (p = .49). Fifteen of the CHWs who completed training and remained engaged with the project for 90 days conducted an additional 54 heart health education and CHW training events (x̄ = 3.6 sessions per trained CHW). They also delivered more than 122 person hours of heart health education (x̄ = 8.1 hours per trained CHW). There were no significant effects on confidence detected in generalized linear model analyses with the covariates of education, experience as CHWs, experience teaching cardiovascular topics, or being trained on the WEHL manual for the first time.
Table 2. CHW confidence to Teach Manual content and Information-Sharing Behavior.
| Outcome Measure | Pretest, N = 19 (%) | Posttest, N = 21 (%) | 30-Day, N = 19 (%) | 90-Day, N = 15 |
|---|---|---|---|---|
| Confidence | ||||
| Very confident | 10 (53) | 14 (67) | 12 (63) | 9 (60) |
| Confident | 6 (33) | 7 (33) | 4 (21) | 6 (40) |
| Somewhat confident | 1 (7) | — | 1 (7) | — |
| Not confident | — | — | 2 (11) | — |
| Missing data | 2 (11) | 2 (11) | 6 (32) | |
| Sharing information | ||||
| Community members | 7 (37) | 8 (42) | ||
| Other CHWs | 11 (60) | 15 (100) | ||
| Family | 19 (100) | 15 (100) | ||
| Changed own behavior | 19 (100) | 15 (100) | ||
| Missing data | 2 (11) | 6 (43) | ||
Note: CHW = community health worker.
CHW Knowledge
There was no significant change in overall group heart health knowledge scores from pretest to posttest. The largest absolute change in mean knowledge scores was seen as a 3-point, 4-point and 4.2-point gain in the scores of CHWs with high school education/vocational schooling or less, CHWs with previous experience teaching cardiovascular topics, and CHWs who were being trained in heart health for the first time, respectively (see Table 3). It was found that a significant increase in knowledge was associated with previous experience teaching cardiovascular topics. CHWs who had taught cardiovascular topics demonstrated significantly greater knowledge improvement (p = .011). Changes in knowledge approached significance for CHWs trained in heart health for the first time and CHWs with at least 3 years' experience as CHWs.
Table 3. CHW Heart Health Knowledge Before and After CHW Peer-to-Peer Heart Health Training Project.
| Outcome Measure, Knowledge | Pretest Score M (SD) | Posttest Score Δ (SD) | p |
|---|---|---|---|
| Overall | 21.05 (2.9) | −0.70 (2.8) | .231 |
| Education | .452 | ||
| High School graduate/vocational school graduate | 21.75 (3.2) | 3.0 (2.9) | |
| Some college or more | 21.87 (3.3) | 1.6 (3.0) | |
| CHW experience, years | .056 | ||
| <3 | 21.33 (1.1) | −2 (3.0) | |
| ≥3 | 20.1 (3.8) | 1.9 (2.7) | |
| First heart health training | .057 | ||
| Yes | 22.36 (3.5) | 1.07 (2.9) | |
| No | 20.40 (1.7) | 4.20 (1.6) | |
| Experience teaching cardiovascular disease topics | .011a | ||
| Yes | 20.00 (6.2) | 4.00 (3.1) | |
| No | 22.33 (1.9) | 1.33 (2.7) |
Significant p.
Training Satisfaction
The training was rated very favorably by the CHWs. The training content, handouts, visual demonstrations, activities, and facilitator delivery style were rated “good,” “very good,” or “excellent” by 95.0% of the CHWs. All the CHWs also indicated that they would share the information learned with community members, family, friends, and peers.
CHW Training Retention
Twenty-one CHWs successfully completed the heart health training. Supplemental Figure 1 (available at http://hpp.sagepub.com/supplemental) indicates no attrition during the 4-day training event, minimal attrition from the project 30 days later (9.5%), and moderate attrition after 90 days (28.5%) as measured by response rates for the 30-day and 90-day follow-up surveys.
