Abstract
Purpose
Interest in using T1 as a potential MRI biomarker of chronic obstructive pulmonary disease (COPD) has recently increased. Since tobacco smoking is the major risk factor for development of COPD, the aim for this study was to examine whether tobacco smoking, pack-years (PY), influenced T1 of the lung parenchyma in asymptomatic current smokers.
Materials and Methods
Lung T1 measurements from 35 subjects, 23 never smokers and 12 current smokers were retrospectively analyzed from an institutional review board approved study. All 35 subjects underwent pulmonary function test (PFT) measurements and lung T1, with similar T1 measurement protocols. A backward linear model of T1 as a function of FEV1, FVC, weight, height, age and PY was tested.
Results
A significant correlation between lung T1 and PY was found with a negative slope of -3.2 ms/year (95% confidence interval [CI] [-5.8, -0.6], p = 0.02), when adjusted for age and height. Lung T1 shortens with ageing among all subjects, -4.0 ms/year (95%CI [-6.3, -1.7], p = 0.001), and among the never smokers, -3.7 ms/year (95%CI [-6.0, -1.3], p = 0.003).
Conclusions
A correlation between lung T1 and PY when adjusted for both age and height was found, and T1 of the lung shortens with ageing. Accordingly, PY and age can be significant confounding factors when T1 is used as a biomarker in lung MRI studies that must be taken into account to detect underlying patterns of disease.
Introduction
Chronic obstructive pulmonary disease (COPD) is a complex heterogeneous disease that is a major cause of morbidity and mortality and is considered the third largest cause of death worldwide [1, 2]. There is a major need to develop new treatments for COPD, as no currently available drug therapy suppresses the persistent progression of the disease [3]. Whole-lung spirometric lung function tests are commonly used for characterization of COPD. However, these methods only measure global lung function, resulting in a loss of sensitivity in early/mild disease and pathophysiological abnormalities that may be present in this heterogeneous condition [4, 5]. Improved disease characterization of COPD is therefore needed as it will allow the use of personalised medicine approaches to COPD treatment, an emerging field in which imaging biomarkers are likely to play an important role [6].
In contrast to spirometric lung function tests, regional biomarkers in COPD lungs are sometimes obtained from computed tomography (CT) [7] or single-photon emission computed tomography (SPECT) [8]. The clinical benefits of CT and SPECT for diagnosis of COPD clearly outweigh the potential harmful effects due to ionizing radiation. However for clinical trials, particularly those including a placebo cohort, repeated exposure to ionizing radiation needs to be considered carefully given that there may be no clinical benefit of the examination to the subject. Therefore, non-ionizing radiation imaging techniques are preferred as alternatives in longitudinal assessments in patients with COPD and in therapy monitoring.
Magnetic resonance imaging (MRI) provides attractive biomarkers for assessment of lung disease in clinical trials as it is free from ionizing radiation, minimally invasive and provides regional information [9–11]. Lung MRI has been hampered by the low density of the lung and the fast signal decay due to susceptibility differences between tissue and air in lung parenchyma. Nevertheless, several lung MRI applications have been developed, and interest in MRI of the lungs has recently increased [9–13]. Specifically, it was recently found that the MR specific parameter T1 relaxation time (subsequently called T1) was shortened in lung for COPD patients [14]. T1 measurements of the lung can be used as a read-out to reflect lung function with oxygen-enhanced MRI [12, 15] and to measure partial pressure of oxygen in the alveolar airspaces using hyperpolarised gases [16].