Training Replication and Heart Health Information Sharing
At 30 days posttraining, 19 CHWs had shared information with family/friends and 94.7% had changed their personal health habits in response to information received during the training. By the 90-day assessment, 15 CHWs reported having shared information with family/friends and changing their health habits. Web-based resources were used by CHWs to support training efforts and as training boosters.
Discussion
Training resulted in appreciable effects on four of five outcome measures. Heart health knowledge increased significantly among experienced CHWs. CHWs were satisfied with training, and training retention was 100%. CHWs also initiated and subsequently delivered 122 person hours of community heart health education and CHW training in their local communities.
The Learning Circle approach is easily tailored and closely simulates CHWs' typical teaching and coaching style. The preliminary evaluation of this training initiative suggests that the methodology may work best for increasing heart health knowledge among experienced CHWs and CHWs who have some prior familiarity in the content area of focus. By virtue of their time in the field, they may be able to share more experiential information that resonates more closely with the experiences of their peers. However, both experienced and less experienced CHWs found that the training was informative and interesting and, most important, led to changes in their own personal health habits and gave them the confidence and content to coach others. Replications of this training will necessarily include a powered sample size to detect significant changes in CHW heart health knowledge and confidence to facilitate ongoing heart health education events.
This training method increases CHWs' confidence in being training facilitators, but that increase in confidence is likely sustainable only through immediate and proximal opportunities for the CHWs to facilitate heart health trainings themselves. Furthermore, although the gains in heart health knowledge within the group did not demonstrate significant increases, the move toward significance is promising and suggests that future iterations of training with a powered sample would lend much depth to what we already know about training CHWs. CHW heart health training using Learning Circles is a practical and replicable method of increasing CHW heart health knowledge and CHW skills. Twenty-one CHWs and 16 community partners have strengthened their skills and community capacity to replicate a sustainable community heart health education program.
Future implementations of this training will benefit from three key protocol amendments. First, facilitating an informational session for all CHWs/affiliated organization dyads before training begins would allow for a more detailed discussion of the needs and expectations of the CHWs and the CBOs/FBOs in a way that was not activated through one-on-one conversations. Second, CHWs expressed a desire to have more opportunities to simulate session planning and facilitation during training in order to build CHWs' confidence further. Third, a greater emphasis on cofacilitation among CHWs and collaborations between CBOs/FBOs in creating heart health education events may also increase the long-term effectiveness and sustainability of the training objectives.
Limitations
It was difficult to recruit CBOs that had CHWs as permanent and/or full-time employees as detailed in the original protocol. To handle this limitation, interested CHWs were encouraged to refer their affiliated organization to the program, and in turn, the organizations' leadership (CEO, directors) indicated support for CHWs' training by providing formal letters of support. The initiative also faced a moderate level of attrition within 90 days as CHWs transitioned to new jobs or assignments or dealt with personal challenges, resulting in incomplete follow-up data.
Sustainability
Without easily accessible opportunities for CHW training, a key community resource for improved cardiovascular health remains underused or untapped. Small CBOs/FBOs remain some of the best agents for grassroots risk behavior modification through their use of CHWs. However, they are often underfunded and lack the resources to routinely fund curriculum-tested training opportunities to their CHWs. Training and coaching CHWs to become trainers in their own organizations and communities provides a level of sustainability that bodes well for developing a cadre of CHWs to address heart health education and promotion.
Replicability
This project demonstrates a replicable method for delivering health-related content to CHWs not trained in health care in a way that is highly accessible and increases information retention and appropriate use. As demonstrated, even a small cadre of well-trained CHWs can replicate training when they are supported by committed CBOs and have reliable access to training resources such as literature, teaching aids, Web-based presentations, and a master trainer or CHW mentor.
Conclusion
The Learning Circle approach is a practical and reliable method for training and coaching CHWs in heart health promotion and education. It holds significant potential for building capacity in resource-poor community organizations, particularly among experienced CHWs who are uniquely positioned to mitigate against disparities in heart health morbidity and mortality in African American women.
Supplementary Material
Acknowledgments
Authors' Note: National Heart, Lung, and Blood Institute (Grant/Award No. HHSN268200900114U).