Pulmonary diseases are previously known to influence lung T1 [17]. Oedema and inflammation lead to an increase in T1 compared to healthy lung tissue [18]. Shortening of T1 has been related to fibrosis [19] and emphysema [20]. These factors will also contribute to the T1 found in COPD patients. However, it is well established that tobacco smoking is a major factor for development of COPD [21, 22], i.e. smokers will be present in COPD cohorts. Smoking results in deposition of particles and coal tar in the lung that induces numerous biological mechanisms responsible for chronic inflammation of the airways and the lung parenchyma and eventually leads to degradation of the lung tissue [23]. Additionally, one could speculate that the presence of tar or other substances [24] that enhance dipolar relaxation in the extracellular tissue water and which accumulate in the lung as a direct consequence of smoking may shorten T1 directly or the subsequent lung damage may result in a T1 reduction. However, at present there are no specific data supporting this hypothesis. To our knowledge, the relationship between lung T1 and tobacco smoke (TS) exposure in healthy subjects has not been previously addressed.
The objective for the present study was to examine whether tobacco smoking influenced T1 of the lung parenchyma in individuals with no known lung disease. We performed lung T1 and pulmonary function test (PFT) measurements in asymptomatic current smokers with no diagnosis of lung disease and healthy age-matched never smokers. Healthy smokers were chosen in order to isolate smoking from disease related factors.
Materials and Methods
Ethics statement
The study was approved from an institutional review board of the Centre for Imaging Sciences, University of Manchester, UK and the ethical review board of Lund University, Lund, Sweden. All subjects gave written informed consent for examination and data evaluation. The written informed consent in the original study permitted future reanalysis of the data. The work was carried out in accordance with The Code of Ethics of the World Medical Association (Declaration of Helsinki).
Subjects
Lung T1 measurements from 35 volunteers, 23 never smokers and 12 current smokers were retrospectively analyzed. Eleven of the never smokers and the smokers were extracted from an existing study from Manchester, United Kingdom, center 1. The other never smokers were from an existing study in Malmö, Sweden, center 2. All 35 subjects underwent lung T1 and PFT measurements with a similar T1 measurement sequence. Each volunteer completed a questionnaire before recruitment to assess their suitability for the study. The enrolled subjects had no previous diagnosis of emphysema, bronchitis, chronic asthma, alpha1-antitrypsin deficiency, bronchiectasis or any other chronic lung disease. Any candidate who reported suffering from a cough or chest infection within eight weeks prior to participation was excluded. On the same questionnaire, volunteers recorded details of their smoking history including the smoking of tobacco products other than cigarettes and whether they were regularly exposed to passive smoke.
Pulmonary function test
Immediately prior, subsequent to or on the day following MRI scanning, standard PFT were carried out to assess forced expiratory volume in 1 s (FEV1 (% predicted)) and forced vital capacity (FVC (% predicted)). The measurements were carried out using a computerized spirometer system (Jaeger Oxycon Pro, Hoechberg, Germany) by a trained test administrator according to ATS/ERS standards [25].
MRI protocol center 1
Imaging was carried out on a 1.5 T-Philips Intera MR system (Philips Medical Systems, Best, Netherlands). In all acquisitions, the q-body coil was used for RF transmission and reception. Throughout the acquisition volunteers were breathing normally, and the imaging was carried out without the use of respiratory or cardiac triggering. A single coronal image slice was positioned at the posterior mediastinum. This slice position gave information on a large area of lung coverage, while avoiding the heart, and was also less likely to be affected by through-plane breathing motion (chest breathing) than more anterior slices. A snapshot FLASH (Fast Low Angle Shot) [26] was used with an initial non-selective inversion pulse. The imaging parameters were: repetition time (TR) 2.2 ms, echo time (TE) 1.0 ms, field of view (FOV) 450 x 450 mm2, flip angle (FA) 5°, 64 x 256 matrix (zero filled to 256 x 256) and a slice thickness of 15 mm. In all, 25 inversion times (TI) were used, with an initial TI of 74 ms acquired at intervals of 143 ms, and the measurement was repeated 10 times over a one minute period.
MRI protocol center 2
Imaging was performed on a 1.5 T-Siemens Magnetom Avanto Fit (Siemens Healthcare, Erlangen, Germany) with a similar approach, slice location and protocol to that used in center 1. Following a non-selective inversion pulse, 16 coronal TIs were acquired with the Snapshot FLASH (21) (TR 3 ms, TE 0.7 ms, FOV 450 x 450 mm2, FA 7°, 128 x 64 matrix zero filled to 256 x 256 and a slice thickness of 15 mm) ranging from 107 ms at intervals of 192 ms, during an light inspiration breath hold over 3 seconds.
Image analysis
Images were registered using techniques defined in [27] to remove respiratory motion in center 1, where free breathing was used, and T1 was obtained by fitting the Look-Locker equation [28] pixel-by-pixel for the single slice. A region of interest was manually placed on the left and right lungs and was used to calculate the median T1 value for each subject. The large pulmonary vessels were manually excluded in the quantification. All data analysis was performed using software written in Matlab (MATLAB, The MathWorks Inc., Natick, MA, USA).
Statistical analysis
First, a potential effect of center (Malmö/Manchester) on T1 was investigated using a multiple regression analysis adjusted for age, weight, height, FEV1 and FVC among the never smokers. The reason for including only the never smokers in this analysis was that never smokers were examined at both centers while all smokers had been examined at a single center. Thereafter, in order to select the most important variables in determining the value of T1, a backward linear model approach was used. The starting model included FEV1, FVC, weight, height, age and pack-years (number of years or equivalent years in which 20 cigarettes a day were smoked, PY) as covariates. Stepwise exclusion of the least significant covariate and refitting of the model was stopped when all remaining covariates showed a significance level of <0.1 with T1. A simpler model containing only PY and age was also examined, to compare the individual influence of PY and age on T1. When evaluating the two final models a p-value <0.05 was considered significant. Due to limited sample size the approach taken is exploratory, i.e. no correction for possible model over-fitting was applied. If not stated otherwise, the reported values are given as the mean ± one standard deviation (SD). Analyses were performed using RStudio (version 0.98.507).
Results
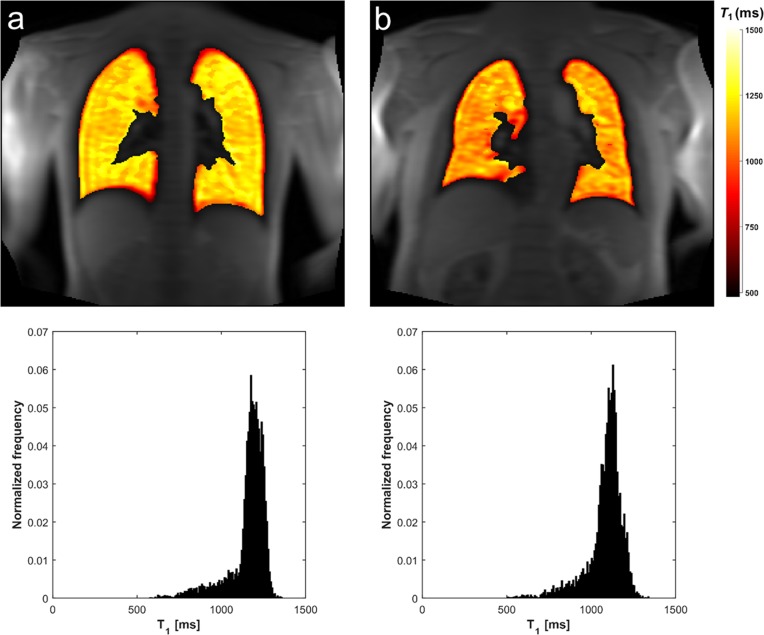
The MRI examinations were completed in all subjects with diagnostic quality. Representative lung T1 maps of two subjects with corresponding histograms are provided in Fig 1. The means ± SD of demographic and PFT parameters for all participants are given in Table 1. The current smokers had smoking histories ranging from 2 to 40 PY (mean 16 ± 12 PY) (Fig 2). The never smoking group included an ex-smoker with a smoking history of 2.5 PY. No significant difference on T1 was found between the centers among the never smokers from the multiple regression analysis (p = 0.35).
Fig 1. Lung T1 maps in a young and old never smoker.