Footnotes
Supplemental Material: The supplemental material is available at http://hpp.sagepub.com/supplemental.
References
- Brownstein JN. Charting the course for community health worker research. Progress in Community Health Partnerships: Research, Education, and Action. 2008;2:177–178. doi: 10.1353/cpr.0.0024. [DOI] [PubMed] [Google Scholar]
- Brownstein JN, Chowdhury FM, Norris SL, Horsley T, Jack L, Jr, Zhang X, Satterfield D. Effectiveness of community health workers in the care of people with hypertension. American Journal of Preventive Medicine. 2007;32:435–447. doi: 10.1016/j.amepre.2007.01.011. [DOI] [PubMed] [Google Scholar]
- Calhoun EA, Whitley EM, Esparza A, Ness E, Greene A, Garcia R, Valverde PA. A national patient navigator training program. Health Promotion Practice. 2010;11:205–215. doi: 10.1177/1524839908323521. [DOI] [PubMed] [Google Scholar]
- Carter-Pokras OD, Jaschek G, Martinez IL, Brown PB, Mora SE, Newton N, Luciani I. Perspectives on Latino lay health promoter programs. American Journal of Public Health. 2011;101:2281–2286. doi: 10.2105/AJPH.2011.300317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christian AH, Rosamond W, White AR, Mosca L. Nine-year trends and racial and ethnic disparities in women's awareness of heart disease and stroke: An American Heart Association national study. Journal of Women's Health. 2007;16:68–81. doi: 10.1089/jwh.2006.M072. [DOI] [PubMed] [Google Scholar]
- Freire P. Pedagogy of the oppressed. New York, NY: Seabury; 1970. [Google Scholar]
- Jurmo P. The case for participatory literacy education. New Directions for Continuing Education. 1989;42:17–34. [Google Scholar]
- Kelly JA, St Lawrence JS, Diaz-Yolanda E, Stevenson LY, Hauth AC, Brasfield TL, et al. Andrew ME. HIV risk behavior reduction following intervention with key opinion leaders of population: An experimental analysis. American Journal of Public Health. 1991;81:186–171. doi: 10.2105/ajph.81.2.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirkpatrick DL. Evaluating training programs: The four levels. 2nd. San Francisco, CA: Berrett-Koehler; 1998. [Google Scholar]
- Kuhajda MC, Cornell CE, Brownstein JN, Littleton MA, Stalker VG, Bittner VA, et al. Raczynski JM. Training community health workers to reduce health disparities in Alabama's Black Belt: The Pine Apple Heart Disease and Stroke Project. Family & Community Health. 2006;29:89–102. doi: 10.1097/00003727-200604000-00005. [DOI] [PubMed] [Google Scholar]
- Margellos-Anast H, Gutierrez MA, Whitman S. Improving asthma management among African-American children via a community health worker model: Findings from a Chicago-based pilot intervention. Journal of Asthma. 2012;49:380–389. doi: 10.3109/02770903.2012.660295. [DOI] [PubMed] [Google Scholar]
- McGlade MS, Saha S, Dahlstrom ME. The Latina paradox: An opportunity for restructuring prenatal care delivery. American Journal of Public Health. 2004;94:2062–2065. doi: 10.2105/ajph.94.12.2062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mock J, McPhee SJ, Nguyen T, Wong C, Doan H, Lai KQ, et al. Bui-Tong N. Effective lay health worker outreach and media-based education for promoting cervical cancer screening among Vietnamese American women. American Journal of Public Health. 2007;97:1693–1700. doi: 10.2105/AJPH.2006.086470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mosca L, Mochari-Greenberger H, Dolor RJ, Newby LK, Robb KJ. Twelve-year follow-up of American women's awareness of cardiovascular disease risk and barriers to heart health. Circulation. 2010;3:120–127. doi: 10.1161/CIRCOUTCOMES.109.915538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mosca L, Hammond G, Mochari-Greenberger H, Towfighi A, Albert MA. Fifteen-year trends in awareness of heart disease in women: Results of a 2012 American Heart Association National Survey. Circulation. 2013;127:1254–1263. doi: 10.1161/CIR.0b013e318287cf2f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norris SL, Chowdhury FM, Van Le K, Horsley F, Brownstein JN, Zhang X, et al. Satterfield DW. Effectiveness of community health workers in the care of persons with diabetes. Diabetic Medicine. 2006;23:544–556. doi: 10.1111/j.1464-5491.2006.01845.x. [DOI] [PubMed] [Google Scholar]