Representative coronal lung MRI T1 maps overlaid on a signal intensity image with corresponding normalized T1 histograms for a 25 years old (a) and a 60 years old (b) never smoker.
Table 1. Demographic and pulmonary function data.
| Never smokers center 1 | Never smokers center 2 | Current smokers center 1 | |
|---|---|---|---|
| No. of subjects | 11 | 12 | 12 |
| No. of men | 4 | 6 | 6 |
| Age (y) | 29 ± 4 (23–35) | 44 ± 12 (26–61) | 43 ±10 (29–60) |
| Weight (kg) | 76 ± 14 (61–97) | 76 ± 13 (53–104) | 77 ± 21 (50–118) |
| Height (cm) | 171 ± 12 (150–186) | 175 ± 8 (167–188) | 173 ± 11 (159–184) |
| Smoking index (pack-years) | 0.2 ± 0.8 (0–1.2) | 0 | 16 ± 12 (2–40) |
| Pulmonary function measurement | |||
| FEV1 (%pred) | 99 ± 20 (69–124) | 104 ± 13 (85–130) | 102 ± 38 (39–197) |
| FVC (%pred) | 112 ± 29 (68–177) | 117 ± 13 (100–148) | 127 ± 34 (81–187) |
| FEV1/FVC | 0.77 ± 0.12 (0.55–0.88) | 0.89 ± 0.09 (0.75–1.04) | 0.67 ± 0.16 (0.37–0.91) |
Data are means ± standard deviations, with ranges in parentheses. Center 1 –Manchester, center 2 –Malmö. ND = no data.
Fig 2. Lung T1 as a function of age and PY for all subjects.
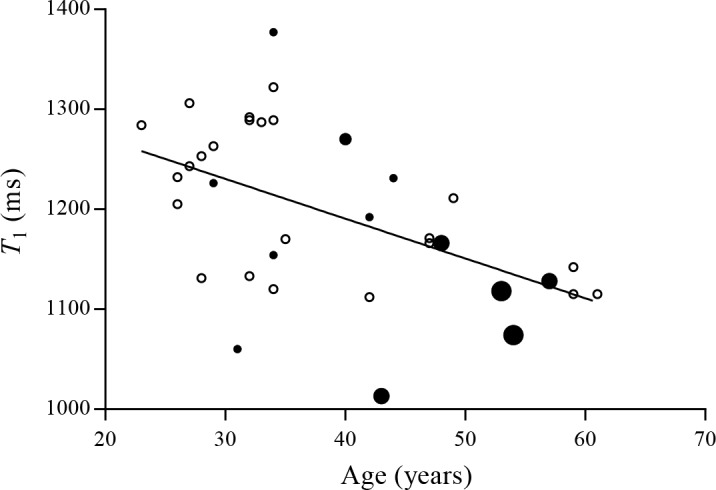
The example line shows the correlation between median lung T1 and age for smokers (●) and never smokers (○), indicating that lung T1 shortens with ageing (p<0.01, r = -0.52). The smoking history of the current smokers is visualized with increased size of the dots ( = 1–10 PY, = 11–20 PY, = 21–30 PY and = 31–40 PY).
Weight, FEV1 and FVC were stepwise excluded in the backward regression procedure for all subjects. The resulting model included PY, age and height as covariates with negative slopes of -3.2 ms/year (95% confidence interval [CI] [-5.8, -0.6], p = 0.02), -2.9 ms/year (95% CI [-5.3, -0.5], p = 0.02) and -2.4 ms/cm (95% CI [-5.0, 0.2], p = 0.07), respectively (Table 2). Excluding height in the simpler model, the slopes of T1 versus age and PY changed to -3.1 ms/year (95% CI [-5.5, -0.6], p = 0.02) and -2.3 ms/year (95% CI [-4.9, 0.3], p = 0.08), respectively. The negative slope was -4.0 ms/year (95% CI [-6.3, -1.7], p = 0.001) when only age was included in the model with r = -0.52, indicating that lung T1 shortens with ageing (Fig 2). Among the never smokers, the slope of T1 as a function of age was found to be -3.7 ms/year (95% CI [-6.0, -1.3], p = 0.003).
Table 2. Influence of covariates on T1 for all subjects (n = 35).
| Model | Covariates | Slopes [ms/x] | 95% CI | p |
|---|---|---|---|---|
| 1 | Height (cm) | -2.4 | [-5.0, 0.2] | 0.07 |
| Age (y) | -2.9 | [-5.3, 0.5] | 0.02 | |
| PY (y) | -3.2 | [-5.8, -0.6] | 0.02 | |
| 2 | Age (y) | -3.1 | [-5.5, -0.6] | 0.02 |
| PY (y) | -2.3 | [-4.9, 0.3] | 0.08 | |
| 3 | Age (y) | -4.0 | [-6.3, -1.7] | 0.001 |
| 4a | Age (y) | -3.7 | [-6.0, -1.3] | 0.003 |
aAmong never smokers, n = 23.
Discussion
Data from this study demonstrate that the association between PY and lung T1 changes from being significant (p = 0.02) when adjusted for both age and height to being non-significant when adjusted for age only, p = 0.08. There is a significant association between age and T1 in both final models (adjusted for height and PY, or adjusted for PY only), as well as in the univariate analysis in never smokers. When looking at the PY effect on T1, it is important to take into account the age of the subjects. Since there is an inherent colinearity between age and PY, it is more likely that subjects with more PY are older. Further investigations in larger cohorts will increase the knowledge of the lung T1 relationship to PY.
There is evidence showing smoke effect in other imaging studies. Fain et al. [29] found that mean ADC values and number of PY were significantly correlated and that relationship remained after adjustment for age with hyperpolarized helium 3 (3He) imaging. Additionally, Fain et al. also found a strong correlation between mean ADC values and age in both never smokers and healthy smokers. The relationship between ADC, indicating structural changes, and age was explained by microstructural changes in the lung related to the ageing process. 3He imaging is a highly sensitive lung imaging technique and the findings with ADC correlations to both PY and age confirms that. Recently, Hamedani et al. [30] found functional differences between never smokers, asymptomatic smokers and symptomatic smokers with heterogeneity metrics using 3He MR imaging. The smokers recruited in the above mentioned 3He imaging studies had similar smoking histories as the smokers in the present study. Taking this knowledge into account, i.e. that structural changes are indeed present in asymptomatic smokers; we might expect that a larger T1 study would increase the possibility to find a T1 relationship to PY. Moreover, literature to assist powering a lung MR T1 study is currently lacking. The results from the present study may be of utility to power future prospective studies to validate these biomarkers.
Recently, we found that lung T1 correlated to CT density and PFTs in an age-matched COPD cohort study, indicating the potential role of T1 mapping as a marker of early detection of COPD and emphysema [14]. The observed finding with shortened T1 in COPD patients was explained by smoking-induced lung pathology, specifically emphysema which was supported by the PFT and CT measurements. No link between lung T1 and PY was found in the COPD subjects. In the present study, the observed indication with shortened T1 in the smokers (p = 0.02, adjusted for age and height), therefore, most likely reflects early signs of smoking-induced lung pathology that is not evident from the spirometric measurements.
There are several potential explanations for the lung T1 relationship to age. In the healthy lung, the blood in the pulmonary circulation is the major source of the assessed lung T1 at conventional echo times [31]. Blood has a long T1 (>1000 ms at 1.5 T) [32] and is relatively close to lung T1 at TEs of the present study (0.7–1 ms). The pulmonary blood volume reduces with age [33] and might therefore explain the shortened lung T1 with ageing of the lung. The lung tissue of healthy subjects looses its supporting structure with age [34] causing emphysematous changes, which had been shown to shorten lung T1 [20]. Furthermore, factors such as reduced perfusion and increased macromolecular collagen content are causes that could shorten T1 in the ageing process of the lung. More accurate models may be constructed with further research incorporating parameters such as hematocrit, oxygenation and other relevant variables to explain the biology behind the T1 relationship to age. Nevertheless, on the basis of our results, age can be a significant confounding factor when T1 is used as a biomarker in lung MRI studies that must be taken into account to detect underlying patterns of disease.