- O'Brien M, Squires A, Bixby R, Larson S. Role development of community health workers: An examination of selection and training processes in the intervention literature. American Journal of Preventive Medicine. 2009;37(6 Suppl. 1):S262–S269. doi: 10.1016/j.amepre.2009.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker EA, Israel BA, Robins TG, Mentz G, Lin X, Brakefield-Caldwell W, et al. Lewis TC. Evaluation of community action against asthma: A community health worker intervention to improve children's asthma-related health by reducing household environmental triggers for asthma. Health Education & Behavior. 2008;35:376–395. doi: 10.1177/1090198106290622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Patient Protection and Affordable Care Act of 2010, H.R. 3590-3 Subtitle D, Sec 5313. Retrieved from http://www.gpo.gov/fdsys/pkg/BILLS-111hr3590enr/pdf/BILLS-111hr3590enr.pdf.
- Pullen-Smith B, Carter-Edwards L, Leathers KH. Community health ambassadors: A model for engaging community leaders to promote better health in North Carolina. Journal of Public Health Management and Practice. 2008;14(Suppl):S73–S81. doi: 10.1097/01.PHH.0000338391.90059.16. [DOI] [PubMed] [Google Scholar]
- Rhodes T. HIV outreach, peer education and community change: Developments and dilemmas. Health Education Journal. 1994;53:92–99. [Google Scholar]
- Riel M, Polin L. Online learning communities: Common ground and critical differences in designing technical environments. In: Barab SA, Kling R, Gray JH, editors. Designing for virtual communities in the service of learning. Cambridge, England: Cambridge University Press; 2004. pp. 16–50. [Google Scholar]
- Rosenthal EL, de Heer H, Rush CH, Holderby LR. Focus on the future: A community health worker research agenda by and for the field. Progress in Community Health Partnerships. 2008;2:183–184. doi: 10.1353/cpr.0.0025. [DOI] [PubMed] [Google Scholar]
- Ruiz Y, Matos S, Kapadia S, Islam N, Cusack A, Kwong S, Trinh-Shevrin C. Lessons learned from a community– academic initiative: The development of a core competency–based training for community–academic initiative community health workers. American Journal of Public Health. 2012;102:2372–2379. doi: 10.2105/AJPH.2011.300429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sánchez J, Silva-Suarez G, Serna CA, De La Rosa M. The Latino Migrant Worker HIV Prevention Program: Building a community partnership through a community health worker training program. Family & Community Health. 2012;35:139–146. doi: 10.1097/FCH.0b013e3182465153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Topping KJ, Ehly SW. Peer assisted learning: A framework for consultation. Journal of Educational and Psychological Consultation. 2001;12:113–132. [Google Scholar]
- Viswanathan M, Kraschnewski J, Nishikawa B, Morgan LC, Thieda P, Honeycutt A, et al. Jonas D. Prepared by the RTI International–University of North Carolina Evidence-Based Practice Center under Contract No 290 2007 10056 I, AHRQ Publication No 09-E014. Rockville, MD: Agency for Healthcare Research and Quality; 2009. Outcomes of community health worker interventions. Evidence Report/Technology Assessment No. 181. [Google Scholar]
- Wells KJ, Luque JS, Miladinovic B, Vargas N, Asvat Y, Roetzheim RG, Kumar A. Do community health worker interventions improve rates of screening mammography in the United States? A systematic review. Cancer Epidemiology Biomarkers & Prevention. 2011;20:1580–1598. doi: 10.1158/1055-9965.EPI-11-0276. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.