There were several limitations with the present study. The small sample size and the study being performed at two centers with slightly different scanning protocols may have introduced an increased uncertainty. However, our multiple regression analysis found that there were no differences between the two centres and it should therefore not affect the analysis of the T1 measurements. Different breathing protocols were used with free breathing in center 1 and breath hold in light inspiration in center 2. Stadler et al. [20] that found a 50 ms difference between full inspiration and expiration, therefore these differences should not be significant for the T1 measurement. Moreover, the two centers had different TE, 1 ms in center 1 and 0.7 ms in center 2. Measured T1 depends on what TE is used in the assessment. According to the data from Thriphan et al. [31] we should have a systematic 50 ms bias, between the two centers, where center 1 would have longer T1. We do not believe these small changes affect the conclusions in this study. Another limitation with this study was the two-dimensional MRI protocol that was restricted to one slice and did not cover the whole lung. A multi-slice or three-dimensional protocol would be preferred for improved regional analysis of the smoking-induced effects. Moreover, with regards to the PY measure and the small cohort of smokers, PY is a course measure, as some subjects with very different smoking habit might end up with similar PY values. There was no information on the time between last smoke exposure and imaging.
Regarding these limitations, further prospective studies are desirable to further validate the utility of T1 mapping in the assessment of healthy smokers. In conclusion, we were able to show a significant relationship between lung T1 and PY when adjusted for both age and height. Additionally, lung T1 shortens with increasing age. Thus, PY and age can be significant confounding factors when T1 is used as a biomarker in lung MRI studies that must be taken into account to detect underlying patterns of disease.
Data Availability
All relevant data are within the paper.
Funding Statement
This work was supported by AstraZeneca and Allmänna Sjukhusets i Malmö stiftelse för bekämpande av Cancer. The funders provided support in the form of salaries for authors DFA, SSIK, SSY, and MO, but did not have any additional role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript. The specific roles of these authors are articulated in the ‘author contributions’ section.
References
- 1.Mannino DM, Watt G, Hole D, Gillis C, Hart C, McConnachie A, et al. The natural history of chronic obstructive pulmonary disease. European Respiratory Journal. 2006;27(3):627–43. 10.1183/09031936.06.00024605 [DOI] [PubMed] [Google Scholar]
- 2.World Health O. World Health Statistics 2008. Geneva, Switzerland: WHO Press; 2008. [Google Scholar]
- 3.Barnes PJ. Chronic obstructive pulmonary disease * 12: New treatments for COPD. Thorax. 2003;58(9):803–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bergin C, Müller N, Nichols DM, Lillington G, Hogg JC, Mullen B, et al. The diagnosis of emphysema. A computed tomographic-pathologic correlation. The American Review of Respiratory Disease. 1986;133(4):541 [DOI] [PubMed] [Google Scholar]
- 5.Swanney MP, Ruppel G, Enright PL, Pedersen OF, Crapo RO, Miller MR, et al. Using the lower limit of normal for the FEV1/FVC ratio reduces the misclassification of airway obstruction. Thorax. 2008;63(12):1046–51. 10.1136/thx.2008.098483 [DOI] [PubMed] [Google Scholar]
- 6.Agusti A. The path to personalised medicine in COPD. Thorax. 2014;69(9):857–64. 10.1136/thoraxjnl-2014-205507 [DOI] [PubMed] [Google Scholar]
- 7.Lynch DA. Imaging of small airways disease and chronic obstructive pulmonary disease. Clinics in chest medicine. 2008;29(1):165–79. 10.1016/j.ccm.2007.11.008 [DOI] [PubMed] [Google Scholar]
- 8.Jögi J, Ekberg M, Jonson B, Bozovic G, Bajc M. Ventilation/perfusion SPECT in chronic obstructive pulmonary disease: an evaluation by reference to symptoms, spirometric lungfunction and emphysema, as assessed with HRCT. European journal of nuclear medicine and molecular imaging. 2011;38(7):1344–52. 10.1007/s00259-011-1757-5 [DOI] [PubMed] [Google Scholar]
- 9.Wild JM, Marshall H, Bock M, Schad LR, Jakob PM, Puderbach M, et al. MRI of the lung (1/3): methods. Insights into imaging. 2012;3(4):345–53. 10.1007/s13244-012-0176-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Biederer J, Beer M, Hirsch W, Wild J, Fabel M, Puderbach M, et al. MRI of the lung (2/3). Why… when… how? Insights into imaging. 2012:1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Biederer J, Mirsadraee S, Beer M, Molinari F, Hintze C, Bauman G, et al. MRI of the lung (3/3)—current applications and future perspectives. Insights into imaging. 2012:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Morgan AR, Parker GJM, Roberts C, Buonaccorsi GA, Maguire NC, Cristinacce PLH, et al. Feasibility assessment of using oxygen-enhanced magnetic resonance imaging for evaluating the effect of pharmacological treatment in COPD. European Journal of Radiology. 2014;83(11):2093–101. 10.1016/j.ejrad.2014.08.004 [DOI] [PubMed] [Google Scholar]
- 13.Zhang W-J, Hubbard Cristinacce PL, Bondesson E, Nordenmark LH, Young SS, Liu Y-Z, et al. MR Quantitative Equilibrium Signal Mapping: A Reliable Alternative to CT in the Assessment of Emphysema in Patients with Chronic Obstructive Pulmonary Disease. Radiology. 2015. [DOI] [PubMed] [Google Scholar]
- 14.Alamidi DF, Morgan AR, Hubbard Cristinacce PL, Nordenmark LH, Hockings PD, Lagerstrand KM, et al. COPD Patients Have Short Lung Magnetic Resonance T1 Relaxation Time. COPD: Journal of Chronic Obstructive Pulmonary Disease. 2015:1–7. 10.3109/15412555.2015.1048851 [DOI] [PubMed] [Google Scholar]
- 15.Edelman RR, Hatabu H, Tadamura E, Li W, Prasad PV. Noninvasive assessment of regional ventilation in the human lung using oxygen–enhanced magnetic resonance imaging. Nature medicine. 1996;2(11):1236–9. [DOI] [PubMed] [Google Scholar]
- 16.Deninger AJ, Eberle B, Ebert M, Grossmann T, Heil W, Kauczor HU, et al. Quantification of Regional Intrapulmonary Oxygen Partial Pressure Evolution during Apnea by 3He MRI. Journal of Magnetic Resonance. 1999;141(2):207–16. [DOI] [PubMed] [Google Scholar]
- 17.Stadler A, Stiebellehner L, Jakob PM, Arnold JF, Eisenhuber E, von Katzler I, et al. Quantitative and o(2) enhanced MRI of the pathologic lung: findings in emphysema, fibrosis, and cystic fibrosis. International journal of biomedical imaging. 2007;2007:23624 10.1155/2007/23624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bottomley PA, Hardy CJ, Argersinger RE, Allen‐Moore G. A review of 1H nuclear magnetic resonance relaxation in pathology: are T1 and T2 diagnostic? Medical physics. 1987;14(1):1–37. [DOI] [PubMed] [Google Scholar]
- 19.Dasenbrook EC, Lu L, Donnola S, Weaver DE, Gulani V, Jakob PM, et al. Normalized T1 Magnetic Resonance Imaging for Assessment of Regional Lung Function in Adult Cystic Fibrosis Patients-A Cross-Sectional Study. PloS one. 2013;8(9):e73286 10.1371/journal.pone.0073286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stadler A, Jakob PM, Griswold M, Stiebellehner L, Barth M, Bankier AA. T1 mapping of the entire lung parenchyma: Influence of respiratory phase and correlation to lung function test results in patients with diffuse lung disease. Magnetic Resonance in Medicine. 2007;59(1):96–101. [DOI] [PubMed] [Google Scholar]
- 21.Hanrahan JP, Sherman CB, Bresnitz EA, Emmons KM, Mannino DM. Cigarette smoking and health. American Thoracic Society. American Journal of Respiratory and Critical Care Medicine. 1996;153(2):861–5. [DOI] [PubMed] [Google Scholar]
- 22.Marsh S, Aldington S, Shirtcliffe P, Weatherall M, Beasley R. Smoking and COPD: what really are the risks? European Respiratory Journal. 2006;28(4):883–4. 10.1183/09031936.06.00074806 [DOI] [PubMed] [Google Scholar]
- 23.Gerhardsson de Verdier M. The Big Three Concept. Proceedings of the American Thoracic Society. 2008;5(8):800–5. 10.1513/pats.200806-058TH [DOI] [PubMed] [Google Scholar]
- 24.Kilburn KH. Particles causing lung disease. Environmental health perspectives. 1984;55:97 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, et al. Standardisation of spirometry. Eur Respir J. 2005;26(2):319–38. [DOI] [PubMed] [Google Scholar]
- 26.Jakob PM, Hillenbrand CM, Wang T, Schultz G, Hahn D, Haase A. Rapid quantitative lung (1)H T(1) mapping. Journal of magnetic resonance imaging: JMRI. 2001;14(6):795–9. [DOI] [PubMed] [Google Scholar]
- 27.Naish JH, Parker GJM, Beatty PC, Jackson A, Young SS, Waterton JC, et al. Improved quantitative dynamic regional oxygen-enhanced pulmonary imaging using image registration. Magnetic Resonance in Medicine. 2005;54(2):464–9. 10.1002/mrm.20570 [DOI] [PubMed] [Google Scholar]
- 28.Deichmann R, Haase A. Quantification of T1 values by SNAPSHOT-FLASH NMR imaging. Journal of magnetic resonance. 1992;96(3):608–12. [Google Scholar]
- 29.Fain SB, Panth SR, Evans MD, Wentland AL, Holmes JH, Korosec FR, et al. Early Emphysematous Changes in Asymptomatic Smokers: Detection with 3He MR Imaging 1. Radiology. 2006;239(3):875–83. [DOI] [PubMed] [Google Scholar]
- 30.Hamedani H, Kadlecek SJ, Ishii M, Xin Y, Emami K, Han B, et al. Alterations of Regional Alveolar Oxygen Tension in Asymptomatic Current Smokers: Assessment with Hyperpolarized 3He MR Imaging. Radiology. 2014. [DOI] [PubMed] [Google Scholar]
- 31.Triphan SMF, Jobst BJ, Breuer FA, Wielpütz MO, Kauczor HU, Biederer J, et al. Echo time dependence of observed T1 in the human lung. Journal of Magnetic Resonance Imaging. 2015. [DOI] [PubMed] [Google Scholar]
- 32.Mai VM, Knight‐Scott J, Berr SS. Improved visualization of the human lung in 1H MRI using multiple inversion recovery for simultaneous suppression of signal contributions from fat and muscle. Magnetic resonance in medicine. 1999;41(5):866–70. [DOI] [PubMed] [Google Scholar]
- 33.Meinel FG, Graef A, Sommer WH, Thierfelder KM, Reiser MF, Johnson TRC. Influence of vascular enhancement, age and gender on pulmonary perfused blood volume quantified by dual-energy-CTPA. European Journal of Radiology. 2013;82(9):1565–70. 10.1016/j.ejrad.2013.04.019 [DOI] [PubMed] [Google Scholar]
- 34.Janssens J, Pache J, Nicod L. Physiological changes in respiratory function associated with ageing. European Respiratory Journal. 1999;13(1):197–205. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the paper.